Fit, Precision, and Trueness of 3D-Printed Zirconia Crowns Compared to Milled Counterparts
Abstract
1. Introduction
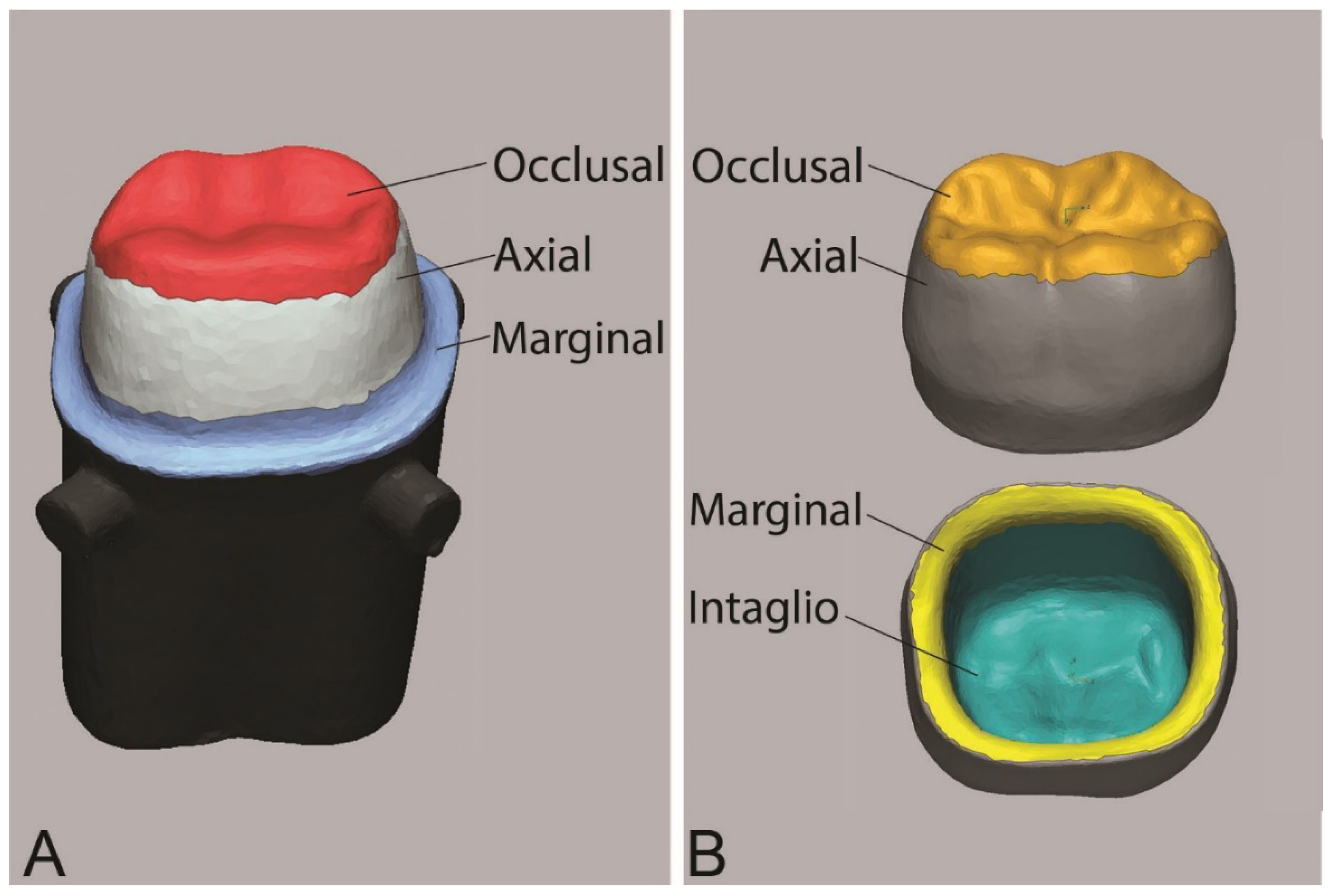
2. Materials and Methods
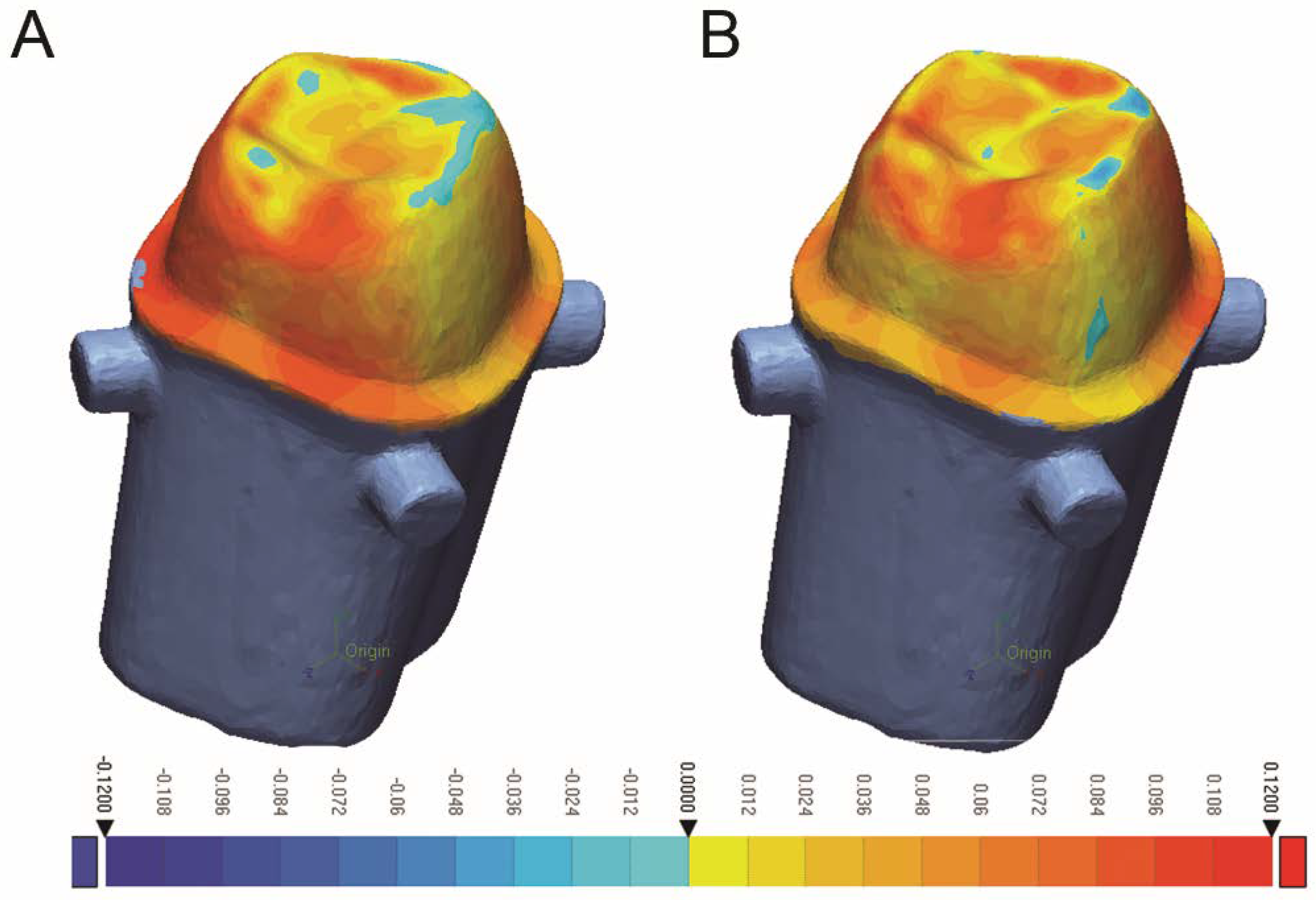
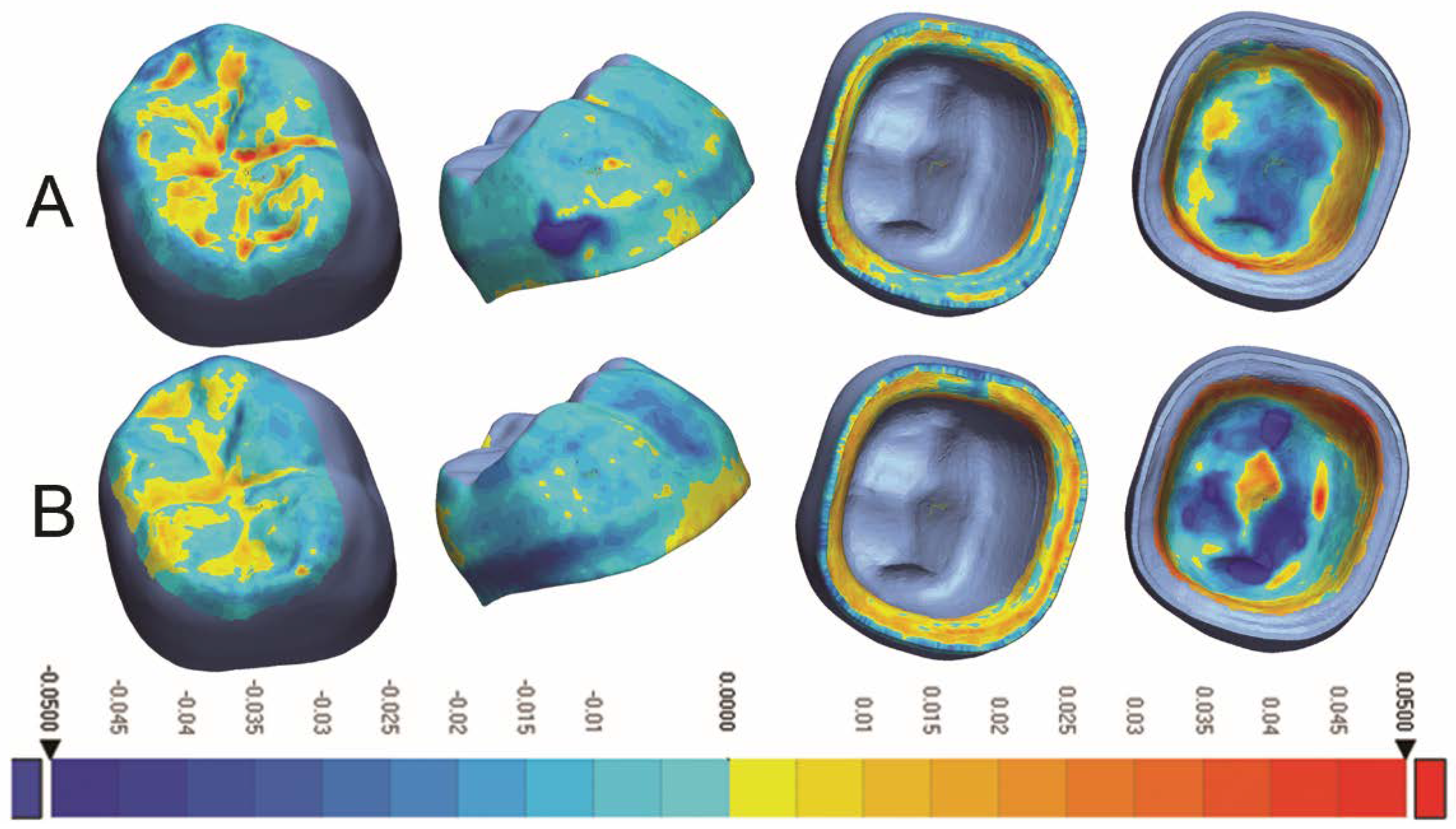
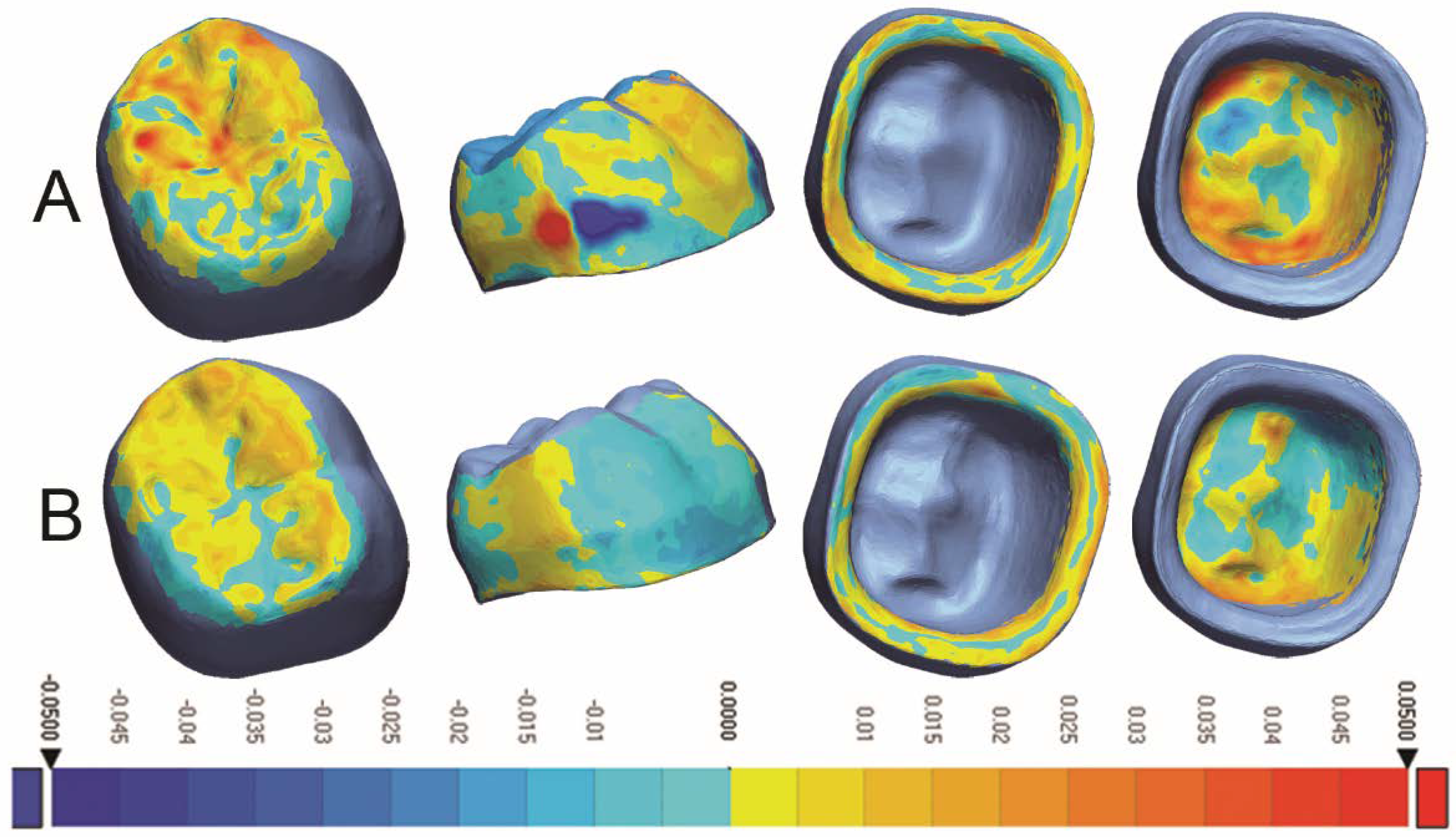
3. Results
4. Discussion
5. Conclusions
- Additive and subtractive manufacturing techniques produced zirconia crowns with comparable internal fit and marginal adaptation.
- The 3D-printed crowns had better occlusal and axial trueness, while milled crowns showed better intaglio trueness.
- 3D printing produced more precise restorations than milling.
- Further in vitro and in vivo studies are needed to evaluate other aspects of 3D-printed zirconia crowns, such as mechanical and optical properties.
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Mazza, L.C.; Lemos, C.; Pesqueira, A.A.; Pellizzer, E.P. Survival and complications of monolithic ceramic for tooth-supported fixed dental prostheses: A systematic review and meta-analysis. J. Prosthet. Dent. 2022, 128, 566–574. [Google Scholar] [CrossRef] [PubMed]
- Cagidiaco, E.F.; Discepoli, N.; Goracci, C.; Carboncini, F.; Vigolo, P.; Ferrari, M. Randomized clinical trial on single zirconia crowns with feather-edge vs chamfer finish lines: Four-year results. Int. J. Periodontics Restor. Dent. 2019, 39, 817–826. [Google Scholar] [CrossRef] [PubMed]
- Mühlemann, S.; Lakha, T.; Jung, R.E.; Hämmerle, C.H.; Benic, G.I. Prosthetic outcomes and clinical performance of CAD-CAM monolithic zirconia versus porcelain-fused-to-metal implant crowns in the molar region: 1-year results of a RCT. Clin. Oral. Implant. Res. 2020, 31, 856–864. [Google Scholar] [CrossRef] [PubMed]
- Mangano, F.; Veronesi, G. Digital versus analog procedures for the prosthetic restoration of single implants: A randomized controlled trial with 1 year of follow-up. BioMed Res. Int. 2018, 18, 5325032. [Google Scholar] [CrossRef] [PubMed]
- Kraus, R.D.; Epprecht, A.; Hämmerle, C.H.; Sailer, I.; Thoma, D.S. Cemented vs screw-retained zirconia-based single implant reconstructions: A 3-year prospective randomized controlled clinical trial. Clin. Implant. Dent. Relat. Res. 2019, 21, 578–585. [Google Scholar] [CrossRef]
- Tabesh, M.; Nejatidanesh, F.; Savabi, G.; Davoudi, A.; Savabi, O.; Mirmohammadi, H. Marginal adaptation of zirconia complete-coverage fixed dental restorations made from digital scans or conventional impressions: A systematic review and meta-analysis. J. Prosthet. Dent. 2021, 125, 603–610. [Google Scholar] [CrossRef]
- Abdulmajeed, A.A.; Lim, K.G.; Närhi, T.O.; Cooper, L.F. Complete-arch implant-supported monolithic zirconia fixed dental prostheses: A systematic review. J. Prosthet. Dent. 2016, 115, 672–677. [Google Scholar] [CrossRef]
- Laumbacher, H.; Strasser, T.; Knütte, H.; Rosentritt, M. Long-term clinical performance and complications of zirconia-based tooth- and implant-supported fixed prosthodontic restorations: A summary of systematic reviews. J. Dent. 2021, 111, 103723. [Google Scholar] [CrossRef]
- Wang, W.; Yu, H.; Liu, Y.; Jiang, X.; Gao, B. Trueness analysis of zirconia crowns fabricated with 3-dimensional printing. J. Prosthet. Dent. 2019, 121, 285–291. [Google Scholar] [CrossRef]
- Guess, P.; Att, W.; Strub, J. Zirconia in fixed implant prosthodontics. Clin. Implant. Dent. Relat. Res. 2012, 14, 633–645. [Google Scholar] [CrossRef]
- Komine, F.; Blatz, M.; Matsumura, H. Current status of zirconia-based fixed restorations. J. Oral. Sci. 2010, 52, 531–539. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Li, L.; Chen, M.; Davim, J. An experimental investigation on milling features of fully-sintered zirconia ceramics using PCD tools. Mater. Manuf. Process 2022, 37, 318–326. [Google Scholar] [CrossRef]
- Saridag, S.; Tak, O.; Alniacik, G. Basic properties and types of zirconia: An overview. World J. Stomatol. 2013, 2, 40–47. [Google Scholar] [CrossRef]
- Miyazaki, T.; Nakamura, T.; Matsumura, H.; Ban, S.; Kobayashi, T. Current status of zirconia restoration. J. Prosthodont. Res. 2013, 57, 236–261. [Google Scholar] [CrossRef] [PubMed]
- Lerner, H.; Nagy, K.; Pranno, N.; Zarone, F.; Admakin, O.; Mangano, F. Trueness and precision of 3D-printed versus milled monolithic zirconia crowns: An in vitro study. J. Dent. 2021, 113, 10379. [Google Scholar] [CrossRef]
- Osman, R.; van der Veen, A.J.; Huiberts, D.; Wismeijer, D.; Alharbi, N. 3D-printing zirconia implants; a dream or a reality? An in-vitro study evaluating the dimensional accuracy, surface topography and mechanical properties of printed zirconia implant and discs. J. Mech. Behav. Biomed. Mater. 2017, 75, 521–528. [Google Scholar] [CrossRef] [PubMed]
- Methani, M.M.; Revilla-Leon, M.; Zandinejad, A. The potential of additive manufacturing technologies and their processing parameters for the fabrication of all-ceramic crowns: A review. J. Esthet. Restor. Dent. 2020, 32, 182–192. [Google Scholar] [CrossRef]
- Nakai, H.; Inokoshi, M.; Nozaki, K.; Komatsu, K.; Kamijo, S.; Liu, H.; Shimizubata, M.; Minakuchi, S.; Van Meerbeek, B.; Vleugels, J.; et al. Additively manufactured zirconia for dental applications. Materials 2021, 14, 3694. [Google Scholar] [CrossRef]
- Quan, H.; Zhang, T.; Xu, H.; Luo, S.; Nie, J.; Zhu, X. Photo-curing 3D printing technique and its challenges. Bioact. Mater. 2020, 5, 110–115. [Google Scholar] [CrossRef]
- Revilla-León, M.; Methani, M.M.; Morton, D.; Zandinejad, A. Internal and marginal discrepancies associated with stereolithography (SLA) additively manufactured zirconia crowns. J. Prosthet. Dent. 2020, 124, 730–737. [Google Scholar] [CrossRef]
- Valenti, C.; Isabella Federici, M.; Masciotti, F.; Marinucci, L.; Xhimitiku, I.; Cianetti, S.; Pagano, S. Mechanical properties of 3D-printed prosthetic materials compared with milled and conventional processing: A systematic review and meta-analysis of in vitro studies. J. Prosthet. Dent. 2022; Online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Larson, T.D. The clinical significance of marginal fit. Northwest Dent. 2012, 91, 22–29. [Google Scholar] [PubMed]
- Holmes, J.R.; Bayne, S.C.; Holland, G.A.; Sulik, W.D. Considerations in measurement of marginal fit. J. Prosthet. Dent. 1989, 62, 405–408. [Google Scholar] [CrossRef]
- Hasanzade, M.; Aminikhak, M.; Afrashtehfar, K.; Alikhasi, M. Marginal and internal adaptation of single crowns and fixed dental prostheses by using digital and conventional workflows: A systematic review and meta-analysis. J. Prosthet. Dent. 2021, 126, 360–368. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, M.S.; Windeler, A.S. An investigation of dental luting cement solubility as a function of the marginal gap. J. Prosthet. Dent. 1991, 65, 436–442. [Google Scholar] [CrossRef]
- Felton, D.A.; Kanoy, B.E.; Bayne, S.C.; Wirthman, G.P. Effect of in vivo crown margin discrepancies on periodontal health. J. Prosthet. Dent. 1991, 65, 357–364. [Google Scholar] [CrossRef]
- Contrepois, M.; Soenen, A.; Bartala, M.; Laviole, O. Marginal adaptation of ceramic crowns: A systematic review. J. Prosthet. Dent. 2013, 110, 447–454. [Google Scholar] [CrossRef]
- McLean, J.W.; von Fraunhofer, J.A. The estimation of cement film thickness by an in vivo technique. Br. Dent. J. 1971, 131, 107–111. [Google Scholar] [CrossRef]
- Son, K.; Lee, S.; Kang, S.H.; Park, J.; Lee, K.B.; Jeon, M.; Yun, B.J. A comparison study of marginal and internal fit assessment methods for fixed dental prostheses. J. Clin. Med. 2019, 8, 785. [Google Scholar] [CrossRef]
- Cetik, S.; Bahrami, B.; Fossoyeux, I.; Atash, R. Adaptation of zirconia crowns created by conventional versus optical impression: In vitro study. J. Adv. Prosthodont. 2017, 9, 208–216. [Google Scholar] [CrossRef]
- Park, J.Y.; Bae, S.Y.; Lee, J.J.; Kim, J.H.; Kim, H.Y.; Kim, W.C. Evaluation of the marginal and internal gaps of three different dental prostheses: Comparison of the silicone replica technique and three-dimensional superimposition analysis. J. Adv. Prosthodont. 2017, 9, 159–169. [Google Scholar] [CrossRef] [PubMed]
- Al Hamad, K.Q.; Al-Rashdan, R.B.; Al-Rashdan, B.A.; Baba, N.Z. Effect of milling protocols on trueness and precision of ceramic crowns. J. Prosthodont. 2021, 30, 171–176. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.M.; Kim, J.H.; Kim, H.Y.; Kim, W.C. Trueness of milled prostheses according to number of ball-end mill burs. J. Prosthet. Dent. 2016, 115, 624–629. [Google Scholar] [CrossRef] [PubMed]
- Kirsch, C.; Ender, A.; Attin, T.; Mehl, A. Trueness of four different milling procedures used in dental CAD/CAM systems. Clin. Oral. Investig. 2017, 21, 551–558. [Google Scholar] [CrossRef] [PubMed]
- Bosch, G.; Ender, A.; Mehl, A. A 3-dimensional accuracy analysis of chairside CAD/CAM milling processes. J. Prosthet. Dent. 2014, 112, 1425–1431. [Google Scholar] [CrossRef]
- Cho, J.H.; Yoon, H.I.; Han, J.S.; Kim, D.J. Trueness of the inner surface of monolithic crowns fabricated by milling of a fully sintered (Y, Nb)-TZP block in chairside CAD–CAM system for single-visit dentistry. Materials 2019, 12, 3253. [Google Scholar] [CrossRef]
- Wang, W.; Sun, J. Dimensional accuracy and clinical adaptation of ceramic crowns fabricated with the stereolithography technique. J. Prosthet. Dent. 2021, 125, 657–663. [Google Scholar] [CrossRef]
- ISO 12836:2015; Digitizing Devices for CAD/CAM Systems for Indirect Dental Restorations—Test Methods for Assessing Accuracy. International Organization for Standardization: Geneve, Switzerland, 2015.
- Lim, J.H.; Mangal, U.; Nam, N.E.; Choi, S.H.; Shim, J.S.; Kim, J.E. A comparison of accuracy of different dental restorative materials between intraoral scanning and conventional impression-taking: An in vitro study. Materials 2021, 14, 2060. [Google Scholar] [CrossRef]
- Ahmed, W.M.; Shariati, B.; Gazzaz, A.; Sayed, M.E.; Carvalho, R.M. Fit of tooth-supported zirconia single crowns—A systematic review of the literature. Clin. Exp. Dent. Res. 2020, 6, 700–716. [Google Scholar] [CrossRef]
- Rau, S.A.; Raedel, M.; Mikeli, A.; Raedel, M.; Walter, M.H. Clinical fit of monolithic zirconia single crowns. Int. J. Prosthodont. 2018, 31, 443–445. [Google Scholar] [CrossRef]
- Sakornwimon, N.; Leevailoj, C. Clinical marginal fit of zirconia crowns and patients’ preferences for impression techniques using intraoral digital scanner versus polyvinyl siloxane material. J. Prosthet. Dent. 2017, 118, 386–391. [Google Scholar] [CrossRef] [PubMed]
- Kokubo, Y.; Tsumita, M.; Kano, T.; Sakurai, S.; Fukushima, S. Clinical marginal and internal gaps of zirconia all-ceramic crowns. J. Prosthodont. Res. 2011, 55, 40–43. [Google Scholar] [CrossRef] [PubMed]
- Freire, Y.; Gonzalo, E.; Lopez-Suarez, C.; Pelaez, J.; Suarez, M.J. Evaluation of the marginal fit of monolithic crowns fabricated by direct and indirect digitization. J. Prosthodont. Res. 2021, 65, 291–297. [Google Scholar] [CrossRef] [PubMed]
- Kale, E.; Yilmaz, B.; Seker, E.; Özcelik, T.B. Effect of fabrication stages and cementation on the marginal fit of CAD-CAM monolithic zirconia crowns. J. Prosthet. Dent. 2017, 118, 736–741. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, W.M.; Abdallah, M.N.; McCullagh, A.P.; Wyatt, C.C.; Troczynski, T.; Carvalho, R.M. Marginal discrepancies of monolithic zirconia crowns: The influence of preparation designs and sintering techniques. J. Prosthodont. 2019, 28, 288–298. [Google Scholar] [CrossRef] [PubMed]
- Revilla-León, M.; Meyer, M.J.; Zandinejad, A.; Özcan, M. Additive manufacturing technologies for processing zirconia in dental applications. Int. J. Comput. Dent. 2020, 23, 27–37. [Google Scholar] [PubMed]
- Galante, R.; Figueiredo-Pina, C.G.; Serro, A.P. Additive manufacturing of ceramics for dental applications: A review. Dent. Mater. 2019, 35, 825–846. [Google Scholar] [CrossRef]
- Schweiger, J.; Edelhoff, D.; Güth, J.F. 3D printing in digital prosthetic dentistry: An overview of recent developments in additive manufacturing. J. Clin. Med. 2021, 10, 2010. [Google Scholar] [CrossRef]
- Marsico, C.; Øilo, M.; Kutsch, J.; Kauf, M.; Arola, D. Vat polymerization-printed partially stabilized zirconia: Mechanical properties, reliability and structural defects. Addit. Manuf. 2020, 36, 101450. [Google Scholar] [CrossRef]
- Revilla-León, M.; Al-Haj Husain, N.; Ceballos, L.; Özcan, M. Flexural strength and Weibull characteristics of stereolithography additive manufactured versus milled zirconia. J. Prosthet. Dent. 2021, 125, 685–690. [Google Scholar] [CrossRef]
- Zandinejad, A.; Methani, M.M.; Schneiderman, E.D.; Revilla-León, M.; Morton, D. Fracture resistance of additively manufactured zirconia crowns when cemented to implant supported zirconia abutments: An in vitro study. J. Prosthodont. 2019, 28, 893–897. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Wang, Y.; Hu, M.; Wang, Y.; Xv, Y.; Liu, Y.; Sun, Y. Strength and adaptation of stereolithography-fabricated zirconia dental crowns: An in vitro study. Int. J. Prosthodont. 2019, 32, 439–443. [Google Scholar] [CrossRef] [PubMed]
- Ren, S.; Jiang, X.; Lin, Y.; Di, P. Crown accuracy and time efficiency of cement-retained implant-supported restorations in a complete digital workflow: A randomized control trial. J. Prosthodont. 2022, 31, 405–411. [Google Scholar] [CrossRef]
- Kim, Y.K.; Han, J.S.; Yoon, H.I. Evaluation of intaglio surface trueness, wear, and fracture resistance of zirconia crown under simulated mastication: A comparative analysis between subtractive and additive manufacturing. J. Adv. Prosthodont. 2022, 14, 122–132. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Xu, T.; Wang, Y.; Sun, Y. Accuracy of zirconia crowns manufactured by stereolithography with an occlusal full-supporting structure: An in vitro study. J. Prosthet. Dent. 2022, S0022–3913, 00064–00066, Online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Schönherr, J.; Baumgartner, S.; Hartmann, M.; Stampfl, J. Stereolithographic additive manufacturing of high precision glass ceramic parts. Materials 2020, 13, 1492. [Google Scholar] [CrossRef]
- Payaminia, L.; Moslemian, N.; Younespour, S.; Koulivand, S.; Alikhasi, M. Evaluating the effect of repeated use of milling burs on surface roughness and adaptation of digitally fabricated ceramic veneers. Heliyon 2021, 7, e06896. [Google Scholar] [CrossRef]
- Baldi, A.; Comba, A.; Ferrero, G.; Italia, E.; Michelotto Tempesta, R.; Paolone, G.; Mazzoni, A.; Breschi, L.; Scotti, N. External gap progression after cyclic fatigue of adhesive overlays and crowns made with high translucency zirconia or lithium silicate. J. Esthet. Restor. Dent. 2022, 34, 557–564. [Google Scholar] [CrossRef]
| Preparation Feature | Amount | Crown Parameters | Amount |
|---|---|---|---|
| Anatomic occlusal reduction | 1.5–2.0 mm | Cement gap | 60 µm |
| Axial reduction | 0.8–1.2 mm | Extra cement gap | 40 µm, 1 mm from margin |
| Finish line | 0.8 mm shoulder with rounded internal line angle | Offset angle | 55° |
| Total occlusal convergence | 8–10° | Offset extension | 0.10 mm |
| Measured Area | Milled Mean Gap ± SD | 3D-Printed Mean Gap ± SD | p-Value |
|---|---|---|---|
| Occlusal | 40.20 ± 7.96 | 45.67 ± 4.57 | 0.0756 |
| Axial | 49.23 ± 5.25 | 47.75 ± 3.16 | 0.4545 |
| Marginal | 36.68 ± 6.04 | 38.26 ± 4.87 | 0.5277 |
| Overall | 44.63 ± 6.24 | 46.67 ± 2.80 | 0.3581 |
| Measured Area | Milled RMS ± SD | 3D-Printed RMS ± SD | p-Value |
|---|---|---|---|
| Occlusal | 14.78 ± 2.23 | 8.77 ± 0.89 | <0.0001 * |
| Axial | 20.37 ± 4.49 | 14.77 ± 2.03 | 0.0021 * |
| Marginal | 16.24 ± 4.62 | 16.35 ± 0.84 | 0.9417 |
| Intaglio | 20.29 ± 3.82 | 23.90 ± 1.60 | 0.0130 * |
| Overall | 18.58 ± 3.03 | 17.00 ± 0.95 | 0.1329 |
| Measured Area | (Milled) RMS ± SD | (3D-Printed) RMS ± SD | p-Value |
|---|---|---|---|
| Occlusal | 13.30 ± 2.46 | 7.82 ± 1.06 | <0.0001 * |
| Axial | 20.76 ± 5.62 | 9.60 ± 1.84 | <0.0001 * |
| Marginal | 16.84 ± 3.94 | 9.73 ± 0.92 | <0.0001 * |
| Intaglio | 15.72 ± 2.96 | 10.68 ± 1.22 | 0.0002 * |
| Overall | 17.31 ± 3.39 | 9.59 ± 0.75 | <0.0001 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abualsaud, R.; Alalawi, H. Fit, Precision, and Trueness of 3D-Printed Zirconia Crowns Compared to Milled Counterparts. Dent. J. 2022, 10, 215. https://doi.org/10.3390/dj10110215
Abualsaud R, Alalawi H. Fit, Precision, and Trueness of 3D-Printed Zirconia Crowns Compared to Milled Counterparts. Dentistry Journal. 2022; 10(11):215. https://doi.org/10.3390/dj10110215
Chicago/Turabian StyleAbualsaud, Reem, and Haidar Alalawi. 2022. "Fit, Precision, and Trueness of 3D-Printed Zirconia Crowns Compared to Milled Counterparts" Dentistry Journal 10, no. 11: 215. https://doi.org/10.3390/dj10110215
APA StyleAbualsaud, R., & Alalawi, H. (2022). Fit, Precision, and Trueness of 3D-Printed Zirconia Crowns Compared to Milled Counterparts. Dentistry Journal, 10(11), 215. https://doi.org/10.3390/dj10110215







