A Systematic Review and Meta-Analysis of the Effect of Pentagalloyl Glucose Administration on Aortic Expansion in Animal Models
Abstract
1. Introduction
2. Methods
2.1. Search Strategy and Eligibility Criteria
2.2. Data Extraction
2.3. Risk of Bias
2.4. Data Analysis
3. Results
3.1. Included Studies
3.2. Risk of Bias of Included Studies
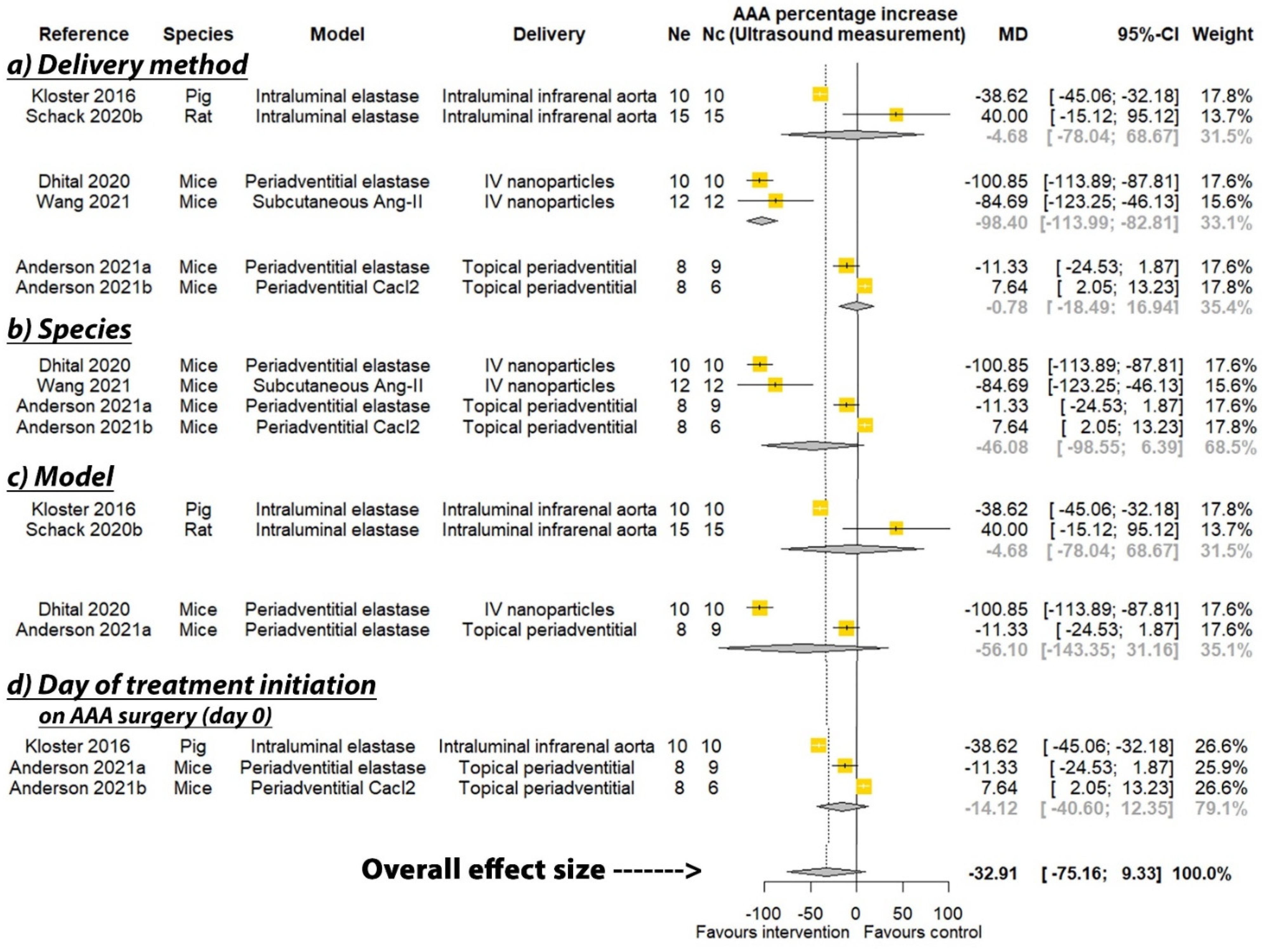
3.3. Effect of PGG on Aortic Expansion
3.4. Effect of PGG on Final AAA Diameter
3.5. Effect of PGG on AAA Incidence
3.6. Findings from Histological and Molecular Biology Analyses
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Correction Statement
References
- Abubakar, I.; Tillmann, T.; Banerjee, A. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015, 385, 117–171. [Google Scholar]
- Chaikof, E.L.; Dalman, R.L.; Eskandari, M.K.; Jackson, B.M.; Lee, W.A.; Mansour, M.A.; Mastracci, T.M.; Mell, M.; Murad, M.H.; Nguyen, L.L. The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J. Vasc. Surg. 2018, 67, 2–77.e2. [Google Scholar] [CrossRef]
- Wanhainen, A.; Verzini, F.; Van Herzeele, I.; Allaire, E.; Bown, M.; Cohnert, T.; Dick, F.; van Herwaarden, J.; Karkos, C.; Koelemay, M. Editor’s choice–European society for vascular surgery (ESVS) 2019 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur. J. Vasc. Endovasc. Surg. 2019, 57, 8–93. [Google Scholar] [CrossRef] [PubMed]
- Filardo, G.; Powell, J.T.; Martinez, M.A.M.; Ballard, D.J. Surgery for small asymptomatic abdominal aortic aneurysms. Cochrane Database Syst. Rev. 2015. [Google Scholar] [CrossRef] [PubMed]
- Lederle, F.A.; Johnson, G.R.; Wilson, S.E.; Ballard, D.J.; Jordan, W.D., Jr.; Blebea, J.; Littooy, F.N.; Freischlag, J.A.; Bandyk, D.; Rapp, J.H. Rupture rate of large abdominal aortic aneurysms in patients refusing or unfit for elective repair. JAMA 2002, 287, 2968–2972. [Google Scholar] [CrossRef] [PubMed]
- Golledge, J.; Moxon, J.V.; Singh, T.P.; Bown, M.J.; Mani, K.; Wanhainen, A. Lack of an effective drug therapy for abdominal aortic aneurysm. J. Intern. Med. 2020, 288, 6–22. [Google Scholar] [CrossRef] [PubMed]
- Golledge, J. Abdominal aortic aneurysm: Update on pathogenesis and medical treatments. Nat. Rev. Cardiol. 2019, 16, 225–242. [Google Scholar] [CrossRef] [PubMed]
- Golledge, J.; Singh, T.P. Effect of blood pressure lowering drugs and antibiotics on abdominal aortic aneurysm growth: A systematic review and meta-analysis. Heart 2021, 107, 1465–1471. [Google Scholar] [CrossRef] [PubMed]
- Patnaik, S.S.; Simionescu, D.T.; Goergen, C.J.; Hoyt, K.; Sirsi, S.; Finol, E.A. Pentagalloyl Glucose and Its Functional Role in Vascular Health: Biomechanics and Drug-Delivery Characteristics. Ann. Biomed. Eng. 2019, 47, 39–59. [Google Scholar] [CrossRef] [PubMed]
- Schack, A.S.; Stubbe, J.; Steffensen, L.B.; Mahmoud, H.; Laursen, M.S.; Lindholt, J.S. Intraluminal infusion of Penta-Galloyl Glucose reduces abdominal aortic aneurysm development in the elastase rat model. PLoS ONE 2020, 15, e0234409. [Google Scholar] [CrossRef]
- Dhital, S.; Vyavahare, N.R. Nanoparticle-based targeted delivery of pentagalloyl glucose reverses elastase-induced abdominal aortic aneurysm and restores aorta to the healthy state in mice. PLoS ONE 2020, 15, e0227165. [Google Scholar] [CrossRef] [PubMed]
- Nosoudi, N.; Chowdhury, A.; Siclari, S.; Parasaram, V.; Karamched, S.; Vyavahare, N. Systemic Delivery of Nanoparticles Loaded with Pentagalloyl Glucose Protects Elastic Lamina and Prevents Abdominal Aortic Aneurysm in Rats. J. Cardiovasc. Transl. Res. 2016, 9, 445–455. [Google Scholar] [CrossRef] [PubMed]
- Isenburg, J.C.; Simionescu, D.T.; Starcher, B.C.; Vyavahare, N.R. Elastin stabilization for treatment of abdominal aortic aneurysms. Circulation 2007, 115, 1729–1737. [Google Scholar] [CrossRef] [PubMed]
- Anderson, J.L.; Niedert, E.E.; Patnaik, S.S.; Tang, R.; Holloway, R.L.; Osteguin, V.; Finol, E.A.; Goergen, C.J. Animal Model Dependent Response to Pentagalloyl Glucose in Murine Abdominal Aortic Injury. J. Clin. Med. 2021, 10, 219. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Hooijmans, C.R.; Rovers, M.M.; de Vries, R.B.; Leenaars, M.; Ritskes-Hoitinga, M.; Langendam, M.W. SYRCLE’s risk of bias tool for animal studies. BMC Med. Res. Methodol. 2014, 14, 43. [Google Scholar] [CrossRef] [PubMed]
- Phie, J.; Thanigaimani, S.; Golledge, J. Systematic Review and Meta-Analysis of Interventions to Slow Progression of Abdominal Aortic Aneurysm in Mouse Models. Arter. Thromb. Vasc. Biol. 2021, 41, 1504–1517. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Savovic, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Sterne, J.A.; Gavaghan, D.; Egger, M. Publication and related bias in meta-analysis: Power of statistical tests and prevalence in the literature. J. Clin. Epidemiol. 2000, 53, 1119–1129. [Google Scholar] [CrossRef]
- Kulinskaya, E.; Morgenthaler, S.; Staudte, R.G. Combining Statistical Evidence. Int. Stat. Rev. 2014, 82, 214–242. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Arnold, F.; Muzzio, N.; Patnaik, S.S.; Finol, E.A.; Romero, G. Pentagalloyl Glucose-Laden Poly(lactide-co-glycolide) Nanoparticles for the Biomechanical Extracellular Matrix Stabilization of an In Vitro Abdominal Aortic Aneurysm Model. ACS Appl. Mater. Interfaces 2021, 13, 25771–25782. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Parasaram, V.; Dhital, S.; Nosoudi, N.; Hasanain, S.; Lane, B.A.; Lessner, S.M.; Eberth, J.F.; Vyavahare, N.R. Systemic delivery of targeted nanotherapeutic reverses angiotensin II-induced abdominal aortic aneurysms in mice. Sci. Rep. 2021, 11, 8584. [Google Scholar] [CrossRef] [PubMed]
- Nosoudi, N.; Chowdhury, A.; Siclari, S.; Karamched, S.; Parasaram, V.; Parrish, J.; Gerard, P.; Vyavahare, N. Reversal of Vascular Calcification and Aneurysms in a Rat Model Using Dual Targeted Therapy with EDTA- and PGG-Loaded Nanoparticles. Theranostics 2016, 6, 1975–1987. [Google Scholar] [CrossRef]
- Kloster, B.O.; Lund, L.; Lindholt, J.S. Inhibition of early AAA formation by aortic intraluminal pentagalloyl glucose (PGG) infusion in a novel porcine AAA model. Ann. Med. Surg. 2016, 7, 65–70. [Google Scholar] [CrossRef] [PubMed]
- Golledge, J.; Pinchbeck, J.; Tomee, S.M.; Rowbotham, S.E.; Singh, T.P.; Moxon, J.V.; Jenkins, J.S.; Lindeman, J.H.; Dalman, R.L.; McDonnell, L.; et al. Randomised-controlled trial testing the efficacy of telmisartan to slow growth of small abdominal aortic aneurysms. JAMA Cardiol. 2020, 5, 1374–1381. [Google Scholar] [CrossRef]
- Moxon, J.V.; Rowbotham, S.E.; Pinchbeck, J.L.; Lazzaroni, S.M.; Morton, S.K.; Moran, C.S.; Quigley, F.; Jenkins, J.S.; Reid, C.M.; Cavaye, D.; et al. A Randomised Controlled Trial Assessing the Effects of Peri-operative Fenofibrate Administration on Abdominal Aortic Aneurysm Pathology: Outcomes From the FAME Trial. Eur. J. Vasc. Endovasc. Surg. 2020, 60, 452–460. [Google Scholar] [CrossRef]
- Pinchbeck, J.L.; Moxon, J.V.; Rowbotham, S.E.; Bourke, M.; Lazzaroni, S.; Morton, S.K.; Matthews, E.O.; Hendy, K.; Jones, R.E.; Bourke, B.; et al. Randomized Placebo-Controlled Trial Assessing the Effect of 24-Week Fenofibrate Therapy on Circulating Markers of Abdominal Aortic Aneurysm: Outcomes From the FAME-2 Trial. J. Am. Heart Assoc. 2018, 7, e009866. [Google Scholar] [CrossRef]
- Pavey, S.N.; Cocciolone, A.J.; Marty, A.G.; Ismail, H.N.; Hawes, J.Z.; Wagenseil, J.E. Pentagalloyl glucose (PGG) partially prevents arterial mechanical changes due to elastin degradation. Exp. Mech. 2021, 61, 41–51. [Google Scholar] [CrossRef]
- Patnaik, S.S.; Piskin, S.; Pillalamarri, N.R.; Romero, G.; Escobar, G.P.; Sprague, E.; Finol, E.A. Biomechanical Restoration Potential of Pentagalloyl Glucose after Arterial Extracellular Matrix Degeneration. Bioengineering 2019, 6, 58. [Google Scholar] [CrossRef]
- Golledge, J.; Wolanski, P.; Parr, A.; Buttner, P. Measurement and determinants of infrarenal aortic thrombus volume. Eur. Radiol. 2008, 18, 1987–1994. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Khan, S.; Salata, K.; Hussain, M.A.; de Mestral, C.; Greco, E.; Aljabri, B.A.; Forbes, T.L.; Verma, S.; Al-Omran, M. A systematic review and meta-analysis of the long-term outcomes of endovascular versus open repair of abdominal aortic aneurysm. J. Vasc. Surg. 2019, 70, 954–969.e30. [Google Scholar] [CrossRef] [PubMed]



| Model | Animals | Age (Months) | Sex | Sample Size † | Sample Size ‡ | Modality * | Aortic Diameter Measurement Protocol | Reference |
|---|---|---|---|---|---|---|---|---|
| Periadventitial infrarenal aortic elastase | C57BL/6 mice | NR | M | 10 | 10 | Ultrasound Photographs of excised aortas (end) and in situ measurements at laparotomy (start) | Systolic maximum inner to inner diameter Maximum outer to outer diameter | [11] |
| Angiotensin II infusion subcutaneously | LDLR−/− mice | 2 | M | 12 | 12 | Ultrasound | Inner to inner aortic diameter | [23] |
| Intraluminal infrarenal aortic elastase | Sprague-Dawley rats | NR | M | 9 | 10 | Photographs of in situ aortas | Maximum outer to outer diameter | [10]a |
| Intraluminal infrarenal aortic elastase | Sprague-Dawley rats | NR | M | 15 ** | 15 ** | Ultrasound Photographs of in situ aortas | Maximum inner to inner anterior posterior aortic diameter Maximum outer to outer diameter | [10]b |
| Periadventitial infrarenal aortic calcium chloride | Sprague-Dawley rats | 1 | M | 6 | 6 | Photographs of aortas | Maximum outer to outer diameter | [24] |
| Periadventitial infrarenal aortic calcium chloride | Sprague-Dawley rats | 1 | M | 6 | 6 | Photographs of in situ aortas | Maximum outer to outer diameter | [12] |
| Periadventitial infrarenal aortic calcium chloride | Sprague-Dawley rats | NR | F | 11 | 12 | Photographs of in situ aortas | Maximum outer to outer diameter | [13]a |
| Periadventitial infrarenal aortic calcium chloride | Sprague-Dawley rats | NR | F | 11 | 12 | Photographs of in situ aortas | Maximum outer to outer diameter | [13]b |
| Intraluminal infrarenal aortic elastase following balloon dilatation and juxtarenal stenosing cuff | Danish Landrace pigs | NR | F | 10 | 10 | Ultrasound | Maximum outer to outer anterior posterior aortic diameter measured in transverse and longitudinal plane | [25] |
| Periadventitial infrarenal aortic elastase | C57BL/6 mice | 2–3.5 | NR | 8 | 9 | Ultrasound | Inner to inner diameter during systole | [14]a |
| Periadventitial infrarenal aortic calcium chloride | C57BL/6 mice | 2–3.5 | NR | 8 | 6 | Ultrasound | Inner to inner diameter during systole | [14]b |
| Group | Dose | Mode of Delivery | Intervention Commenced † | Duration of Follow-Up ‡ | Direct Aortic Percentage | p | Direct Aortic Diameter ⸶ | p | Ultrasound Aortic Percentage | p | Ultrasound Aortic Diameter ⸷ | p Value | AAA Development, n (%) | Reference |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | 3 mg PGG in 10 mg/kg nanoparticle (on day 14 and 21) | Intravenous | 14 | 14 | 24.78 ± 15.62 * | <0.0001 | NR | 9.69 ± 5.24 * | <0.0001 | NR | NR | [11] | ||
| Control | No administration | NA | NA | 14 | 144.27 ± 28.18 * | NR | 110.54 ± 20.37 * | NR | NR | |||||
| Intervention | PGG in 10 mg/kg nanoparticles (on day 28 and 42) | Intravenous | 28 | 28 | NR | NR | 97.75 ± 49.77 | <0.05 | NR | NR | [23] | |||
| Control | Blank in 10 mg/kg nanoparticles (on day 28 and 42) | Intravenous | 28 | 28 | NR | NR | 182.44 ± 46.55 | NR | NR | |||||
| Intervention | 0.6 mg/mL PGG for 15 min (Once on day 0) | Direct intraluminal delivery | 0 | 28 | 71.40 ± 46.00 | <0.01 | 3.48 ± 0.91 | <0.01 | NR | NR | NR | [10]a | ||
| Control | 2% ethanol, 2.5% DMSO in isotonic saline (Once on day 0) | Direct intraluminal delivery | 0 | 28 | 159.00 ± 77.50 | 5.24 ± 1.61 | NR | NR | NR | |||||
| Intervention | 0.6 mg/mL PGG for 15 min (Once on day 0) | Intraluminal delivery via eluting balloon | 0 | 28 | 183.00 ± 59.10 | NS | 6.13 ± 1.01 | NS | 143.00 ± 91.50 | NS | 5.22 ± 1.06 | NS | NR | [10]b |
| Control | 2% ethanol, 2.5% DMSO in isotonic saline (Once on day 0) | Intraluminal delivery via eluting balloon | 0 | 28 | 149.00 ± 104.00 | 5.15 ± 1.96 | 129.20 ± 97.30 | 4.75 ± 1.91 | NR | |||||
| Intervention | PGG in 10 mg/kg nanoparticles (on day 42 and 56) | Intravenous | 42 | 42 | 66.00 ± 21.00 | <0.05 | NR | NR | NR | 6 (100%) | [24] | |||
| Control | Blank in 10 mg/kg nanoparticles (on day 42 and 56) | Intravenous | 42 | 42 | 185.00 ± 25.00 | NR | NR | NR | 6 (100%) | |||||
| Intervention | PGG in 10 mg/kg nanoparticles conjugated with elastin antibody (Once every two weeks from day 10) | Intravenous | 10 | 28 | 57.00 ± 22.00 | <0.05 | NR | NR | NR | NR | [12] | |||
| Control | Blank in 10 mg/kg nanoparticles (Once every two weeks from day 10) | Intravenous | 10 | 28 | 158.00 ± 43.00 | NR | NR | NR | NR | |||||
| Intervention | 0.03% w/w PGG in saline for 15 min (Once on day 0) | Periadventitial application for 15 min | 0 | 28 | 8.00 ± 7.00 | <0.05 | 1.60 ± 0.09 | NR | NR | NR | 8 (66.7%) (p = NR) | [13]a | ||
| Control | Saline (Once on day 0) | Periadventitial application for 15 min | 0 | 28 | 42.00 ± 10.00 | 1.90 ± 0.10 | NR | NR | 2 (18.2%) (p = NR) | |||||
| Intervention | 0.03% w/w PGG in saline for 15 min (Once on day 28) | Periadventitial application for 15 min | 28 | 28 | 25.00 ± 7.00 | <0.05 | NR | NR | NR | NR | [13]b | |||
| Control | Saline (Once on day 28) | Periadventitial application for 15 min | 28 | 28 | 47.10 ± 11.00 | NR | NR | NR | NR | |||||
| Intervention | 25 or 50 mg PGG | Intraluminal delivery | 0 | 28 | NR | NR | 18.41 ± 2.11 | <0.001 | 12.17 ± 0.13 | <0.001 | NR | [25] | ||
| Control | No administration | Intraluminal delivery | 0 | 28 | NR | NR | 57.03 ± 10.17 | 16.26 ± 0.93 | NR | |||||
| Intervention | 0.3% w/w PGG in saline for 15 min (Once on day 0) | Periadventitial | 0 | 14 | NR | NR | 137.65 ± 11.98 * | NS | 0.85 ± 0.15 | NS | NR | [14]a | ||
| Control | Saline (Once on day 0) | Periadventitial | 0 | 14 | NR | NR | 148.98 ± 15.71 * | 0.97 ± 0.18 | NR | |||||
| Intervention | 0.3% w/w PGG in saline for 15 min (Once on day 0) | Periadventitial | 0 | 28 | NR | NR | 114.48 ± 6.98 * | NS | 0.73 ± 0.09 | NS | NR | [14]b | ||
| Control | Saline (Once on day 0) | Periadventitial | 0 | 28 | NR | NR | 106.84 ± 3.50 * | 0.68 ± 0.07 | NR |
| Reference | [11] | [23] | [10]a | [10]b | [24] | [12] | [13]a | [13]b | [25] | [14]a | [14]b | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Quality Criteria | ||||||||||||
| Was the allocation sequence adequately generated and applied? | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Were the groups similar at baseline or were they adjusted for confounders in the analysis? | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | |
| Was the allocation adequately concealed? | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Were the animals randomly housed during the experiment? | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Were the caregivers and/or investigators blinded from knowledge of which intervention each animal received during the experiment? | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Were animals selected at random for outcome assessment? | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Was the outcome assessor blinded? | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Were incomplete outcome data adequately addressed? | 0 | 0 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | |
| Are reports of the study free of selective outcome reporting? | 0 | 0 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | |
| Was the dose of intervention (PGG) justified? | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Was the sample size estimation performed? | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Was the aortic diameter reported within 1 day prior to first allocation to PGG or control and at study completion? | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | |
| Was the reproducibility of aortic diameter measurement reported? | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Total Score | 1 | 2 | 5 | 4 | 4 | 2 | 2 | 2 | 4 | 2 | 2 | |
| Percentage of possible score | 7.69 | 15.38 | 38.46 | 30.77 | 30.77 | 15.38 | 15.38 | 15.38 | 30.77 | 15.38 | 15.38 | |
| Risk of bias | High | High | High | High | High | High | High | High | High | High | High | |
| Histology Findings | Molecular Biology Findings | Reference |
|---|---|---|
| Suggested aortic elastic fibers were restored in the medial layer (no quantitation); Significantly decreased CD68 positive aortic macrophages (p < 0.05) | Suggested decreased MMP-2 (p = NR), MMP-9 (p = NR) and TGF-b1 (p = NR) | [11] |
| Repaired aortic elastic laminae, improved morphology, and minimal cell infiltration. | Significantly reduced aortic MMP-2 (p < 0.05) activity and increased TIMP-1 and -2 (p < 0.05). Significantly reduced serum IFN-y and spleen CD68 positive cells (p < 0.05) | [23] |
| Controls had significantly more degraded aortic medial elastic fibers than the PGG-administered group (p < 0.01) | mRNA levels of LOX and macrophage marker F4/80 not significantly different between groups | [10]a |
| NR | mRNA levels of LOX, LOXL1 and macrophage marker F4/80 not significantly different between groups | [10]b |
| Reduced aortic collagen deposition in PGG-administered compared to controls (not quantitated) | Significant suppression of aortic MMP (p < 0.05) and increased LOX (p < 0.05) activity compared to controls | [24] |
| Reduced elastin degradation, calcification, macrophage staining in the adventitial layers (not quantitated) | Significant suppression of aortic MMP (p < 0.05) and increased LOX (p < 0.05) activity and desmosine content (p < 0.05) compared to controls | [12] |
| Minimal decrease in elastin content and preserved elastic laminar integrity and waviness visually; Significantly greater aortic desmosine (p < 0.05) | No significant difference in MMP-2, 9 and TIMP-2. Macrophages and lymphocytes were unaffected (All p > 0.05). | [13]a |
| Improved preservation of elastic laminar integrity and waviness and overall preserved tissue architecture. Aorta media thickness was significantly reduced (p < 0.05). | NR | [13]b |
| Integrity of elastic lamellae was preserved. Light to moderate irregular scattered focal muscle atrophy in the tunica media | NR | [25] |
| Unchanged levels of calcium and elastin content. Did not exhibit inflammatory characteristic seen in controls. | NR | [14]a |
| Calcium content was found to be significantly lower in the PGG-treated cohort (p = 0.036). No change in elastin content. The extracellular microarchitecture was well preserved (p = NR). | NR | [14]b |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Golledge, J.; Thanigaimani, S.; Phie, J. A Systematic Review and Meta-Analysis of the Effect of Pentagalloyl Glucose Administration on Aortic Expansion in Animal Models. Biomedicines 2021, 9, 1442. https://doi.org/10.3390/biomedicines9101442
Golledge J, Thanigaimani S, Phie J. A Systematic Review and Meta-Analysis of the Effect of Pentagalloyl Glucose Administration on Aortic Expansion in Animal Models. Biomedicines. 2021; 9(10):1442. https://doi.org/10.3390/biomedicines9101442
Chicago/Turabian StyleGolledge, Jonathan, Shivshankar Thanigaimani, and James Phie. 2021. "A Systematic Review and Meta-Analysis of the Effect of Pentagalloyl Glucose Administration on Aortic Expansion in Animal Models" Biomedicines 9, no. 10: 1442. https://doi.org/10.3390/biomedicines9101442
APA StyleGolledge, J., Thanigaimani, S., & Phie, J. (2021). A Systematic Review and Meta-Analysis of the Effect of Pentagalloyl Glucose Administration on Aortic Expansion in Animal Models. Biomedicines, 9(10), 1442. https://doi.org/10.3390/biomedicines9101442







