HPV Vaccine-Related Myths Encountered in Romanian Clinical Practice: A Cross-Sectional Survey of Family Doctors
Abstract
Introduction
Methods
Study design
Statistical analysis
Ethics considerations
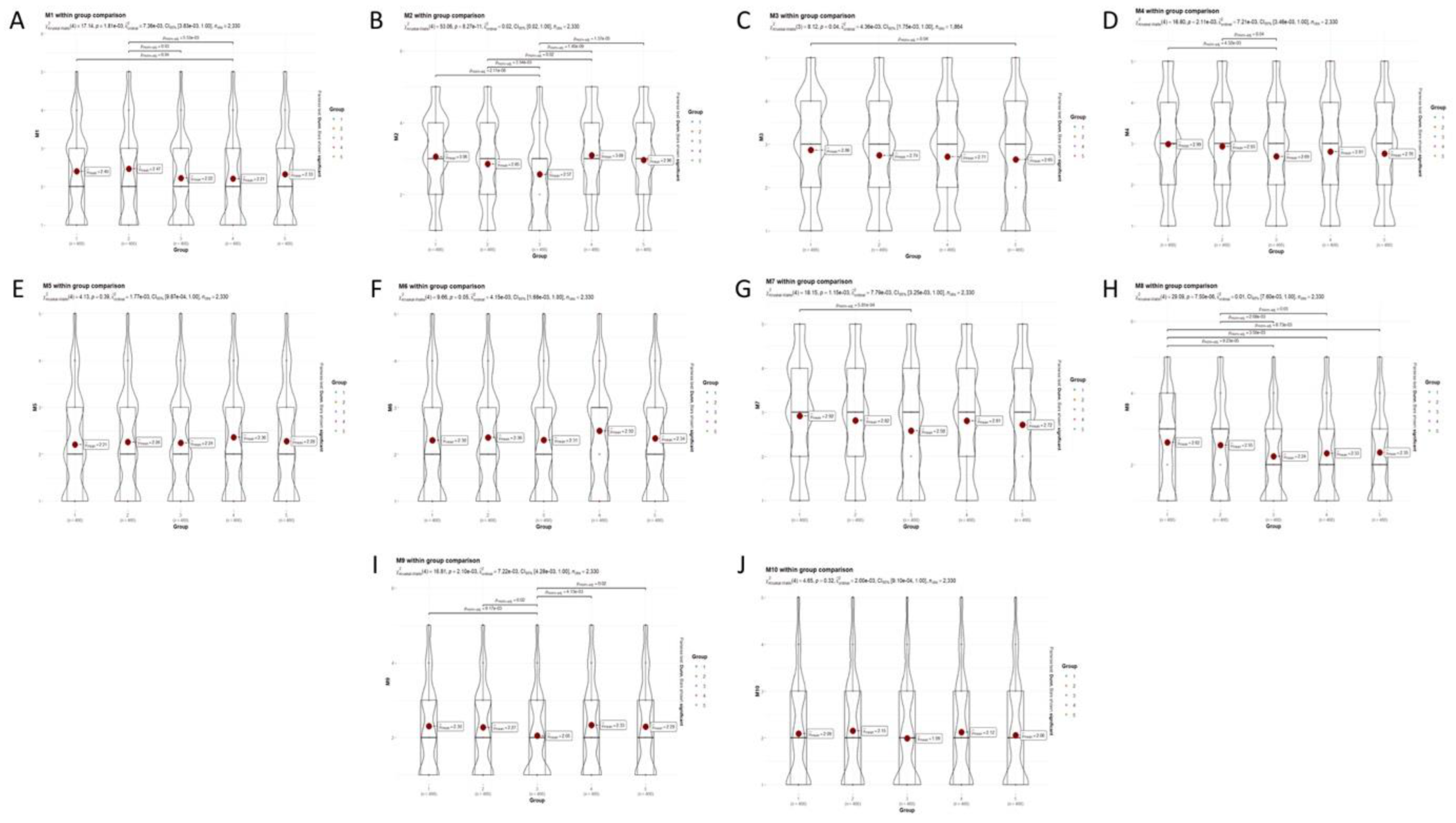
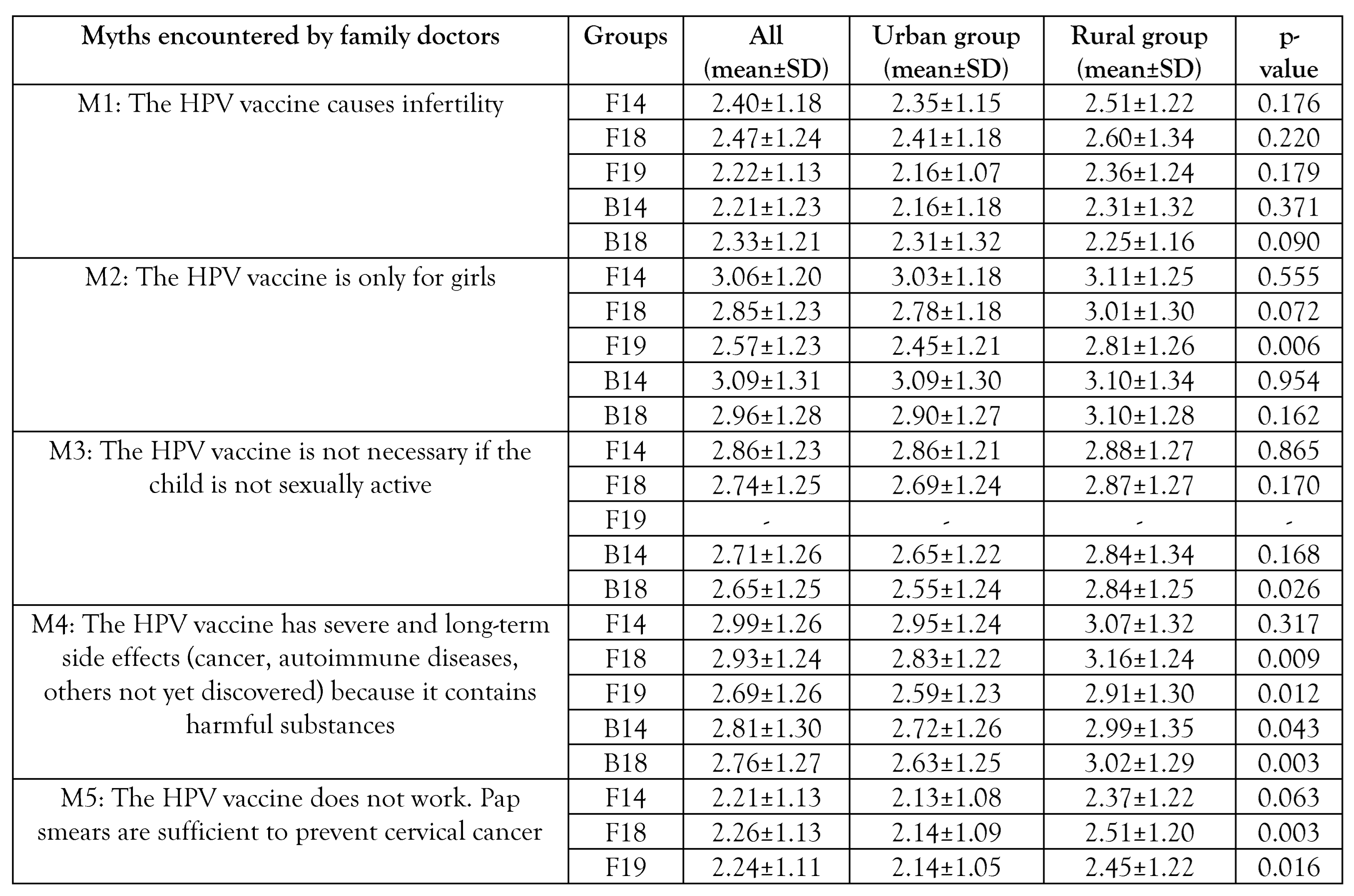
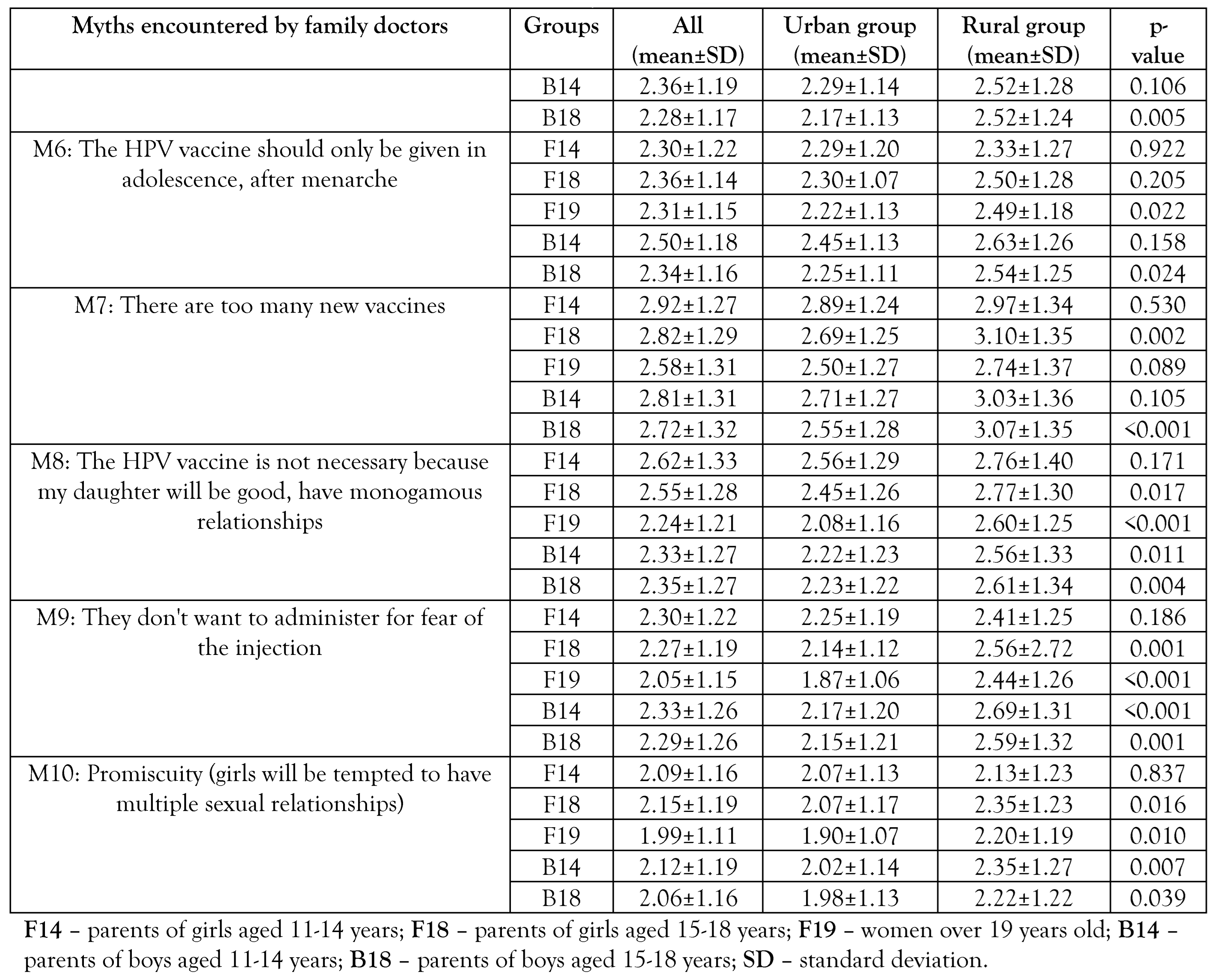
Results
Participants
Discussion
Vaccine safety
Vaccine effectiveness
Behavior consequences
Communication
Limitations
Generalizability
Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- ICO/IARC Information Centre on HPV and Cancer. Romania Human Papillomavirus and Related Cancers, Fact Sheet 2023. Available online: https://hpvcentre.net/statistics/reports/ROU_FS.pdf (accessed on 22 February 2025).
- Institutul Național de Sănătate Publică. Raport privind evolutia vaccinarii impotriva HPV 2024. Available online: https://insp.gov.ro/centrul-national-de-supraveghere-si-control-al-bolilor-transmisibile-cnscbt/analiza-date-supraveghere/ (accessed on 22 February 2025).
- Furtunescu, F.; Bohiltea, R.E.; Neacsu, A.; et al. Cervical cancer mortality in Romania: trends, regional and rural-urban inequalities, and policy implications. Medicina (Kaunas) 2021, 58, 18. [Google Scholar] [CrossRef]
- Brisson, M.; Drolet, M. Global elimination of cervical cancer as a public health problem. Lancet Oncol. 2019, 20, 319–321. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global strategy to accelerate the elimination of cervical cancer as a public health problem. Available online: https://www.who.int/publications/i/item/9789240014107 (accessed on day month year).
- Simion, L.; Rotaru, V.; Cirimbei, C.; et al. Inequities in screening and HPV vaccination programs and their impact on cervical cancer statistics in Romania. Diagnostics (Basel). 2023, 13, 2776. [Google Scholar] [CrossRef]
- Todor, R.D.; Bratucu, G.; Moga, M.A.; Candrea, A.N.; Marceanu, L.G.; Anastasiu, C.V. Challenges in the prevention of cervical cancer in Romania. Int J Environ Res Public Health. 2021, 18, 1721. [Google Scholar] [CrossRef]
- Voidăzan, S.; Tarcea, M.; Morariu, S.H.; Grigore, A.; Dobreanu, M. Human papillomavirus vaccine - knowledge and attitudes among parents of children aged 10-14 years: a cross-sectional study, Tîrgu Mureş, Romania. Cent Eur J Public Health. 2016, 24, 29–38. [Google Scholar] [CrossRef]
- Ministry of Health. Comunicat de presă Ministerul Sănătăţii demarează campania de informare pentru prevenirea prin vaccinare a cancerului de col uterin. Available online: https://old.ms.ro/index.php?pag=62&id=6683&pg=1 (accessed on 22 February 2025).
- Stefanopol, I.A.; Baroiu, L.; Chirila, S.; et al. The influence of living in rural areas on the evolution and management of pediatric ovarian cystic lesions: a retrospective study on a cohort from South Eastern Romania. Int J Gen Med. 2022, 15, 5273–5284. [Google Scholar] [CrossRef]
- Manolescu, L.S.C.; Zugravu, C.; Zaharia, C.N.; et al. Barriers and facilitators of Romanian HPV (human papillomavirus) vaccination. Vaccines (Basel). 2022, 10, 1722. [Google Scholar] [CrossRef]
- Voidăzan, T.S.; Budianu, M.A.; Rozsnyai, F.F.; Kovacs, Z.; Uzun, C.C.; Neagu, N. Assessing the level of knowledge, beliefs and acceptance of HPV vaccine: a cross-sectional study in Romania. Int J Environ Res Public Health. 2022, 19, 6939. [Google Scholar] [CrossRef]
- Penţa, M.A.; Băban, A. Dangerous agent or saviour? HPV vaccine representations on online discussion forums in Romania. Int J Behav Med. 2014, 21, 20–28. [Google Scholar] [CrossRef]
- Penţa, M.A.; Băban, A. Mass media coverage of HPV vaccination in Romania: a content analysis. Health Educ Res. 2014, 29, 977–992. [Google Scholar] [CrossRef] [PubMed]
- Turcu-Stiolica, A.; Boicea, A.R.; Nechita, F.; et al. Development and validation of a questionnaire to measure COVID-19 vaccine hesitancy within the Romanian industrial laborers. Front Public Health. 2025, 13, 1482778. [Google Scholar] [CrossRef]
- Dumitra, G.G.; Alexiu, S.A.; Sănduțu, D.; et al. Segmenting attitudes toward vaccination –behavioral insights into influenza vaccination refusal in Romania. Germs. 2024, 14, 362–374. [Google Scholar] [CrossRef]
- Dascalu, S.; Geambasu, O.; Covaciu, O.; et al. Prospects of COVID-19 vaccination in Romania: challenges and potential solutions. Front Public Health. 2021, 9, 644538. [Google Scholar] [CrossRef]
- Dube, E.; Pistol, A.; Stanescu, A.; et al. Vaccination barriers and drivers in Romania: a focused ethnographic study. Eur J Public Health. 2023, 33, 222–227. [Google Scholar] [CrossRef] [PubMed]
- Societatea Națională de Medicina Familiei. Comunicat de presă - Atitudinea populației față de vaccinuri și vaccinare - Sondaj privind vaccinarea. Available online: https://snmf.ro/2019/03/10/atitudinea-populatiei-fata-de-vaccinuri-si-vaccinare-sondaj-de-opinie-inscop-research/ (accessed on 15 September 2024).
- Achimaș-Cadariu, T.; Pașca, A.; Jiboc, N.M.; Puia, A.; Dumitrașcu, D.L. Vaccine hesitancy among European parents-psychological and social factors influencing the decision to vaccinate against HPV: a systematic review and meta-analysis. Vaccines (Basel). 2024, 12, 127. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health. Ordin nr. 3120 din 12 septembrie 2023 pentru aprobarea segmentelor populaționale care beneficiază de prescrierea, eliberarea și decontarea în regim de compensare a medicamentelor imunologice folosite pentru producerea imunității active sau folosite pentru prevenirea unor boli transmisibile. Available online: https://legislatie.just.ro/public/DetaliiDocument/274488 (accessed on 2 February 2025).
- Ministerul Sănătății România. Ordin nr. 3278/804/2023 privind completarea anexei nr. 1 la ordinul ministrului sănătății și al președintelui Casei Naționale de Asigurări de Sănătate nr. 564/499/2021 pentru aprobarea protocoalelor terapeutice. Monitorul Oficial. Available online: https://legislatie.just.ro/Public/DetaliiDocument/274834 (accessed on 17 July 2024).
- Guvernul României. Hotărâre privind aprobarea strategiei nationale de vaccinare 2023-2030. Available online: https://sgglegis.gov.ro/legislativ/docs/2023/08/g63hp1tcrwfb8s02dv5m.pdf (accessed on 30 August 2024).
- Institutul Român pentru Evaluare și Strategie. Percepții, atitudini și comportamente cu privire la vaccinarea COVID-19 - sondaj de opinie septembrie 2021. Available online: https://ires.ro/uploads/articole/ires_pac_vaccinare-covid-19_sondaj-national_sept-2021_romania-curata_prezentare.pdf (accessed on 23 February 2025).
- Casa Națională de Asigurări de Sănătate, Raport de activitate ianuarie-decembrie 2023. Available online: https://cnas.ro/wp-content/uploads/2024/10/Raport-de-activitate-al-CNAS-pentru-anul-2023.pdf (accessed on 1 March 2025).
- Bednarczyk, R.A. Addressing HPV vaccine myths: practical information for healthcare providers. Hum Vaccin Immunother. 2019, 15, 1628–1638. [Google Scholar] [CrossRef]
- Zimet, G.D.; Rosberger, Z.; Fisher, W.A.; Perez, S.; Stupiansky, N.W. Beliefs, behaviors and HPV vaccine: correcting the myths and the misinformation. Prev Med. 2013, 57, 414–418. [Google Scholar] [CrossRef] [PubMed]
- Schuler, C.L.; Hanley, C.J.; Coyne-Beasley, T. Misconception: human papillomavirus vaccine and infertility. Clin Pediatr (Phila). 2014, 53, 158–165. [Google Scholar] [CrossRef]
- Levy, M.S.; Hunt, K.N.; Rinehart, S.; et al. COVID-19 vaccine information and infertility posts on X: insights on a misinformation pandemic. Perm J. 2024, 28, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Berkowitz, H.E.; Vann, J.C.J. Strategies to address COVID-19 vaccine and pregnancy myths. MCN Am J Matern Child Nurs. 2023, 48, 215–223. [Google Scholar] [CrossRef]
- Schmuhl, N.B.; Mooney, K.E.; Zhang, X.; Cooney, L.G.; Conway, J.H.; LoConte, N.K. No association between HPV vaccination and infertility in U.S. females 18-33 years old. Vaccine. 2020, 38, 4038–4043. [Google Scholar] [CrossRef]
- Dempsey, A.F.; Butchart, A.; Singer, D.; Clark, S.; Davis, M. Factors associated with parental intentions for male human papillomavirus vaccination: results of a national survey. Sex Transm Dis. 2011, 38, 769–776. [Google Scholar] [CrossRef] [PubMed]
- Muscianisi, F.; Foresta, C.; Garolla, A. Role of HPV vaccination for prevention of male infertility. Minerva Endocrinol (Torino). 2022, 47, 70–76. [Google Scholar] [CrossRef]
- Angelo, M.G.; David, M.P.; Zima, J.; et al. Pooled analysis of large and long-term safety data from the human papillomavirus-16/18-AS04-adjuvanted vaccine clinical trial programme. Pharmacoepidemiol Drug Saf. 2014, 23, 466–479. [Google Scholar] [CrossRef]
- Lu, B.; Kumar, A.; Castellsagué, X.; Giuliano, A.R. Efficacy and safety of prophylactic vaccines against cervical HPV infection and diseases among women: a systematic review & meta-analysis. BMC Infect Dis. 2011, 11, 13. [Google Scholar] [CrossRef]
- Joshi, J.; Das, M.K.; Polpakara, D.; Aneja, S.; Agarwal, M.; Arora, N.K. Vaccine Safety and Surveillance for Adverse Events Following Immunization (AEFI) in India. Indian J Pediatr. 2018, 85, 139–148. [Google Scholar] [CrossRef] [PubMed]
- Dey, A.; Wang, H.; Quinn, H.; et al. Surveillance of adverse events following immunisation in Australia: annual report, 2018. Commun Dis Intell. 2020, 44, 1–28. [Google Scholar] [CrossRef]
- Guo, B.; Page, A.; Wang, H.; Taylor, R.; McIntyre, P. Systematic review of reporting rates of adverse events following immunization: an international comparison of post-marketing surveillance programs with reference to China. Vaccine. 2013, 31, 603–617. [Google Scholar] [CrossRef]
- Dey, A.; Wang, H.; Quinn, H.; et al. Surveillance of adverse events following immunisation in Australia annual report, 2017. Commun Dis Intell. 2019, 43, 1–28. [Google Scholar] [CrossRef]
- Bonanni, P.; Zanella, B.; Santomauro, F.; Lorini, C.; Bechini, A.; Boccalini, S. Safety and perception: what are the greatest enemies of HPV vaccination programmes? Vaccine. 2018, 36, 5424–5429. [Google Scholar] [CrossRef]
- Turki, Y.M.; Alqurashi, J. Knowledge, attitudes, and perceptions towards human papillomavirus (HPV) vaccination among adult women in primary health care centers in Makkah, Saudi Arabia. Cureus. 2023, 15, e44157. [Google Scholar] [CrossRef]
- Offit, P.A.; Quarles, J.; Gerber, M.A.; et al. Addressing parents' concerns: do multiple vaccines overwhelm or weaken the infant's immune system? Pediatrics. 2002, 109, 124–129. [Google Scholar] [CrossRef]
- Chan, J.Y.K.; Cheung, M.K.; Lan, L.; et al. Characterization of oral microbiota in HPV and non-HPV head and neck squamous cell carcinoma and its association with patient outcomes. Oral Oncol. 2022, 135, 106245. [Google Scholar] [CrossRef]
- 44. Constantin, M.; Chifiriuc, M.C.; Mihaescu, G.; et al. Implications of oral dysbiosis and HPV infection in head and neck cancer: from molecular and cellular mechanisms to early diagnosis and therapy. Front Oncol. 2023, 13, 1273516. [Google Scholar] [CrossRef]
- Alemany, L.; Cubilla, A.; Halec, G.; et al. Role of human papillomavirus in penile carcinomas worldwide. Eur Urol. 2016, 69, 953–961. [Google Scholar] [CrossRef] [PubMed]
- Iorga, L.; Marcu, D.R.; Diaconu, C.C.; et al. Penile carcinoma and HPV infection (Review). Exp Ther Med. 2020, 20, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Miralles-Guri, C.; Bruni, L.; Cubilla, A.L.; Castellsagué, X.; Bosch, F.X.; de Sanjosé, S. Human papillomavirus prevalence and type distribution in penile carcinoma. J Clin Pathol. 2009, 62, 870–878. [Google Scholar] [CrossRef]
- Șandru, F.; Radu, A.M.; Petca, A.; Dumitrașcu, M.C.; Petca, R.C.; Roman, AM. Unveiling the therapeutic horizon: HPV vaccines and their impact on cutaneous diseases-a comprehensive review. Vaccines (Basel). 2024, 12, 228. [Google Scholar] [CrossRef] [PubMed]
- Pham, C.T.; Juhasz, M.; Sung, C.T.; Mesinkovska, N.A. The human papillomavirus vaccine as a treatment for human papillomavirus-related dysplastic and neoplastic conditions: a literature review. J Am Acad Dermatol. 2020, 82, 202–212. [Google Scholar] [CrossRef]
- Ng, S.S.; Hutubessy, R.; Chaiyakunapruk, N. Systematic review of cost-effectiveness studies of human papillomavirus (HPV) vaccination: 9-valent vaccine, gender-neutral and multiple age cohort vaccination. Vaccine. 2018, 36, 2529–2544. [Google Scholar] [CrossRef]
- Colzani, E.; Johansen, K.; Johnson, H.; Pastore Celentano, L. Human papillomavirus vaccination in the European Union/European Economic Area and globally: a moral dilemma. Euro Surveill. 2021, 26, 2001659. [Google Scholar] [CrossRef]
- Jentschke, M.; Kampers, J.; Becker, J.; Sibbertsen, P.; Hillemanns, P. Prophylactic HPV vaccination after conization: a systematic review and meta-analysis. Vaccine. 2020, 38, 6402–6409. [Google Scholar] [CrossRef]
- Baisley, K.; Kemp, T.J.; Mugo, N.R.; et al. Comparing one dose of HPV vaccine in girls aged 9-14 years in Tanzania (DoRIS) with one dose in young women aged 15-20 years in Kenya (KEN SHE): an immunobridging analysis of randomised controlled trials. Lancet Glob Health. 2024, 12, e491–e499. [Google Scholar] [CrossRef]
- Seyferth, E.R.; Bratic, J.S.; Bocchini, J.A., Jr. Human papillomavirus epidemiology and vaccine recommendations: selected review of the recent literature. Curr Opin Pediatr. 2016, 28, 400–406. [Google Scholar] [CrossRef] [PubMed]
- Valentino, K.; Poronsky, C.B. Human papillomavirus infection and vaccination. J Pediatr Nurs. 2016, 31, e155–e166. [Google Scholar] [CrossRef] [PubMed]
- Pagina de Psihologie. În România, 22,5% dintre adolescenți au primul contact sexual înainte de 15 ani, iar 11,8% prima naștere. Interviu cu Gabriel Brumariu (2022). Available online: https://www.paginadepsihologie.ro/in-romania-225-dintre-adolescenti-au-primul-contact-sexual-inainte-de-15-ani-iar-118-prima-nastere-interviu-cu-gabriel-brumariu/?srsltid=AfmBOorUq3LWVaT6AsciaqGbWaBLpmUAXc7wUIe3UZ_hJDhVCwBoSraV (accessed on 1 March 2025).
- Libertatea. Studiu: La ce vârstă își încep copiii români viața sexuală. Available online: https://www.libertatea.ro/stiri/studiu-la-ce-varsta-isi-incep-copiii-romani-viata-sexuala-1166420 (accessed on 1 March 2025).
- Simion, L.; Rotaru, V.; Cirimbei, C.; et al. Inequities in screening and HPV vaccination programs and their impact on cervical cancer statistics in Romania. Diagnostics (Basel). 2023, 13, 2776. [Google Scholar] [CrossRef]
- Ministry of Health. Planul Național de Combatere și Control al Cancerului. Comisia Multidisciplinară de Oncologie (2023). Available online: https://www.ms.ro/media/documents/Planul_Național_de_Combatere_și_Control_al_Cancerului_RIQiTXG.pdf (accessed on 28 February 2025).
- Gavillon, N.; Vervaet, H.; Derniaux, E.; Terrosi, P.; Graesslin, O.; Quereux, C. Papillomavirus humain (HPV): comment ai-je attrapé ça? [How did I contract human papillomavirus (HPV)?]. Gynecol Obstet Fertil. 2010, 38, 199–204. [Google Scholar] [CrossRef]
- Brouwer, A.F.; Meza, R.; Eisenberg, M.C. Transmission heterogeneity and autoinoculation in a multisite infection model of HPV. Math Biosci. 2015, 270 Pt A, 115–125. [Google Scholar] [CrossRef]
- Kero, K.; Rautava, J. HPV infections in heterosexual couples: mechanisms and covariates of virus transmission. Acta Cytol. 2019, 63, 143–147. [Google Scholar] [CrossRef]
- Sethi, S.; Ju, X.; Antonsson, A.; et al. Oral HPV infection among Indigenous Australians; incidence, persistence, and clearance at 12-month follow-up. Cancer Epidemiol Biomarkers Prev. 2022, 31, 604–613. [Google Scholar] [CrossRef] [PubMed]
- Wei, F.; Gaisa, M.M.; D'Souza, G.; et al. Epidemiology of anal human papillomavirus infection and high-grade squamous intraepithelial lesions in 29 900 men according to HIV status, sexuality, and age: a collaborative pooled analysis of 64 studies. Lancet HIV. 2021, 8, e531–e543. [Google Scholar] [CrossRef]
- Donken, R.; Ogilvie, G.S.; Bettinger, J.A.; Sadarangani, M.; Goldman, R.D. Effect of human papillomavirus vaccination on sexual behaviour among young females. Can Fam Physician. 2018, 64, 509–513. [Google Scholar]
- Rysavy, M.B.; Kresowik, J.D.; Liu, D.; Mains, L.; Lessard, M.; Ryan, G.L. Human papillomavirus vaccination and sexual behavior in young women. J Pediatr Adolesc Gynecol. 2014, 27, 67–71. [Google Scholar] [CrossRef] [PubMed]
- Vázquez-Otero, C.; Thompson, E.L.; Daley, E.M.; Griner, S.B.; Logan, R.; Vamos, C.A. Dispelling the myth: exploring associations between the HPV vaccine and inconsistent condom use among college students. Prev Med. 2016, 93, 147–150. [Google Scholar] [CrossRef]
- Stupiansky, N.W.; Zimet, G.D. Chapter 11 - STD vaccine acceptability in sexually transmitted diseases. In Sexually Transmitted Diseases, 2nd ed.; Stanberry, L.R., Rosenthal, S.L., Eds.; Academic Press, 2013; pp. 251–269. [Google Scholar] [CrossRef]
- Kunitoki, K.; Funato, M.; Mitsunami, M.; Kinoshita, T.; Reich, M.R. Access to HPV vaccination in Japan: increasing social trust to regain vaccine confidence. Vaccine. 2021, 39, 6104–6110. [Google Scholar] [CrossRef]
- Mundagowa, P.T.; Vora, S.; Seck, F.; Dhankhode, N.; Sakyi, K.S.; Kanyangarara, M. Exploring the views of barbers and stylists on the acceptability of delivering community-based interventions to promote COVID-19 testing and vaccination in South Carolina. Vaccines (Basel). 2024, 12, 1011. [Google Scholar] [CrossRef]
- Surugiu, R.; Iancu, M.A.; Lăcătus, A.M.; et al. Unveiling the presence of social prescribing in Romania in the context of sustainable healthcare—a scoping review. Sustainability. 2023, 15, 11652. [Google Scholar] [CrossRef]
- Gagneur, A. Motivational interviewing: a powerful tool to address vaccine hesitancy. Can Commun Dis Rep. 2020, 46, 93–97. [Google Scholar] [CrossRef] [PubMed]
- Gagneur, A.; Lemaître, T.; Gosselin, V.; et al. A postpartum vaccination promotion intervention using motivational interviewing techniques improves short-term vaccine coverage: PromoVac study. BMC Public Health. 2018, 18, 811. [Google Scholar] [CrossRef] [PubMed]
 |
  |
© GERMS 2025.
Share and Cite
Dumitra, G.G.; Dogaru, C.-A.; Alexiu, S.A.; Sănduţu, D.; Berbecel, C.; Curelea, M.; Barbu, C.V.; Deleanu, A.; Grom, A.; Lup, M.; et al. HPV Vaccine-Related Myths Encountered in Romanian Clinical Practice: A Cross-Sectional Survey of Family Doctors. Germs 2025, 15, 37-55. https://doi.org/10.18683/germs.2025.1453
Dumitra GG, Dogaru C-A, Alexiu SA, Sănduţu D, Berbecel C, Curelea M, Barbu CV, Deleanu A, Grom A, Lup M, et al. HPV Vaccine-Related Myths Encountered in Romanian Clinical Practice: A Cross-Sectional Survey of Family Doctors. Germs. 2025; 15(1):37-55. https://doi.org/10.18683/germs.2025.1453
Chicago/Turabian StyleDumitra, Gheorghe Gindrovel, Carmen-Adriana Dogaru, Sandra Adalgiza Alexiu, Dorica Sănduţu, Cosmina Berbecel, Monica Curelea, Cristina Vasilica Barbu, Anca Deleanu, Adrian Grom, Maria Lup, and et al. 2025. "HPV Vaccine-Related Myths Encountered in Romanian Clinical Practice: A Cross-Sectional Survey of Family Doctors" Germs 15, no. 1: 37-55. https://doi.org/10.18683/germs.2025.1453
APA StyleDumitra, G. G., Dogaru, C.-A., Alexiu, S. A., Sănduţu, D., Berbecel, C., Curelea, M., Barbu, C. V., Deleanu, A., Grom, A., Lup, M., Budiu, I., Vesa, M., Proşa, F., Ştefănescu, D., Surugiu, R., Popescu, Ş. O., Lăcătuş, A., Iancu, M. A., & Turcu-Stiolica, A. (2025). HPV Vaccine-Related Myths Encountered in Romanian Clinical Practice: A Cross-Sectional Survey of Family Doctors. Germs, 15(1), 37-55. https://doi.org/10.18683/germs.2025.1453





