Purulent Pericarditis in a Patient with Community-Acquired Methicillin-Resistant Staphylococcus aureus: A Case Report with Mini-Review
Abstract
Introduction
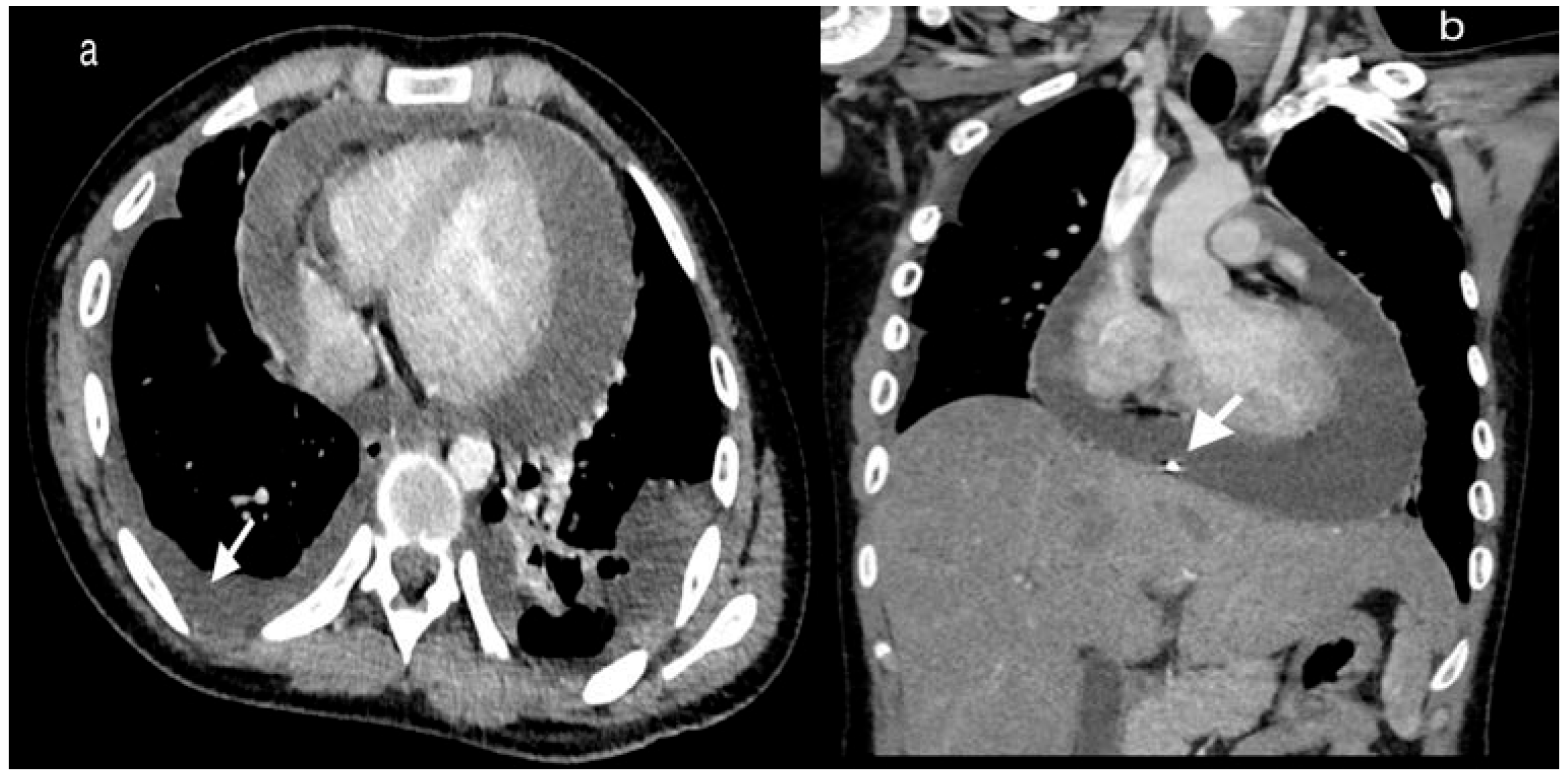
Case report
Discussion
Author Contributions
Funding
Informed Consent Statement
Conflicts of Interest
References
- Klevens, R.M.; Morrison, M.A.; Nadle, J.; et al. Invasive methicillin-resistant Staphylococcus aureus infections in the United States. JAMA 2007, 298, 1763–1771. [Google Scholar] [CrossRef] [PubMed]
- Imazio, M.; Gaita, F.; LeWinter, M. Evaluation and treatment of pericarditis a systematic review. JAMA 2015, 314, 1498–1506. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Li, J.; Qiao, Y.; Ning, X.; Zeng, T.; Shen, X. Prevalence and invasiveness of community-acquired methicillin-resistant Staphylococcus aureus: A meta-analysis. Indian J. Microbiol. 2014, 57, 418–422. [Google Scholar] [CrossRef]
- Pankuweit, S.; Ristić, A.D.; Seferović, P.M.; Maisch, B. Bacterial pericarditis: Diagnosis and management. Am. J. Cardiovasc. Drugs. 2005, 5, 103–112. [Google Scholar] [CrossRef] [PubMed]
- Adler, Y.; Charron, P.; Imazio, M.; et al. 2015 ESC Guidelines for the diagnosis and management of pericardial diseases: The Task Force for the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology (ESC) Endorsed by: The European Association for Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 2015, 36, 2921–2964. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.; Maves, R.; Barrozo, C.P.; et al. Mycotic pseudoaneurysm and purulent pericarditis attributable to methicillin-resistant Staphylococcus aureus. Mil. Med. 2006, 171, 784–787. [Google Scholar] [CrossRef] [PubMed]
- Hussam, M.A.; Ragai, M.F.; Iman, M.F.; Zakaria, A. Community-acquired methicillin-resistant Staphylococcus aureus pericarditis presenting as cardiac tamponade. South. Med. J. 2010, 103, 834–836. [Google Scholar] [CrossRef] [PubMed]
- Arora, N.P.; Kottam, A.; Mahajan, N.; et al. Purulent pericardial effusion from community-acquired methicillin-resistant Staphylococcus aureus. Am. J. Med. Sci. 2012, 344, 160–162. [Google Scholar] [CrossRef] [PubMed]
- Kurahara, Y.; Kawaguchi, T. Cardiac tamponade with community-acquired methicillin-resistant Staphylococcus aureus pericarditis. Intern. Med. 2013, 52, 1753. [Google Scholar] [CrossRef] [PubMed]
- Lutmer, J.E.; Yates, A.R.; Bannerman, T.L.; Marcon, M.J.; Karsies, T.J. Purulent pericarditis secondary to community-acquired, methicillin-resistant Staphylococcus aureus in previously healthy children. A sign of the times? Ann. Am. Thorac. Soc. 2013, 10, 235–238. [Google Scholar] [CrossRef] [PubMed]
- Terada, M.; Watanabe, H.; Kobukai, Y.; et al. Successful treatment of a patient with purulent pericarditis by daily intrapericardial washouts. Ann. Thorac. Surg. 2014, 98, 1451–1454. [Google Scholar] [CrossRef] [PubMed]
- Mada, P.K.; Cady, B.; De Silva, A.; Alam, M. Disseminated MRSA infection with purulent pericarditis. BMJ Case Rep. 2017, 2017, bcr2016218463. [Google Scholar] [CrossRef] [PubMed]
- Sanchez, J.; Schneider, A.; Tretter, J.T.; et al. Community-acquired MRSA pericarditis and mediastinitis in a previously healthy infant. J. Pediatr. Intensive Care 2018, 7, 97–101. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Haq, N.; Moussa, Z.; Farhat, M.H.; Chandrasekar, L.; Asmar, B.I. Infectious and noninfectious acute pericarditis in children: An 11-year experience. Int. J. Pediatr. 2018, 2018, 5450697. [Google Scholar] [CrossRef] [PubMed]
- Ganji, M.; Ruiz, J.; Kogler, W.; Lung, J.; Hernandez, J.; Isache, C. Methicillin-resistant Staphylococcus aureus pericarditis causing cardiac tamponade. IDCases 2019, 18, e00613. [Google Scholar] [CrossRef] [PubMed]
 |
© GERMS 2020.
Share and Cite
Meena, D.S.; Kumar, D.; Gopalakrishnan, M.; Bohra, G.K.; Midha, N.; Vijayvargiya, P.; Tiwari, S. Purulent Pericarditis in a Patient with Community-Acquired Methicillin-Resistant Staphylococcus aureus: A Case Report with Mini-Review. Germs 2020, 10, 249-253. https://doi.org/10.18683/germs.2020.1212
Meena DS, Kumar D, Gopalakrishnan M, Bohra GK, Midha N, Vijayvargiya P, Tiwari S. Purulent Pericarditis in a Patient with Community-Acquired Methicillin-Resistant Staphylococcus aureus: A Case Report with Mini-Review. Germs. 2020; 10(3):249-253. https://doi.org/10.18683/germs.2020.1212
Chicago/Turabian StyleMeena, Durga Shankar, Deepak Kumar, Maya Gopalakrishnan, Gopal Krishana Bohra, Naresh Midha, Parag Vijayvargiya, and Sarbesh Tiwari. 2020. "Purulent Pericarditis in a Patient with Community-Acquired Methicillin-Resistant Staphylococcus aureus: A Case Report with Mini-Review" Germs 10, no. 3: 249-253. https://doi.org/10.18683/germs.2020.1212
APA StyleMeena, D. S., Kumar, D., Gopalakrishnan, M., Bohra, G. K., Midha, N., Vijayvargiya, P., & Tiwari, S. (2020). Purulent Pericarditis in a Patient with Community-Acquired Methicillin-Resistant Staphylococcus aureus: A Case Report with Mini-Review. Germs, 10(3), 249-253. https://doi.org/10.18683/germs.2020.1212




