Incidence of Methicillin Resistant Staphylococcus aureus (MRSA) in Burn Intensive Care Unit: A Systematic Review
Abstract
Introduction
Methods
Population intervention comparator and outcome
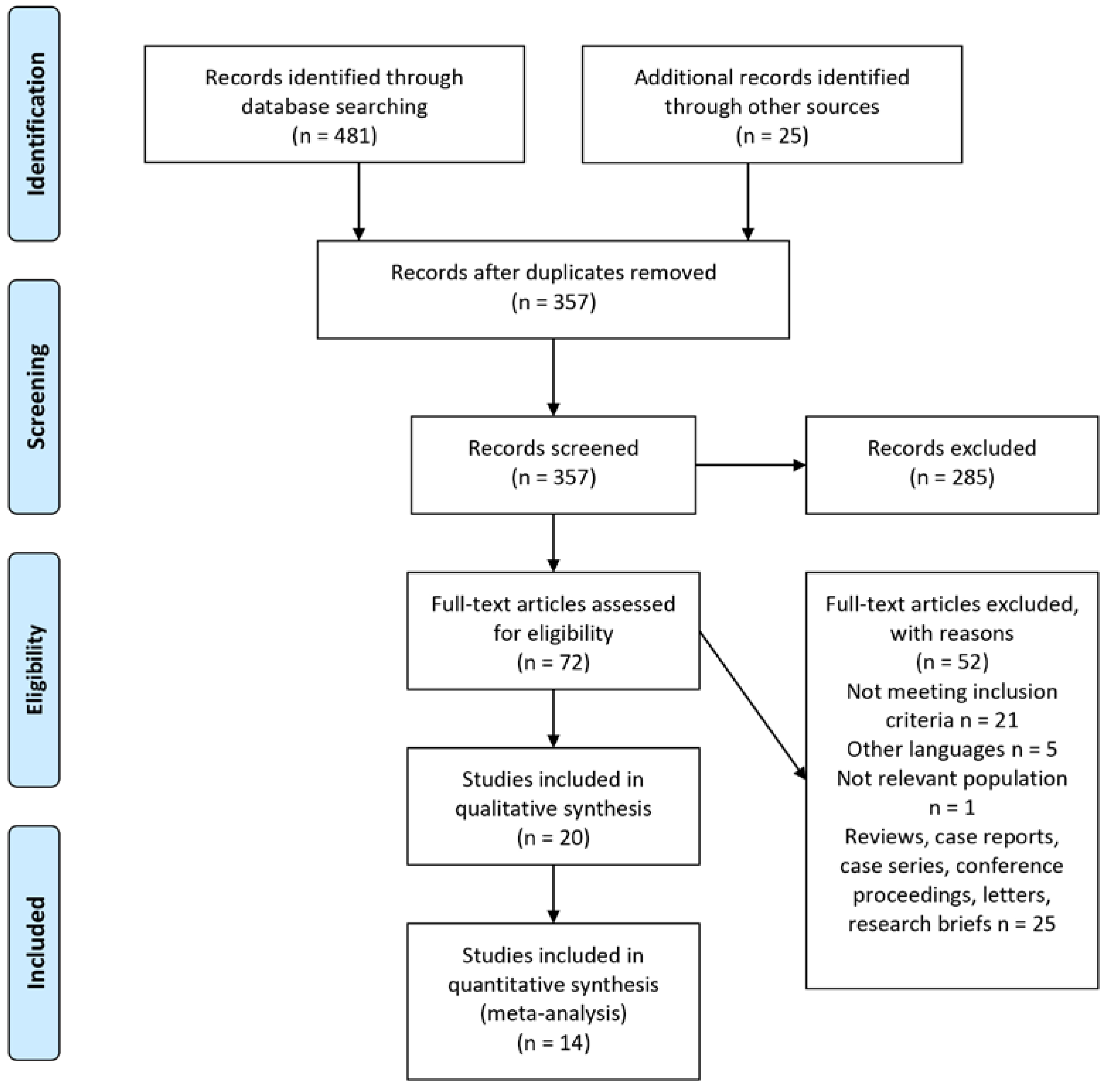
Study selection
Data extraction and quality assessment
Data synthesis and analysis
Results
Study selection
Study characteristics
Quality assessment
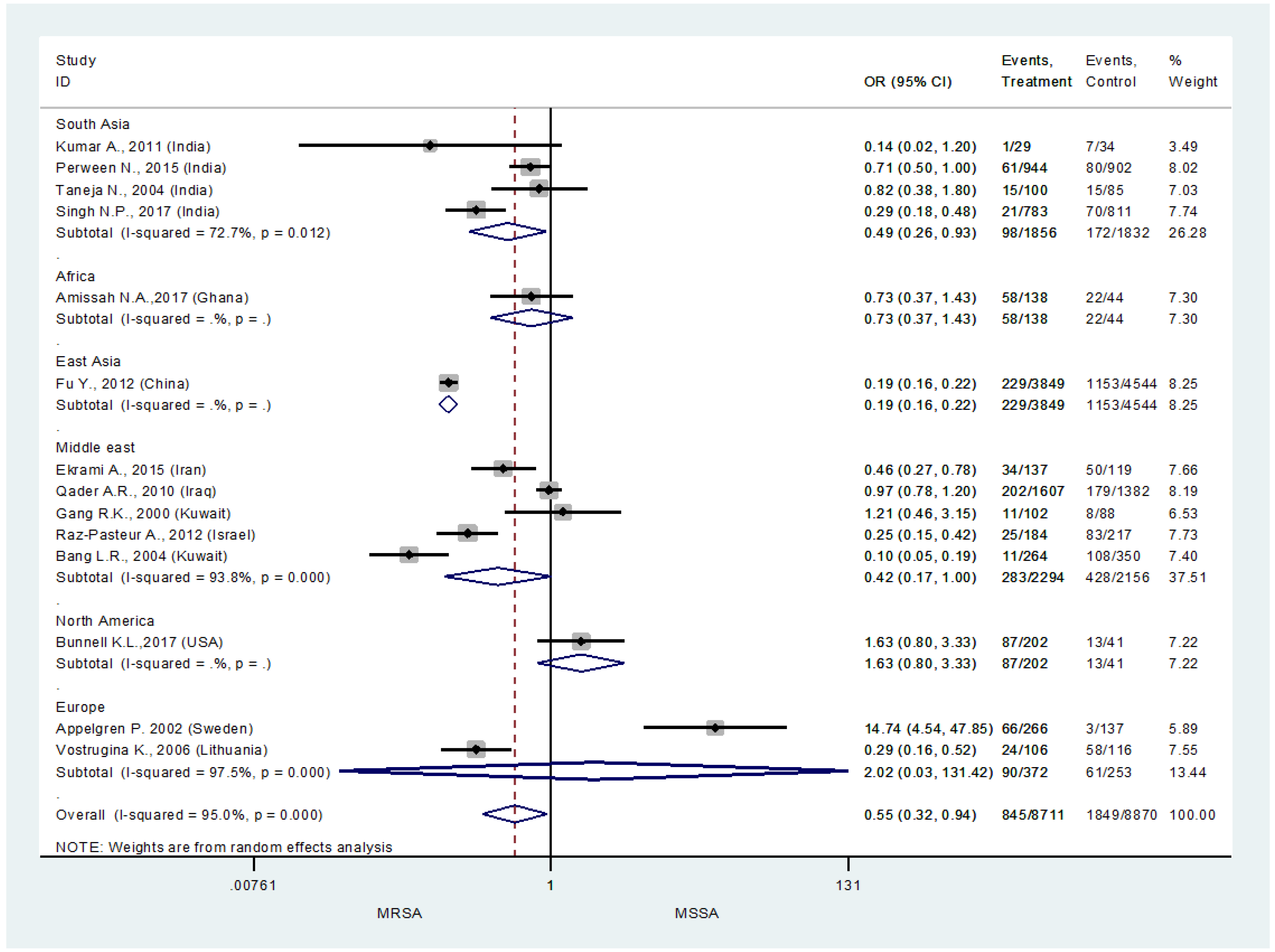
Overall risk of MRSA in burn ICU
Discussion
Conclusions
Authors Contributions
Funding
Acknowledgments
Conflicts of interest
Appendix A
| First author, country, year (ref) | Study design | Study year | Recruitment site | Condition /diagnosis | No. of participants | Total no. of isolates | S. aureus | MSSA | MRSA | Antibiotic resistance profile of MRSA isolates | Quality score | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Resistant | Susceptible | |||||||||||
| Kumar A, India, 2011 | Cohort study | 2009-2010 | Burn ward of Guru Teg Bahadur Hospital | Sepsis/septicemia | 80 | 28 | 8 | 1 | 7 | Cephalexin (62.5%), erythromycin (62.5%), amoxicillin (62.5%), ciprofloxacin (62.5%), cefoxitin (87.5%), co-trimoxazole (75%), gentamicin (50%) | Vancomycin (100%) | 7 |
| Perween N, India, 2015 | Cross-sectional study | 2012 | Burn ward of a tertiary care hospital | Burn wound infection | 1294 | 883 | 141 | 61 | 80 | Penicillin (100%), cephalexin (100%), cefazolin (100%), erythromycin (98.7%), clindamycin (97.4%), gentamicin (97.4%), amikacin (84.6%), ofloxacin (96.2%), ciprofloxacin (100%) | Vancomycin (100%), teicoplanin (100%), linezolid (97.4%), chloramphenicol (85.9%), rifampicin (88.5%) | 6 |
| Amissah NA, Ghana, 2017 | Cross- sectional study | 2014-2015 | Burn unit, Reconstructive Plastic Surgery and Burn Center of Korle Bu Teaching Hospital | Nosocomial infections/burn wound infection | 62 | 80 | 80 | 58 | 22 | N/A | N/A | 7 |
| Fu Y, China, 2012 | Cross-sectional study | 1998-2009 | Burn center, Changhai Hospital | Burn wound infection | 114 | 3620 | 1382 | 229 | 1153 | N/A | Vancomycin (100%) | 7 |
| Taneja N, India, 2004 | Cohort study | 2000-2001 | Burn unit of a tertiary care referral center | Hospital-acquired infections/burn wound infection | 74 | 85 | 30 | 15 | 15 | Erythromycin (66.6%), netilmicin (22.2%), cefotaxime (55.5%), ciprofloxacin (44.4%), gentamicin (77.7%) | N/A | 8 |
| Ekrami A, Iran, 2015 | Cross-sectional study | 2013-2014 | Burn center, Taleghani burn hospital | Burn wound infection | N/A | 103 | 96 | 34 | 50 | Penicillin (100%), cefoxitin (93%), ampicillin (89%), erythromycin (71%), tetracycline (75%), gentamicin (64%), ciprofloxacin (71%), ampicillin-sulbactam (57%), ceftazidime (79%) | N/A | 7 |
| Cen H, China, 2015 | Cross-sectional study | 2011-2013 | Burn ward of Zhejiang University of Medicine | Hospital-acquired infections/ burn wound infection | 1942 | 2212 | 410 | N/A | 324 | N/A | N/A | 6 |
| Qader AR, Iraq, 2010 | Cross-sectional study | 2008-2009 | Sulaimani Burn, Reconstructive and Plastic Surgery Hospital | Nosocomial infections/ burn wound infection | 760 | 1405 | 462 | 202 | 179 | N/A | N/A | 7 |
| Bunnell KL, USA, 2017 | Cohort study | 2012-2015 | Trauma and burn ICU at Rhode Island Hospital, a level I trauma center | Nosocomial infections | 80 | 115 | N/A | 87 | 13 | N/A | N/A | 6 |
| Gang RK, Kuwait, 2000 | Cohort study | 1992-1998 | Burn Unit of the Al-Babtain Centre for Burns and Plastic Surgery of the Ibn Sina Hospital | Sepsis/septicemia | 80 | 91 | N/A | 11 | 8 | N/A | N/A | 6 |
| DiMuzio EE, USA, 2012 | Cross-sectional study | 2004-2011 | Cincinnati Shriners Hospital for Children | Burn wound infection | N/A | 7217 | 1790 | N/A | 806 | N/A | N/A | 8 |
| Raz-Pasteur A, Israel, 2012 | Cross-sectional study | 2001-2009 | Rambam Healthcare Campus (RHC) Burn Unit and ICU | Sepsis | 159 | 159 | N/A | 25 | 83 | N/A | N/A | 8 |
| Ronat J, Iraq, 2014 | Cross-sectional study | 2008-2009 | Sulaymaniyah burn center | Systemic infections due to burns | 1169 | 65 | 17 | N/A | N/A | Penicillin G (100%), oxacillin (100%), gentamicin (88%), fusidic acid (71%), levofloxacin (59%), clindamycin (35%), minocycline (29%), rifampin (29%) | Quinupristin-dalfopristin (88%), nitrofurantoin (100%), vancomycin (100%) | 7 |
| Appelgren P, Sweden, 2002 [19] | Cohort study | 1993-1995 | Burn unit of Karolinska Hospital | Nosocomial/community acquired infections | 230 | 200 | 69 | 66 | 3 | N/A | N/A | 8 |
| Bang LR, Kuwait, 2004 | Cohort study | 1992-2001 | Burns Unit, Al-Babtain Centre for Burns and Plastic Surgery | Sepsis/septicemia | 166 | 253 | 119 | 11 | 108 | N/A | N/A | 6 |
| Vostrugina K, Lithuania, 2006 | Cohort study | 1999-2003 | Department of Plastic Surgery and Burns of Kaunas University of Medicine Hospital | 82 | 82 | N/A | 24 | 58 | N/A | N/A | 7 | |
| Schweizer M, USA, 2012 | Cohort study | 2009-2010 | BTU of a teaching hospital with a level-1 trauma center | Sepsis/bacteremia | 144 | 144 | N/A | N/A | 24 | Erythromycin (91%) | Linezolid (100%), daptomycin (100%), quinupristin-dalfopristin (100%), rifampin (100%), co-trimoxazole (100%), gentamicin (100%), vancomycin (100%) | 6 |
| Naqvi Z.A., Pakistan, 2007 | Cross-sectional study | 2002-2003 | Department of Microbiology, Basic Medical Sciences Institute, Jinnah Postgraduate Medical Centre, Karachi | Burn wound infection | 52 | 190 | 41 | N/A | 10 | Clindamycin (70%), amikacin (90%), ciprofloxacin (100%), gentamicin (80%), clarithromycin (80%) | Vancomycin (100%), chloramphenicol (100%) | 6 |
| Lee H.G., Korea, 2013 | Cross-sectional study | 2007-2011 | Burn intensive care unit | Nosocomial infections/burn wound infection | 397 | 562 | 81 | N/A | 78 | N/A | N/A | 8 |
| Singh N.P., India, 2017 | Cross-sectional study | 2010-2014 | Burn wards and intensive care unit | Nosocomial infections/burn wound infection | N/A | 762 | N/A | 21 | 70 | N/A | N/A | 6 |
| Fransen J., Sweden, 2016 | Cross-sectional study | 1994-2012 | The Burn Center, Department of Hand, Plastic and Burn Surgery, University Hospital of Linko Ping | Burn wound infection | 1570 | 4531 | 851 | N/A | 15 | N/A | N/A | 8 |
References
- Norbury, W.; Herndon, D.N.; Tanksley, J.; Jeschke, M.G.; Finnerty, C.C. Infection in burns. Surg Infect (Larchmt). 2016, 17, 250–255. [Google Scholar] [CrossRef]
- Perween, N.; Krishanprakash, S.; Bharara, T. Bacteriological profile of burn wound infection in a tertiary care hospital in North India with special reference to methicillin resistant Staphylococcus aureus. Int Multispec J Health 2015, 1, 6–11. [Google Scholar]
- Church, D.; Elsayed, S.; Reid, O.; Winston, B.; Lindsay, R. Burn wound infections. Clin Microbiol Rev 2006, 19, 403–434. [Google Scholar] [CrossRef] [PubMed]
- Alebachew, T.; Yismaw, G.; Derabe, A.; Sisay, Z. Staphylococcus aureus burn wound infection among patients attending Yekatit 12 Hospital burn unit, Addis Ababa, Ethiopia. Ethiop J Health Sci 2012, 22, 209–213. [Google Scholar] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann Intern Med 2009, 151, 264–269. [Google Scholar] [PubMed]
- Kumar, A.; Kashyap, B.; Mishra, S.; Agarwal, V.; Kaur, I.R. Bacteriological analysis and antibacterial resistance pattern in burn sepsis: An observation at a tertiary care hospital in East Delhi. Infect Dis Clin Pract 2011, 19, 406–412. [Google Scholar] [CrossRef]
- Singh, N.P.; Rani, M.; Gupta, K.; Sagar, T.; Kaur, I.R. Changing trends in antimicrobial susceptibility pattern of bacterial isolates in a burn unit. Burns 2017, 43, 1083–1087. [Google Scholar] [CrossRef]
- Taneja, N.; Emmanuel, R.; Chari, P.S.; Sharma, M. A prospective study of hospital-acquired infections in burn patients at a tertiary care referral centre in North India. Burns 2004, 30, 665–669. [Google Scholar] [CrossRef]
- Schweizer, M.; Ward, M.; Cobb, S.; et al. The epidemiology of methicillin-resistant Staphylococcus aureus on a burn trauma unit. Infect Control Hosp Epidemiol 2012, 33, 1118–1125. [Google Scholar] [CrossRef]
- Bunnell, K.L.; Zullo, A.R.; Collins, C.; Adams, C.A., Jr. Methicillin-resistant Staphylococcus aureus pneumonia in critically ill trauma and burn patients: A retrospective cohort study. Surg Infect (Larchmt) 2017, 18, 196–201. [Google Scholar] [CrossRef]
- DiMuzio, E.E.; Healy, D.P.; Durkee, P.; Neely, A.N.; Kagan, R.J. Trends in bacterial wound isolates and antimicrobial susceptibility in a pediatric hospital. J Burn Care Res 2014, 35, e304–e311. [Google Scholar] [CrossRef] [PubMed]
- Jahangard-Rafsanjani, Z.; Sarayani, A.; Nosrati, M.; et al. Effect of a community pharmacist-delivered diabetes support program for patients receiving specialty medical care: A randomized controlled trial. Diabetes Educ 2015, 41, 127–135. [Google Scholar] [CrossRef]
- Fu, Y.; Xie, B.; Ben, D.; et al. Pathogenic alteration in severe burn wounds. Burns 2012, 38, 90–94. [Google Scholar] [CrossRef]
- Ronat, J.B.; Kakol, J.; Khoury, M.N.; et al. Highly drug-resistant pathogens implicated in burn-associated bacteremia in an Iraqi burn care unit. PLoS ONE 2014, 9, e101017. [Google Scholar] [CrossRef]
- Qader, A.R.; Muhamad, J.A. Nosocomial infection in Sulaimani Burn Hospital, Iraq. Ann Burns Fire Disasters 2010, 23, 177–181. [Google Scholar] [PubMed]
- Bang, R.L.; Sharma, P.N.; Sanyal, S.C.; Bang, S.; Ebrahim, M.K. Burn septicaemia in Kuwait: Associated demographic and clinical factors. Med Princ Pract 2004, 13, 136–141. [Google Scholar] [CrossRef]
- Gang, R.K.; Sanyal, S.C.; Bang, R.L.; Mokaddas, E.; Lari, A.R. Staphylococcal septicaemia in burns. Burns 2000, 26, 359–366. [Google Scholar] [CrossRef] [PubMed]
- Fransén, J.; Huss, F.R.; Nilsson, L.E.; Rydell, U.; Sjöberg, F.; Hanberger, H. Surveillance of antibiotic susceptibility in a Swedish Burn Center 1994-2012. Burns 2016, 42, 1295–1303. [Google Scholar] [CrossRef]
- Appelgren, P.; Björnhagen, V.; Bragderyd, K.; Jonsson, C.E.; Ransjö, U. A prospective study of infections in burn patients. Burns 2002, 28, 39–46. [Google Scholar] [CrossRef]
- Amissah, N.A.; van Dam, L.; Ablordey, A.; et al. Epidemiology of Staphylococcus aureus in a burn unit of a tertiary care center in Ghana. PLoS ONE 2017, 12, e0181072. [Google Scholar] [CrossRef]
- Leslie, T.; Briceño, M.; Mayan, I.; et al. The impact of phenotypic and genotypic G6PD deficiency on risk of Plasmodium vivax infection: A case-control study amongst Afghan refugees in Pakistan. PLoS Med 2010, 7, e1000283. [Google Scholar] [CrossRef]
- Raz-Pasteur, A.; Hussein, K.; Finkelstein, R.; Ullmann, Y.; Egozi, D. Blood stream infections (BSI) in severe burn patients—early and late BSI: A 9-year study. Burns 2013, 39, 636–642. [Google Scholar] [CrossRef] [PubMed]
- Vostrugina, K.; Gudaviciene, D.; Vitkauskiene, A. Bacteremias in patients with severe burn trauma. Medicina (Kaunas) 2006, 42, 576–579. [Google Scholar]
- Naqvi, Z.A.; Hashmi, K.; Kharal, S.A. Methicillin resistant S. aureusin burn patients. Pak J Pharmacol 2007, 24, 7–11. [Google Scholar]
- Lee, H.G.; Jang, J.; Choi, J.E.; et al. Blood stream infections in patients in the burn intensive care unit. Infect Chemother 2013, 45, 194–201. [Google Scholar] [CrossRef]
- Cen, H.; Wu, Z.; Wang, F.; Han, C. Pathogen distribution and drug resistance in a burn ward: A three-year retrospective analysis of a single center in China. Int J Clin Exp Med 2015, 8, 19188–19199. [Google Scholar]
- Ekrami, A.; Montazeri, E.A.; Kaydani, G.A.; Shokoohizadeh, L. Methicillin resistant staphylococci: Prevalence and susceptibility patterns in a burn center in Ahvaz from 2013-2014. Iran J Microbiol 2015, 7, 208–213. [Google Scholar] [PubMed]
- Taneja, N.; Emmanuel, R.; Chari, P.; Sharma, M. A prospective study of hospital-acquired infections in burn patients at a tertiary care referral centre in North India. Burns 2004, 30, 665–669. [Google Scholar] [CrossRef]
- Foster, T.J. The Staphylococcus aureus “superbug”. J Clin Invest 2004, 114, 1693–1696. [Google Scholar] [CrossRef]
- Chatterjee, S.S.; Otto, M. Improved understanding of factors driving methicillin-resistant Staphylococcus aureus epidemic waves. Clin Epidemiol 2013, 5, 205–217. [Google Scholar]
- Voss, A.; Loeffen, F.; Bakker, J.; Klaassen, C.; Wulf, M. Methicillin-resistant Staphylococcus aureus in pig farming. Emerg Infect Dis 2005, 11, 1965–1966. [Google Scholar] [CrossRef] [PubMed]
- Alvarez, C.; Labarca, J.; Salles, M. Prevention strategies for methicillin-resistant Staphylococcus aureus (MRSA) in Latin America. Braz J Infect Dis 2010, 14 Suppl 2, S107–S108. [Google Scholar] [CrossRef]
- Clements, A.; Halton, K.; Graves, N.; et al. Overcrowding and understaffing in modern health-care systems: Key determinants in meticillin-resistant Staphylococcus aureus transmission. Lancet Infect Dis 2008, 8, 427–434. [Google Scholar] [CrossRef]
- Duerden, B.; Fry, C.; Johnson, A.P.; Wilcox, M.H. The control of methicillin-resistant Staphylococcus aureus blood stream infections in England. Open Forum Infect Dis 2015, 2, ofv035. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.R.; Cho, I.H.; Jeong, B.C.; Lee, S.H. Strategies to minimize antibiotic resistance. Int J Environ Res Public Health 2013, 10, 4274–4305. [Google Scholar] [CrossRef] [PubMed]
| Databases | Number of records |
|---|---|
| PubMed | 121 |
| Embase (OVID) | 261 |
| Cochrane | 13 |
| CINAHL Plus | 29 |
| Scopus | 57 |
© GERMS 2018.
Share and Cite
Khan, T.M.; Kok, Y.L.; Bukhsh, A.; Lee, L.-H.; Chan, K.-G.; Goh, B.-H. Incidence of Methicillin Resistant Staphylococcus aureus (MRSA) in Burn Intensive Care Unit: A Systematic Review. Germs 2018, 8, 113-125. https://doi.org/10.18683/germs.2018.1138
Khan TM, Kok YL, Bukhsh A, Lee L-H, Chan K-G, Goh B-H. Incidence of Methicillin Resistant Staphylococcus aureus (MRSA) in Burn Intensive Care Unit: A Systematic Review. Germs. 2018; 8(3):113-125. https://doi.org/10.18683/germs.2018.1138
Chicago/Turabian StyleKhan, Tahir Mehmood, Yee Leng Kok, Allah Bukhsh, Learn-Han Lee, Kok-Gan Chan, and Bey-Hing Goh. 2018. "Incidence of Methicillin Resistant Staphylococcus aureus (MRSA) in Burn Intensive Care Unit: A Systematic Review" Germs 8, no. 3: 113-125. https://doi.org/10.18683/germs.2018.1138
APA StyleKhan, T. M., Kok, Y. L., Bukhsh, A., Lee, L.-H., Chan, K.-G., & Goh, B.-H. (2018). Incidence of Methicillin Resistant Staphylococcus aureus (MRSA) in Burn Intensive Care Unit: A Systematic Review. Germs, 8(3), 113-125. https://doi.org/10.18683/germs.2018.1138




