Balloon Cell Melanoma: Presentation of Four Cases with a Comprehensive Review of the Literature
Abstract
:1. Introduction
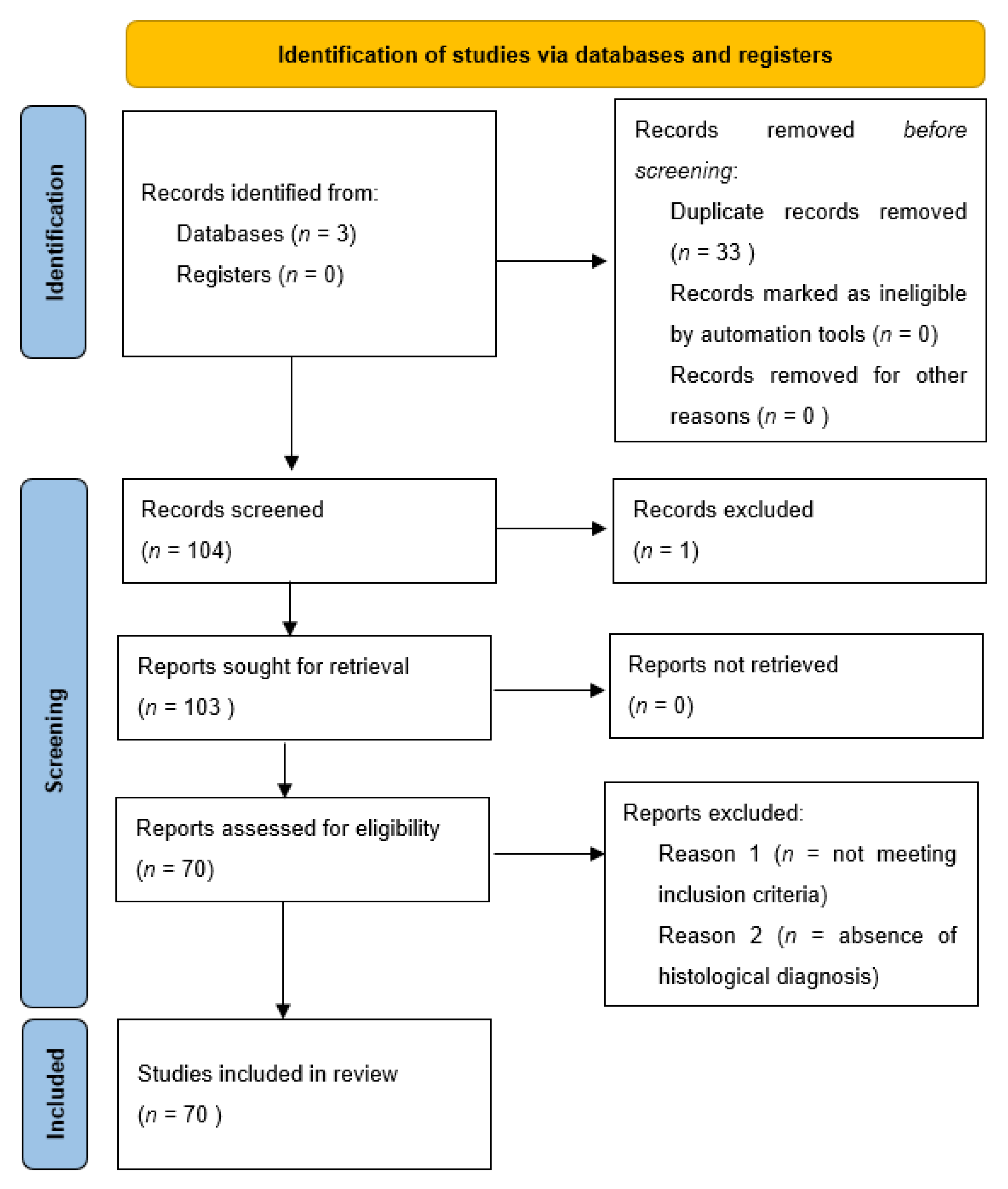
2. Materials and Methods
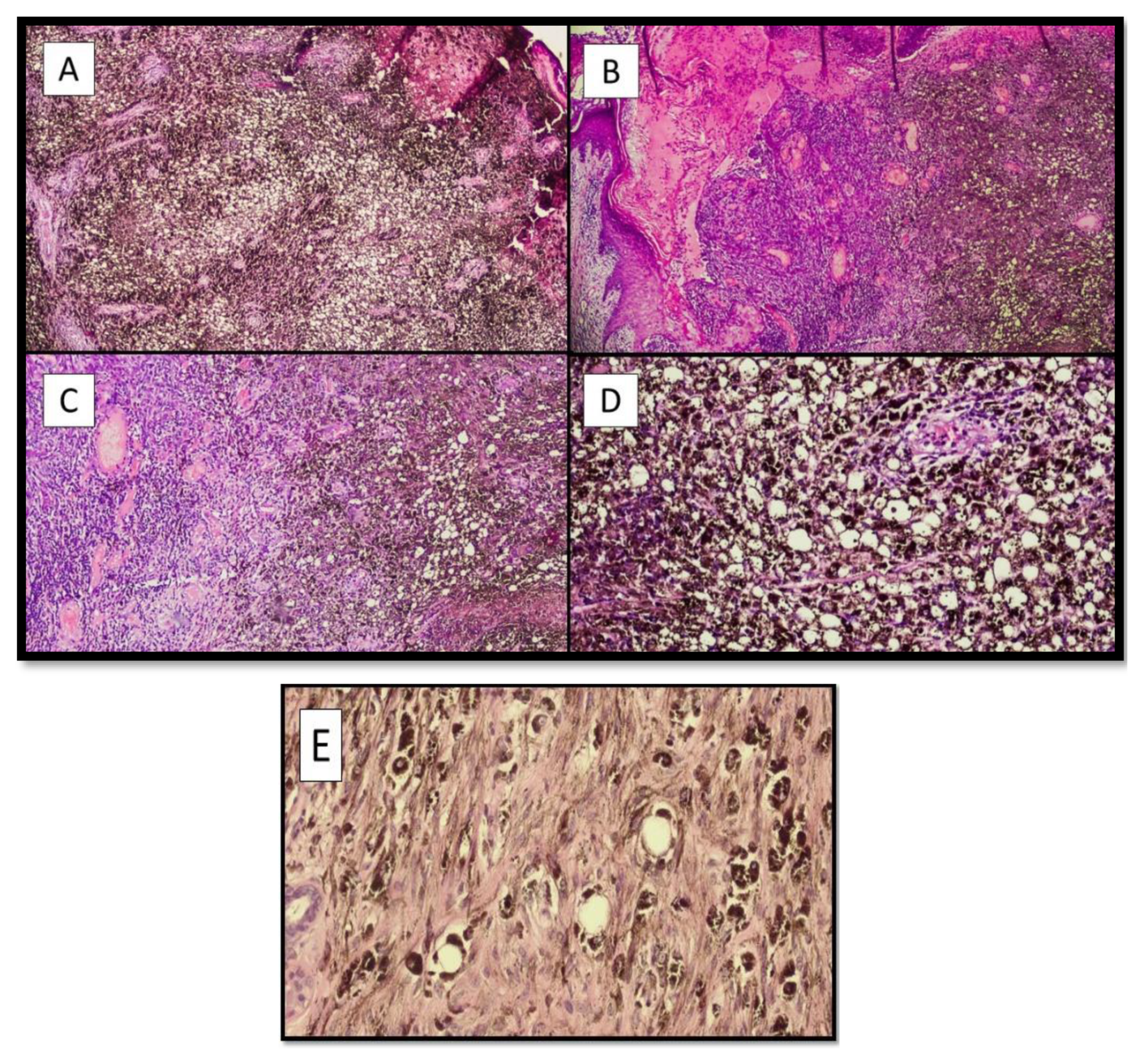
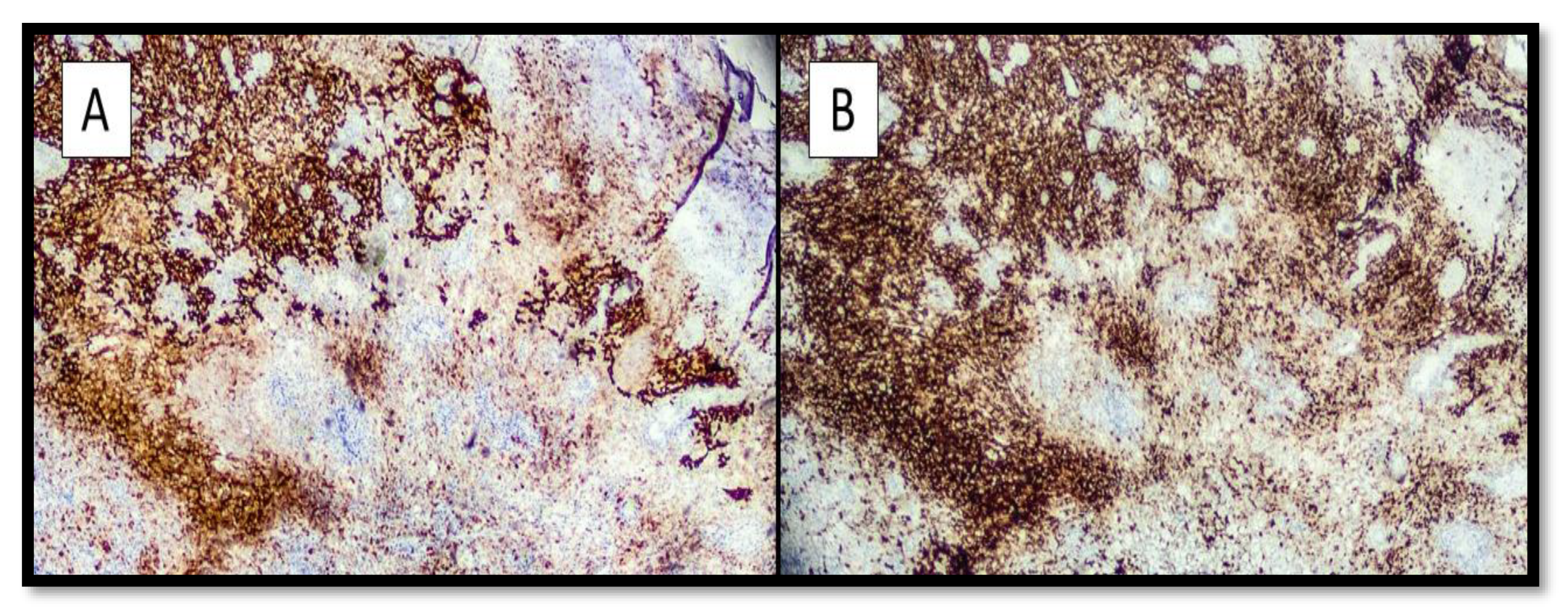
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Abbas, O.; Miller, D.D.; Bhawan, J. Cutaneous malignant melanoma: Update on diagnostic and prognostic biomarkers. Am. J. Dermatopathol. 2014, 36, 363–379. [Google Scholar] [CrossRef]
- Kozovska, Z.; Gabrisova, V.; Kucerova, L. Malignant melanoma: Diagnosis, treatment and cancer stem cells. Neoplasma 2016, 63, 510–517. [Google Scholar] [CrossRef] [Green Version]
- Limongelli, L.; Cascardi, E.; Capodiferro, S.; Favia, G.; Corsalini, M.; Tempesta, A.; Maiorano, E. Multifocal Amelanotic Melanoma of the Hard Palate: A Challenging Case. Diagnostics 2020, 10, 424. [Google Scholar] [CrossRef] [PubMed]
- Verginelli, F.; Pisacane, A.; Gambardella, G.; D’Ambrosio, A.; Candiello, E.; Ferrio, M.; Panero, M.; Casorzo, L.; Benvenuti, S.; Cascardi, E.; et al. Cancer of unknown primary stem-like cells model multi-organ metastasis and unveil liability to MEK inhibition. Nat. Commun. 2021, 12, 2498. [Google Scholar] [CrossRef] [PubMed]
- Tucci, M.; Pasculli, A.; Sgaramella, L.I.; Cazzato, G.; Macorano, E.; Piscitelli, D.; Gurrado, A.; Testini, M. Severe anemia in a patient with vulvar melanoma. Surgery 2020, 168, e21–e22. [Google Scholar] [CrossRef]
- Massi, G.; Leboit, E.P. Histological Diagnosis of Nevi and Melanoma, 2nd ed.; Spinger: Berlin/Heidelberg, Germany, 2013. [Google Scholar]
- Maher, J.; Cameron, A.; Wallace, S.; Acosta-Rojas, R.; Weedon, D.; Rosendahl, C. Balloon cell melanoma: A case report with polarized and non-polarized dermatoscopy and dermatopathology. Dermatol. Pract. Concept. 2014, 4, 69–73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oxford Centre for Evidence-Based Medicine. Levels of Evidence. 2011. Available online: http://www.cebm.net/wp-content/uploads/2014/06/CEBM-Levels-of-Evidence-2.1.pdf (accessed on 31 December 2021).
- Gardner, W.A.; Vazquez, M.D. Balloon cell melanoma. Arch. Pathol. 1970, 89, 470–472. [Google Scholar]
- Ranchod, M. Metastatic melanoma with balloon cell changes. Cancer 1972, 30, 1006–1013. [Google Scholar] [CrossRef]
- Riley, F.C. Balloon cell melanoma of the choroid. Arch. Ophthalmol. 1974, 92, 131–133. [Google Scholar] [CrossRef]
- Rodrigues, M.M.; Shields, J.A. Malignant melanoma of the choroid with balloon cells a clinicopathologic study of three cases. Can. J. Ophthalmol. 1976, 11, 208–216. [Google Scholar]
- Gatteschi, B.; Lapertosa, G.; Quaglia, A.C. Diagnosis of a case of partly clear-cell melanoblastoma (balloon cell melanoma) with metastases. Pathologica 1978, 70, 221–226. [Google Scholar] [PubMed]
- Jakobiec, F.A.; Shields, J.A.; Desjardins, L.; Iwamoto, T. Balloon cell melanomas of the ciliary body. Arch. Ophthalmol. 1979, 97, 1687–1692. [Google Scholar] [CrossRef]
- Søndergaard, K.; Henschel, A.; Hou-Jensen, K. Metastatic melanoma with balloon cell changes: An electron microscopic study. Ultrastruct. Pathol. 1980, 1, 357–360. [Google Scholar] [CrossRef] [PubMed]
- Ferracini, R.; Manetto, V.; Minghetti, G.; Lanzanova, G. Cerebellar balloon-cell metastasis of a melanoma. Tumori 1982, 68, 177–180. [Google Scholar] [CrossRef] [PubMed]
- Friedman, M.; Rao, U.; Fox, S. The cytology of metastatic balloon cell melanoma. Acta Cytol. 1982, 26, 39–43. [Google Scholar]
- Khalil, M.K. Balloon cell malignant melanoma of the choroid: Ultrastructural studies. Br. J. Ophthalmol. 1983, 67, 579–584. [Google Scholar] [CrossRef]
- Horton, J.J.; MacDonald, D.M. Balloon cell melanoma: A case report. Br. J. Dermatol. 1983, 108, 617–619. [Google Scholar] [CrossRef]
- Fievez, M. Balloon cell melanoma of the skin. Review of the literature. Apropos of 1 case. Ann. Pathol. 1984, 4, 231–235. [Google Scholar]
- Peters, M.S.; Su, W.P. Balloon cell malignant melanoma. J. Am. Acad. Dermatol. 1985, 13 Pt 2, 351–354. [Google Scholar] [CrossRef]
- Driot, J.Y.; Liotet, S. Ultrastructural study of a choroidal balloon-cell melanoma. Bull. De La Soc. Belg. Ophtalmol. 1986, 218, 103–113. [Google Scholar]
- Da, J.P. Primary anorectal malignant melanoma--report of 7 cases and review of literature. Chin. J. Oncol. 1987, 9, 372–374, 17. [Google Scholar]
- Driot, J.Y.; Rault, J.; Bonnin, P.; Liotet, S. Electron microscopy of three cases of choroid malignant melanomas. Int. Ophthalmol. 1987, 10, 193–202. [Google Scholar] [CrossRef] [PubMed]
- Aloi, F.G.; Coverlizza, S.; Pippione, M. Balloon cell melanoma: A report of two cases. J. Cutan. Pathol. 1988, 15, 230–233. [Google Scholar] [CrossRef]
- Margo, C.E. Conjunctival melanoma with balloon cell transformation. Case report. Arch. Ophthalmol. 1988, 106, 1653–1654. [Google Scholar] [CrossRef]
- Napoli, P. Balloon cell malignant melanoma. Pathologica 1988, 80, 379–385. [Google Scholar] [PubMed]
- Heid, E. A case for diagnosis: Primary melanoma or metastasis of a melanoma with balloon-like cells. Ann. Dermatol. Venereol. 1988, 115, 489–490. [Google Scholar]
- Akslen, L.A.; Myking, A.O. Balloon cell melanoma mimicking clear cell carcinoma. Pathol. Res. Pract. 1989, 184, 548–550. [Google Scholar] [CrossRef]
- Martinez, F.; Merenda, G.; Bedrossian, C.W. Lipid-rich metastatic balloon-cell melanoma: Diagnosis by a multimodal approach to aspiration biopsy cytology. Diagn. Cytopathol. 1990, 6, 427–433. [Google Scholar] [CrossRef]
- Kao, G.F.; Helwig, E.B.; Graham, J.H. Balloon cell malignant melanoma of the skin. A clinicopathologic study of 34 cases with histochemical, immunohistochemical, and ultrastructural observations. Cancer 1992, 69, 2942–2952. [Google Scholar] [CrossRef]
- Messmer, E.; Bornfeld, N.; Foerster, M.; Schilling, H.; Wessing, A. Histopathologic findings in eyes treated with a ruthenium plaque for uveal melanoma. Graefes. Arch. Clin. Exp. Ophthalmol. 1992, 230, 391–396. [Google Scholar] [CrossRef]
- Cardesi, E.; Cassia, A.; Cera, G. A case of anatomo-clinical diagnosis of balloon cell melanoma metastasis. Minerva Med. 1993, 84, 709–712. [Google Scholar] [PubMed]
- Megahed, M.; Hofmann, U.; Scharffetter-Kochanek, K.; Ruzicka, T. Amelanotic polypoid malignant melanoma of the balloon cell type. Der Pathol. 1994, 15, 350–353. [Google Scholar]
- Mowat, A.; Reid, R.; Mackie, R. Balloon cell metastatic melanoma: An important differential in the diagnosis of clear cell tumours. Histopathology 1994, 24, 469–472. [Google Scholar] [CrossRef] [PubMed]
- Adamek, D.; Kaluza, J.; Stachura, K. Primary balloon cell malignant melanoma of the right temporo-parietal region arising from meningeal naevus. Clin. Neuropathol. 1995, 14, 29–32. [Google Scholar]
- Kawamura, T.; Ohtake, N.; Takayama, O.; Furue, M.; Tamaki, K. Balloon cell melanoma cells in metastatic lesions from pedunculated malignant melanoma. J. Dermatol. 1995, 22, 527–529. [Google Scholar] [CrossRef]
- Kiene, P.; Petres-Dunsche, C.; Funke, G.; Christophers, E. Nodular balloon cell component in a cutaneous melanoma of the superficial spreading type. Dermatology 1996, 192, 274–276. [Google Scholar] [CrossRef]
- Gregel, C.; Wolter, M.; Kaufmann, R. Coincidence of balloon cell melanoma with balloon cells in a dermal nevus. Der Pathol. 1998, 19, 151–153. [Google Scholar]
- Terayama, K.; Hirokawa, M.; Shimizu, M.; Mikami, Y.; Kanahara, T.; Manabe, T. Balloon melanoma cells mimicking foamy histiocytes. Acta Cytol. 1999, 43, 325–326. [Google Scholar]
- Requena, L.; de la Cruz, A.; Moreno, C.; Sangüeza, O.; Requena, C. Animal type melanoma: A report of a case with balloon-cell change and sentinel lymph node metastasis. Am. J. Dermatopathol. 2001, 23, 341–346. [Google Scholar] [CrossRef]
- August, C.; Baba, H.A.; Heinig, J.; Nashan, D.; Höhn, P.; Holzhausen, H.J.; Metze, D.; Böcker, W. Endometrial metastasis of a “balloon” cell melanoma mimicking a “xanthomatous endometritis”. Der Pathol. 2001, 22, 145–150. [Google Scholar]
- Baehner, F.L.; Ng, B.; Sudilovsky, D. Metastatic balloon cell melanoma: A case report. Acta Cytol. 2005, 49, 543–548. [Google Scholar] [CrossRef] [PubMed]
- Hoque, S.R.; Cliff, S.H. Balloon cell melanoma: A rare form of malignant melanoma in three patients. Br. J. Dermatol. 2005, 153, 13–14. [Google Scholar]
- McGowan, J.W.; Smith, M.K.; Ryan, M.; Hood, A.F. Proliferative nodules with balloon-cell change in a large congenital melanocytic nevus. J. Cutan. Pathol. 2006, 33, 253–255. [Google Scholar] [CrossRef] [PubMed]
- Plaza, J.A.; Torres-Cabala, C.; Evans, H.; Diwan, H.A.; Suster, S.; Prieto, V.G. Cutaneous metastases of malignant melanoma: A clinicopathologic study of 192 cases with emphasis on the morphologic spectrum. Am. J. Dermatopathol. 2010, 32, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Lee, L.; Zhou, F.; Simms, A.; Wieczorek, R.; Fang, Y.; Subietas-Mayol, A.; Wang, B.; Heller, P.; Huang, H.; Pei, Z.; et al. Metastatic balloon cell malignant melanoma: A case report and literature review. Int. J. Clin. Exp. Pathol. 2011, 4, 315–321. [Google Scholar]
- Gessi, M.; Fischer, H.P.; Rösseler, L.; Urbach, H.; Pietsch, T.; van Landeghem, F.K. Unusual balloon cell features in melanoma brain metastasis: A potential diagnostic pitfall in surgical neuropathology. Clin. Neuropathol. 2011, 30, 86–88. [Google Scholar] [CrossRef]
- Richardson, M.D.; Somerset, H.; Kleinschmidt-DeMastersm, B.K.; Waziri, A. 76-year-old man with a cerebellar lesion. Brain Pathol. 2012, 22, 861–864. [Google Scholar] [CrossRef]
- Inskip, M.; Magee, J.; Barksdale, S.; Weedon, D.; Rosendahl, C. Balloon cell melanoma in primary care practice: A case report. Dermatol. Pract. Concept. 2013, 3, 25–29. [Google Scholar] [CrossRef] [Green Version]
- Bal, M.M.; Ramadwar, M.; Deodhar, K. Balloon cell melanoma of the anal canal: A wolf in sheep’s clothing? J. Cancer Res. Ther. 2013, 9, 706–708. [Google Scholar] [CrossRef]
- WHO. Classification of Skin Tumours. In WHO Classification of Tumours, 4th ed.; WHO: Genevan, Switzerland, 2018; Volume 11. [Google Scholar]
- Bures, N.; Monaco, S.E.; Palekar, A.; Pantanowitz, L. Cytomorphology of metastatic balloon cell melanoma. Diagn. Cytopathol. 2015, 43, 485–487. [Google Scholar] [CrossRef]
- Han, J.S.; Won, C.H.; Chang, S.E.; Lee, M.W.; Choi, J.H.; Moon, K.C. Primary cutaneous balloon cell melanoma: A very rare variant. Int J. Dermatol. 2014, 53, e535–e536. [Google Scholar] [CrossRef] [PubMed]
- Duman, N.; Şahin, S.; Özaygen, G.E.; Gököz, Ö. Dermoscopy of satellite metastasis of balloon cell melanoma. J. Am. Acad. Dermatol. 2014, 71, e11–e12. [Google Scholar] [CrossRef] [PubMed]
- McComiskey, M.; Iavazzo, C.; Datta, M.; Slade, R.; Winter-Roach, B.; Lambe, G.; Sangar, V.K.; Smith, M. Balloon Cell Urethral Melanoma: Differential Diagnosis and Management. Case Rep. Obstet. Gynecol. 2015, 2015, 919584. [Google Scholar] [CrossRef] [PubMed]
- Seabra Resende, F.S.; Conforti, C.; Giuffrida, R.; Corneli, P.; Fagotti, S.; Custrin, A.; Shaffiei, V.; Zalaudek, I.; Di Meo, N. Balloon Cell Primary Nodular Melanoma: Dermoscopy Evidence. Dermatol. Pract. Concept. 2019, 9, 155–156. [Google Scholar] [CrossRef] [Green Version]
- Inskip, M.; James, N.; Magee, J.; Rosendahl, C. Pigmented primary cutaneous balloon cell melanoma demonstrating balloon cells in the dermoepidermal junction: A brief case report with dermatoscopy and histopathology. Int J. Dermatol. 2016, 55, e110–e112. [Google Scholar] [CrossRef]
- Hattori, Y.; Sentani, K.; Hattori, T.; Matsuo, Y.; Kawai, M.; Shindo, H.; Tanaka, M.; Hide, M.; Yasui, W. Balloon Cell Malignant Melanoma in a Young Female: A Case Report and Review of the Literature. Case Rep. Oncol. 2016, 9, 262–266. [Google Scholar] [CrossRef]
- Chavez-Alvarez, S.; Villarreal-Martinez, A.; Miranda-Maldonado, I.; Ocampo-Candiani, J.; Garza-Rodriguez, V. Balloon Cell Melanoma and Its Metastasis, a Rare Entity. Am. J. Dermatopathol. 2017, 39, 404–411. [Google Scholar] [CrossRef]
- Iliadis, A.; Zaraboukas, T.; Selviaridis, P.; Chatzisotiriou, A. Balloon cell melanoma metastasis to the temporal lobe. Indian J. Pathol. Microbiol. 2017, 60, 622–623. [Google Scholar] [CrossRef]
- Saharti, S.; Isaila, B.; Mudaliar, K.; Wojcik, E.M.; Pambuccian, S.E. Balloon cells in metastatic melanoma. Diagn. Cytopathol. 2017, 45, 828–831. [Google Scholar] [CrossRef]
- Friedman, B.J.; Stoner, R.; Sahu, J.; Lee, J.B. Association of Clinical, Dermoscopic, and Histopathologic Findings with Gene Expression in Patients with Balloon Cell Melanoma. JAMA Dermatol. 2018, 154, 77–81. [Google Scholar] [CrossRef]
- Farah, M.; Nagarajan, P.; Torres-Cabala, C.A.; Curry, J.L.; Amaria, R.N.; Wargo, J.; Tawbi, H.; Ivan, D.; Prieto, V.G.; Tetzlaff, M.T.; et al. Metastatic melanoma with balloon/histiocytoid cytomorphology after treatment with immunotherapy: A histologic mimic and diagnostic pitfall. J. Cutan. Pathol. 2018, 45, 545–549. [Google Scholar] [CrossRef] [PubMed]
- Ravaioli, G.M.; Baraldi, C.; Dika, E.; Fanti, P.A.; Misciali, C. An Ulcerated Reddish Nodule of the Chest: When You See, Think …. Dermatopathology 2018, 5, 117–120. [Google Scholar] [CrossRef]
- Caltabiano, R.; Broggi, G.; Garro, R.; Terranova, M.; Argenziano, G. Balloon cell melanoma: An uncommon entity representing a diagnostic pitfall in dermatopathology. Ital. J. Dermatol. Venereol. 2021, 156, 82–88. [Google Scholar] [CrossRef]
- Goto, H.; Shimauchi, T.; Fukuchi, K.; Yokota, N.; Koizumi, S.; Aoshima, M.; Endo, Y.; Masuda, Y.; Miyazawa, H.; Kasuya, A.; et al. Therapeutic Effectiveness of Immunoradiotherapy on Brain-metastatic BRAF/MEK Inhibitor-resistant Melanoma with Balloon Cell Change. Acta Derm. Venereol. 2019, 99, 612–613. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, Y.Y.; Lan, C.E.; Yen, M.C.; Cheng, S.T. Balloon cell melanoma possessed the ability to develop BRAF V600E mutation in cancer cells. Kaohsiung J. Med. Sci. 2021, 37, 154–155. [Google Scholar] [CrossRef] [PubMed]
- Wei, G.; Hennessy, K.; Kevin Heard, L.; Gaudi, S.; Mhaskar, R.; Patel, R.R.; Bennett, A.E. Balloon cell melanoma: A systematic review. Int J. Dermatol. 2021, 61, 266–277. [Google Scholar] [CrossRef]
- García-Piqueras, P.; Avilés-Izquierdo, J.A.; Almodóvar-Real, A.; Nieto-Benito, L.M.; Rodríguez Lomba, E. Clues in dermoscopy: White and yellow structures in balloon cell melanoma. Eur. J. Dermatol. 2021, 31, 676–677. [Google Scholar] [CrossRef]
- Laforga, J.B. Fine-needle aspiration cytological findings in three cases of metastatic amelanotic melanoma to the parotid gland with divergent differentiation. Diagn. Cytopathol. 2021, 24. [Google Scholar] [CrossRef]
- Macák, J.; Krc, I.; Elleder, M.; Lukás, Z.; Nádasdy, T.; Güttnerová, J. Balloon cell melanoma of the skin. Part I: Histology, immunohistology and histochemistry. Acta Univ. Palacki. Olomuc. Fac. Med. 1990, 126, 71–82. [Google Scholar]
- Macák, J.; Krc, I. Balloon cell melanoma of the skin. Part II: An electron-microscopic study. Acta Univ. Palacki. Olomuc. Fac. Med. 1990, 126, 83–92. [Google Scholar]
- Barnhill, R.L. Pathology and prognostic factors. Curr. Opin. Oncol. 1993, 5, 364–376. [Google Scholar] [CrossRef] [PubMed]
- Nowak, M.A.; Fatteh, S.M.; Campbell, T.E. Glycogen-rich malignant melanomas and glycogen-rich balloon cell malignant melanomas: Frequency and pattern of PAS positivity in primary and metastatic melanomas. Arch. Pathol. Lab. Med. 1998, 122, 353–360. [Google Scholar] [PubMed]
- McCarthy, S.W.; Scolyer, R.A. Melanocytic lesions of the face: Diagnostic pitfalls. Ann. Acad. Med. Singap. 2004, 33, 3–14. [Google Scholar] [PubMed]
- Larre Borges, A.; Zalaudek, I.; Longo, C.; Dufrechou, L.; Argenziano, G.; Lallas, A.; Piana, S.; Moscarella, E. Melanocytic nevi with special features: Clinical-dermoscopic and reflectance confocal microscopic-findings. J. Eur. Acad. Dermatol. Venereol. 2014, 28, 833–845. [Google Scholar] [CrossRef]
- Kazlouskaya, V.; Guo, Y.; Maia-Cohen, S.; Mones, J. Clear-cell melanocytic lesions with balloon-cell and sebocyte-like melanocytes: A unifying concept. Am. J. Dermatopathol. 2014, 36, 380–386. [Google Scholar] [CrossRef]
- Valdivielso-Ramos, M.; Burdaspal, A.; Conde, E.; de la Cueva, P. Balloon-cell variant of the Spitz nevus. J. Eur. Acad. Dermatol Venereol. 2016, 30, 1621–1622. [Google Scholar] [CrossRef]
- Borsa, S.; Toonstra, J.; van der Putte, S.C.; van Vloten, W.A. Balloon-cell variant of the Spitz nevus. Hautarzt 1991, 42, 707–708. [Google Scholar]
- Budde, M.; Schlötzer-Schrehardt, U.; Hofmann-Rummelt, C.; Holbach, L.M. Conjunctival balloon cell nevi--light- and electronmicroscopic findings in 2 patients. Klin. Monbl. Augenheilkd. 2001, 218, 269–272. [Google Scholar] [CrossRef]
| Number of Patient | Age | Gender | Localization | Clinical Appereance |
|---|---|---|---|---|
| 1 | 76 | F | left hand back | Malignant melanoma |
| 2 | 75 | M | back | Malignant melanoma |
| 3 | 36 | F | Left leg | Dysplastic nevus |
| 4 | 51 | M | Right side | Malignant melanoma |
| Author(s) | Year | Number of Patient | Localization | Clinical Appeareance | Primitive/Metastastic |
|---|---|---|---|---|---|
| Gardner et al. [9] | 1970 | 1 | back | MM | primitive |
| Ranchod, M. [10] | 1972 | 2 | Right calf and inguinal lymph node | Metastasis of MM and soft tissue tumour | both metastatic |
| Riley, F.C [11] | 1974 | 2 | Ciliary body | Pigmented lesion | primitive |
| Rodrigues et al. [12] | 1976 | 3 | Choroid | Pigmented lesion | primitive |
| Gatteschi et al. [13] | 1978 | 1 | Back | MM | primitive and then metastatic |
| Jakobiec et al. [14] | 1979 | 1 | Ciliary body | Pigmented lesion | primitive |
| Søndergaard et al. [15] | 1980 | 1 | Back | MM | primitive |
| Ferracini et al. [16] | 1982 | 1 | Cerebellar | MM | metastatic |
| Friedman et al. [17] | 1982 | 2 | / | / | metastatic |
| Khalil et al. [18] | 1983 | 1 | Choroid | pigmented lesion | primitive |
| Horton et al. [19] | 1983 | 1 | arm | MM | primitive |
| Fievez et al. [20] | 1984 | 1 | back | MM | primitive |
| Peters et al. [21] | 1985 | 1 | Back with satellitosis | MM | primitive |
| Driot [22] | 1986 | 1 | Choroid | pigmented lesion | primitive |
| Da [23] | 1987 | 7 | anorectal | pigmented lesion | Primitive (7) |
| Driot et al. [24] | 1987 | 1 | Choroid | pigmented lesion | primitive |
| Aloi et al. [25] | 1988 | 2 | Back and arm | Pigmented lesion and amelanotic lesion | primitive (2) |
| Margo et al. [26] | 1988 | 1 | conjunctiva | pigmented macule | primitive |
| Napoli [27] | 1988 | 1 | arm | pigmented lesion | primitive |
| Heid [28] | 1988 | 1 | forearm | MM | primitive or metastatic ? |
| Akslen et al. [29] | 1989 | 1 | unknown | / | metastatic |
| Martinez et al. [30] | 1990 | 1 | eye | pigmented lesion | metastatic (liver) |
| Kao et al. [31] | 1992 | 34 | various site | pigmented and/or amelanotic lesion | primitive and then metastatic |
| Messmer et al. [32] | 1992 | 1 | uveal melanoma | pigmented macule | primitive |
| Cardesi et al. [33] | 1993 | 1 | lymph node | not detected | metastatic |
| Megahed et al. [34] | 1994 | 1 | / | MM | primitive (polipoid) |
| Mowat et al. [35] | 1994 | 2 | back (2) | MM (2) | primitive (2) |
| Adamek et al. [36] | 1995 | 1 | meninges | pigmented lesion | primitive from meningeal nevus |
| Kawamura et al. [37] | 1995 | 1 | forearm | MM | metastatic |
| Kiene et al. [38] | 1996 | 1 | back | MM | primitive |
| Gregel et al. [39] | 1998 | 1 | back | MM | primitive |
| Terayama et al. [40] | 1999 | 1 | arm | / | primitive |
| Requena et al. [41] | 2001 | 1 | back | MM | primitive and then metastatic |
| August et al. [42] | 2001 | 1 | unknow | / | metastatic |
| Baehner et al. [43] | 2005 | 1 | unknow | laterocervical swelling (right) | metastatic |
| Hoque et al. [44] | 2005 | 3 | Back (2) and arm (1) | MM (3) | primitive (3) |
| McGowan et al. [45] | 2006 | 1 | back | pigmented lesion | primitive |
| Plaza et al. [46] | 2010 | 2 of 192 lesions | back | MM | primitive |
| Lee et al. [47] | 2011 | 1 | neck | neck swelling | primitive and then metastatic |
| Gessi et al. [48] | 2011 | 1 | brain | MM (skin) | primitive, then metastatic |
| Richardson et al. [49] | 2012 | 1 | cerebellum | MM (skin) | primitive, then metastatic |
| Inskip et al. [50] | 2013 | 1 | back | pigmented lesion | primitive |
| Bal et al. [51] | 2013 | 1 | anal canal | pigmented macule | primitive |
| Maher et al. [52] | 2014 | 1 | left forearm | pale nodule | primitive |
| Bures et al. [53] | 2015 | 1 | right tibia | amelanotic lesion | Metastatic from head BCM |
| Han et al. [54] | 2014 | 1 | right shin | Black nodule | primitive |
| Duman et al. [55] | 2014 | 1 | chest | papule | Primitive with satellitosis |
| McComiskey et al. [56] | 2015 | 1 | urethra | nodule | Primitive urethral MM |
| Seabra Resende et al. [57] | 2019 | 1 | right leg | reddish nodule | primitive |
| Inskip et al. [58] | 2016 | 1 | right posterior upper arm | atypical pigmented lesion | primitive |
| Hattori et al. [59] | 2016 | 1 | left lumbar region | atypical lesion | Primitive and then metastatic |
| Chavez-Alvarez et al. [60] | 2017 | 1 | chest | pigmented lesion | primitive |
| Iliadis et al. [61] | 2017 | 1 | unknown | / | metastatic to temporal lobe |
| Saharti et al. [62] | 2017 | 1 | left scapula | hyperpigmented lesion | primitive and then metastatic |
| Friedman et al. [63] | 2018 | 2 | back (1) left shoulder (1) | pigmented papule (1) black macule (1) | primitive (2) |
| Farah et al. [64] | 2018 | 1 | lymph node swelling | previous MM on feet | metastatic |
| Ravaioli et al. [65] | 2018 | 1 | chest | reddish nodule | primitive |
| Caltabiano et al. [66] | 2019 | 1 | back | amelanotic papule | primitive |
| Goto et al. [67] | 2019 | 1 | brain | nodule | metastatic |
| Chen et al. [68] | 2021 | 1 | upper conjunctiva | brownish noduloplauques | metastatic |
| Wei et al. [69] | 2021 | 1 | left infraorbital fold | subcutaneous nodule | primitive |
| García-Piqueras et al. [70] | 2021 | 3 | back (2) and arm (1) | pigmented lesion | primitive (3) |
| Laforga et al. [71] | 2021 | 1 | neck | pigmented lesion | metastatic to the parotid |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cazzato, G.; Cascardi, E.; Colagrande, A.; Cimmino, A.; Ingravallo, G.; Lospalluti, L.; Romita, P.; Demarco, A.; Arezzo, F.; Loizzi, V.; et al. Balloon Cell Melanoma: Presentation of Four Cases with a Comprehensive Review of the Literature. Dermatopathology 2022, 9, 100-110. https://doi.org/10.3390/dermatopathology9020013
Cazzato G, Cascardi E, Colagrande A, Cimmino A, Ingravallo G, Lospalluti L, Romita P, Demarco A, Arezzo F, Loizzi V, et al. Balloon Cell Melanoma: Presentation of Four Cases with a Comprehensive Review of the Literature. Dermatopathology. 2022; 9(2):100-110. https://doi.org/10.3390/dermatopathology9020013
Chicago/Turabian StyleCazzato, Gerardo, Eliano Cascardi, Anna Colagrande, Antonietta Cimmino, Giuseppe Ingravallo, Lucia Lospalluti, Paolo Romita, Aurora Demarco, Francesca Arezzo, Vera Loizzi, and et al. 2022. "Balloon Cell Melanoma: Presentation of Four Cases with a Comprehensive Review of the Literature" Dermatopathology 9, no. 2: 100-110. https://doi.org/10.3390/dermatopathology9020013
APA StyleCazzato, G., Cascardi, E., Colagrande, A., Cimmino, A., Ingravallo, G., Lospalluti, L., Romita, P., Demarco, A., Arezzo, F., Loizzi, V., Dellino, M., Trilli, I., Bellitti, E., Parente, P., Lettini, T., Foti, C., Cormio, G., Maiorano, E., & Resta, L. (2022). Balloon Cell Melanoma: Presentation of Four Cases with a Comprehensive Review of the Literature. Dermatopathology, 9(2), 100-110. https://doi.org/10.3390/dermatopathology9020013














