Case report
We present the case of a 72-year-old patient diagnosed with SARS-CoV-2 infection by reverse transcription-polymerase chain reaction (RT-PCR) testing from nasal and pharyngeal swab. She was hospitalized for fever, chills, dry cough, shortness of breath, myalgia, arthralgia, physical asthenia, loss of appetite.
The patient was admitted three days after experiencing the above symptoms, which progressively worsened, the RT-PCR test that came back positive was performed one day before admission.
Pathological history showed that the patient had hypertension, ischemic heart disease, hypothyroidism and gout, as well as a history of ischemic stroke in 2018. At the time of the presentation the chronic conditions were stable.
At the time of admission, the oxygen saturation was 95% in ambient air, native thoracopulmonary computed tomography (CT) revealed a mild form of SARS-CoV-2 pneumonia. Laboratory analyses collected showed mild inflammatory syndrome, increased interleukin 6 (IL6) value (79.59 pg/mL, normal range = 0–4 pg/mL), normal blood count, normal lactate dehydrogenase (LDH), prothrombin time (PT), activated partial thromboplastin times (APTT), D-dimers and troponin (
Table 1), and negative results for HBsAg, antiHBc, HCV antibodies, HIV test, Epstein Barr and cytomegalovirus antibodies.
The patient received from the beginning of hospitalization antiviral therapy with favipiravir orally 1600 mg twice a day, one day, then 600 mg twice a day (for a total of 10 days), according to the national protocol, thromboprophylaxis with dalteparin in a single daily subcutaneous dose (5000 IU), non-steroidal anti-inflammatory drug, with a favorable evolution until the fifth day of hospitalization, when the patient presented fever and decrease in oxygen saturation (91% in ambient air).
The second emergency native CT scan showed a worsening of SARS-CoV-2 pneumonia, the performed analyses revealed increasing inflammatory syndrome, and dexamethasone 6 mg twice a day intravenously, 5 days, and oxygen therapy 8 L/min delivered by face mask, were added to the treatment.
The clinical evolution was favorable, with the decrease of the oxygen requirement for another 3 days, and the improvement of the inflammatory syndrome.
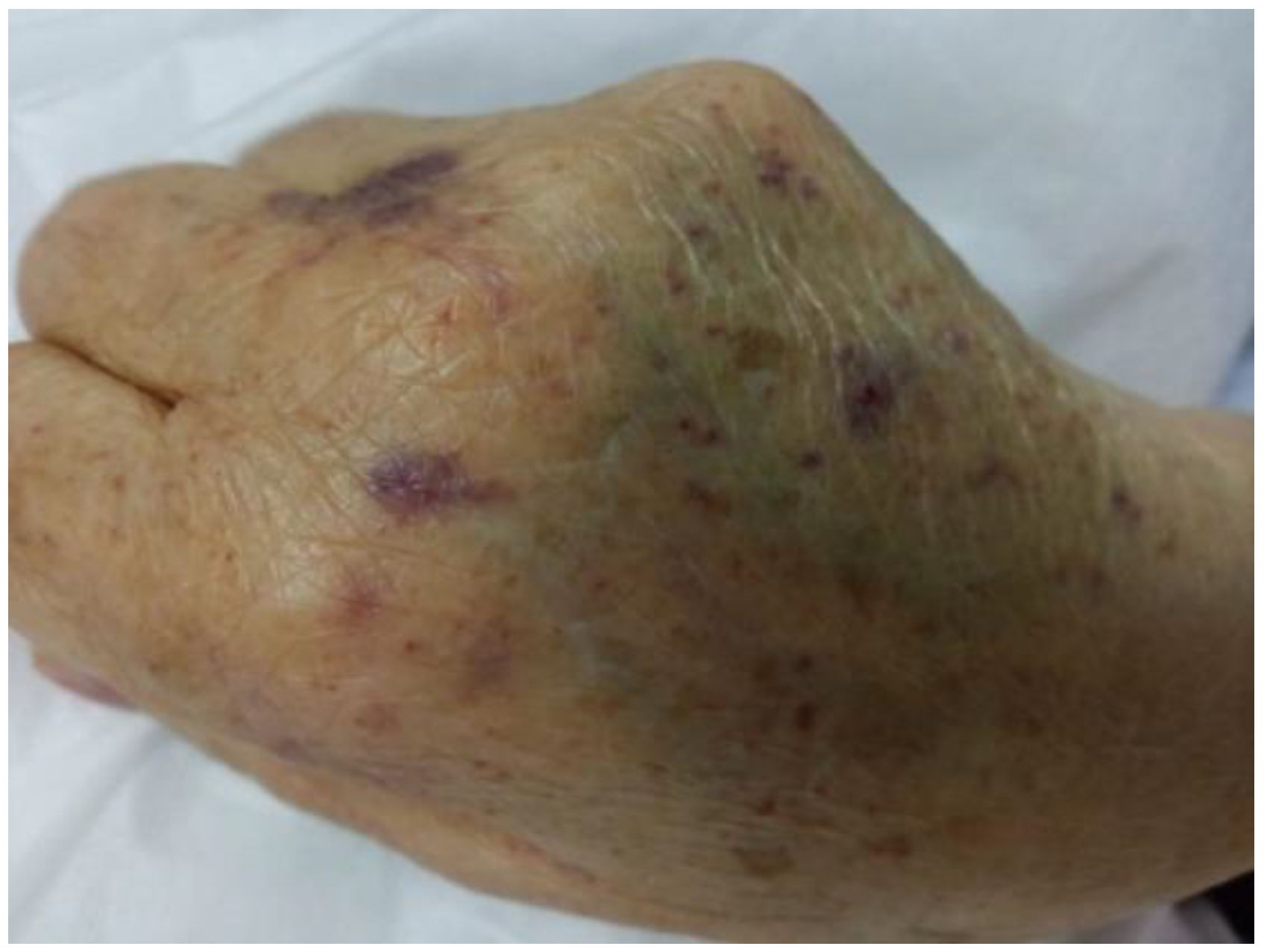
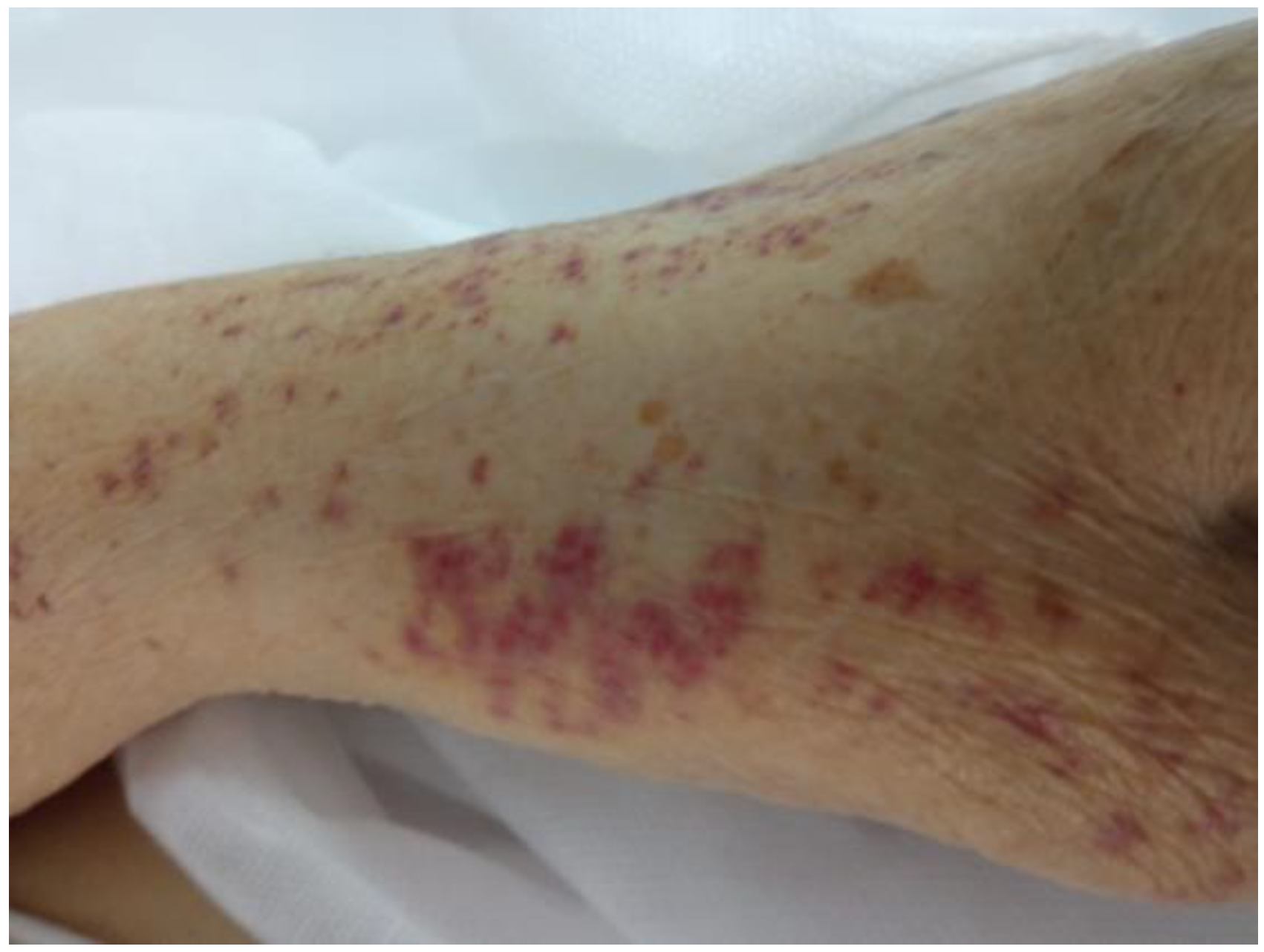
On the tenth day of hospitalization, the patient presented a generalized purple rash on the skin and mucous membranes, predominantly on the upper limbs, chest and mouth, with a tendency to spontaneous bleeding (
Figure 1,
Figure 2 and
Figure 3).
Laboratory assessments revealed severe thrombocytopenia with a number of 3 × 10⁹/L, without the association of other abnormalities; PT/INR and APTT values were normal.
The SARS-CoV-2 RT-PCR test collected at the onset of the purple rash was positive with a viral load of 6468 copies/mL and positive anti-platelet antibody test.
Given these results, anticoagulant prophylaxis was stopped, and hematological consultation was requested. ITP secondary to infection with SARS-CoV-2 was established and dexamethasone treatment initiated in a higher dose, 40 mg/day (equivalent to 0.5 mg/kg/day) intravenously. Due to the increased risk of bleeding, platelet transfusions were associated, 4 UI/day, for a total of three days.
After four days of treatment with dexamethasone (on the 14th day of hospitalization), the general condition improved, the petechiae began to disappear and on the 16th day of hospitalization the value of platelets was normal.
The patient was hospitalized for a total of 18 days, and was discharged in good general condition, with remission of purpuric rash, both on the skin and on mucous membranes, with no oxygen requirement, normal platelet values and negative SARS-CoV-2 RT-PCR test, with the recommendation to continue oral methylprednisolone therapy for another 14 days at the initial dose of 32 mg/day × 7 days followed by 16 mg/day × 7 days, and outpatient hematological monitoring.
After one month of follow-up, the patient continues to be in good general condition, with total remission of the purplish rash and a normal platelet count.
Discussion
The association between SARS-CoV-2 and ITP has been described in the last year in several cases.
Bennet et al. describe the case of a 73-year-old woman who was hospitalized with COVID-19 pneumonia and severe thrombocytopenia. The patient received platelet mass without improvement in platelet counts, but no corticosteroids were administered to avoid the hypothetical risk of SARS-CoV-2 replication. The patient responded well to intravenous immune globulin (ivIg) administration with an increase in platelet count after three days of administration [
5]. About one month after discharge, the patient was hospitalized again for generalized petechiae eruption and low platelet counts, which improved after administration of pulse therapy with dexamethasone [
5].
In the case of our patient, although high doses of dexamethasone were administered, no increase in SARS-CoV-2 replication was found, the evolution was favorable, the RT-PCR test was negative on discharge. The hematologist’s recommendation was to start treatment with dexamethasone and platelet mass, and in case of lack of response after 4 days, to initiate treatment with ivIg.
María José Macías-Reyes et al. described the case of a 67-year-old patient with severe form of COVID-19 who developed ITP, with a favorable evolution under treatment with immunoglobulins and pulse therapy with methylprednisolone [
6]. The authors made a differential diagnosis with disseminated intravascular coagulation (coagulation times within normal limits, increased fibrinogen values) and endocarditis (fever, inflammatory syndrome, thrombocytopenia, purpura), but blood cultures were negative, no new heart murmurs were found, and transthoracic ultrasound of the heart did not detect vegetations [
6,
7].
As in our case, Abrar-Ahmad Zulfiqar et al. published the case of a 65-year-old patient, also with moderate form of COVID-19, who developed ITP on day 9 of the disease and secondary hemorrhagic stroke. Intravenous immune globulin was administered at a rate of 1 g/kg body weight (two days) associated with platelet administration and eltrombopag 75 mg/day, with a favorable evolution of both thrombocytopenic purpura and stroke that resolved without sequelae [
8].
Mahevas et al. described a series of 14 cases in which ITP appeared in the second phase of the evolution of COVID-19 (on average one week after the onset of symptoms), most of them (12 patients) had moderate pneumonia on CT scan, and approximately half of them had bleeding [
9]. Patients received treatment with dexamethasone in most cases, ivIg or eltrombopag, complete remission of symptoms occurred between 30 and 60 days [
9], and in our case 22 days after the onset of ITP.
A recent review of a total of 45 cases [
4], concluded that ITP occurred on average on the 13th day of illness (in a few cases in the post-recovery period) in patients with moderate COVID-19 pneumonia, one third without significant bleeding at the time of diagnosis of ITP, with median nadir platelet count 5 × 10
9/L (nadir platelet count 2 × 10
9/L in our case). Most of them received treatment with ivIg, glucocorticoids or thrombopoietin receptor agonist (TP-RA); platelet transfusions were used only in a few patients with severe bleeding [
4].
In conclusion, hematological manifestations in COVID-19 are common, and ITP can occur in patients with moderate COVID-19 pneumonia, most often during the disease, but also in the post-COVID-19 period. The disease generally has a good evolution under treatment with glucocorticoids or ivIg; platelet transfusions are administered only in cases with severe bleeding.
Our case was the only one observed in patients with COVID-19 hospitalized in our hospital in the last year (over 3000 patients). Despite a very low platelet count, the evolution was favorable under treatment with glucocorticoids and platelet transfusions.