The Heart Rate Variability Changes in Measles, HIV, and Sars-Cov-2 Infections; A Subtle Autonomic Involvement—A Pilot Study
Abstract
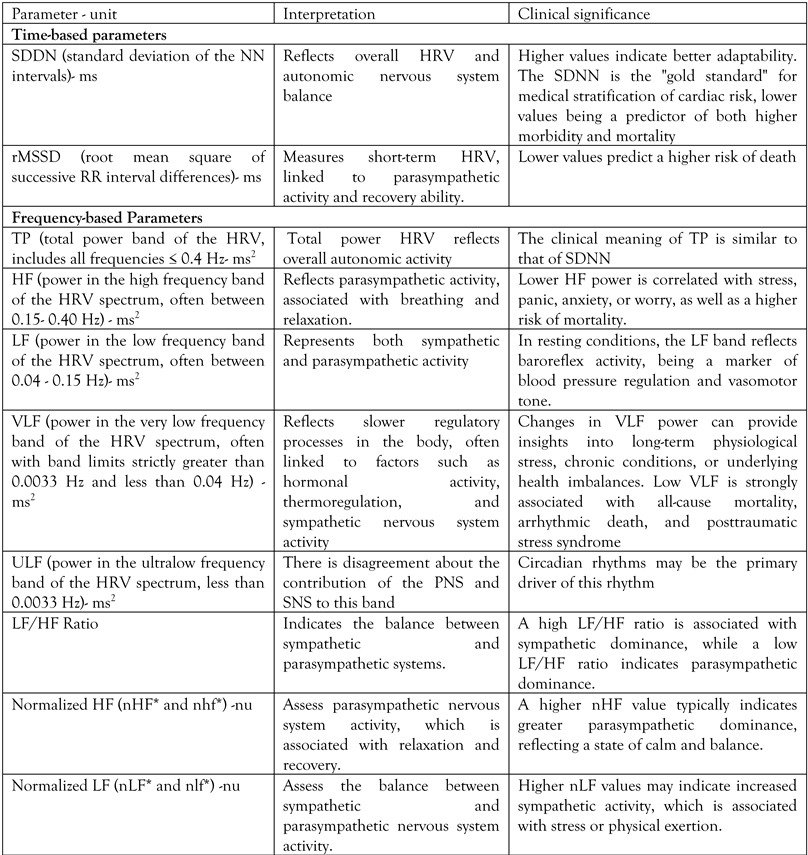
Introduction
Methods
Results
Discussion
Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Malik, M.; Hnatkova, K.; Huikuri, H.V.; Lombardi, F.; Schmidt, G.; Zabel, M. CrossTalk proposal: heart rate variability is a valid measure of cardiac autonomic responsiveness. J Physiol. 2019, 597, 2595–2598. [Google Scholar] [CrossRef]
- Buccelletti, E.; Gilardi, E.; Scaini, E.; et al. Heart rate variability and myocardial infarction: systematic literature review and metanalysis. Eur Rev Med Pharmacol Sci. 2009, 13, 299–307. [Google Scholar]
- Ling, N.; Li, C.L.; Wang, Z.Z.; Zhang, H.N.; Xu, H.; An, X.J. Heart rate variability in children with myocarditis presenting with ventricular arrhythmias. Eur Rev Med Pharmacol Sci. 2018, 22, 1102–1105. [Google Scholar] [PubMed]
- Bhati, P.; Alam, R.; Moiz, J.A.; Hussain, M.E. Subclinical inflammation and endothelial dysfunction are linked to cardiac autonomic neuropathy in type 2 diabetes. J Diabetes Metab Disord. 2019, 18, 419–428. [Google Scholar] [CrossRef]
- Rosas-Ballina, M.; Olofsson, P.S.; Ochani, M.; et al. Acetylcholine-synthesizing T cells relay neural signals in a vagus nerve circuit. Science. 2011, 334, 98–101. [Google Scholar] [CrossRef] [PubMed]
- Sharma, D.; Farrar, J.D. Adrenergic regulation of immune cell function and inflammation. Semin Immunopathol. 2020, 42, 709–717. [Google Scholar] [CrossRef]
- Milovanovic, B.; Djajic, V.; Bajic, D.; et al. Assessment of autonomic nervous system dysfunction in the early phase of infection with SARS-CoV-2 virus. Front Neurosci. 2021, 15, 640835. [Google Scholar] [CrossRef]
- Tsuji, H.; Venditti, F.J.; Manders, E.S.; et al. Reduced heart rate variability and mortality risk in an elderly cohort. The Framingham Heart Study. Circulation. 1994, 90, 878–883. [Google Scholar] [CrossRef]
- Tatsuo, H.; Ono, N.; Tanaka, K.; Yanagi, Y. SLAM (CDw150) is a cellular receptor for measles virus. Nature. 2000, 406, 893–897. [Google Scholar] [CrossRef]
- Blecharz-Lang, K.G.; Wagner, J.; Fries, A.; et al. Interleukin 6-mediated endothelial barrier disturbances can be attenuated by blockade of the IL6 receptor expressed in brain microvascular endothelial cells. Transl Stroke Res. 2018, 9, 631–642. [Google Scholar] [CrossRef] [PubMed]
- Nance, D.M.; Sanders, V.M. Autonomic innervation and regulation of the immune system (1987-2007). Brain Behav Immun. 2007, 21, 736–745. [Google Scholar] [CrossRef]
- Mueller, B.R.; Mehta, M.; Campbell, M.; et al. The autonomic nervous system (ANS)-immune network in people living with HIV. Res Sq [Preprint]. 2024, rs.3.rs5504909. [Google Scholar] [CrossRef]
- Kleiger, R.E.; Stein, P.K.; Bigger, J.T. Heart rate variability: measurement and clinical utility. Ann Noninvasive Electrocardiol Off J Int Soc Holter Noninvasive Electrocardiol Inc. 2005, 10, 88–101. [Google Scholar] [CrossRef]
- Koenig, J.; Thayer, J.F. Sex differences in healthy human heart rate variability: a meta-analysis. Neurosci Biobehav Rev. 2016, 64, 288–310. [Google Scholar] [CrossRef] [PubMed]
- Burr, R.L. Interpretation of normalized spectral heart rate variability indices in sleep research: a critical review. Sleep. 2007, 30, 913–919. [Google Scholar] [CrossRef]
- Rajendra Acharya, U.; Paul Joseph, K.; Kannathal, N.; Lim, C.M.; Suri, J.S. Heart rate variability: a review. Med Biol Eng Comput. 2006, 44, 1031–1051. [Google Scholar] [CrossRef] [PubMed]
- Shaffer, F.; McCraty, R.; Zerr, C.L. A healthy heart is not a metronome: an integrative review of the heart's anatomy and heart rate variability. Front Psychol. 2014, 5, 1040. [Google Scholar] [CrossRef] [PubMed]
- Umetani, K.; Singer, D.H.; McCraty, R.; Atkinson, M. Twenty-four hour time domain heart rate variability and heart rate: relations to age and gender over nine decades. J Am Coll Cardiol. 1998, 31, 593–601. [Google Scholar] [CrossRef]
- Penttilä, J.; Helminen, A.; Jartti, T.; et al. Time domain, geometrical and frequency domain analysis of cardiac vagal outflow: effects of various respiratory patterns. Clin Physiol Oxf Engl. 2001, 21, 365–376. [Google Scholar] [CrossRef]
- Ergun, U.; Demirci, M.; Nurlu, G.; Komürcü, F. Power spectral analysis of heart rate variability: normal values of subjects over 60 years old. Int J Neurosci. 2008, 118, 1165–1173. [Google Scholar] [CrossRef]
- Shaffer, F.; Ginsberg, J.P. An overview of heart rate variability metrics and norms. Front Public Health. 2017, 5, 258. [Google Scholar] [CrossRef] [PubMed]
- Kaliyaperumal, D.; Rk, K.; Alagesan, M.; Ramalingam, S. Characterization of cardiac autonomic function in COVID-19 using heart rate variability: a hospital based preliminary observational study. J Basic Clin Physiol Pharmacol. 2021, 32, 247–253. [Google Scholar] [CrossRef] [PubMed]
- Komaenthammasophon, C.; Pachinburavan, M.; Chokesuwattanaskul, R. Heart rate variability and mortality in critically ill COVID-19 pneumonia patients. Heliyon. 2024, 10, e34842. [Google Scholar] [CrossRef] [PubMed]
- Mittal, C.M.; Wig, N.; Mishra, S.; Deepak, K.K. Heart rate variability in human immunodeficiency virus-positive individuals. Int J Cardiol. 2004, 94, 1–6. [Google Scholar] [CrossRef]
- Riabokon, Y.Y.; Bilokobyla, S.O.; Riabokon, O.V. Clinical description of measles complications in adults in connection with changes in the functional state of the autonomic nervous system. Pathologia. 2019, 16, 339–344. [Google Scholar] [CrossRef]
 |
| Measles | SARS-CoV-2 | HIV | Control | |
|---|---|---|---|---|
| Number of patients | 9 | 8 | 8 | 8 |
| Age in years, median (IQR) | 46 (38.0-47.5) | 67 (63.5-73.0) | 46.50 (35.3-54.5) | 54.5 (41.0-70.8) |
| Male:female | 2:7 | 3:5 | 3:5 | 5:3 |
| High blood pressure, n (%) | 2, (22.2) | 6 (75.0) | 3 (37.5) | 2 (25.0) |
| Diabetes, n (%) | 0 (0.0) | 6 (62.5) | 2 (25.0) | 2 (25.0) |
| Heart failure, n (%) | 0 (0.0) | 4 (50.0) | 0 (0.0) | 3 (37.5) |
| Atrial fibrillation, n (%) | 0 (0.0) | 3 (37.5) | 0 (0.0) | 1 (12.5) |
| Ischemic heart disease, n (%) | 1 (12.5) | 3 (37.5) | 1 (12.5) | 2 (25.0) |
| CRP (mg/dL), median (IQR) | 21.6 (17.8-61.7) | 2.1 (1.4-11.6) | 2.1 (0.4-8.0) | 1.5 (0.6-3.9) |
| Fibrinogen (mg/dL), median (IQR) | 428.0 (376.5-509.0) | 463.0 (365.8-599.3) | 284.5 (237.0-381.8) | 319.0 (267.8-474.8) |
| Variables (median) (IQR) | Measles | p | SARS-CoV-2 | p | HIV | p | Control group |
| SDNN | 62.70 (33.10-65.55) | 0.217 | 114.00 (72.57-166.90) | 0.075 | 40.40 (28.80-102.90) | 0.486 | 64.80 (51.62-90.67) |
| rMSSD | 68.60 (31.55-81.50) | 0.161 | 157.65 (109.50-218.72) | 0,063 | 42.00 (23.40-134.60) | 0.441 | 76.60 (56.42-129.45) |
| TP | 318.70 (214.10-1493.75) | 0.817 | 3203,05 (1210.50-6503.37) | 0.042 | 493,85 (106.55-970.25) | 0.271 | 988.50 (283.05-1381.52) |
| HF | 98.00 (52.30-604.85) | 0.682 | 1470.60 (688.40-2923.15) | 0.036 | 45.70 (26.87-481.95) | 0.203 | 304.90 (78.52-703.80) |
| LF | 135.70 (51.65-488.05) | 0.824 | 1044.65 (315.25-2190.65) | 0.067 | 132.75 (25.20-305.47) | 0.234 | 344.45 (60,60-638,65) |
| VLF | 134.10 (82.10-346.70) | 0.835 | 588.60 (154.40-1185.6) | 0.046 | 109.90 (49.25-280.95) | 0.613 | 190.35 (57.57-259.70) |
| LF/HF | 0.90 (0.85-1.85) | 0.719 | 0.61 (0.49-0.85) | 0.172 | 0.90 (0.62-2.07) | 0.611 | 0.71 (0.39-2.12) |
| ULF | 11.80 (5.40-44.85) | 0.488 | 21.45 (8.15-272.12) | 0.206 | 9.40 (1.02-132.85) | 0.243 | 17.90 (3.35-26.50) |
| VLF+ULF | 134.20 (91.85-478.95) | 0.677 | 695.50 (162.55-1502.30) | 0.043 | 113.45 (53.20-412.12) | 0.994 | 204.45 (72.87-268.57) |
| HF+LF/TP | 0.70 (0.44-0.73) | 0.264 | 0.78 (0.75-0.84) | 0.636 | 0.53 (0.45-0.72) | 0.098 | 0.79 (0.54-0.86) |
| VLF/TP | 0.25 (0.23-0.45) | 0.232 | 0.17 (0.14-0.24) | 0.790 | 0.39 (0.18-5.35) | 0.114 | 0.19 (0.12-0.23) |
| VLF+ULF/TP | 0.27 (0.26-0.56) | 0.264 | 0.21 (0.15-0.25) | 0.637 | 0.47 (0.28-0.55) | 0.098 | 0.20 (0.14-0.46) |
| HF+LF/VLF+ULF | 2.38 (0.79-2.73) | 0.157 | 3.67 (3.07-5.57) | 0.985 | 1.12 (0.83-2.74) | 0.112 | 3.92 (1.45-6.07) |
| HF+LF/VLF | 2.75 (1.26-3.00) | 0.109 | 4.44 (3.12-5.95) | 0.895 | 0.53 (0.45-0.72) | 0.006 | 4.14 (2.37-7.16) |
| Variables (median) (IQR) | Measles | p | SARS-CoV-2 | p | HIV | p | Control group |
| nHF= HF/TP-VLF | 0.52 (0.32-0.54) | 0.353 | 0.56 (0.52-0.66) | 0.323 | 0.45 (0.32-0.59) | 0.294 | 0.57 (0.34-5.94) |
| nLF= LF/TP-VLF | 0.45 (0.43-0.51) | 0.442 | 0.36 (0.32-0.43) | 0.571 | 0.43 (0.38-0.48) | 0.711 | 0.40 (0,24-0,62) |
| nhf=HF/HF+LF | 0.53 (0.35-0.55) | 0.258 | 0.62 (0.54-0.67) | 0.531 | 0.53 (0.34-0.60) | 0.329 | 0.59 (0.37-0.73) |
| nlf=LF/HF+LF | 0.46 (0.44-0.64) | 0.255 | 0.38 (0.33-0.46) | 0.534 | 0.47 (0.39-0.66) | 0.326 | 0.41 (0.27-0.63) |
| Measles vs. HIV | Measles vs. SARS-CoV-2 | HIV vs. SARS-CoV-2 | |
|---|---|---|---|
| SDNN | 0.794 | 0.016 | 0.029 |
| rMSSD | 0.699 | 0.002 | 0.017 |
| TP | 0.445 | 0.021 | 0.018 |
| HF | 0.437 | 0.023 | 0.011 |
| LF | 0.424 | 0.056 | 0.023 |
| VLF | 0.502 | 0.052 | 0.035 |
| LF/HF | 0.775 | 0.026 | 0.120 |
| Ncoh | 0.120 | 0.140 | 0.022 |
| ULF | 0.773 | 0.369 | 0.471 |
| VLF+ULF | 0.703 | 0.056 | 0.044 |
| HF+LF/TP | 0.466 | 0.075 | 0.021 |
| VLF/TP | 0.601 | 0.097 | 0.039 |
| VLF+ULF/TP | 0.466 | 0.075 | 0.021 |
| HF+LF/VLF+ULF | 0.711 | 0.111 | 0.075 |
| HF+LF/VLF | 0.010 | 0.890 | 0.002 |
| nHF= HF/TP-VLF | 0.799 | 0.027 | 0.030 |
| nLF= LF/TP-VLF | 0.594 | 0.014 | 0.138 |
| nhf=HF/HF+LF | 0.980 | 0.013 | 0.042 |
| nlf=LF/HF+LF | 0.980 | 0.013 | 0.042 |
| HIV | Measles | SARS-CoV-2 | |||||
|---|---|---|---|---|---|---|---|
| Fibrinogen | CRP | Fibrinogen | CRP | Fibrinogen | CRP | ||
| SDNN | r | -0.598 | -0.266 | 0.147 | -0.156 | -0.358 | 0.300 |
| p | 0.118 | 0.524 | 0.706 | 0.688 | 0.383 | 0.470 | |
| rMSSD | r | -0.732 | -0.463 | -0.085 | -0.343 | -0.374 | 0.149 |
| p | 0.039 | 0.248 | 0.827 | 0.366 | 0.362 | 0.724 | |
| TP | r | -0.335 | -0.002 | -0.160 | -0.122 | -0.148 | 0.278 |
| p | 0.418 | 0.996 | 0.681 | 0.755 | 0.726 | 0.504 | |
| HF | r | -0.628 | -0.342 | -0.221 | -0.195 | -0.177 | 0.193 |
| p | 0.096 | 0.407 | 0.567 | 0.614 | 0.674 | 0.646 | |
| LF | r | -0.339 | -0.099 | -0.137 | -0.151 | -0.146 | 0.422 |
| p | 0.412 | 0.815 | 0.726 | 0.698 | 0.731 | 0.298 | |
| VLF | r | 0.253 | 0.649 | -0.121 | 0.069 | -0.098 | 0.049 |
| p | 0.546 | 0.081 | 0.757 | 0.860 | 0.817 | 0.909 | |
| LF/HF | r | 0.767 | 0.955 | 0.793 | 0.576 | 0.163 | 0.497 |
| p | 0.026 | <0.001 | 0.011 | 0.104 | 0.701 | 0.210 | |
| ULF | r | 0.085 | 0.286 | 0.278 | 0.387 | -0.003 | 0.682 |
| p | 0.841 | 0.492 | 0.469 | 0.304 | 0.994 | 0.062 | |
| VLF+ULF | r | 0.207 | 0.558 | 0.015 | 0.215 | -0.087 | 0.213 |
| p | 0.622 | 0.151 | 0.969 | 0.578 | 0.838 | 0.613 | |
| HF+LF/TP | r | -0.702 | -0.601 | -0.314 | -0.607 | -0.654 | -0.237 |
| p | 0.052 | 0.115 | 0.410 | 0.083 | 0.079 | 0.573 | |
| VLF/TP | r | 0.718 | 0.502 | 0.163 | 0.406 | 0.605 | 0.053 |
| p | 0.045 | 0.205 | 0.675 | 0.278 | 0.112 | 0.901 | |
| VLF+ULF/TP | r | 0.702 | 0.601 | 0.314 | 0.607 | 0.654 | 0.237 |
| p | 0.052 | 0.115 | 0.410 | 0.083 | 0.079 | 0.573 | |
| HF+LF/VLF+ULF | r | -0.689 | -0.371 | -0.303 | -0.448 | -0.417 | -0.248 |
| p | 0.059 | 0.366 | 0.428 | 0.227 | 0.304 | 0.554 | |
| HF+LF/VLF | r | -0.702 | -0.601 | -0.273 | -0.414 | -0.445 | -0.045 |
| p | 0.052 | 0.115 | 0.478 | 0.268 | 0.269 | 0.915 | |
| nHF= HF/TP-VLF | r | -0.682 | -0.834 | -0.722 | -0.669 | -0.453 | -0.642 |
| p | 0.062 | 0.010 | 0.028 | 0.049 | 0.260 | 0.086 | |
| nLF= LF/TP-VLF | r | 0.609 | 0.440 | 0.781 | 0.329 | -0.007 | 0.292 |
| p | 0.109 | 0.276 | 0.013 | 0.388 | 0.986 | 0.482 | |
| nhf=HF/HF+LF | r | -0.786 | -0.902 | -0.797 | -0.624 | -0.186 | -0.493 |
| p | 0.021 | 0.002 | 0.010 | 0.073 | 0.658 | 0.215 | |
| nlf=LF/HF+LF | r | 0.786 | 0.992 | 0.797 | 0.626 | 0.186 | 0.493 |
| p | 0.021 | 0.002 | 0.010 | 0.073 | 0.658 | 0.215 | |
© GERMS 2025.
Share and Cite
Savulescu-Fiedler, I.; Deaconu, T.; Siliste, R.; Homentcovschi, C.; Gurghean, A.; Toader, I.; Benea, S. The Heart Rate Variability Changes in Measles, HIV, and Sars-Cov-2 Infections; A Subtle Autonomic Involvement—A Pilot Study. GERMS 2025, 15, 104-115. https://doi.org/10.18683/germs.2025.1460
Savulescu-Fiedler I, Deaconu T, Siliste R, Homentcovschi C, Gurghean A, Toader I, Benea S. The Heart Rate Variability Changes in Measles, HIV, and Sars-Cov-2 Infections; A Subtle Autonomic Involvement—A Pilot Study. GERMS. 2025; 15(2):104-115. https://doi.org/10.18683/germs.2025.1460
Chicago/Turabian StyleSavulescu-Fiedler, Ilinca, Teodora Deaconu, Roxana Siliste, Corina Homentcovschi, Adriana Gurghean, Ioana Toader, and Serban Benea. 2025. "The Heart Rate Variability Changes in Measles, HIV, and Sars-Cov-2 Infections; A Subtle Autonomic Involvement—A Pilot Study" GERMS 15, no. 2: 104-115. https://doi.org/10.18683/germs.2025.1460
APA StyleSavulescu-Fiedler, I., Deaconu, T., Siliste, R., Homentcovschi, C., Gurghean, A., Toader, I., & Benea, S. (2025). The Heart Rate Variability Changes in Measles, HIV, and Sars-Cov-2 Infections; A Subtle Autonomic Involvement—A Pilot Study. GERMS, 15(2), 104-115. https://doi.org/10.18683/germs.2025.1460




