Abstract
Introduction: Bordetella bronchiseptica is a rare cause of hemorrhagic bronchopneumonia. Important to the clinician is a clear understanding that the treatment of this rare organism differs greatly from the successful antibiotic treatment of the more common Bordetella species, pertussis and parapertussis. Case report: A 64-year-old female presented to the emergency department after experiencing one week of worsening hemoptysis. Upon admission, she was afebrile and all initial laboratory test results were normal. Bronchoalveolar hemorrhage suggested by radiographic imaging was confirmed by bronchoscopy. Bronchoalveolar lavage (BAL) cultures contained unspeciated Bordetella. Rapid worsening of the hemoptysis led to intubation and the decision to perform bronchial artery embolization. However, the intensity of the hemoptysis persisted. Septic shock ensued despite treatment with broad spectrum antibiotics including azithromycin, vancomycin, and cefepime. The microbiological speciation results finalized shortly after the patient’s death. The identified organism was B. bronchiseptica. Conclusions: Although macrolide antibiotics are first line treatment for B. pertussis and parapertussis, macrolide antibiotics are generally not effective against B. bronchiseptica. Clinical suspicion of B. bronchiseptica infection should prompt consideration of alternative antibiotics known to be effective against this rare species, including carbapenems and fluoroquinolones. The use of these latter antibiotics may advisably be considered as an empirical treatment during the delay of microbiological speciation.
Introduction
The Bordetella genus comprises several species, two of which, pertussis and parapertussis, are well-known for causing whooping cough. [1] The other species rarely cause human infection. B. bronchiseptica is primarily considered a zoonotic pathogen, causing respiratory illness in cats, dogs and pigs. [2,3] Transmission to humans occurs through contact with saliva or mucus of these animals, although a history of animal contact is not always present. Human respiratory illness is very rare and typically limited to severely debilitated and/or immunocompromised patients (i.e., patients with AIDS). [4,5] The unfamiliarity of this organism as a cause of human infection may result in dismissal of its clinical relevance when identified in culture. We report a case of B. bronchiseptica pneumonia presenting as hemoptysis that rapidly progressed to fatal diffuse pulmonary hemorrhage and septicemia.
Case report
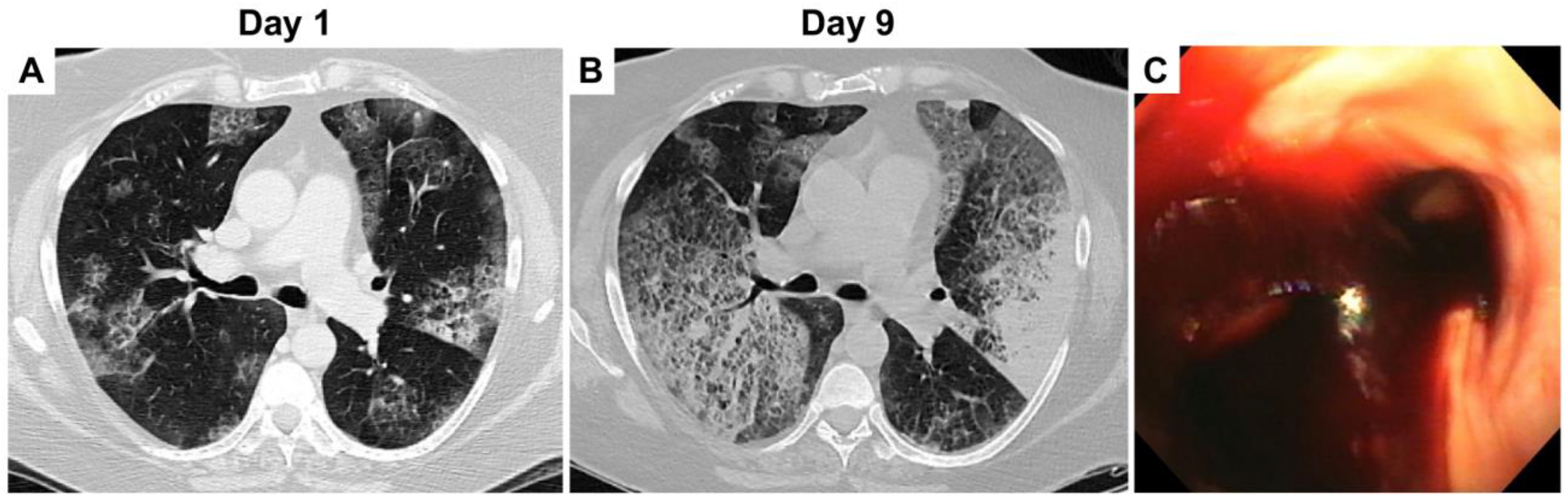
A 64-year-old female with moderate chronic obstructive pulmonary disease (COPD) was treated by her primary care provider with a 5-day-course of azithromycin for one week of hemoptysis. Persistent hemoptysis despite outpatient antibiotic therapy prompted admission to the emergency department (ED). Her chronic therapies included tiotropium bromide 10 mcg inhaler daily, and mometasone furoate and formoterol fumarate dihydrate 200-5 mcg/act inhaler 2 puffs twice daily. The patient did not have fever, chills, hematuria, epistaxis, and bleeding gums. Her blood pressure was 149/63 mmHg, heart rate 105 bpm, respiratory rate 20 bpm, and temperature 98 °F. The oxygen saturation was in the high 80s on room air. Admission lab results included a white count of 8.9 × 103/µL (ref. range: 4.31-10.16 × 103) with a normal differential, hemoglobin 10.6 g/dL (ref. range: 11.5-15.4), platelets 236 × 103/µL, and normal complete metabolic panel. C-reactive protein and sedimentation rate were 7.3 mg/L (ref. range: < 3) and 11 mm/hour (ref. range: 1-20), respectively. Faint bilateral opacities predominately in the upper lung fields were present on the admission chest X-ray. Bilateral upper lobe ground glass opacities with peripheral sparing, and several additional patches of ground glass opacities in the right middle lobe and bilateral lower lobes were noted on chest computed tomography (CT) (Figure 1A). Suspicion of evolving diffuse alveolar hemorrhage prompted serological testing for autoimmune diseases and vasculitides (complement C1Q, C3, C4, lupus anticoagulant, β2-glycoprotein antibody, cardiolipin antibody, anti-DNAse B antibody, histone antibody, anti-nuclear antibody, glomerular basement membrane antibody, anti-neutrophilic cytoplasmic antibody, rheumatoid factor, IgA levels). The results of these tests were negative. INR and PTT were 1.03 (ref. range: 0.84-1.19) and 29 s (ref. range: 23-37), respectively. Bronchoscopy demonstrated clotted blood at the carina and within both major bronchi (Figure 1C). Bronchoalveolar lavage (BAL) was performed with serial aliquots; the degree of noted blood was similar in all containers. The BAL specimen grew only two colonies of unspeciated Bordetella and were negative for malignancy, viruses, fungi, Legionella, and acid-fast bacilli. Synchronous blood cultures were negative. Following the bronchoscopy, empiric pulse dose steroids were initiated with 1 g of methylprednisolone for 3 days.
Figure 1.
(A) Day 1, lung view on chest CT showing bilateral pulmonary ground glass opacities. (B) Day 9, worsening bilateral ground glass opacities on repeat chest CT. (C) Bronchoscopy showing clotted blood at the carina.
Due to increasing supplemental oxygen requirements and persistent hemoptysis over the next 4 days, the patient was transferred to the intensive care unit. The hemoptysis progressively worsened with rapidly deteriorating oxygenation for which endotracheal intubation was required.
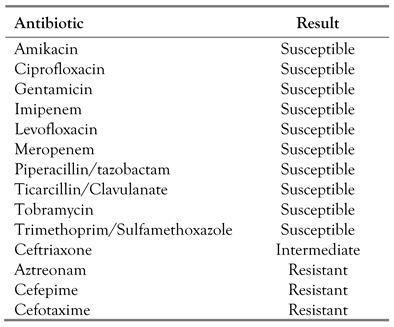
Empiric i.v. azithromycin 500 mg was initiated given an unknown etiology and the few colonies of Bordetella identified on BAL fluid. Repeat bronchoscopy identified active bleeding from both upper lobes. Repeat BAL of the right upper lobe grew 4+ Bordetella. Microbiological speciation was requested provided this significant increase in bacterial growth. She was started on broad spectrum antibiotics with i.v. cefepime 2 g every 12 h and vancomycin 15 mg/kg every 12 h. Over the next two days, the patient’s pulmonary hemorrhage persisted. Worsening bilateral ground glass opacities were noted on repeat chest CT (Figure 1B). Pulmonary angiogram identified bleeding from the bronchial arteries within both upper lobes, which were embolized. Despite these interventions, pulmonary hemorrhage continued, requiring additional bronchoscopies for evacuation of blood in both the upper and lower lobes. The patient deteriorated, with hemodynamic shock refractory to vasopressor therapy. Repeat bronchoscopy now grew 5+ Bordetella. Repeat blood cultures were also positive for Bordetella. At this time, the patient’s family elected to stop life support and the patient died. The next day postmortem, speciation from the bronchoscopy and blood cultures resulted as Bordetella bronchiseptica. The susceptibilities of the organism are summarized in Table 1.

Table 1.
Antibiotic susceptibility profile results from the B. bronchiseptica isolates of our case.
Discussion
Although rare, this case emphasizes the importance of recognizing B. bronchiseptica as a human pathogen. Symptoms of infection range from a mild upper respiratory illness to a persistent cough, hemoptysis, pneumonia, acute respiratory distress syndrome (ARDS), and septic shock. [5,6] Several cases have reported a fatal outcome. Prominent among risk factors for B. bronchiseptica infection are immunodeficiency and pre-existing respiratory illnesses such as COPD, cystic fibrosis, and lung cancer. [6]
B. bronchiseptica produces multiple adhesins and secreted virulence factors. The genetic expression of these factors is regulated by the BvgAS two-component signal transduction system. Provided the right environmental conditions, the virulent genes are upregulated, enabling the organism to attach to and invade the lower respiratory epithelium. Adhesion to the respiratory epithelium is achieved through the action of fimbriae, filamentous hemagglutinins, and pertactin present on the surface of the bacteria. [7] Intracellular invasion and bacterial survival within respiratory epithelial cells and alveolar macrophages is enabled by adenylate cyclase toxin, which reduces the bactericidal ability of host cells. The presence of pulmonary hemorrhage in patients infected by B. bronchiseptica may be explained by the effect of a secreted protein called dermonecrotic toxin (heat-labile toxin). This toxin induces pathologic vasoconstriction by direct action on vascular smooth muscle cells, which may result in ischemia, necrosis, and hemorrhage. [8,9]
Diagnosis relies upon identification of B. bronchiseptica by culture of blood or respiratory tract fluid. It has been proposed that pathogenic infection may be distinguished from normal colonization of the respiratory tract by bacterial colony counts >104 CFU/mL in BAL fluid. [4] In our patient, the initial culture obtained by bronchoscopy only grew two colonies and therefore was not supportive of a true infection. However, the subsequent bronchial cultures contained significantly increased growth. This case reminds us of the importance that the presence of unspeciated Bordetella in a BAL or blood specimen should not be readily dismissed as a non-pathogenic growth. In the setting of hemoptysis without a known cause, the identification of Bordetella on respiratory culture should alert the clinician to treat bronchiseptica as the possible culprit.
Among 29 patients with HIV/AIDS and B. bronchiseptica infections, the most reliably effective antibiotics were carbapenems and fluoroquinolones. [4] A combination of aminoglycosides and beta-lactams with beta-lactamase inhibitors were also highly effective. [4] Likewise, imipenem, ciprofloxacin, and the aminoglycosides amikacin, gentamicin, and tobramycin were reliably effective in other in vitro experiments. [3] While these studies found variable effectiveness of trimethoprim/sulfamethoxazole (TMP/SMX), a 1988 multicenter surveillance project found their isolates to be 82% susceptible to these antibiotics. [10] Most important is the recognition that B. bronchiseptica is generally not susceptible to macrolides, which is the preferred regimen in the treatment of B. pertussis and parapertussis.
Conclusions
Our case exemplifies the importance of recognizing the association between B. bronchiseptica infection and its clinical presentation of hemoptysis/pulmonary hemorrhage. Our case also emphasizes the aggressive potential of this organism and rapidity with which an afflicted patient may deteriorate. Most importantly, B. bronchiseptica has a unique antibiotic susceptibility and resistance profile among the Bordetella species.
Author Contributions
Conception and design: F.I., S.T. Acquisition of data: F.I., M.T., M.N., T.L. Analysis and interpretation of data: F.I., M.T., M.N., T.L., S.T., S.L. Drafting of manuscript: S.T. Revision of manuscript: F.I., S.T., S.L., M.T., M.N., T.L. Final approval of manuscript: F.I., S.T., S.L, M.T., M.N., T.L. All authors read and approved the final version of the manuscript. All authors agree to be accountable for all aspects of the work.
Funding
None to declare.
Conflicts of Interest
All authors—none to declare.
Consent
Written informed consent was obtained from the next-of-kin for publication of their case report and any accompanying images.
Availability of Data
The data supporting the findings of this study are available from the corresponding author, upon reasonable request.
References
- Linz, B.; Ma, L.; Rivera, I.; et al. Genotypic and phenotypic adaptation of pathogens: Lesson from the genus Bordetella. Curr Opin Infect Dis. 2019, 32, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Goodnow, R.A. Biology of Bordetella bronchiseptica. Microbiol Rev. 1980, 44, 722–738. [Google Scholar] [CrossRef] [PubMed]
- Woolfrey, B.F.; Moody, J.A. Human infections associated with Bordetella bronchiseptica. Clin Microbiol Rev. 1991, 4, 243–255. [Google Scholar] [CrossRef] [PubMed]
- Gujju, V.R.; Akram, B.; Shibib, D.R.; McGhee, M.A.; Drevets, D.A. Bordetella bronchiseptica infections in patients with HIV/AIDS: A case report and review of the literature. Medicine (Baltimore) 2021, 100, e28244. [Google Scholar] [CrossRef] [PubMed]
- Tamion, F.; Girault, C.; Chevron, V.; Pestel, M.; Bonmarchand, G. Bordetella bronchoseptica pneumonia with shock in an immunocompetent patient. Scand J Infect Dis. 1996, 28, 197–198. [Google Scholar] [CrossRef] [PubMed]
- Clements, J.; McGrath, C.; McAllister, C. Bordetella bronchiseptica pneumonia: Beware of the dog! BMJ Case Rep. 2018, 2018, bcr2018224588. [Google Scholar] [CrossRef]
- Guetter, S.D.; Eiteman, M.A. Production of biomass and filamentous hemagglutinin by Bordetella bronchiseptica. Bioprocess Biosyst Eng. 2014, 37, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Endoh, M.; Nagai, M.; Ueda, T.; Yoshida, Y.; Nakase, Y. Cytopathic effect of heat-labile toxin of Bordetella parapertussis on aortic smooth muscle cells from pigs or guinea pigs. Microbiol Immunol. 1988, 32, 423–428. [Google Scholar] [CrossRef] [PubMed]
- Brockmeier, S.L.; Register, K.B.; Magyar, T.; Lax, A.J.; Pullinger, G.D.; Kunkle, R.A. Role of the dermonecrotic toxin of Bordetella bronchiseptica in the pathogenesis of respiratory disease in swine. Infect Immun. 2002, 70, 481–490. [Google Scholar] [CrossRef] [PubMed]
- Kurzynski, T.A.; Boehm, D.M.; Rott-Petri, J.A.; Schell, R.F.; Allison, P.E. Antimicrobial susceptibilities of Bordetella species isolated in a Multicenter Pertussis Surveillance Project. Antimicrob Agents Chemother. 1988, 32, 137–140. [Google Scholar] [CrossRef] [PubMed]
© GERMS 2023.