Introduction
Influenza causes epidemics every year and is a leading cause of vaccine-preventable disease (VPD)-associated morbidity and mortality, accounting for at least 40,000 deaths in the European Union (EU) annually [
1]. Despite the required annual administration and moderate effectiveness that varies between seasons, vaccination remains the most affordable and accessible means of prevention [
1,
2]. Although annual vaccination for healthcare professionals (HCP) is recommended, coverage in many EU countries remains low [
1,
3].
The rationale for vaccinating HCP lies beyond the protection of vulnerable populations, as it also ensures uninterrupted operation of medical services and provision of healthcare [
1,
2]. Nevertheless, most medical schools merely recommend vaccination and or guide students appropriately, as influenza vaccine uptake rarely exceeds 40% in these populations [
1,
4]. These shortcomings are often encountered due to the low perceived risk from the disease, as well as misconceptions regarding vaccine significance, effectiveness and safety [
5,
6,
7,
8].
Communication and education are crucial in vaccine acceptance among medical students and HCP [
9,
10]. In Europe, surveys frequently show high acceptance rates and positive attitudes towards vaccination but suboptimal coverage and compliance, mainly due to lack of incentives and accessibility [
5,
6,
7,
8].
Influenza can present with symptoms similar to coronavirus disease-2019 (COVID-19), a novel respiratory infectious disease caused by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) [
11]. COVID-19 has resulted in significant mortality and morbidity, leading to one of the largest pandemics in human history [
11]. Recent development of vaccines has raised the need to ensure widespread access, especially among high-risk groups [
11].
Young adults, such as students, may have a role in disease spread due to their high social activity, increased mobility, and regular contact with patients [
6]. Additionally, young and healthy individuals may be asymptomatic carriers, acting as a hidden reservoir for respiratory viruses. Achieving high vaccination coverage among medical students will increase coverage among HCP in the future, as previous vaccination is an important vaccination determinant [
12].
Our aim is to evaluate determinants of vaccination against influenza and SARS-CoV-2 in medical students in the Republic of Cyprus, by assessing current vaccination status, perceptions, and attitudes towards vaccination among medical students. We hypothesized that clinical students have better knowledge and more favorable attitudes towards vaccination.
Methods
For this cross-sectional study, an original questionnaire in English was used (Appendix). The questionnaire was pilot tested with six persons and was available online as a Google forms© survey that could be completed only once. It was comprised of five demographic questions requesting gender, age, nationality, university, and year of study, as well as 28 multiple choice questions about knowledge of recommendations, attitudes, and perceptions of the two vaccines.
The questionnaire was distributed and completed in March-April 2021. All students of two out of three Medical Schools in the Republic of Cyprus (European University Cyprus, EUC and University of Cyprus, UCY) were invited to complete it through university emails. The 2 participating schools are 6-year medical schools, where years 1-3 are preclinical and years 4-6 are clinical which primarily consist of clinical clerkships. Public health, physiology, pathophysiology, clinical microbiology and infectious diseases, are included early in the medical school curricula. Thus, medical students are expected to understand the importance of vaccination before entering the clinical part of their studies. During the study period, 4 vaccines against SARS-CoV-2 (Vaxzevria/Astrazeneca, Comirnaty/Pfizer, Spikevax/Moderna, Janssen) were licensed and used in the Republic of Cyprus and more than 200,000 doses were administered (including more than 57,000 persons fully vaccinated) among a total population of 875,000 [
13].
The total number of students in the two medical schools when the questionnaire was distributed was 826. For 826 students, with a 5% margin error and 95% confidence interval, minimum sample size for statistical significance is 263. We defined hesitancy as the percentage of students that wish to receive SARS-CoV-2 vaccination after a few months or a year, instead of when the vaccine is available, and refusal as the percentage of students that wish to never receive vaccination. Associations of knowledge and attitudes with participants’ clinical exposure (years 1-3 and 4-6) and perceptions were assessed using the Chi-square test (χ²). Responses "Agree/Slightly agree” were grouped as "Yes”, "Disagree/Slightly disagree” as "No” and "Neutral/I don’t know” as "I don’t know”. Statistical significance was set at 5% significance level (p<0.05). Data were processed and analyzed using IBM SPSS Statistics for Windows, Version 27.0 (IBM Corp, USA) and Microsoft Office Excel version 16.47 for Mac, (Microsoft Press, USA).
Permission was granted from the University Research Committees and the Cyprus National Bioethics Committee (ΕΕΒΚ ΠΚ 2021.01.46, February 22nd, 2021). Participation was voluntary and anonymous. Participants consented to providing their information and were ensured that any personally identifiable information would not be saved.
Discussion
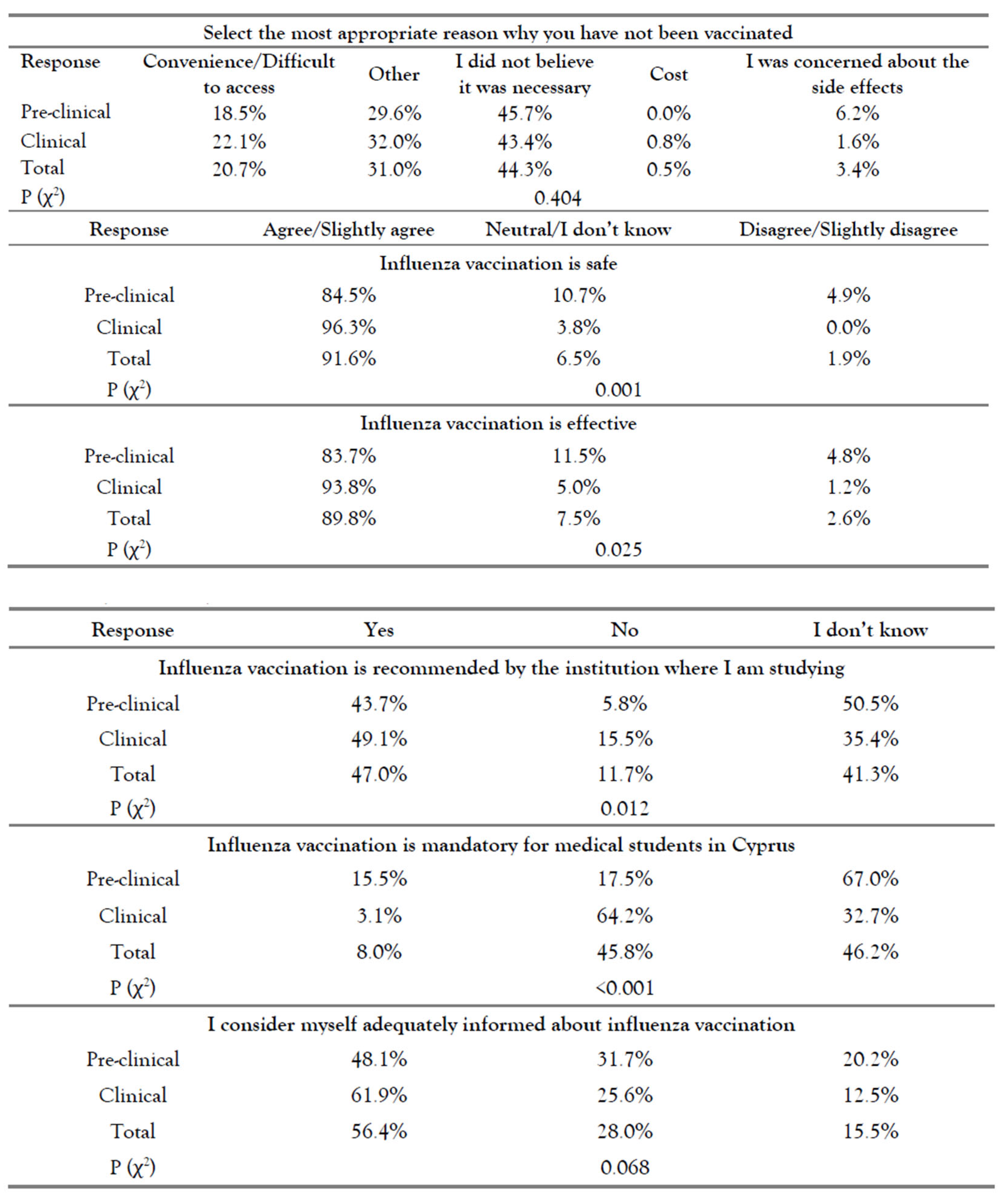
Reasons for high acceptance of the influenza vaccine in previous studies were self-protection, recommendation to vaccinate, positive attitudes towards vaccination, patient protection, professional ethics, and free vaccination [
6,
7,
8]. Reasons for vaccine refusal were inconvenience, forgetfulness, side-effects concerns, perceiving vaccination as unnecessary, vaccine cost and lack of knowledge [
6,
7,
8,
14].
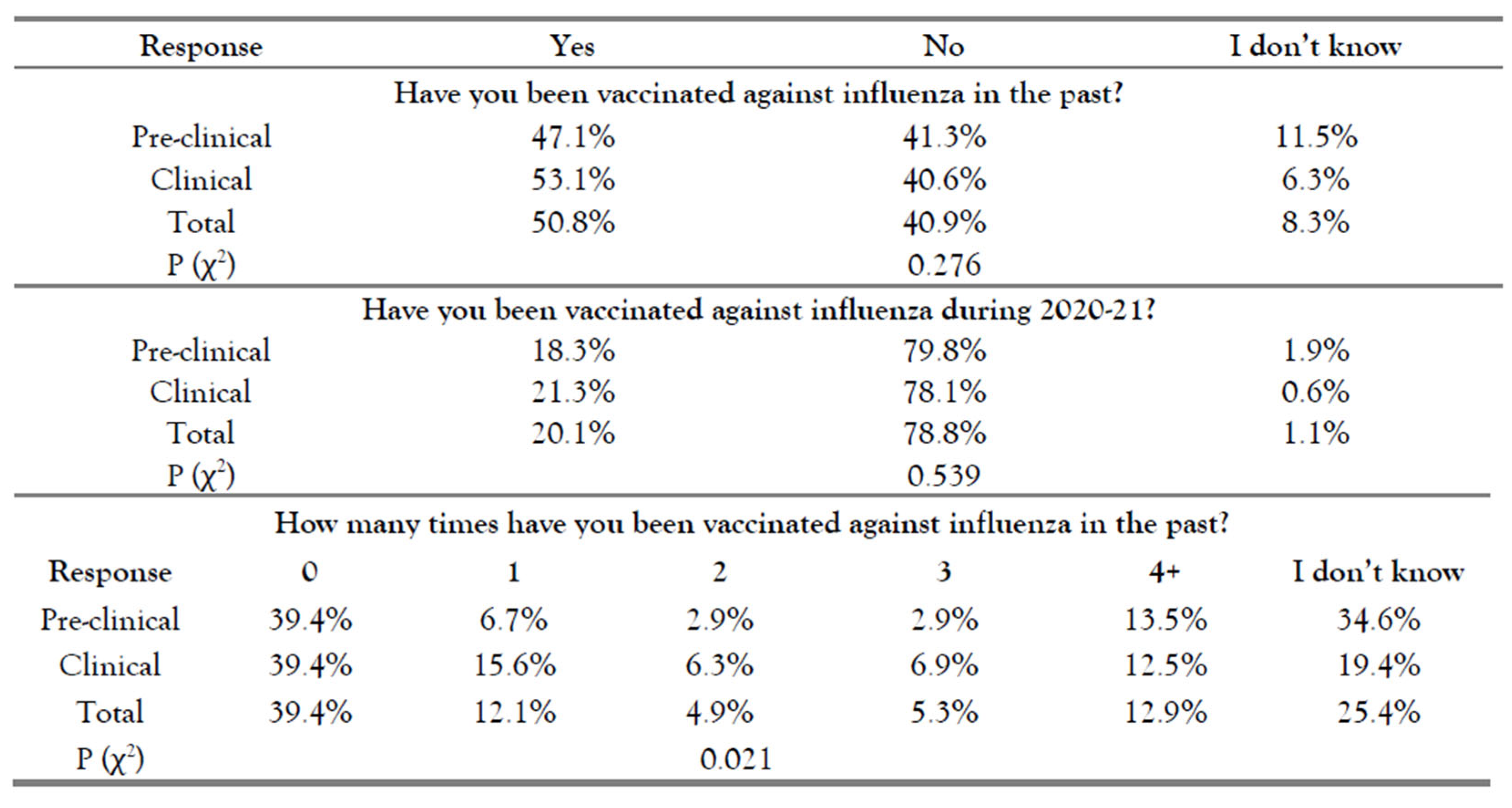
Reported vaccination coverage for influenza ranges from 4.7% to 58.1% [
6]. In accordance, our study showed a 50.6% past vaccination rate overall and a disappointingly low rate of 20.1% in 2020-2021. However, this proportion is comparable to the reported vaccination coverage for influenza (31.8%) among healthcare workers in Cyprus [
15]. Possible explanations other than low-risk perception could be that influenza was not expected to be so prominent, that our students did not expect significant clinical exposure, or had limited accessibility to vaccination sites due to COVID-19 restrictions. Clinical students have been described as more likely to be vaccinated than preclinical students, [
7,
8] although we did not observe a significant difference.
Other studies found a similar correlation between clinical exposure and knowledge or attitudes towards vaccination [
6,
7,
8,
16]. More clinical students in our sample showed positive attitudes and were informed regarding the current recommendations. We also observed that more clinical students were confident in their knowledge and were not hesitant to receive vaccination. These findings are in line with Saftenburg et al., that report correlation between semester of studies and knowledge about national vaccination recommendations, [
16] as well as Hernández-García et al., where clinical students had better knowledge concerning influenza [
17].
More than half (54.2%) of the students replied incorrectly when asked if influenza vaccination is mandatory in Cyprus (82.5% of preclinical, 35.8% of clinical students, p<0.001) and 41.5% didn’t know if it was recommended by their institution. When asked if they considered themselves adequately informed about influenza vaccination, only 56.4% of students replied positively. This is in accordance with the results by Kernéis et al., who reported significant knowledge gaps and a need to clarify recommendations [
18].
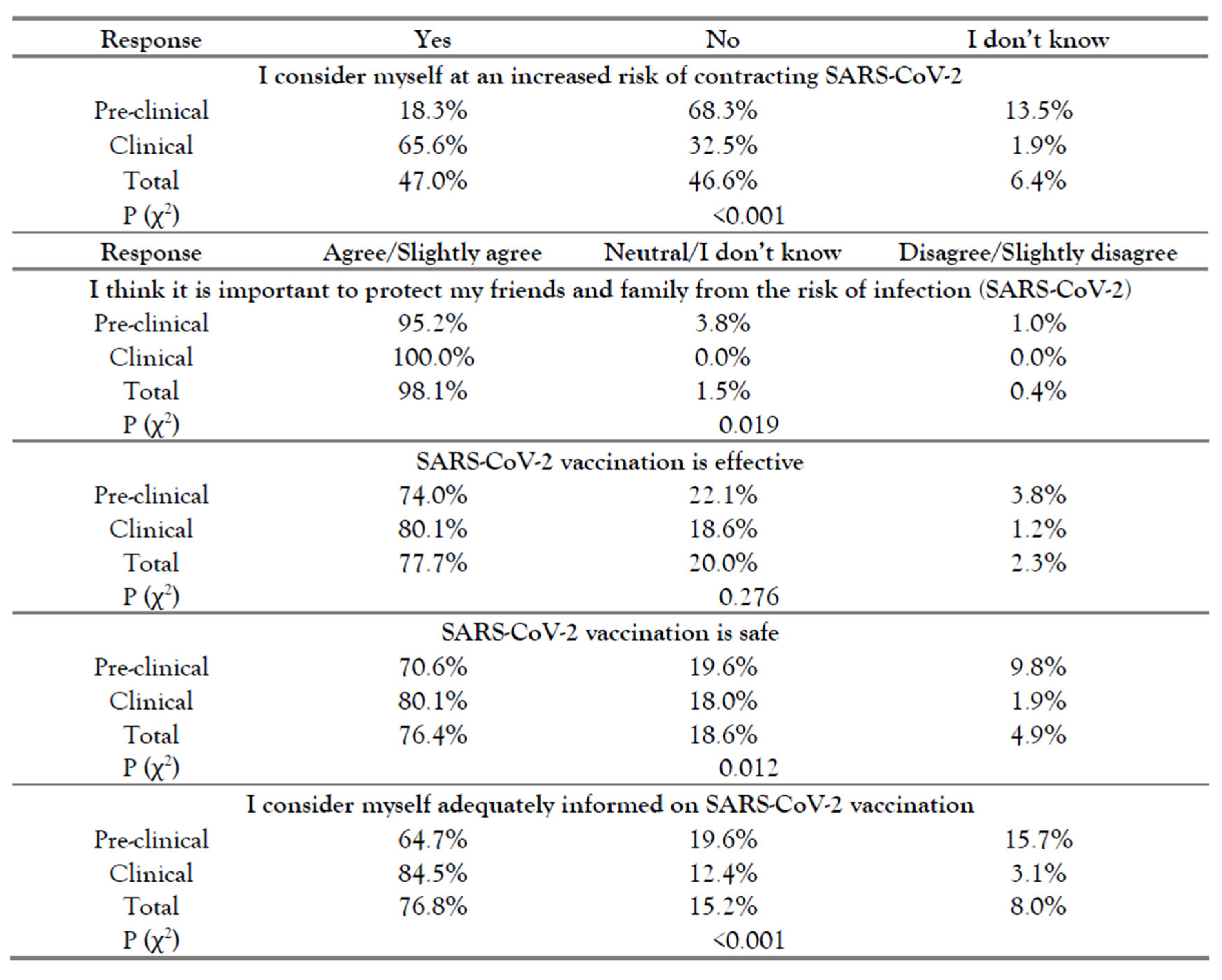
A limited number of studies focused on SARS-CoV-2 vaccination determinants in medical students [
19,
20,
21,
22]. Almost all students in the study by Lucia et al. had positive attitudes towards vaccination and agreed they were likely to be exposed to COVID-19 [
19]. In Saied et al., 90.5% perceived the importance of vaccination and in Szmyd et al., more than 90% of medical students wanted to get vaccinated [
20,
22]. In our study, 89.4% replied positively to "If my Institution/country offers free vaccination, I will get the vaccine”.
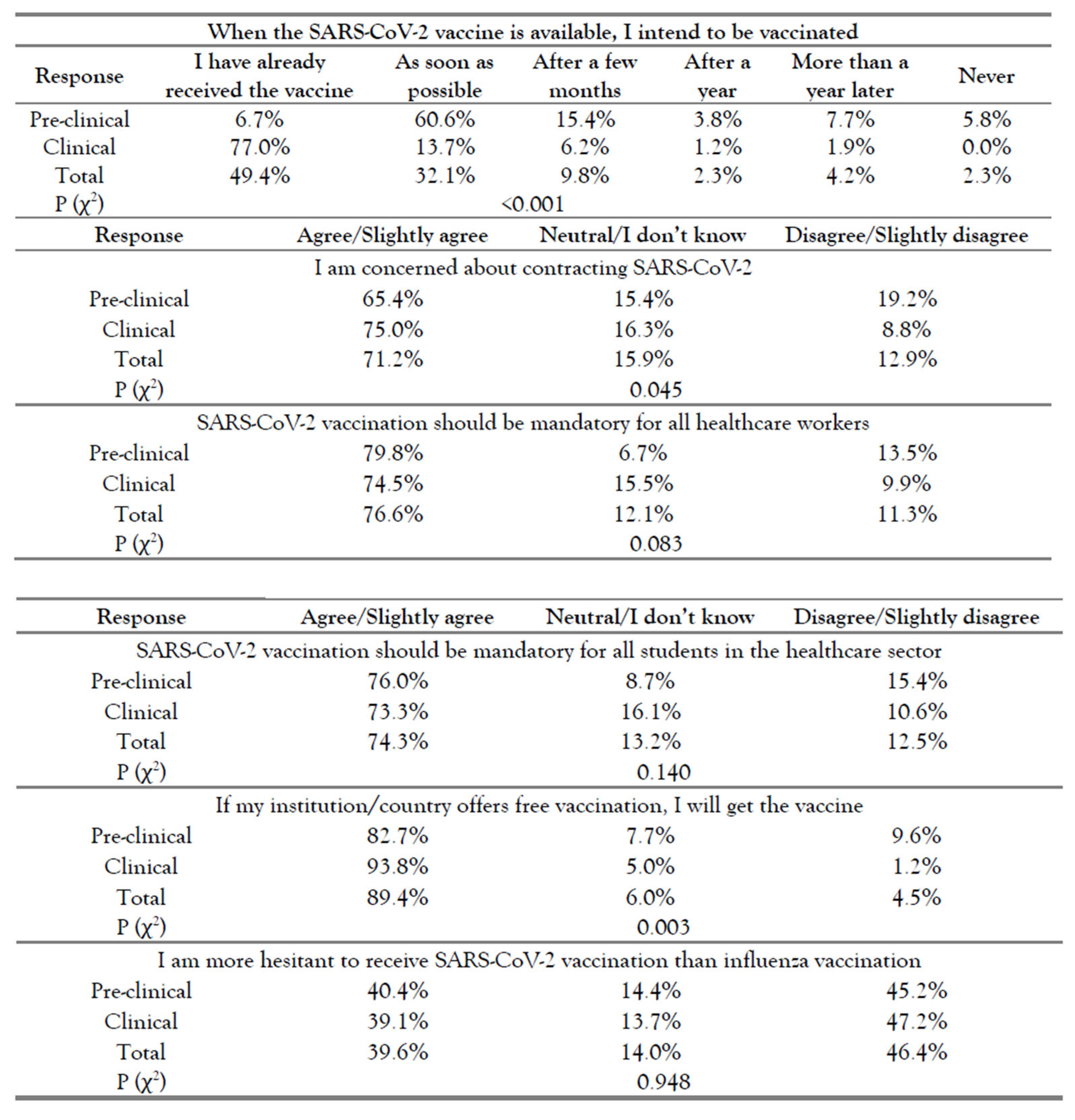
In the literature, the percentage of students characterized as hesitant was 13.9-46% [
20,
21]. Similarly, there was marked hesitancy in our sample (16.3%). Saied et al. reported that most of the students (71%) accepted the vaccine but would postpone it for some time, and Lucia et al. reported that 23% of medical students were unwilling to be vaccinated immediately upon FDA approval [
19,
20]. Among our students, more preclinical students appeared hesitant than clinical students (63.7% vs 90.7%; p<0.001). SARS-CoV-2 vaccination had already been offered to clinical students at the time of questionnaire completion, which explains the difference in the number of vaccinated students (77% clinical, 6.7% preclinical, p<0.001). Saied et al. reported an interestingly lower percentage (13%) of students that intended to receive the vaccine "as soon as possible” compared to 32.1% in our study and 76.3% by Szmyd et al [
20,
22]. This proportion could have been ~81.5% in our study, if 49.4% hadn’t already received the vaccine. Willingness to get vaccinated as soon as possible was amplified by fear of passing on the virus to relatives, fear of infection and disease complications, as well as the year of study. Vaccination refusal was 2.3%, which is markedly lower compared to 13.9% – 16% in the literature [
20,
22]. In previous studies, the most reported factor affecting SARS-CoV-2 vaccine hesitancy was fear of side and adverse effects [
19,
20,
21,
22].
As with influenza, more clinical students have positive attitudes towards vaccination, are confident with their knowledge and are not hesitant as often as preclinical students. In agreement with previous observations, [
5,
18] most of our students (76.8%) consider themselves adequately informed concerning SARS-CoV-2, with significantly more clinical students (84.5%) replying positively compared to 64.7% of preclinical students (p<0.001). This is also in line with a previous survey among university students in Cyprus before vaccines became available, where postgraduate students exhibited higher levels of knowledge related to COVID-19 characteristics and prevention measures [
5]. Saied et al. reported that their students perceived themselves at elevated risk to contract COVID-19 (77.6%), which is notably larger compared to our results (47%) [
20]. This is in accordance with Wicker et al., who suggested that students may be inaccurate when assessing their risk to contract specific VPDs [
8]. However, a high percentage of students in our sample had already been vaccinated and may not have been exposed to patients due to remote learning.
We observed that more students had positive attitudes towards SARS-CoV-2 vaccination compared to influenza and more were concerned about contracting SARS-CoV-2 (71.2%) than influenza (25.4%). Most students (76.8%) considered themselves adequately informed about SARS-CoV-2 vaccination, but fewer (56.6%) replied similarly for influenza, despite the latter being discussed early and repeatedly in medical education. This could be explained by the publicity of the pandemic, the increased risk perception of SARS-CoV-2 or the low risk perception of influenza. In our sample, only 77.1% would participate in free annual influenza vaccination, compared to 89.1% that would participate in SARS-CoV-2 vaccination. Commenting on "I think it is important to protect my friends and family from the risk of infection” 98.1% replied positively for SARS-CoV-2, compared to 88.7% for influenza, further indicating their perception of SARS-CoV-2 as a greater threat.
Easy access to the vaccine is not always offered to medical students, even during clinical training [
6]. Organizational barriers, such as vaccination not being offered, have been considered possible factors in hindering vaccination [
6,
17,
23,
24]. This could partly explain the intention-behavior gap that has been observed in the literature [
6]. In our study, 20.6% of the students chose convenience and accessibility as their main reason for not taking the influenza vaccine. Only 46.8% of students indicated that they have easy access to an influenza vaccine, while 77.4% would get the vaccine if it was offered for free by the institution they attend. More than a third of those students had never been vaccinated against influenza. Among our clinical students, 77% had been vaccinated against SARS-CoV-2 but only 21.3% had been vaccinated against influenza for 2020-2021, at the time of questionnaire completion. This may be attributed to their increased risk perception of SARS-CoV-2, but also to vaccination being organized and directly offered for free by the University. Our data support the theory that lecture-based education alone, may not have the desired effects when it comes to vaccination [
18]. Specific targeted but easy to integrate interventions, such as hands-on or case-based learning, have demonstrated a positive shift in attitudes towards vaccination [
18,
23,
25]. Specifically, the invitation from the University and a specific training about influenza vaccination have been shown to improve acceptance of vaccination [
18,
23,
25].
Certain limitations in our study should be acknowledged. Two out of three Medical Schools in Cyprus participated in this study, which may affect its generalizability. The subject’s sensitivity may introduce bias, especially if students believe that vaccination is mandatory. The aim of our study was to identify attitudes and perceptions; future studies should examine vaccination determinants among students in depth, in order to identify opportune occasions to enhance vaccination. Additionally, perceptions and attitudes were not included in a scoring system, thus limiting the ability for comparisons.