Comparison of Clinical Outcomes between Salvage and Elective Thoracic Endovascular Aortic Repair in Patients with Advanced Esophageal Cancer with Aortic Invasion: A Retrospective Cohort Study
Abstract
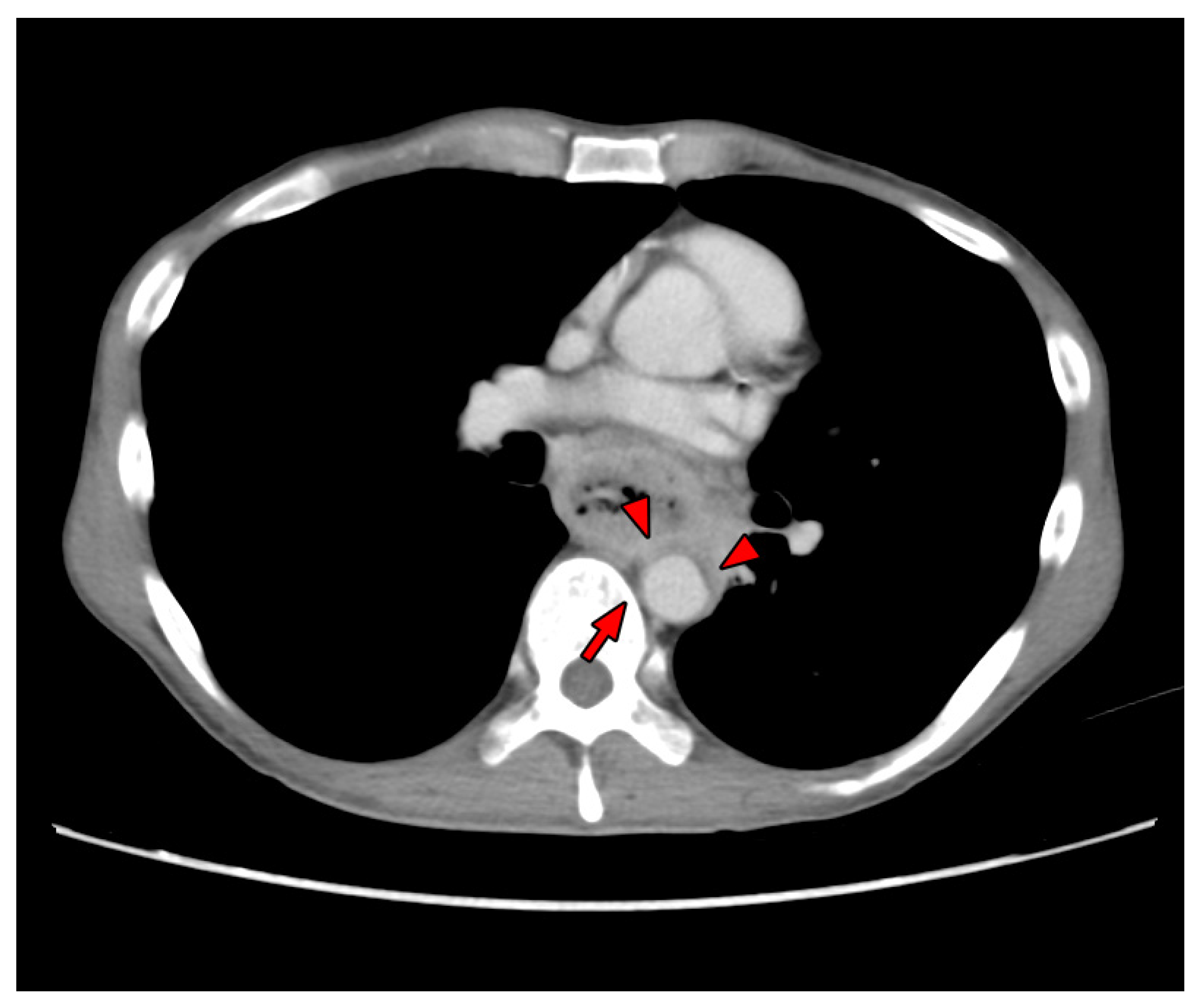
:1. Introduction
2. Materials and Methods
2.1. Data Collection
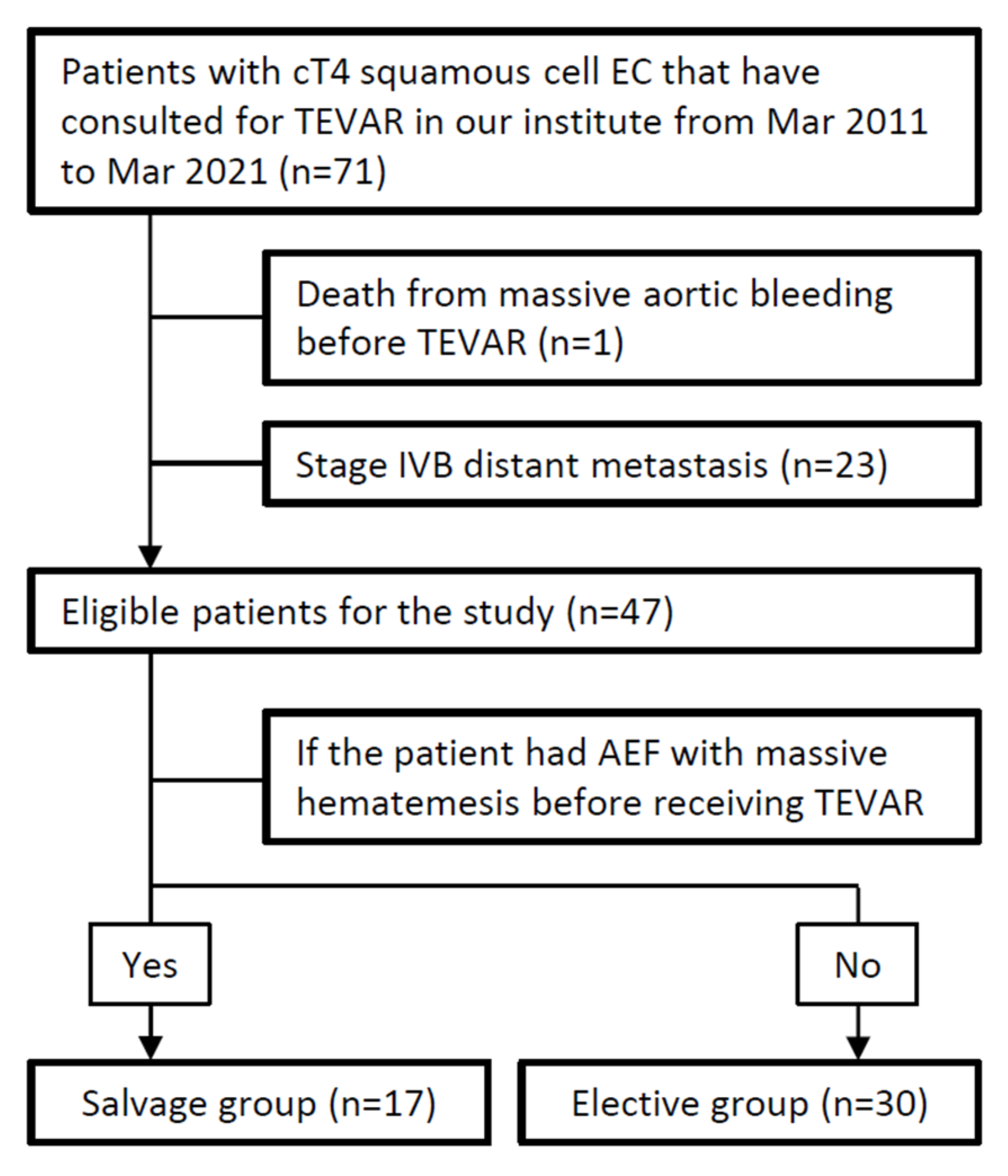
2.2. Study Design
2.3. TEVAR Procedure and Post-Procedural Management
2.4. Study Outcome
2.5. Statistical Analysis
3. Results
3.1. Patient Characteristics
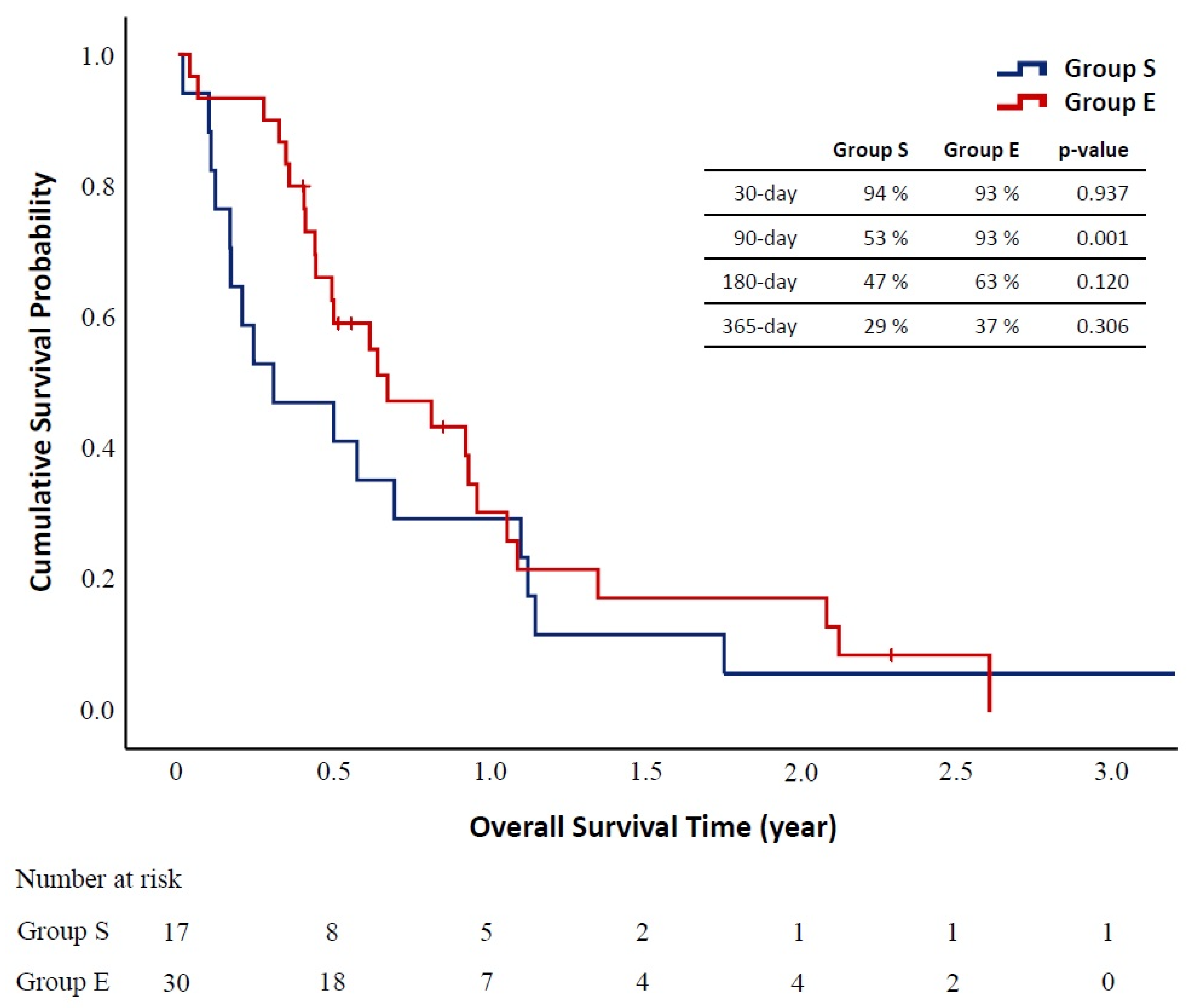
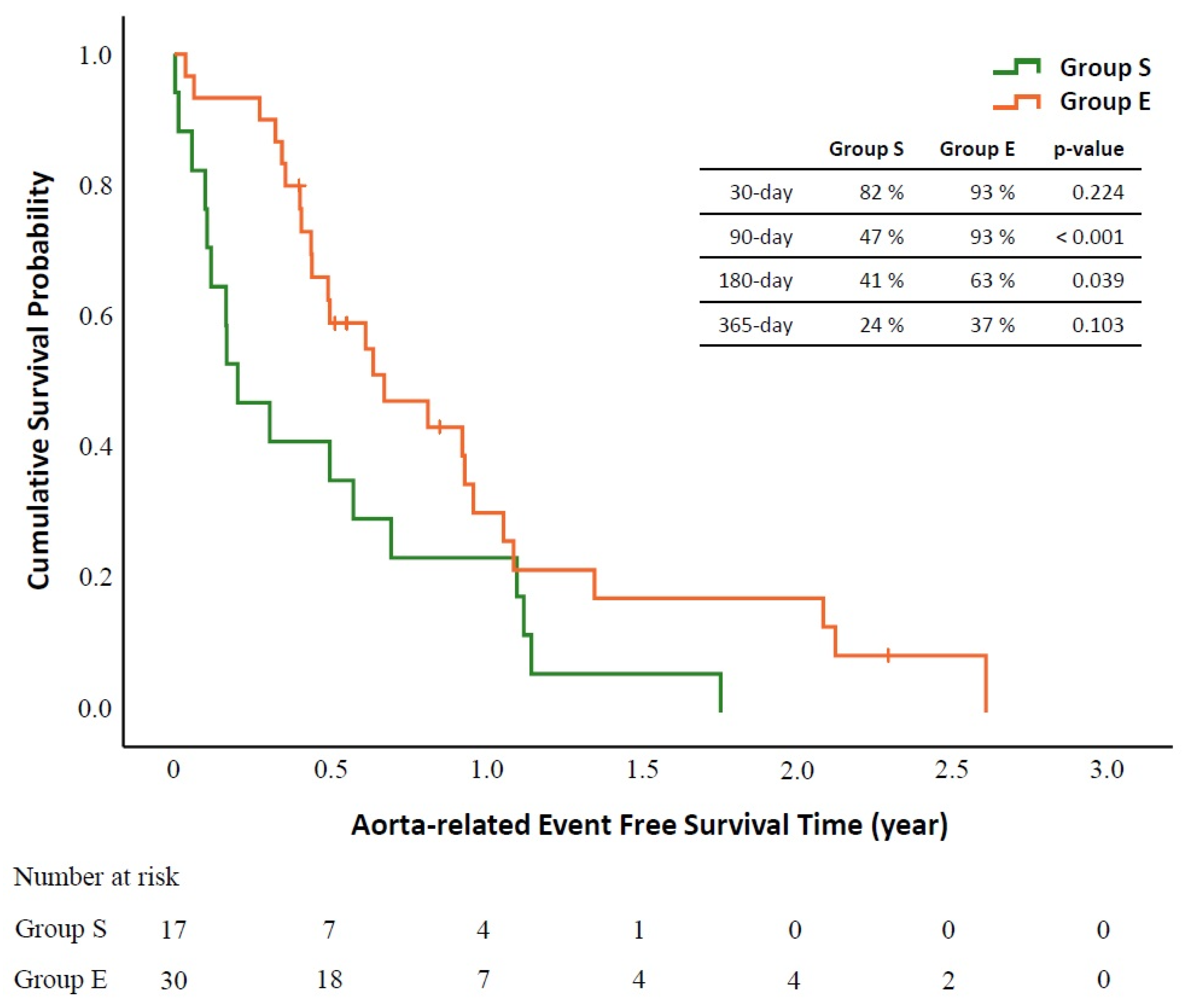
3.2. Primary Outcomes
3.3. Secondary Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mezzetto, L.; Scorsone, L.; De Pasqual, C.A.; Weindelmayer, J.; Giacopuzzi, S.; De Manzoni, G.; Veraldi, G.F.; Luca, M.; Lorenzo, S.; Alberto, D.P.C.; et al. Preliminary Experience with Prophylactic Thoracic Endovascular Aortic Repair in Patients Affected by Advanced Esophageal Cancer. Ann. Vasc. Surg. 2019, 61, 142–147. [Google Scholar] [CrossRef] [PubMed]
- Taniguchi, H.; Yamazaki, K.; Boku, N.; Funakoshi, T.; Hamauchi, S.; Tsushima, T.; Todaka, A.; Sakamoto, T.; Tomita, H.; Machida, N.; et al. Risk factors and clinical courses of chemoradiation-related arterio-esophageal fistula in esophageal cancer patients with clinical invasion of the aorta. Int. J. Clin. Oncol. 2011, 16, 359–365. [Google Scholar] [CrossRef] [PubMed]
- Rice, T.W.; Patil, D.T.; Blackstone, E.H. 8th edition AJCC/UICC staging of cancers of the esophagus and esophagogastric junction: Application to clinical practice. Ann. Cardiothorac. Surg. 2017, 6, 119–130. [Google Scholar] [CrossRef] [Green Version]
- Chen, K.-C.; Wu, I.-H.; Chang, C.-Y.; Huang, P.-M.; Lin, M.-W.; Lee, J.-M. The Long-Term Clinical Impact of Thoracic Endovascular Aortic Repair (TEVAR) for Advanced Esophageal Cancer Invading Aorta. Ann. Surg. Oncol. 2021, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Yokota, T.; Kato, K.; Hamamoto, Y.; Tsubosa, Y.; Ogawa, H.; Ito, Y.; Hara, H.; Ura, T.; Kojima, T.; Chin, K.; et al. Phase II study of chemoselection with docetaxel plus cisplatin and 5-fluorouracil induction chemotherapy and subsequent conversion surgery for locally advanced unresectable oesophageal cancer. Br. J. Cancer 2016, 115, 1328–1334. [Google Scholar] [CrossRef]
- de Manzoni, G.; Pedrazzani, C.; Pasini, F.; Bernini, M.; Minicozzi, A.M.; Giacopuzzi, S.; Grandinetti, A.; Cordiano, C. Chemoradiotherapy followed by surgery for squamous cell carcinoma of the thoracic esophagus with clinical evidence of adjacent organ invasion. J. Surg. Oncol. 2007, 95, 261–266. [Google Scholar] [CrossRef] [PubMed]
- Akiyama, Y.; Iwaya, T.; Endo, F.; Nikai, H.; Baba, S.; Chiba, T.; Kimura, T.; Takahara, T.; Otsuka, K.; Nitta, H.; et al. Safety of thoracoscopic esophagectomy after induction chemotherapy for locally advanced unresectable esophageal squamous cell carcinoma. Asian J. Endosc. Surg. 2019, 13, 152–159. [Google Scholar] [CrossRef]
- Watanabe, M.; Nakajima, M.; Nishikawa, K.; Kato, H.; Matsubara, H. Thoracic endovascular aortic repair for esophageal cancer invading the thoracic aorta: A questionnaire survey study. Esophagus 2019, 17, 74–80. [Google Scholar] [CrossRef]
- Shimizu, H.; Okada, M.; Tangoku, A.; Doki, Y.; Endo, S.; Fukuda, H.; Hirata, Y.; Iwata, H.; Kobayashi, J.; Kumamaru, H.; et al. Thoracic and cardiovascular surgeries in Japan during 2017. Gen. Thorac. Cardiovasc. Surg. 2020, 68, 414–449. [Google Scholar] [CrossRef] [Green Version]
- Yamatsuji, T.; Naomoto, Y.; Shirakawa, Y.; Gunduz, M.; Hiraki, T.; Yasui, K.; Kawata, M.; Hanazaki, M.; Morita, K.; Sano, S.; et al. Intra-aortic stent graft in oesophageal carcinoma invading the aorta. Prophylaxis for fatal haemorrhage. Int. J. Clin. Pract. 2006, 60, 1600–1603. [Google Scholar] [CrossRef]
- Nakajima, M.; Muroi, H.; Kikuchi, M.; Yamaguchi, S.; Sasaki, K.; Tsuchioka, T.; Takei, Y.; Shibasaki, I.; Fukuda, H.; Kato, H. Salvage esophagectomy combined with partial aortic wall resection following thoracic endovascular aortic repair. Gen. Thorac. Cardiovasc. Surg. 2018, 66, 736–743. [Google Scholar] [CrossRef]
- Chakfé, N.; Diener, H.; Lejay, A.; Assadian, O.; Berard, X.; Caillon, J.; Fourneau, I.; Glaudemans, A.; Koncar, I.; Lindholt, J.; et al. Editor’s Choice—European Society for Vascular Surgery (ESVS) 2020 Clinical Practice Guidelines on the Management of Vascular Graft and Endograft Infections. Eur. J. Vasc. Endovasc. Surg. 2020, 59, 339–384. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Czerny, M.; Eggebrecht, H.; Sodeck, G.; Weigang, E.; Livi, U.; Verzini, F.; Schmidli, J.; Chiesa, R.; Melissano, G.; Kahlberg, A.L.; et al. New insights regarding the incidence, presentation and treatment options of aorto-oesophageal fistulation after thoracic endovascular aortic repair: The European Registry of Endovascular Aortic Repair Complications. Eur. J. Cardio-Thoracic Surg. 2013, 45, 452–457. [Google Scholar] [CrossRef] [Green Version]
- Chiesa, R.; Melissano, G.; Marone, E.M.; Marrocco-Trischitta, M.M.; Kahlberg, A.L. Aorto-oesophageal and Aortobronchial Fistulae Following Thoracic Endovascular Aortic Repair: A National Survey. Eur. J. Vasc. Endovasc. Surg. 2010, 39, 273–279. [Google Scholar] [CrossRef] [Green Version]
- Eggebrecht, H.; Mehta, R.H.; Dechene, A.; Tsagakis, K.; Kühl, H.; Huptas, S.; Gerken, G.; Jakob, H.G.; Erbel, R. Aortoesophageal Fistula After Thoracic Aortic Stent-Graft Placement: A Rare but Catastrophic Complication of a Novel Emerging Technique. JACC Cardiovasc. Interv. 2009, 2, 570–576. [Google Scholar] [CrossRef] [Green Version]
- Smeds, M.R.; Duncan, A.A.; Harlander-Locke, M.P.; Lawrence, P.F.; Lyden, S.; Fatima, J.; Eskandari, M.K.; Steenberge, S.P.; Tomita, T.M.; Morasch, M.; et al. Treatment and outcomes of aortic endograft infection. J. Vasc. Surg. 2016, 63, 332–340. [Google Scholar] [CrossRef] [Green Version]
- Agha, R.; Abdall-Razak, A.; Crossley, E.; Dowlut, N.; Iosifidis, C.; Mathew, G.; Beamishaj; Bashashati, M.; Millham, F.H.; Orgill, D.P.; et al. STROCSS 2019 Guideline: Strengthening the reporting of cohort studies in surgery. Int. J. Surg. 2019, 72, 156–165. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.; Chen, H.; Wu, S.; Chen, H.; Hung, W.; Lin, C.; Wang, B. Esophageal squamous cell carcinoma and prognosis in Taiwan. Cancer Med. 2018, 7, 4193–4201. [Google Scholar] [CrossRef] [PubMed]
- Delpisheh, A.; Veisani, Y.; Sayehmiri, K.; Rahimi, E. Esophageal carcinoma: Long-term survival in consecutive series of patients through a retrospective cohort study. Gastroenterol. Hepatol. Bed Bench 2014, 7, 101–107. [Google Scholar]
- Picus, D.; Balfe, D.M.; Koehler, R.E.; Roper, C.L.; Owen, J.W. Computed tomography in the staging of esophageal carcinoma. Radiology 1983, 146, 433–438. [Google Scholar] [CrossRef]
- Hong, S.J.; Kim, T.J.; Nam, K.B.; Lee, I.S.; Yang, H.C.; Cho, S.; Kim, K.; Jheon, S.; Lee, K.W. New TNM Staging System for Esophageal Cancer: What Chest Radiologists Need to Know. RadioGraphics 2014, 34, 1722–1740. [Google Scholar] [CrossRef] [PubMed]
- Kawakami, T.; Tsushima, T.; Omae, K.; Ogawa, H.; Shirasu, H.; Kito, Y.; Yoshida, Y.; Hamauchi, S.; Todaka, A.; Machida, N.; et al. Risk factors for esophageal fistula in thoracic esophageal squamous cell carcinoma invading adjacent organs treated with definitive chemoradiotherapy: A monocentric case-control study. BMC Cancer 2018, 18, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, A.; Kanaoka, Y.; Baba, T.; Takizawa, R.; Hara, M.; Maeda, K.; Nishikawa, K.; Suzuki, Y.; Yanaga, K.; Ohki, T. Result of Thoracic Endovascular Aortic Repair for Patients with Esophageal Cancer. World J. Surg. 2017, 42, 1551–1558. [Google Scholar] [CrossRef] [PubMed]
- Shinoda, M.; Ando, N.; Kato, K.; Ishikura, S.; Kato, H.; Tsubosa, Y.; Minashi, K.; Okabe, H.; Kimura, Y.; Kawano, T.; et al. Randomized study of low-dose versus standard-dose chemoradiotherapy for unresectable esophageal squamous cell carcinoma (JCOG0303). Cancer Sci. 2015, 106, 407–412. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Total (n = 47) | Salvage Group (n = 17) | Elective Group (n = 30) | p-Value | |
|---|---|---|---|---|
| Age (years) * | 61 (36–80) | 57 (38–71) | 62 (36–80) | 0.249 |
| BMI (kg/m2) * | 20.7 (13.0–27.2) | 20.7 (16.6–27.2) | 20.7 (13.0–26.9) | 0.603 |
| Sex | 0.294 | |||
| Male | 44 (94%) | 15 (88%) | 29 (97%) | |
| Female | 3 (6%) | 2 (12%) | 1 (3%) | |
| ECOG | 0.597 | |||
| 0 | 18 (38%) | 4 (24%) | 14 (47%) | |
| 1 | 15 (32%) | 6 (35%) | 9 (30%) | |
| 2 | 6 (13%) | 3 (18%) | 3 (10%) | |
| 3 | 6 (13%) | 3 (18%) | 3 (10%) | |
| 4 | 2 (4%) | 1 (6%) | 1 (3%) | |
| Substance use | ||||
| Alcohol | 36 (77%) | 12 (71%) | 24 (80%) | 0.349 |
| Betel nut | 18 (38%) | 6 (35%) | 12 (40%) | 0.750 |
| Cigarette | 38 (81%) | 13 (76%) | 25 (83%) | 0.417 |
| Tumor Location | 0.255 | |||
| Upper Third | 5 (11%) | 3 (18%) | 2 (7%) | |
| Upper and Middle Third | 6 (13%) | 4 (24%) | 2 (7%) | |
| Middle Third | 18 (38%) | 5 (29%) | 13 (43%) | |
| Middle and Lower Third | 8 (17%) | 3 (18%) | 5 (17%) | |
| Lower Third | 10 (21%) | 2 (12%) | 8 (27%) | |
| Comorbidity | ||||
| Coronary artery disease | 3 (6%) | 1 (6%) | 2 (7%) | 0.706 |
| Chronic kidney disease | 3 (6%) | 2 (12%) | 1 (3%) | 0.294 |
| Diabetes mellitus | 5 (11%) | 4 (24%) | 1 (3%) | 0.051 |
| Hypertension | 21 (45%) | 6 (35%) | 15 (50%) | 0.253 |
| Liver cirrhosis | 7 (15%) | 5 (29%) | 2 (7%) | 0.049 |
| COPD | 5 (11%) | 1 (6%) | 4 (13%) | 0.397 |
| Cerebrovascular accident | 1 (2%) | 0 | 1 (3%) | 0.638 |
| Others | 7 (15%) | 3 (18%) | 4 (13%) | 0.499 |
| Pre-TEVAR treatment | ||||
| Chemoradiotherapy | 18 (38%) | 12 (71%) | 6 (20%) | 0.001 |
| Esophagectomy | 2 (4%) | 2 (12%) | 0 | 0.126 |
| Total (n = 47) | Salvage Group (n = 17) | Elective Group (n = 30) | p-Value | |
|---|---|---|---|---|
| Post-TEVAR Treatment | ||||
| Chemoradiotherapy | 34 (72%) | 9 (53%) | 25 (83%) | 0.025 |
| Esophagectomy | 22 (47%) | 4 (24%) | 18 (60%) | 0.017 |
| Post-TEVAR Complications | 9 (19%) | 8 (47%) | 1 (3%) | <0.001 |
| Recurrent AEF Hemorrhage | 2 (4%) | 2 (12%) | 0 | |
| Tumor bleeding | 2 (4%) | 2 (12%) | 0 | |
| Endograft Infection | 3 (6%) | 3 (18%) | 0 | |
| Hypoperfusion-related Irreversible Organ Failure | 1 (2%) | 1 (6%) | 0 | |
| Hypoperfusion-related Reversible Organ Dysfunction | 3 (6%) | 2 (12%) | 1 (3%) | |
| Neurological Complication # | 0 | 0 | 0 | |
| Post-TEVAR Index Hospital Stay (days) * | 12 (1–124) | 16 (3–124) | 11 (1–100) | 0.061 |
| Device | 0.105 | |||
| C-TAG®, Gore® | 24 (51%) | 12 (71%) | 12 (40%) | |
| Valiant™, Medtronic | 21 (45%) | 5 (29%) | 16 (53%) | |
| Zenith Alpha™, Cook | 2 (4%) | 0 | 2 (7%) | |
| Proximal Landing zone | 0.005 | |||
| Zone 2 | 5 (11%) | 3 (18%) | 2 (7%) | |
| Zone 3 | 19 (40%) | 11 (65%) | 8 (27%) | |
| Zone 4 | 23 (49%) | 3 (18%) | 20 (67%) | |
| TEVAR length (cm) * | 15.0 (10.0–19.0) | 15.0 (10.0–19.0) | 15.0 (10.0–19.0) | 0.653 |
| TEVAR diameter | ||||
| Proximal (mm) * | 31 (24–38) | 31 (26–37) | 31 (24–38) | 0.712 |
| Distal (mm) * | 28 (21–38) | 26 (21–34) | 28 (24–38) | 0.092 |
| Concomitant procedure | ||||
| Total LSCA procedure | 5 (11%) | 3 (18%) | 2 (7%) | 0.336 |
| LSCA revascularization | 4 (4%) | 2 (12%) | 2 (7%) | |
| LSCA embolization | 1 (2%) | 1 (6%) | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, S.-H.; Lee, J.-M.; Wu, I.-H. Comparison of Clinical Outcomes between Salvage and Elective Thoracic Endovascular Aortic Repair in Patients with Advanced Esophageal Cancer with Aortic Invasion: A Retrospective Cohort Study. Biomedicines 2021, 9, 1889. https://doi.org/10.3390/biomedicines9121889
Lin S-H, Lee J-M, Wu I-H. Comparison of Clinical Outcomes between Salvage and Elective Thoracic Endovascular Aortic Repair in Patients with Advanced Esophageal Cancer with Aortic Invasion: A Retrospective Cohort Study. Biomedicines. 2021; 9(12):1889. https://doi.org/10.3390/biomedicines9121889
Chicago/Turabian StyleLin, Sian-Han, Jang-Ming Lee, and I-Hui Wu. 2021. "Comparison of Clinical Outcomes between Salvage and Elective Thoracic Endovascular Aortic Repair in Patients with Advanced Esophageal Cancer with Aortic Invasion: A Retrospective Cohort Study" Biomedicines 9, no. 12: 1889. https://doi.org/10.3390/biomedicines9121889
APA StyleLin, S.-H., Lee, J.-M., & Wu, I.-H. (2021). Comparison of Clinical Outcomes between Salvage and Elective Thoracic Endovascular Aortic Repair in Patients with Advanced Esophageal Cancer with Aortic Invasion: A Retrospective Cohort Study. Biomedicines, 9(12), 1889. https://doi.org/10.3390/biomedicines9121889






