A Case Report of a Patient on Therapeutic Warfarin Who Died of COVID-19 Infection with a Sudden Rise in D-Dimer
Abstract
:1. Introduction
2. Case Presentation
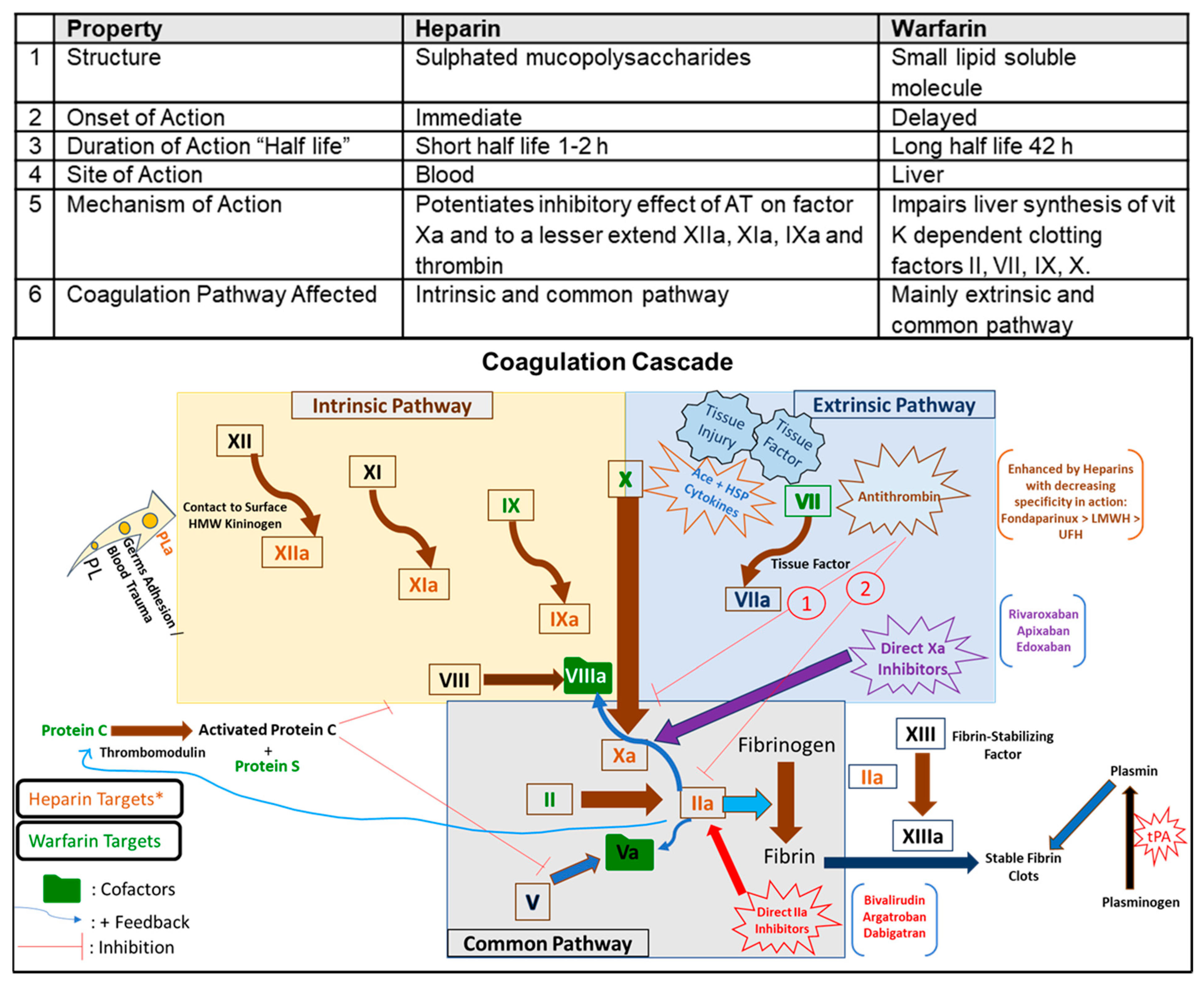
3. Discussion
4. Conclusions
5. Clinical Relevance
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Shang, Y.; Li, H.; Zhang, R. Effects of Pandemic Outbreak on Economies: Evidence from Business History Context. Front. Public Health 2021, 9, 632043. [Google Scholar] [CrossRef]
- Chakraborty, I.; Maity, P. COVID-19 outbreak: Migration, effects on society, global environment and prevention. Sci. Total. Environ. 2020, 728, 138882. [Google Scholar] [CrossRef] [PubMed]
- Zaim, S.; Chong, J.H.; Sankaranarayanan, V.; Harky, A. COVID-19 and Multiorgan Response. Curr. Probl. Cardiol. 2020, 45, 100618. [Google Scholar] [CrossRef]
- Di Gennaro, F.; Pizzol, D.; Marotta, C.; Antunes, M.; Racalbuto, V.; Veronese, N.; Smith, L. Coronavirus Diseases (COVID-19) Current Status and Future Perspectives: A Narrative Review. Int. J. Environ. Res. Public Health 2020, 17, 2690. [Google Scholar] [CrossRef] [Green Version]
- Shimabukuro-Vornhagen, A.; Gödel, P.; Subklewe, M.; Stemmler, H.J.; Schlößer, H.A.; Schlaak, M.; Kochanek, M.; Böll, B.; von Bergwelt-Baildon, M.S. Cytokine release syndrome. J. Immunother. Cancer 2018, 6, 56. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mehta, P.; McAuley, D.F.; Brown, M.; Sanchez, E.; Tattersall, R.S.; Manson, J.J. COVID-19: Consider cytokine storm syndromes and immunosuppression. Lancet 2020, 395, 1033–1034. [Google Scholar] [CrossRef]
- Crosby, J.C.; Heimann, M.A.; Burleson, S.L.; Anzalone, B.C.; Swanson, J.F.; Wallace, D.W.; Greene, C.J. COVID-19: A review of therapeutics under investigation. J. Am. Coll. Emerg. Physicians Open 2020, 1, 231–237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA 2020, 323, 1061–1069. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Tang, N.; Li, D.; Wang, X.; Sun, Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J. Thromb. Haemost. JTH 2020, 18, 844–847. [Google Scholar] [CrossRef] [Green Version]
- NIH.GOV. COVID-19 Treatment Guidelines Panel. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. National Institutes of Health. Available online: https://www.covid19treatmentguidelines.nih.gov/ (accessed on 5 May 2021).
- Driggin, E.; Madhavan, M.V.; Bikdeli, B.; Chuich, T.; Laracy, J.; Biondi-Zoccai, G.; Brown, T.S.; Der Nigoghossian, C.; Zidar, D.A.; Haythe, J.; et al. Cardiovascular Considerations for Patients, Health Care Workers, and Health Systems during the COVID-19 Pandemic. J. Am. Coll. Cardiol. 2020, 75, 2352–2371. [Google Scholar] [CrossRef]
- WHO. Clinical Management of Severe Acute Respiratory Infection (SARI) When COVID-19 Disease Is Suspected: Interim Guidance V 1.2. Available online: https://www.who.int/publications/i/item/clinical-management-of-covid-19 (accessed on 5 May 2021).
- Magnani, H.N. Rationale for the Role of Heparin and Related GAG Antithrombotics in COVID-19 Infection. Clin. Appl. Thromb./Hemost. 2021, 27, 1076029620977702. [Google Scholar] [CrossRef] [PubMed]
- Dobesh, P.P.; Trujillo, T.C. Coagulopathy, Venous Thromboembolism, and Anticoagulation in Patients with COVID-19. Pharmacotherapy 2020, 40, 1130–1151. [Google Scholar] [CrossRef]
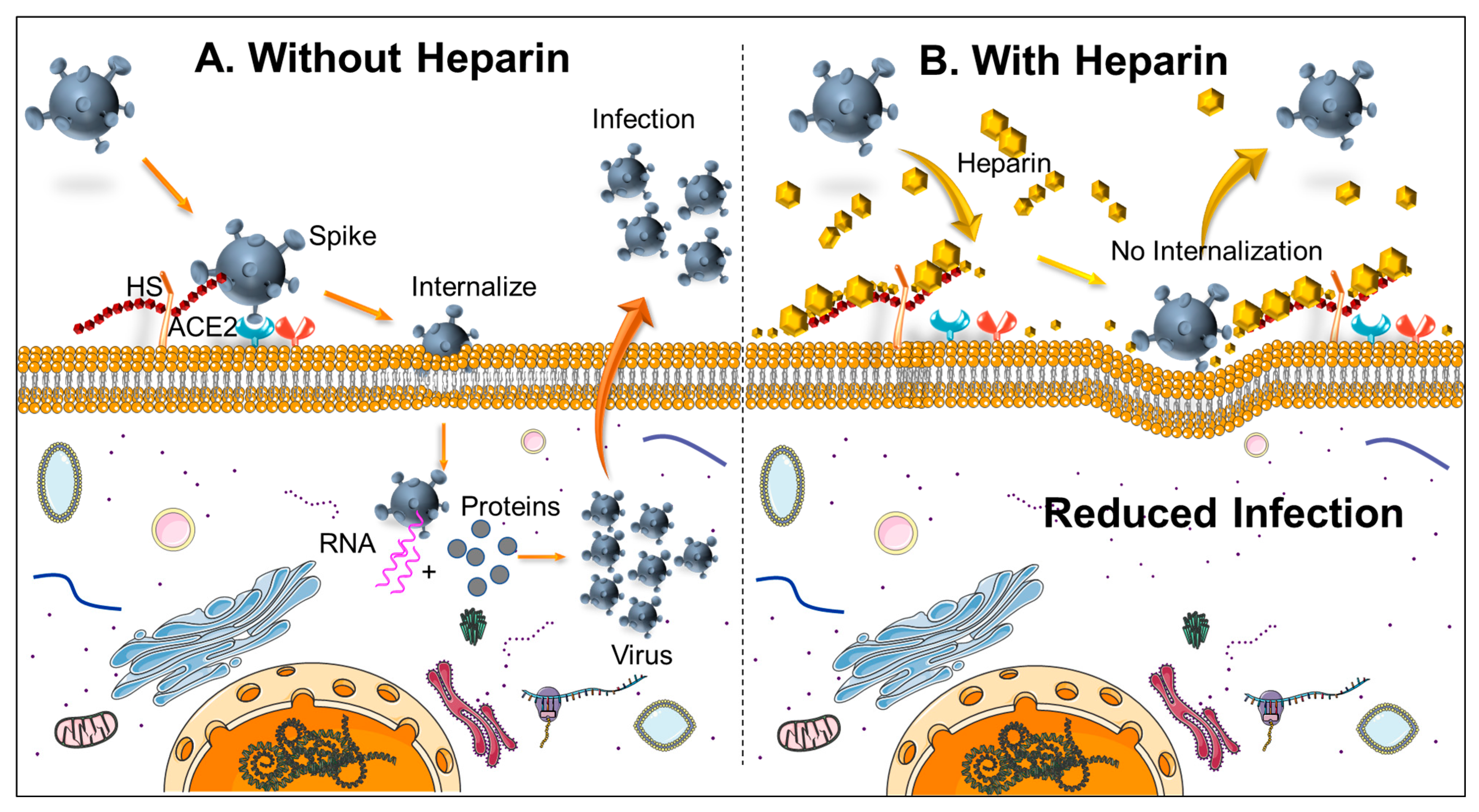
- Gozzo, L.; Viale, P.; Longo, L.; Vitale, D.C.; Drago, F. The Potential Role of Heparin in Patients with COVID-19: Beyond the Anticoagulant Effect. A Review. Front. Pharmacol. 2020, 11, 1307. [Google Scholar] [CrossRef] [PubMed]
- Clausen, T.M.; Sandoval, D.R.; Spliid, C.B.; Pihl, J.; Perrett, H.R.; Painter, C.D.; Narayanan, A.; Majowicz, S.A.; Kwong, E.M.; McVicar, R.N.; et al. SARS-CoV-2 Infection Depends on Cellular Heparan Sulfate and ACE2. Cell 2020, 183, 1043–1057.e1015. [Google Scholar] [CrossRef] [PubMed]
- Vaz de Paula, C.B.; de Azevedo, M.L.V.; Nagashima, S.; Martins, A.P.C.; Malaquias, M.A.S.; Miggiolaro, A.; da Silva Motta Júnior, J.; Avelino, G.; do Carmo, L.A.P.; Carstens, L.B.; et al. IL-4/IL-13 remodeling pathway of COVID-19 lung injury. Sci. Rep. 2020, 10, 18689. [Google Scholar] [CrossRef]
- Subramaniam, S.; Scharrer, I. Procoagulant activity during viral infections. Front. Biosci. 2018, 23, 1060–1081. [Google Scholar] [CrossRef] [Green Version]
- Delvaeye, M.; Conway, E.M. Coagulation and innate immune responses: Can we view them separately? Blood 2009, 114, 2367–2374. [Google Scholar] [CrossRef]
- Fiusa, M.M.; Carvalho-Filho, M.A.; Annichino-Bizzacchi, J.M.; De Paula, E.V. Causes and consequences of coagulation activation in sepsis: An evolutionary medicine perspective. BMC Med. 2015, 13, 105. [Google Scholar] [CrossRef] [Green Version]
- Tavassoly, O.; Safavi, F.; Tavassoly, I. Heparin-binding Peptides as Novel Therapies to Stop SARS-CoV-2 Cellular Entry and Infection. Mol. Pharmacol. 2020, 98, 612–619. [Google Scholar] [CrossRef]
- Ceranowicz, P.; Dembinski, A.; Warzecha, Z.; Dembinski, M.; Cieszkowski, J.; Rembisz, K.; Konturek, S.J.; Kusnierz-Cabala, B.; Tomaszewska, R.; Pawlik, W.W. Protective and therapeutic effect of heparin in acute pancreatitis. J. Physiol. Pharmacol. 2008, 59 (Suppl. 4), 103–125. [Google Scholar]
- Warzecha, Z.; Sendur, P.; Ceranowicz, P.; Dembiński, M.; Cieszkowski, J.; Kuśnierz-Cabala, B.; Olszanecki, R.; Tomaszewska, R.; Ambroży, T.; Dembiński, A. Protective Effect of Pretreatment with Acenocoumarol in Cerulein-Induced Acute Pancreatitis. Int. J. Mol. Sci. 2016, 17, 1709. [Google Scholar] [CrossRef]
- Maduzia, D.; Ceranowicz, P.; Cieszkowski, J.; Gałązka, K.; Kuśnierz-Cabala, B.; Warzecha, Z. Pretreatment with Warfarin Attenuates the Development of Ischemia/Reperfusion-Induced Acute Pancreatitis in Rats. Molecules 2020, 25, 2493. [Google Scholar] [CrossRef] [PubMed]
- Warzecha, Z.; Dembinski, A.; Ceranowicz, P.; Dembinski, M.; Sendur, R.; Cieszkowski, J.; Sendur, P.; Tomaszewska, R. Heparin inhibits protective effect of ischemic preconditioning in ischemia/reperfusion-induced acute pancreatitis. J. Physiol. Pharmacol. 2012, 63, 355–365. [Google Scholar]
- Warzecha, Z.; Sendur, P.; Ceranowicz, P.; Dembinski, M.; Cieszkowski, J.; Kusnierz-Cabala, B.; Tomaszewska, R.; Dembinski, A. Pretreatment with low doses of acenocoumarol inhibits the development of acute ischemia/reperfusion-induced pancreatitis. J. Physiol. Pharmacol. 2015, 66, 731–740. [Google Scholar]
- Warzecha, Z.; Sendur, P.; Ceranowicz, P.; Cieszkowski, J.; Dembiński, M.; Sendur, R.; Bonior, J.; Jaworek, J.; Ambroży, T.; Olszanecki, R.; et al. Therapeutic Effect of Low Doses of Acenocoumarol in the Course of Ischemia/Reperfusion-Induced Acute Pancreatitis in Rats. Int. J. Mol. Sci. 2017, 18, 882. [Google Scholar] [CrossRef] [PubMed]
- Maduzia, D.; Ceranowicz, P.; Cieszkowski, J.; Chmura, A.; Galazka, K.; Kusnierz-Cabala, B.; Warzecha, Z. Administration of warfarin accelerates the recovery in ischemia/reperfusion-induced acute pancreatitis. J. Physiol. Pharmacol. 2020, 71. [Google Scholar] [CrossRef]
- Young, E. The anti-inflammatory effects of heparin and related compounds. Thromb. Res. 2008, 122, 743–752. [Google Scholar] [CrossRef] [PubMed]
- Milewska, A.; Zarebski, M.; Nowak, P.; Stozek, K.; Potempa, J.; Pyrc, K. Human coronavirus NL63 utilizes heparan sulfate proteoglycans for attachment to target cells. J. Virol. 2014, 88, 13221–13230. [Google Scholar] [CrossRef] [Green Version]
- Shi, C.; Wang, C.; Wang, H.; Yang, C.; Cai, F.; Zeng, F.; Cheng, F.; Liu, Y.; Zhou, T.; Deng, B.; et al. The Potential of Low Molecular Weight Heparin to Mitigate Cytokine Storm in Severe COVID-19 Patients: A Retrospective Cohort Study. Clin. Transl. Sci. 2020, 13, 1087–1095. [Google Scholar] [CrossRef]
- Linkins, L.A.; Takach Lapner, S. Review of D-dimer testing: Good, Bad, and Ugly. Int. J. Lab. Hematol. 2017, 39 (Suppl. 1), 98–103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thachil, J. All those D-dimers in COVID-19. J. Thromb./Haemost. JTH 2020, 18, 2075–2076. [Google Scholar] [CrossRef] [PubMed]
- Marongiu, F.; Barcellona, D. Fondaparinux: Should It Be Studied in Patients with COVID-19 Disease? TH Open Companion J. Thromb. Haemost. 2020, 4, e300–e302. [Google Scholar] [CrossRef] [PubMed]
- Gülcü, O.; Aksakal, E.; Aydemir, S.; Doğan, R.; Saraç, İ.; Aydın, S.; Öztürk, M.; Aksu, U.; Kalkan, K.; Tanboğa, İ.H. Association between previous anticoagulant use and mortality among hospitalized patients with COVID-19. J. Thromb. Thrombolysis 2021, 1–8. [Google Scholar] [CrossRef]
| Marker | Units | Day 0/Admit | Day 1 | Day 2 | Day 3 | Day 4/Death |
|---|---|---|---|---|---|---|
| Protein | g/dL | 7.1 | 6.7 | 6.0 L | 6.1 L | |
| Albumin | g/dL | 3.2 L | 3.1 L | 2.7 L | 2.8 L | |
| T.Bil | mg/dL | 1.1 | 1.1 | 0.5 | 0.6 | |
| AlkPhos | U/L | 68 | 67 | 68 | 77 | |
| A | U/L | 75 H | 62 H | 67 H | 35 H | |
| ALT01 | U/L | 59 H | 53 | 61 H | 50 |
| Marker | Units | Day 0/Admit | Day 1 | Day 2 | Day 3 | Day 4/Death |
|---|---|---|---|---|---|---|
| PT | Sec | 26.7 H | 27.5 H | 26.1 H | 26.4 H | |
| INR | Ratio | 2.50 H | 2.60 H | 2.43 H | 2.48 | |
| Fibrinogen | mg/dL | 818 H | ||||
| D-Dimer | ug/mL | 1.14 H | 1.04 H | - | >20.0 H | |
| CRP | mg/L | 126.6 H | 81.8 H | - | 60.7 H | |
| Ferritin | ng/mL | 2495.0 H | 2432.0 H | - | 1845.0 H | |
| Procalcitonin | ng/mL | 0.14 | 0.09 | - | 0.06 | |
| LDH-V | U/L | 650 H | 646 H | - | 780 H | |
| Lactic Acid | mmol/L | 1.5 | 1.5 | - | 1.5 | |
| CPK | U/L | 496 H | 318 H | - | 165 | |
| Troponin-I | ng/mL | 0.0 | 0.028 | - | - | 0.063 H |
| BNP | pg/mL | 58 | 50 | 36 | ||
| Cortisol | ug/dL | 2.6 |
| Marker | Units | Day 0/Admit | Day 1 | Day 2 |
|---|---|---|---|---|
| HgbA1c | % | 8.3 H | ||
| Chol | mg/dL | 138 | ||
| Trigly | mg/dL | 84 | ||
| HDL | mg/dL | 39 | ||
| LDL | mg/dL | 82.2 | ||
| TSH (0) | ulU/mL | 0.6 | ||
| VitD | ng/mL | 11 | ||
| B12 (0) | pg/mL | 379 | ||
| FolA (0) | ng/mL | 5.2 L | ||
| Iron | ug/dL | 34 L |
| CBC | Units | Day 0/Admit | Day 1 | Day 2 | Day 3 | Day 4/Death |
|---|---|---|---|---|---|---|
| WBC4 | 103/uL | 10.66 H | 8.96 H | 12.29 H | 11.43 H | 11.61 H |
| HGB4 | g/dL | 12. L | 11.6 L | 10.6 L | 10.9 L | 10.60 L |
| HCT4 | % | 35.0 L | 32.9 L | 29.9 L | 30.7 L | 29.8 L |
| PLT4 | 103/uL | 480.0 H | 468.0 H | 517.0 H | 544.0 H | 293 H |
| NEUT%4 | % | 87.5 H | 78.4 H | 86.9 H | 85.7 H | 80.0 H |
| LY%4 | % | 7.5 L | 15.4 L | 6.8 L | 7.2 L | 8.9 L |
| Chemistry | Units | Day 0/Admit | Day 1 | Day 2 | Day 3 | Day 4/death |
|---|---|---|---|---|---|---|
| Na | mmol/L | 137 | 139 | 133 L | 136 | 136 |
| K+ | mmol/L | 3.3 L | 3.2 L | 4 | 4 | 3.6 |
| CL− | mmol/L | 97 L | 99 L | 101 | 104 | 103 |
| CO2-V | mmol/L | 29 H | 27 | 22 | 23 | 21 L |
| BUN | mg/dL | 15 | 17 | 26 H | 19 | 19 |
| Creat2 | mg/dL | 0.96 | 0.97 | 1.12 | 0.96 | 0.83 |
| Gluc | mg/dL | 133 H | 139 H | 323 H | 242 H | 236 H |
| Ca | mg/dL | 8.3 L | 8.2 L | 7.8 L | 8.0 L | 8.0 L |
| iCa | nmol/L | 0.99 L | 1.01 L | 1.05 L | 1.14 L | |
| Phos | mg/dL | 1.5 L | 2.9 | 2.2 L | 2.6 | |
| Mg++ | mg/dL | 1.6 | 2.8 | 1.9 | 1.6 | |
| EGFR | mL/min | 78 | 78.2 | 93.4 | 110.5 |
| Tests | Units | Result | Flag | Ref. Intervals |
|---|---|---|---|---|
| IL-4, Serum | pg/mL | <31.2 | 0.0–31.2 | |
| IL-8, Serum | U/mL | 437.1 | HIGH | 0.0–66.1 |
| SARS-CoV-2 Semi-Quant Total Ab | U/mL | 224.9 | HIGH | <0.80 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Agarwal, R.N.; Aggarwal, H.; Verma, A.; Tripathi, M.K. A Case Report of a Patient on Therapeutic Warfarin Who Died of COVID-19 Infection with a Sudden Rise in D-Dimer. Biomedicines 2021, 9, 1382. https://doi.org/10.3390/biomedicines9101382
Agarwal RN, Aggarwal H, Verma A, Tripathi MK. A Case Report of a Patient on Therapeutic Warfarin Who Died of COVID-19 Infection with a Sudden Rise in D-Dimer. Biomedicines. 2021; 9(10):1382. https://doi.org/10.3390/biomedicines9101382
Chicago/Turabian StyleAgarwal, Reita N., Hersheth Aggarwal, Ashmit Verma, and Manish K. Tripathi. 2021. "A Case Report of a Patient on Therapeutic Warfarin Who Died of COVID-19 Infection with a Sudden Rise in D-Dimer" Biomedicines 9, no. 10: 1382. https://doi.org/10.3390/biomedicines9101382
APA StyleAgarwal, R. N., Aggarwal, H., Verma, A., & Tripathi, M. K. (2021). A Case Report of a Patient on Therapeutic Warfarin Who Died of COVID-19 Infection with a Sudden Rise in D-Dimer. Biomedicines, 9(10), 1382. https://doi.org/10.3390/biomedicines9101382






