Testing the Accuracy of Pont’s Index in Diagnosing Maxillary Transverse Discrepancy as Compared to the University of Pennsylvania CBCT Analysis
Abstract
:1. Introduction
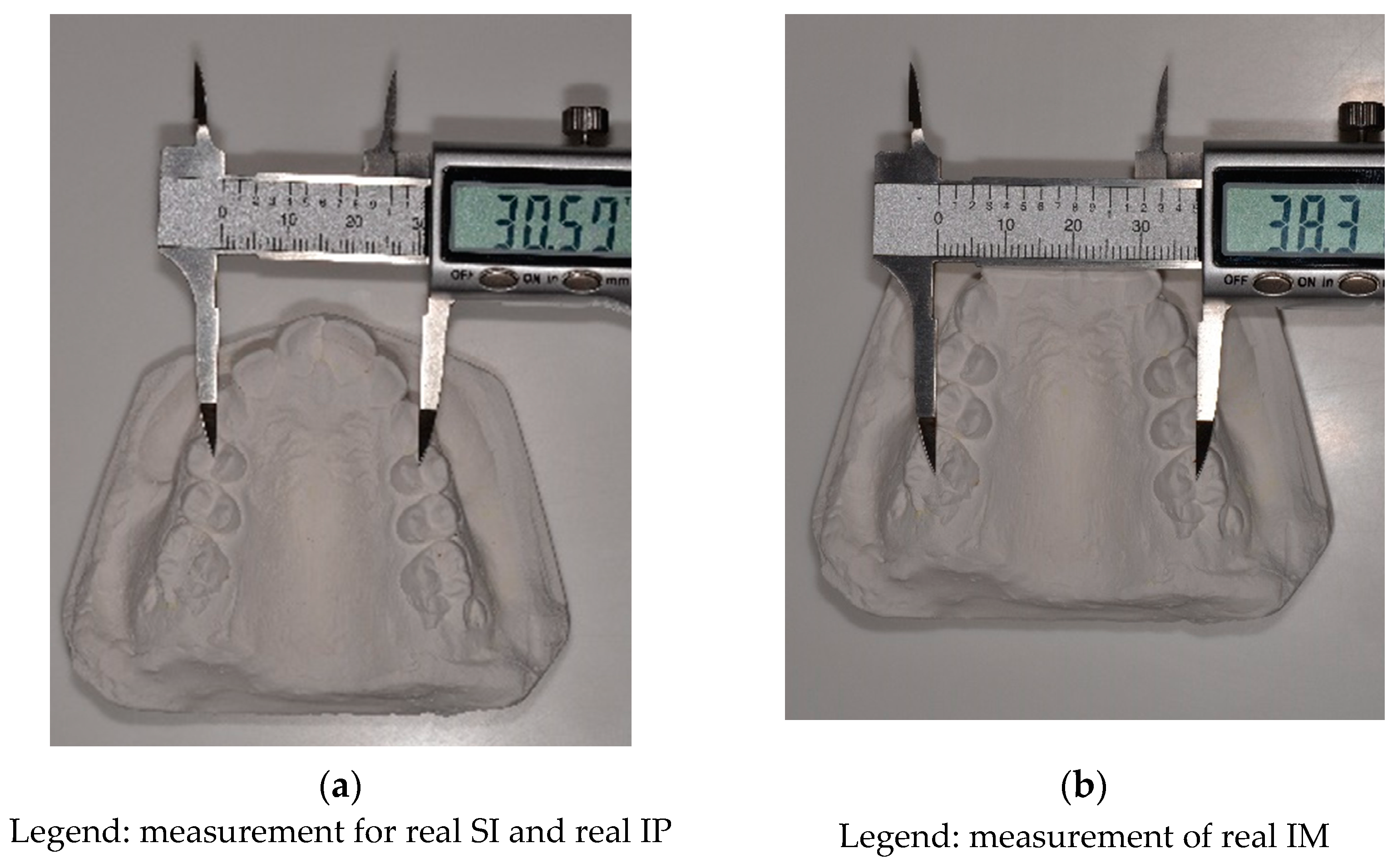
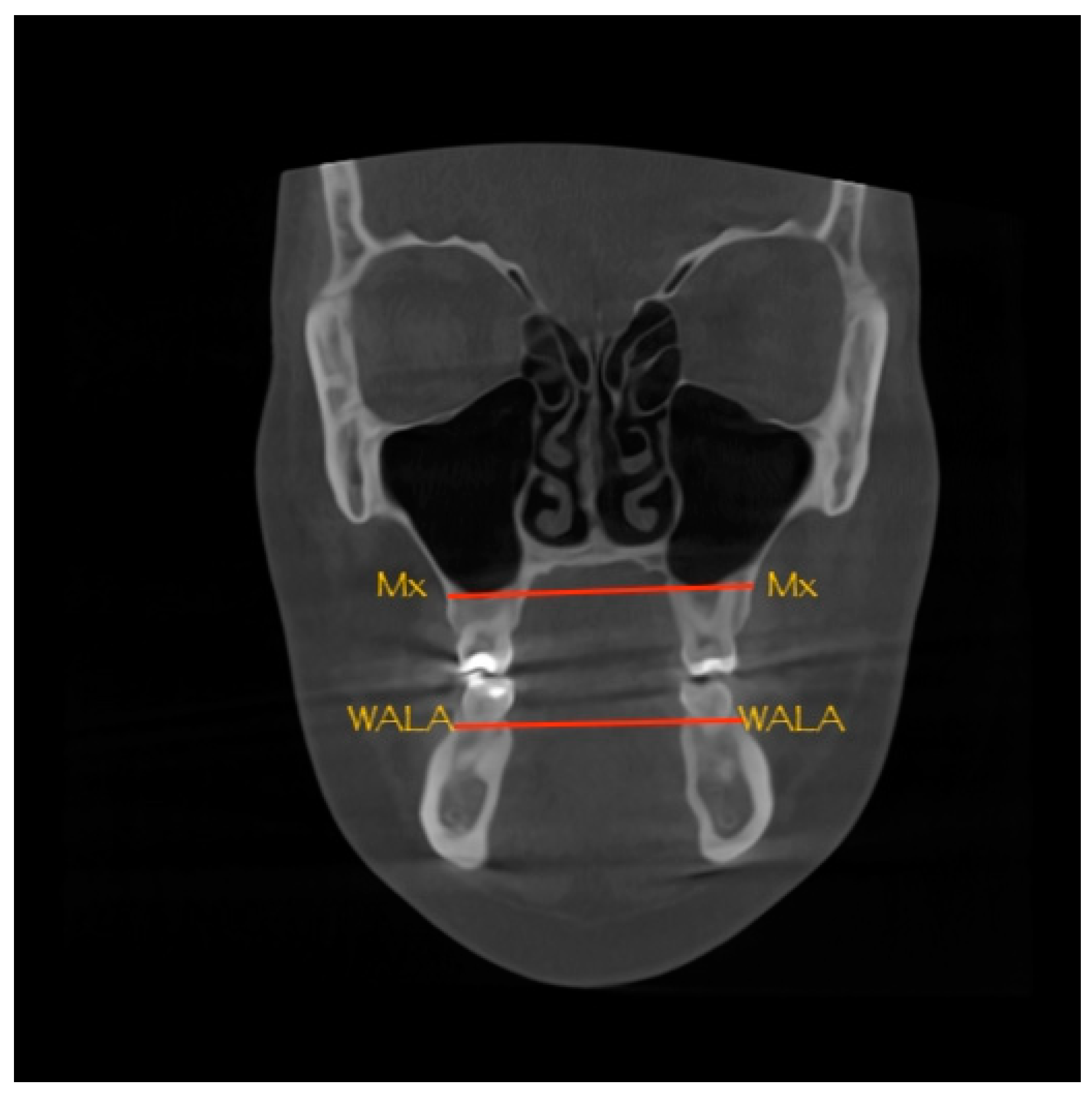
2. Materials and Methods
Statistical Analysis
3. Results
- ⚬
- When UPCBCT analysis indicates MTD and PI indicates MTD in the premolar region (IP);
- ⚬
- When UPCBCT analysis indicates MTD and PI indicates MTD in the molar region (IM);
- ⚬
- When UPCBCT analysis indicates MTD and PI indicates MTD both in the premolar (IP) and molar (IM) regions.
4. Discussions
5. Conclusions
- There was no statistically significant difference between the two diagnostic methods as the null hypothesis was accepted.
- Since CBCT is not a daily used investigation and PI has a relatively high sensitivity (69%), PI is suitable to detect MTD. However, assessment of MTD on CBCT can be recommended for cases where the midpalatal suture maturation should also be evaluated.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Ca se Number | CBCT I mAge Quality Infor mAtion |
|---|---|
| 1 | Ø20.2 × 20.2 cm (504 × 504 × 504) 400 μm 90 KV 12 mA 4.678 s |
| 2 | Ø20.3 × 20.3 cm (507 × 507 × 507) 400 μm 90 KV 12 mA 13.746 s |
| 3 | Ø20.2 × 20.2 cm (504 × 504 × 504) 400 μm 88 KV 11 mA 4.716 s |
| 4 | Ø20.1 × 20.1 cm (503 × 503 × 503) 400 μm 85 KV 8 mA 4.73 s |
| 5 | Ø20.0 × 20.0 cm (501 × 501 × 501) 400 μm 90 KV 12 mA 13.857 s |
| 6 | Ø20.1 × 20.1 cm (503 × 503 × 503) 400 μm 84 KV 10 mA 13.764 s |
| 7 | Ø20.1 × 20.1 cm (502 × 502 × 502) 400 μm 88 KV 6 mA 4.701 s |
| 8 | Ø20.0 × 20.0 cm (500 × 500 × 500) 400 μm 87 KV 12 mA 4.675 s |
| 9 | Ø20.1 × 20.1 cm (502 × 502 × 502) 400 μm 88 KV 10 mA 4.747 s |
| 10 | Ø20.1 × 20.1 cm (502 × 502 × 502) 400 μm 90 KV 8 mA 13.865 s |
| 11 | Ø20.2 × 20.2 cm (504 × 504 × 504) 400 μm 88 KV 11 mA 4.72 s |
| 12 | Ø10.0 × 10.0 cm (250 × 250 × 250) 400 μm 90 KV 7 mA 4.074 s 256.0mGyxcm2 |
| 13 | Ø20.0 × 20.0 cm (500 × 500 × 500) 400 μm 82 KV 8 mA 13.55 s |
| 14 | Ø20.2 × 20.2 cm (504 × 504 × 504) 400 μm 88 KV 9 mA 13.8 s |
| 15 | Ø20.1 × 20.1 cm (502 × 502 × 502) 400 μm 86 KV 8 mA 4.5 s |
| 16 | Ø16.0 × 16.0 cm (800 × 800 × 800) 200 μm 99 KV 8 mA 9.0 s 1610.0mGyxcm2 |
| 17 | Ø20.2 × 20.2 cm (504 × 504 × 504) 400 μm 86 KV 11 mA 4.691 s |
| 18 | Ø20.1 × 20.1 cm (502 × 502 × 502) 400 μm 89 KV 11 mA 13.435 s |
| 19 | Ø20.0 × 20.0 cm (501 × 501 × 501) 400 μm 80 KV 11 mA 4.699 s |
| 20 | Ø20.2 × 20.2 cm (504 × 504 × 504) 400 μm 88 KV 11 mA 4.72 s |
| 21 | Ø20.1 × 20.1 cm (503 × 503 × 503) 400 μm 84 KV 9 mA 6.4 s |
| 22 | Ø20.1 × 20.1 cm (502 × 502 × 502) 400 μm 90 KV 10 mA 4.875 s |
| 23 | Ø20.0 × 20.0 cm (500 × 500 × 500) 400 μm 85 KV 11 mA 4.575 s |
| 24 | Ø20.2 × 20.2 cm (504 × 504 × 504) 400 μm 90 KV 10 mA 11.8 s |
| 25 | Ø20.1 × 20.1 cm (503 × 503 × 503) 400 μm 85 KV 10 mA 7.4 s |
| 26 | Ø20.1 × 20.1 cm (502 × 502 × 502) 400 μm 88 KV 11 mA 13.747 s |
| 27 | Ø20.3 × 20.3 cm (507 × 507 × 507) 400 μm 90 KV 12 mA 12.646 s |
| 28 | Ø20.1 × 20.1 cm (502 × 502 × 502) 400 μm 88 KV 7 mA 5.701 s |
| 29 | Ø20.0 × 20.0 cm (500 × 500 × 500) 400 μm 88 KV 9 mA 13.675 s |
| 30 | Ø20.0 × 20.0 cm (501 × 501 × 501) 400 μm 89 KV 11 mA 9.457 s |
| 31 | Ø20.1 × 20.1 cm (502 × 502 × 502) 400 μm 87 KV 8 mA 9.701 s |
| 32 | Ø20.2 × 20.2 cm (504 × 504 × 504) 400 μm 87 KV 10 mA 9.8 s |
| 33 | Ø20.0 × 20.0 cm (501 × 501 × 501) 400 μm 87 KV 9 mA 8.457 s |
| 34 | Ø20.1 × 20.1 cm (503 × 503 × 503) 400 μm 88 KV 11 mA 9.4 s |
| 35 | Ø20.1 × 20.1 cm (502 × 502 × 502) 400 μm 87 KV 9 mA 4.8476 s |
| 36 | Ø20.3 × 20.3 cm (507 × 507 × 507) 400 μm 90 KV 12 mA 11.896 s |
| 37 | Ø20.2 × 20.2 cm (504 × 504 × 504) 400 μm 88 KV 10 mA 7.886 s |
| 38 | Ø20.1 × 20.1 cm (502 × 502 × 502) 400 μm 89 KV 9 mA 7.788 s |
| 39 | Ø20.0 × 20.0 cm (500 × 500 × 500) 400 μm 90 KV 11 mA 4.745 s |
| 40 | Ø20.0 × 20.0 cm (501 × 501 × 501) 400 μm 88 KV 10 mA 7.885 s |
| 41 | Ø20.1 × 20.1 cm (503 × 503 × 503) 400 μm 86 KV 9 mA 9.55 s |
| 42 | Ø20.1 × 20.1 cm (502 × 502 × 502) 400 μm 87 KV 8 mA 5.767 s |
| 43 | Ø20.2 × 20.2 cm (504 × 504 × 504) 400 μm 87 KV 9 mA 6.89 s |
| 44 | Ø20.1 × 20.1 cm (502 × 502 × 502) 400 μm 88 KV 11 mA 13.47 s |
| 45 | Ø20.1 × 20.1 cm (502 × 502 × 502) 400 μm 90 KV 10 mA 8.387 s |
| 46 | Ø20.0 × 20.0 cm (501 × 501 × 501) 400 μm 89 KV 12 mA 13.765 s |
| 47 | Ø20.0 × 20.0 cm (501 × 501 × 501) 400 μm 90 KV 11 mA 4.885 s |
| 48 | Ø20.1 × 20.1 cm (503 × 503 × 503) 400 μm 85 KV 10 mA 7.4 s |
| 49 | Ø20.1 × 20.1 cm (502 × 502 × 502) 400 μm 90 KV 9 mA 8.797 s |
| 50 | Ø20.1 × 20.1 cm (502 × 502 × 502) 400 μm 90 KV 10 mA 6.747 s |
| 51 | Ø20.1 × 20.1 cm (502 × 502 × 502) 400 μm 88 KV 10 mA 4.887 s |
| 52 | Ø20.1 × 20.1 cm (503 × 503 × 503) 400 μm 84 KV 10 mA 5.34 s |
| 53 | Ø10.0 × 10.0 cm (250 × 250 × 250) 400 μm 89 KV 8 mA 5.066 s |
| 54 | Ø20.0 × 20.0 cm (500 × 500 × 500) 400 μm 87 KV 9 mA 4.545 s |
| 55 | Ø20.3 × 20.3 cm (507 × 507 × 507) 400 μm 90 KV 11 mA 10.556 s |
| 56 | Ø20.1 × 20.1 cm (502 × 502 × 502) 400 μm 87 KV 6 mA 4.134 s |
| 57 | Ø20.2 × 20.2 cm (504 × 504 × 504) 400 μm 88 KV 9 mA 12.876 s |
| 58 | Ø20.0 × 20.0 cm (501 × 501 × 501) 400 μm 90 KV 12 mA 12.757 s |
| 59 | Ø20.1 × 20.1 cm (502 × 502 × 502) 400 μm 88 KV 11 mA 8.767 s |
| 60 | Ø20.1 × 20.1 cm (502 × 502 × 502) 400 μm 87 KV 8 mA 6.877 s |
References
- Tamburrino, R.K.; Boucher, N.S.; Vanarsdall, R.L.; Secchi, A. The Transverse Dimension: Diagnosis and Relevance to Functional Occlusion. Roth Williams Int. Soc. Orthod. J. 2010, 2, 13–22. [Google Scholar]
- Sawchuka, D.; Curriea, K.; Vich, M.L.; Palomob, J.M.; Flores-Mira, C. Diagnostic methods for assessing maxillary skeletal and dental transverse deficiencies: A systematic review. Korean J. Orthod. 2016, 46, 331–342. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Festila, D.; Enache, M.; Ghergie, L.M. Treatment modalities of skeletal maxillary deficiency: A review. Rom. J. Stomatol. 2018, 64, 172–178. [Google Scholar] [CrossRef]
- Kapila, S.D.; Nervina, J.M. CBCT in orthodontics: Assessment of treatment outcomes and indications for its use. Dentomaxillofacial Radiol. 2015, 44, 20140282. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Proffit, W.R.; Fields, H.W.; Larson, B.E.; Sarver, D.M. Contemporary Orthodontics; Elsevier Inc.: Philadelphia, PA, USA, 2019. [Google Scholar]
- Andrucioli, M.C.D.; Matsumoto, M.A.N. Transverse maxillary deficiency: Treatment alternatives in face of early skeletal maturation. Dent. Press J. Orthod. 2020, 25, 70–79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Joondeph, D.R.; Riedel, R.A.; Moore, A.W. Pont’s index: A clinical evaluation. Angle Orthod. 1970, 40, 112–118. [Google Scholar] [CrossRef] [PubMed]
- McNamara, J.A. Maxillary transverse deficiency. Am. J. Orthod. Dentofac. Orthop. 2000, 117, 567–570. [Google Scholar] [CrossRef] [PubMed]
- Betts, N.J.; Vanarsdall, R.L.; Barber, H.D.; Higgins-Barber, K.; Fonseca, R.J. Diagnosis and treatment of transverse maxillary deficiency. Int. J. Adult Orthod. Orthognath. Surg. 1995, 10, 75–96. [Google Scholar] [PubMed]
- Leonardi, R.; Lo Giudice, A.; Rugeri, M.; Muraglie, S.; Cordasco, G.; Barbato, E. Three-dimensional evaluation on digital casts of maxillary palatal size and morphology in patients with functional posterior crossbite. Eur. J. Orthod. 2018, 40, 556–562. [Google Scholar] [CrossRef] [PubMed]
- González, A.G.; López, A.F.; Fernández, S.T.; Ocampo, A.M.; Valencia, J.E. Sensitivity and specificity of a radiographic, tomographic and digital model analysis for determining transverse discrepancies. Rev. Mex. De Ortod. 2018, 6, 26–32. [Google Scholar]
- Hayes, J. The etiology of malocclusion and the “scientific method”. Orthod. Pract. 2020, 11, 62–65. [Google Scholar]
- Giudice, A.L.; Ronsivalle, V.; Lagravere, M.; Leonardi, R.; Martina, S.; Isola, G. Transverse dentoalveolar response of mandibular arch after rapid maxillary expansion (RME) with tooth-borne and bone-borne appliances. Angle Orthod. 2020, 90, 680–687. [Google Scholar] [CrossRef] [PubMed]
- Baysal, A.; Veli, I.; Ucar, F.I.; Eruz, M.; Ozer, T.; Uysal, T. Changes in mandibular transversal arch dimensions after rapid maxillary expansion procedure assessed through cone-beam computed tomography. Korean J. Orthod. Korean Assoc. Orthod. 2011, 41, 200–210. [Google Scholar] [CrossRef] [Green Version]
- Kathiravan, P.; Khurshead, A.M.; Wei, C.N. Pont’s Index Is Not Exact Science: A Reappraisal. Int. Med. J. 2013, 20, 204–207. [Google Scholar]
- Terrez, Y.C.; Fitzmaurice, O.S.; Tejada, H.E.P. Pont’s index in study models of patients who finished a non-extraction orthodontic treatment at the Orthodontic Clinic of the Postgraduate Studies and Research Division of the National University of Mexico. Rev. Mex. De Ortod. 2013, 1, e7–e12. [Google Scholar] [CrossRef] [Green Version]
- Tamburrino, R.K. Complete Clinical Orthodontics® Orthodontic Treatment Design. Available online: https://www.raffaelespenaortodonzia.it/public/files/page_79/cco-treatment%20design%202018.pdf (accessed on 19 November 2021).
- Free Statistical Calculators. MedCalc. Available online: https://www.medcalc.org/calc/diagnostic_test.php (accessed on 19 November 2021).
- Bowers, D. Medical Statistics from Scratch: An Introduction for Health Professionals, 2nd ed.; John Wiley & Sons Ltd.: West Sussex, UK, 2008; ISBN 978-047-051-301-9. [Google Scholar]
- Hazra, A.; Gogtay, N. Biostatistics series module 7: The statistics of diagnostic tests. Indian J. Dermatol. 2017, 62, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Campbell, M.J.; Freeman, J.V. The University of Sheffield. Available online: https://www.sheffield.ac.uk/polopoly_fs/1.43990!/file/Tutorial-13-diagnostic-tests.pdf (accessed on 19 November 2021).
- Mandrekar, J.N. Simple Statistical Measures for Diagnostic Accuracy Assessment. J. Thorac. Oncol. 2010, 5, 763–764. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meier, K.U.S. Department of Health and Human Services Food and Drug Administration Center for Devices and Radiological Health. Available online: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/statistical-guidance-reporting-results-studies-evaluating-diagnostic-tests-guidance-industry-and-fda (accessed on 19 November 2021).
- Agarwal, A.; Mathur, R. Maxillary Expansion. Int. J. Clin. Pediatric Dent. 2010, 3, 139–146. [Google Scholar] [CrossRef] [PubMed]
- Angelieri, F.; Cevidanes, L.H.; Franchi, L.; Gonçalves, R.; Benavides, E.; McNamara, J.A., Jr. Midpalatal suture maturation: Classification method for individual assessment before rapid maxillary expansion. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 759–769. [Google Scholar] [CrossRef] [Green Version]
- Centre for Reviews and Dissemination, University of York. Available online: https://www.york.ac.uk/media/crd/Systematic_Reviews.pdf (accessed on 19 November 2021).
- Wenge, Z.; Zeng, N.F.; Wang, N. Sensitivity, Specificity, Accuracy, Associated Confidence Interval and ROC Analysis with Practical SAS Implementations. Health Care Life Sci. 2010, 19, 67. [Google Scholar]
- Bossuyt, P.M.; Reitsma, J.B.; Bruns, D.E.; Gatsonis, C.A.; Glasziou, P.P.; Irwig, L.; Lijmer, J.G.; Moher, D.; Rennie, D.; de Vet, H.C.; et al. STARD 2015: An Updated List of Essential Items for Reporting Diagnostic Accuracy Studies. Radiology 2015, 277, 826–832. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agnihotri, G.; Gulati, M. Maxillary molar and premolar indices in North Indians. Internet J. Biol. Anthropol. 2008, 2, 1–5. [Google Scholar]
| Case Number | Pont’s Index | UPCBCT Results (mm) | Results Match * YES(Y)/NO(N) | TP/FP/TN/FN ** | |
|---|---|---|---|---|---|
| Calculated–Measured IP (mm) | Calculated–Measured IM (mm) | ||||
| 1 | −1.9 | 1.75 | −3.4 | Y | TN |
| 2 | 2.9875 | 2.599375 | 0.19 | Y | TP |
| 3 | 2.2175 | 1.296875 | −2.2 | N | FP |
| 4 | 1.58 | 6.93 | 1 | Y | TP |
| 5 | 5.8875 | 4.391875 | 4 | Y | TP |
| 6 | 3.85 | 4.8175 | 0.2 | Y | TP |
| 7 | 3.5025 | 7.698125 | 3.8 | Y | TP |
| 8 | 2.63 | 1.2375 | −3 | N | FP |
| 9 | 4.085 | 6.20625 | 2.19 | Y | TP |
| 10 | 8.3675 | 8.674375 | 2.6 | Y | TP |
| 11 | 5.45 | 4.6225 | 2.4 | Y | TP |
| 12 | 2.99 | 2.485 | 1.8 | Y | TP |
| 13 | −2.63 | 4.84 | −2.2 | N | FP |
| 14 | 4.925 | 9.93375 | 5.4 | Y | TP |
| 15 | 4.8475 | 5.339375 | −4.6 | N | FP |
| 16 | 1.995 | 4.43375 | −0.19 | N | FP |
| 17 | 3.375 | 6.12625 | −3.8 | N | FP |
| 18 | −1.825 | 0.72375 | 0.8 | N | FN |
| 19 | 2.78 | 0.6125 | 1.8 | Y | TP |
| 20 | 2.9325 | 3.050625 | 0.2 | Y | TP |
| 21 | 3.9025 | 4.083125 | 3.8 | Y | TP |
| 22 | −0.82 | −1.56 | −1 | Y | TN |
| 23 | 2.6375 | 2.046875 | 5.4 | Y | TP |
| 24 | −1.0325 | −2.725625 | 12 | N | FN |
| 25 | 3.7125 | 3.270625 | 3.8 | Y | TP |
| 26 | 2.1725 | −0.814375 | 5.1 | Y | TP |
| 27 | 1.62 | 0.6625 | −0.6 | Y | TN |
| 28 | 8.1825 | 12.930625 | 2.6 | Y | TP |
| 29 | 4.7325 | 3.115625 | 5.4 | Y | TP |
| 30 | 2.175 | 0.36125 | −0.3 | N | FP |
| 31 | 6.82 | 5.5125 | 4.6 | Y | TP |
| 32 | 5.965 | 7.65875 | −1 | N | FP |
| 33 | 7.4 | 4.15 | 5 | Y | TP |
| 34 | 3.3875 | 3.984375 | 1.2 | Y | TP |
| 35 | −2.115 | −3.85375 | 4.6 | N | FN |
| 36 | −1.275 | −3.07375 | 5 | N | FN |
| 37 | 0.165 | −7.59125 | 12.6 | N | FN |
| 38 | 1.5275 | 4.664375 | −2 | N | FP |
| 39 | 0.7275 | 0.421875 | 3 | N | FN |
| 40 | 5.2 | 6 | 1.18 | Y | TP |
| 41 | −2.855 | −2.35125 | 2.6 | N | FN |
| 42 | 0.1625 | −2.113125 | 6.6 | N | FN |
| 43 | 1.3025 | −1.206875 | 1.11 | N | FN |
| 44 | 2.6625 | 3.528125 | 1.01 | Y | TP |
| 45 | 4.9025 | 8.370625 | −0.2 | N | FP |
| 46 | 3.2375 | 4.546875 | 3.37 | Y | TP |
| 47 | 3.79 | 3.8925 | −1.8 | N | FP |
| 48 | 0.2925 | 3.190625 | −3 | N | FP |
| 49 | 3.2375 | 8.636875 | −0.19 | N | FP |
| 50 | −0.1725 | −3.213125 | 5.8 | N | FN |
| 51 | 4.875 | 6.42375 | 1.04 | Y | TP |
| 52 | 0.2375 | −1.103125 | 1 | N | FN |
| 53 | −2.97 | −4.3175 | 1.4 | N | FN |
| 54 | 4.025 | 0.58375 | −2.2 | N | FP |
| 55 | 2.7 | 3.565 | 5.8 | Y | TP |
| 56 | 0.64 | 5.3125 | −1.8 | N | FP |
| 57 | 2.495 | 2.80875 | 7.4 | Y | TP |
| 58 | 2.155 | −0.08125 | 4.6 | Y | TP |
| 59 | 1.46 | 2.105 | 1 | Y | TP |
| 60 | 1.2875 | 1.199375 | 8.2 | N | FN |
| Pont’s Analysis Compared to Penn CBCT | Gold Standard | ||
|---|---|---|---|
| Diagnostic test | CBCT Positive | CBCT Negative | Total |
| Pont Positive | True positive 29 | False positive 15 | 44 |
| Pont Negative | False negative 13 | True negative 3 | 16 |
| Total | 42 | 18 | 60 |
| Accuracy Indicator | Value | Upper and Lower Limits (Confidence Interval: 95%) |
|---|---|---|
| Sensitivity | 69% | 52.91–82.38% |
| Specificity | 16.6% | 3.58–41.42% |
| PPV | 65% | 59.14–72.08% |
| NPV | 18.75% | 6.95–41.61% |
| LR+ | 0.83 | 0.62–1.11% |
| LR− | 1.86 | 0.6–5.73% |
| Accuracy | 53.28% | 40–66.33% |
| Case Number | Pont’s Index | Penn CBCT | Pretest-Posttest |
| 1 | 0 | 0 | 0 |
| 2 | 1 | 1 | 0 |
| 3 | 1 | 0 | 1 |
| 4 | 1 | 1 | 0 |
| 5 | 1 | 1 | 0 |
| 6 | 1 | 1 | 0 |
| 7 | 1 | 1 | 0 |
| 8 | 1 | 0 | 1 |
| 9 | 1 | 1 | 0 |
| 10 | 1 | 1 | 0 |
| 11 | 1 | 1 | 0 |
| 12 | 1 | 1 | 0 |
| 13 | 1 | 0 | 1 |
| 14 | 1 | 1 | 0 |
| 15 | 1 | 0 | 1 |
| 16 | 1 | 0 | 1 |
| 17 | 1 | 0 | 1 |
| 18 | 0 | 1 | −1 |
| 19 | 1 | 1 | 0 |
| 20 | 1 | 1 | 0 |
| 21 | 1 | 1 | 0 |
| 22 | 0 | 0 | 0 |
| 23 | 1 | 1 | 0 |
| 24 | 0 | 1 | −1 |
| 25 | 1 | 1 | 0 |
| 26 | 1 | 1 | 0 |
| 27 | 0 | 0 | 0 |
| 28 | 1 | 1 | 0 |
| 29 | 1 | 1 | 0 |
| 30 | 1 | 0 | 1 |
| 31 | 1 | 1 | 0 |
| 32 | 1 | 0 | 1 |
| 33 | 1 | 1 | 0 |
| 34 | 1 | 1 | 0 |
| 35 | 0 | 1 | −1 |
| 36 | 0 | 1 | −1 |
| 37 | 0 | 1 | −1 |
| 38 | 1 | 0 | 1 |
| 39 | 0 | 1 | −1 |
| 40 | 1 | 1 | 0 |
| 41 | 0 | 1 | −1 |
| 42 | 0 | 1 | −1 |
| 43 | 0 | 1 | −1 |
| 44 | 1 | 1 | 0 |
| 45 | 1 | 0 | 1 |
| 46 | 1 | 1 | 0 |
| 47 | 1 | 0 | 1 |
| 48 | 1 | 0 | 1 |
| 49 | 1 | 0 | 1 |
| 50 | 0 | 1 | −1 |
| 51 | 1 | 1 | 0 |
| 52 | 0 | 1 | −1 |
| 53 | 0 | 1 | −1 |
| 54 | 1 | 0 | 1 |
| 55 | 1 | 1 | 0 |
| 56 | 1 | 0 | 1 |
| 57 | 1 | 1 | 0 |
| 58 | 1 | 1 | 0 |
| 59 | 1 | 1 | 0 |
| 60 | 0 | 1 | −1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Feştilă, D.; Enache, A.M.; Nagy, E.B.; Hedeşiu, M.; Ghergie, M. Testing the Accuracy of Pont’s Index in Diagnosing Maxillary Transverse Discrepancy as Compared to the University of Pennsylvania CBCT Analysis. Dent. J. 2022, 10, 23. https://doi.org/10.3390/dj10020023
Feştilă D, Enache AM, Nagy EB, Hedeşiu M, Ghergie M. Testing the Accuracy of Pont’s Index in Diagnosing Maxillary Transverse Discrepancy as Compared to the University of Pennsylvania CBCT Analysis. Dentistry Journal. 2022; 10(2):23. https://doi.org/10.3390/dj10020023
Chicago/Turabian StyleFeştilă, Dana, Aurelia Magdalena Enache, Evelyn Beatrix Nagy, Mihaela Hedeşiu, and Mircea Ghergie. 2022. "Testing the Accuracy of Pont’s Index in Diagnosing Maxillary Transverse Discrepancy as Compared to the University of Pennsylvania CBCT Analysis" Dentistry Journal 10, no. 2: 23. https://doi.org/10.3390/dj10020023
APA StyleFeştilă, D., Enache, A. M., Nagy, E. B., Hedeşiu, M., & Ghergie, M. (2022). Testing the Accuracy of Pont’s Index in Diagnosing Maxillary Transverse Discrepancy as Compared to the University of Pennsylvania CBCT Analysis. Dentistry Journal, 10(2), 23. https://doi.org/10.3390/dj10020023






