Update on Urogenital Tuberculosis in Southern Tunisia: A Review of a 26-Year Period
Abstract
Introduction
Methods
Study design
Data collection and case definitions
Statistical analysis
Results
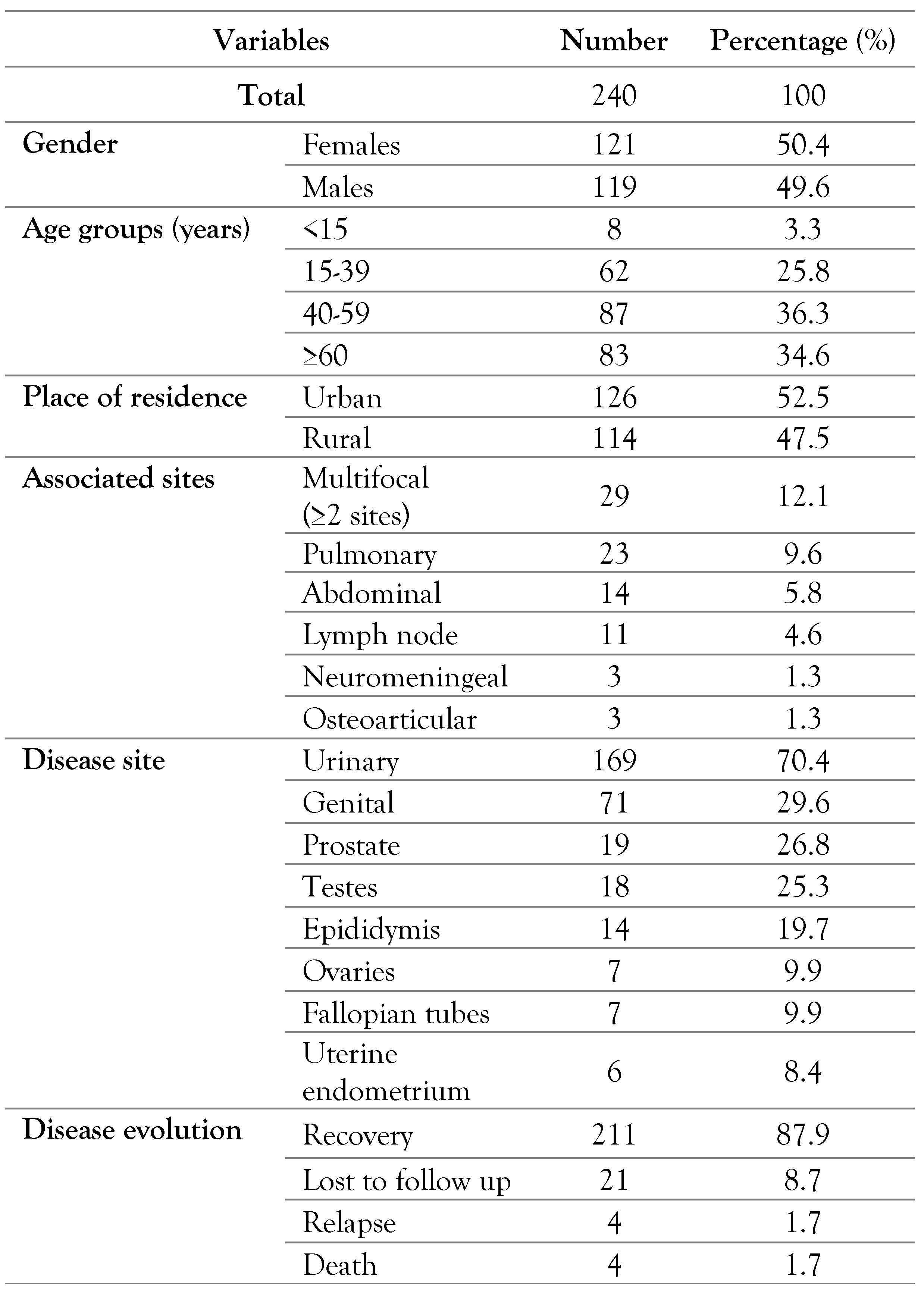
Patients’ characteristics
Chronological trends of urogenital tuberculosis between 1992 and 2017
Epidemiological and clinical characteristics of urogenital tuberculosis
Discussion
Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- World Health Organization. Global Tuberculosis Report. 2018. Available online: https://www.who.int/tb/publications/global_report/en/ (accessed on 4 February 2020).
- United Nations. Ensure Healthy Lives and Promote Wellbeing for All at All Ages. Sustainable Development Goals. 2018. Available online: https://www.un.org/sustainabledevelopment/health/ (accessed on 4 February 2020).
- Kulchavenya, E.; Kholtobin, D. Diseases masking and delaying the diagnosis of urogenital tuberculosis. Ther Adv Urol 2015, 7, 331–338. [Google Scholar] [CrossRef] [PubMed]
- Yadav, S.; Singh, P.; Hemal, A.; Kumar, R. Genital tuberculosis: Current status of diagnosis and management. Transl Androl Urol 2017, 6, 222–233. [Google Scholar] [CrossRef]
- Grace, G.A.; Devaleenal, D.B.; Natrajan, M. Genital tuberculosis in females. Indian J Med Res 2017, 145, 425–436. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.J.; Lee, W.; Jeong, W.Y.; et al. Chronic kidney disease with genitourinary tuberculosis: Old disease but ongoing complication. BMC Nephrol 2018, 19, 193. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Tuberculosis Report. 2019. Available online: https://apps.who.int/iris/bitstream/handle/10665/329368/9789241565714-eng.pdf?ua=1 (accessed on 15 June 2020).
- Zayet, S.; Berriche, A.; Ammari, L.; et al. [Epidemio-clinical features of genital tuberculosis among Tunisian women: A series of 47 cases]. Pan Afr Med J 2018, 30, 71. [Google Scholar] [CrossRef]
- Trigui, M.; Ben Ayed, H.; Koubaa, M.; et al. Multifocal tuberculosis in southern Tunisia what is specific with? J Tuberc 2018, 2, 1006. [Google Scholar]
- Kapoor, R.; Ansari, M.S.; Mandhani, A.; Gulia, A. Clinical presentation and diagnostic approach in cases of genitourinary tuberculosis. Indian J Urol 2008, 24, 401–405. [Google Scholar] [CrossRef] [PubMed]
- Chhonkar, A.; Tambe, S.; Aswani, Y.; Nayak, C.S. Case series of genital tuberculosis. Indian J Sex Transm Dis AIDS 2017, 38, 183–186. [Google Scholar] [CrossRef]
- Verma, R.; Patil, T.B.; Lalla, R. Disseminated tuberculosis manifesting as pulmonary, meningeal and spinal tuberculosis in an immunocompetent patient. BMJ Case Rep 2012, 2012, bcr2012007778. [Google Scholar] [CrossRef]
- Jagodziński, J.; Zielonka, T.M.; Peplińska, K.; Życińska, K. Tuberculosis of the urogenital tract in adults in a tertiary referral center. Adv Exp Med Biol 2018, 1040, 29–37. [Google Scholar] [CrossRef]
- Fillion, A.; Koutlidis, N.; Froissart, A.; Fantin, B. [Investigation and management of genito-urinary tuberculosis]. Rev Med Interne 2014, 35, 808–814. [Google Scholar] [CrossRef] [PubMed]
- Yuan, J. Genitourinary presentation of tuberculosis. Rev Urol 2015, 17, 102–105. [Google Scholar] [PubMed]
- Nakane, K.; Yasuda, M.; Deguchi, T.; et al. Nationwide survey of urogenital tuberculosis in Japan. Int J Urol 2014, 21, 1171–1177. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Jacoiste Asín, M.A.; Fernández-Ruiz, M.; López Medrano, F.; et al. Bacillus Calmette-Guérin (BCG) infection following intravesical BCG administration as adjunctive therapy for bladder cancer: Incidence, risk factors, and outcome in a single-institution series and review of the literature. Medicine (Baltimore) 2014, 93, 236–254. [Google Scholar] [CrossRef] [PubMed]
- Figueiredo, A.A.; Lucon, A.M.; Junior, R.F.; Srougi, M. Epidemiology of urogenital tuberculosis worldwide. Int J Urol 2008, 15, 827–832. [Google Scholar] [CrossRef] [PubMed]
- Taghinejad, J.; Sadeghi Oroumiyeh, A.; Barati, B.; Karimi, S.; Jahantab, M.; Molayi Kohneshahri, S. Epidemiologic study of tuberculosis during 2006–2015 in Salmas, Iran. Int J Health Life Sci 2018, 4, e80210. [Google Scholar] [CrossRef]
- Lee, J.Y. Diagnosis and treatment of extrapulmonary tuberculosis. Tuberc Respir Dis (Seoul) 2015, 78, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Sharma, J.B.; Singh, N.; Dharmendra, S.; et al. Six months versus nine months anti-tuberculous therapy for female genital tuberculosis: A randomized controlled trial. Eur J Obstet Gynecol Reprod Biol 2016, 203, 264–273. [Google Scholar] [CrossRef] [PubMed]
- Gokce, G.; Kilicarslan, H.; Ayan, S.; et al. Genitourinary tuberculosis: A review of 174 cases. Scand J Infect Dis 2002, 34, 338–340. [Google Scholar] [CrossRef] [PubMed]
- Ben Ayed, H.; Koubaa, M.; Gargouri, L.; et al. Epidemiology and disease burden of tuberculosis in south of Tunisia over a 22-year period: Current trends and future projections. PLoS ONE 2019, 14, e0212853. [Google Scholar] [CrossRef] [PubMed]


 |
 |
© GERMS 2020.
Share and Cite
Hammami, F.; Koubaa, M.; Ben Ayed, H.; Rekik, K.; Ben Jemaa, M.; Ben Hmida, M.; Trigui, M.; Marrakchi, C.; Dammak, J.; Ben Jemaa, M. Update on Urogenital Tuberculosis in Southern Tunisia: A Review of a 26-Year Period. Germs 2020, 10, 150-156. https://doi.org/10.18683/germs.2020.1200
Hammami F, Koubaa M, Ben Ayed H, Rekik K, Ben Jemaa M, Ben Hmida M, Trigui M, Marrakchi C, Dammak J, Ben Jemaa M. Update on Urogenital Tuberculosis in Southern Tunisia: A Review of a 26-Year Period. Germs. 2020; 10(3):150-156. https://doi.org/10.18683/germs.2020.1200
Chicago/Turabian StyleHammami, Fatma, Makram Koubaa, Houda Ben Ayed, Khaoula Rekik, Maissa Ben Jemaa, Mariem Ben Hmida, Maroua Trigui, Chakib Marrakchi, Jamel Dammak, and Mounir Ben Jemaa. 2020. "Update on Urogenital Tuberculosis in Southern Tunisia: A Review of a 26-Year Period" Germs 10, no. 3: 150-156. https://doi.org/10.18683/germs.2020.1200
APA StyleHammami, F., Koubaa, M., Ben Ayed, H., Rekik, K., Ben Jemaa, M., Ben Hmida, M., Trigui, M., Marrakchi, C., Dammak, J., & Ben Jemaa, M. (2020). Update on Urogenital Tuberculosis in Southern Tunisia: A Review of a 26-Year Period. Germs, 10(3), 150-156. https://doi.org/10.18683/germs.2020.1200




