Introduction
The genus
Prevotella includes both pigmented and nonpigmented bacilli that were previously classified as genus
Bacteroides [
1].
Prevotella bacilli are prevalent in the body as members of the normal flora. However, in some cases they can be involved in infections throughout the body [
2].
Prevotella bivia is a member of a nonpigment group found in the resident flora of the female genital tract and it is occasionally seen in the oral cavity [
3,
4].
P. bivia is associated with infections in the female urogenital tract. The growth of
P. bivia increases during the follicular phase of the menstrual cycle due to the increased levels of estrogen [
3,
5,
6,
7].
P. bivia can be associated with infections in rare locations of the body such as chest wall, intervertebral discs, paronychium and knee joint [
5,
7,
8]. We describe a very rare case of a 39-year-old woman with fulminant generalized peritonitis secondary to purulent salpingitis caused by
P. bivia.
Case report
A 39-year-old woman presented to our emergency department complaining of two days of abdominal pain, vaginal discharge, fever of 38.5 °C and diarrhea. At the onset of pain, she took nonsteroidal anti-inflammatory drugs for temperature and pain relief. The patient had had two deliveries through caesarean section – four and seven years previously, respectively. She was on the 12
th day of her menstrual cycle. She did not have medical history of gynecological problems or any major medical diseases – diabetes mellitus, cardiovascular or renal issues. The abdominal examination revealed pain in the lower abdomen, muscle rigidity and rebound tenderness. During gynecological examination, the patient had pain in the left fallopian tube and cavum Douglasi. Transvaginal sonography showed free fluid in cul-de-sac, thickness and hyperechoic structures on the wall of the left fallopian tube. Laboratory data results revealed leukocytosis accompanied by a left shift, hypoproteinemia, hypoalbuminemia and high levels of fibrinogen. Pelvic inflammatory disease was suspected and after surgical examination, we admitted the patient in the gynecology clinic. Immediately after hospitalization culdocentesis was performed. We aspirated 60 mL purulent material from the cavum Douglasi and sent it for aerobic and anaerobic pathogenic cultures. Initial empirical antimicrobial therapy was initiated immediately: gentamicin (120 mg every 12 h, i.m.), cefazolin (2 g every 12 h, i.v.), metronidazole (500 mg every 8 h, i.v.). Empirical antimicrobial therapy was continued for 48 hours, until microbiological results became available. On the second day the patient got worse: the temperature increased to 39 °C and vomiting, abdominal pain and reduced intestine peristalsis occurred. Abdominal X-ray and surgical examination were ordered to evaluate alimentary tract obstruction or perforation. Abdominal X-ray showed air-fluid levels in the intestine without free gas under the diaphragm. Our conclusion was that she might be suffering from generalized peritonitis due to gynecological pathology. The patient underwent diagnostic laparoscopy. She was informed that there is a possibility for conversion from laparoscopic to open surgery. We performed the open technique method of first port insertion in order to avoid bowel perforation. Intraoperative findings included: around 300 mL purulent fluid and fibrinous adhesions in the peritoneal cavity, small bowel dilation, edematous left fallopian tube and fibrinopurulent exudate on serosa of the appendix, without perforation (
Figure 1).
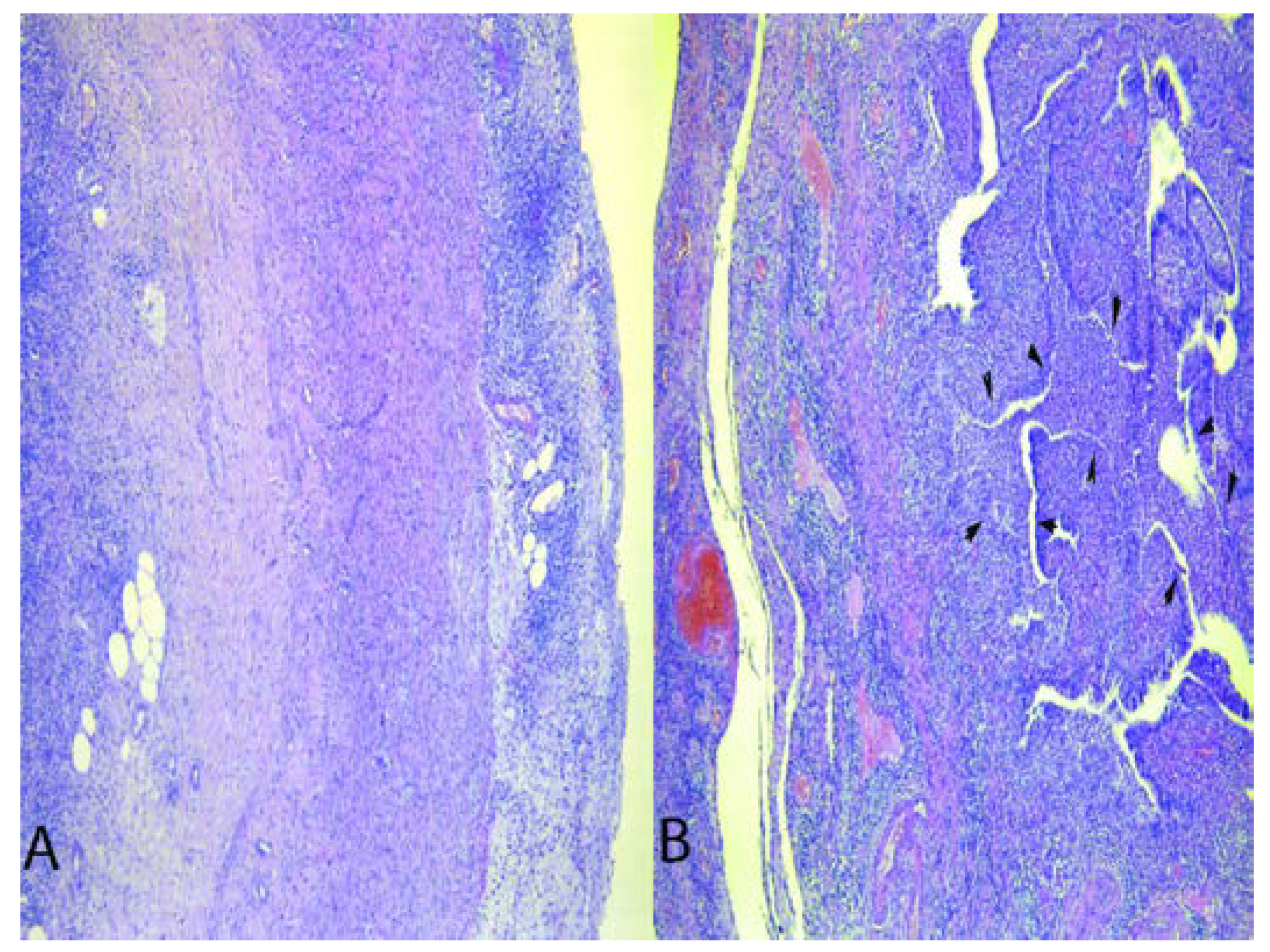
After intraoperative consultation with the surgeon, we decided to perform a median laparotomy to thoroughly explore the abdominal cavity. Liver, gall-bladder and alimentary organs were normal. Left salpingectomy, appendectomy and abdominal peritoneal lavage were performed. We left two drains in the abdominal cavity. Histopathological examination revealed periappendicitis and purulent salpingitis (
Figure 2).
The purulent specimen from cavum Douglasi was inoculated onto Schaedler blood agar and thioglycolate broth. P. bivia was identified on bacterial anaerobic culture test 48 hours later through Vitek 2 system. There was an absence of pathogenic aerobes. P. bivia was found to be metronidazole sensitive. Therefore, the patient continued treatment with a seven-day course of metronidazole (500 mg every 8 h, i.v.). On the next three postoperative days, the patient was subfebrile with normal peristalsis and diuresis. On postoperative day 5 both drainages were removed and the patient felt well. On postoperative day 8, the patient was discharged in good health condition and oral metronidazole 500 mg twice daily for seven days was prescribed. A year and a half after the operation the patient is in good health.
Discussion
Prevotella bivia is a common vaginal commensal, which has been detected in the vaginal epithelia in 40% of healthy women [
4,
9]. In bacterial vaginosis there is a symbiosis between
P. bivia and other anaerobes [
3].
Gardnerella vaginalis biofilm stimulates growth of
P. bivia [
9].
P. bivia is also detected concomitantly with aerobic bacteria [
3]. It has been reported to invade the cervix, causing intrauterine infections with pregnancy complications – preterm labor, premature rupture of membranes, or postpartum endometritis [
4]. In gynecology,
P. bivia causes bacterial vaginosis, endometritis and pelvic inflammatory disease [
4,
5,
8]. Several unusual gynecological cases associated with
P. bivia have been reported. Sang-Min Shim reported a case of a 40-year-old woman with a 6 cm abscess on the cuff two months after laparoscopic supracervical hysterectomy.
P. bivia was identified on bacterial culture test. He concluded that clinicians should be aware of the possibility of
P. bivia infections despite their rarity.
4 Purushothaman and colleagues described a case of spondylodiscitis caused by the anaerobe
Prevotella that indicated the underlying diagnosis of serous cystadenofibroma of the ovaries. They concluded that the genitourinary system should be inspected if a musculoskeletal infection is caused by
Prevotella [
8].
P. bivia can be associated with infections in atypical locations of the body. Hsu and colleagues reported a case of a chest wall abscess due to
P. bivia [
7]. Mirza described two cases of mixed infections of the paronychium with
P. bivia [
5]. Cases of fasciitis, osteomyelitis, septic arthritis of the knee joint, all caused by
P. bivia have been described [
5].
A diagnosis of
P. bivia requires starting the culture within 1 hour after sampling [
2,
3]. For rapid detection of
Prevotella, both direct and indirect fluorescent antibody techniques may be an option [
2]. Initial empiric antibiotic therapy should be administered immediately as microbiological results do not become available for 24 to 72 hours. There is no utilized consensus for the optimal antimicrobial treatment of
P. bivia infections [
5,
7]. Studies have reported that clindamycin, amoxicillin/clavulanate, metronidazole, and imipenem are effective against
P. bivia [
2,
5,
7,
10]. One-third to one-half of
Prevotella strains are resistant to tetracyclines, ciprofloxacin, and most
P. bivia strains are β- lactamase positive [
1,
7]. If antibiotic treatment fails, surgery should be performed. This includes drainage of abscesses and/or excision of necrotic tissue [
1].
In our survey from literature, we did not find a case of generalized peritonitis secondary to purulent salpingitis caused by
P. bivia. It is suggested that sex steroids regulate the growth of this microbe as
P. bivia increases during the follicular phase of the menstrual cycle [
3]. Our case seems to confirm this, as the patient’s symptoms started during the follicular phase of the menstrual cycle. Mimako observed
P. bivia in a rat pyometra model. He concluded that in a mixed infection (
P. bivia and aerobes), the rate of inflammatory change of the uterus was higher than in a sole infection with
P. bivia [
6]. In most cases described,
P. bivia was mixed with aerobes and caused bacterial vaginosis and pelvic inflammatory disease, whereas in our case study
P. bivia was the only microbe that was isolated. The infection was fulminant and caused generalized peritonitis. Rapid and systemic infections typically occur in immunocompromised hosts, however our patient was in good health condition and immunocompetent [
7,
10]. We cannot explain the fulminant infection in our case study. Nevertheless, we can conclude that multidisciplinary team management is crucial for managing the infection.