A Brief Review of the Pharmacology of Amitriptyline and Clinical Outcomes in Treating Fibromyalgia
Abstract
:1. Introduction
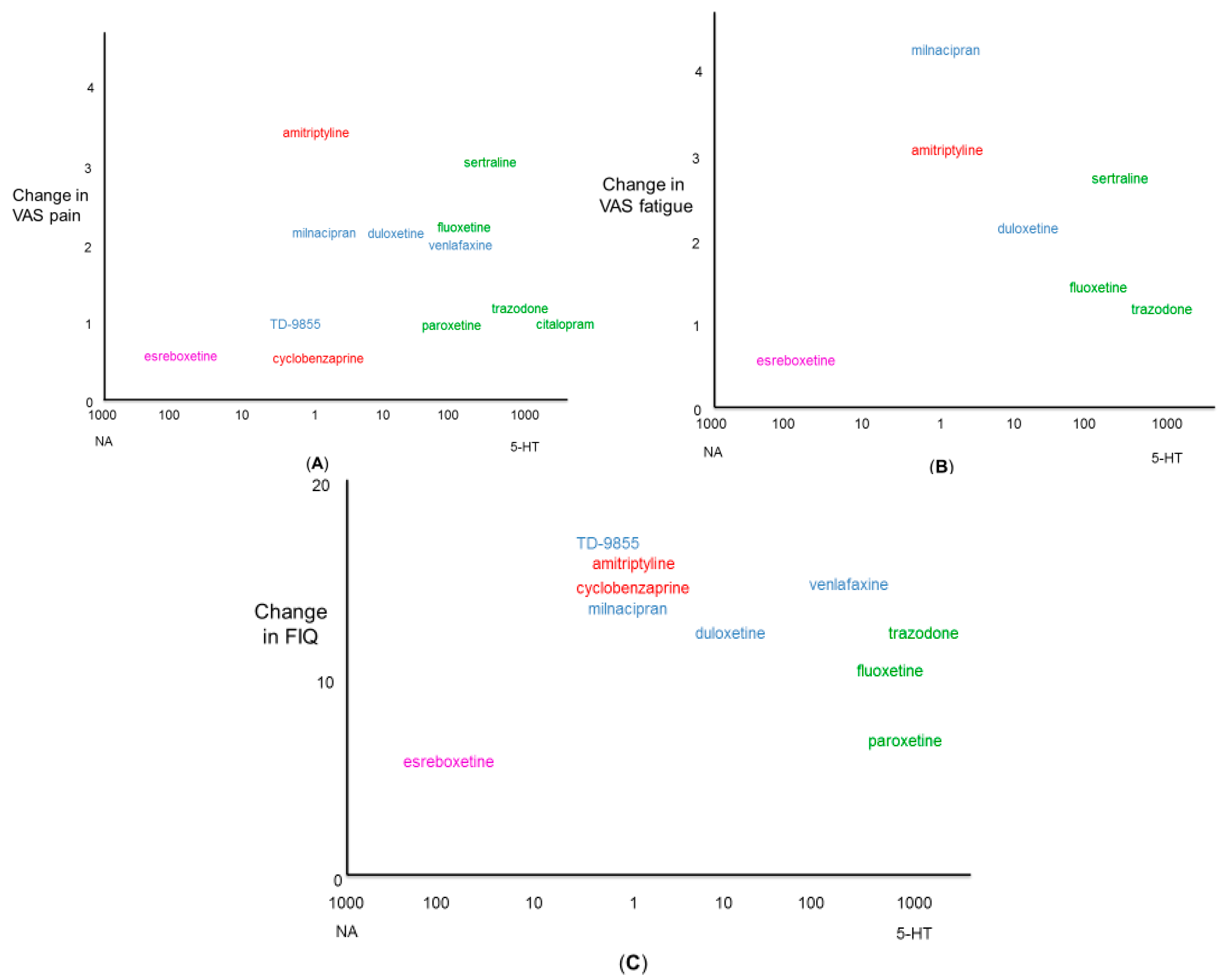
2. Pharmacology of Antidepressants and Fibromyalgia
3. Pharmacology of Amitriptyline and Fibromyalgia
4. Conclusions
Acknowledgments
Conflicts of Interest
References
- Borchers, A.T.; Gershwin, M.E. Fibromyalgia: A critical and comprehensive review. Clin. Rev. Allergy Immunol. 2016, 49, 100–151. [Google Scholar] [CrossRef] [PubMed]
- Lawson, K. Potential drug therapies for the treatment of fibromyalgia. Exp. Opin. Investig. Drugs 2016, 25, 1071–1081. [Google Scholar] [CrossRef] [PubMed]
- Queiroz, L.P. Worldwide epidemiology of fibromyalgia. Curr. Pain Headache Rep. 2013, 17, 356. [Google Scholar] [CrossRef] [PubMed]
- Macfarlane, G.J.; Kronisch, C.; Dean, L.E.; Atzeni, F.; Häuser, W.; Fluß, E.; Choy, E.; Kosek, E.; Amris, K.; Branco, J.; et al. EULAR revised recommendations for the management of fibromyalgia. Ann. Rheum. Dis. 2016. [Google Scholar] [CrossRef] [PubMed]
- Häuser, W.; Arnold, B.; Eich, W.; Felde, E.; Flügge, C.; Henningsen, P.; Herrmann, M.; Köllner, V.; Kühn, E.; Nutzinger, D.; et al. Management of fibromyalgia syndrome—An interdisciplinary evidence-based guideline. Ger. Med. Sci. 2008, 6, 1–11. [Google Scholar]
- Kia, S.; Choy, E. Update on treatment guideline in fibromyalgia syndrome with focus on pharmacology. Biomedicines 2017, 5, 20. [Google Scholar] [CrossRef]
- Mika, J.; Zychowska, M.; Makuch, W.; Rojewska, E.; Przewlocka, B. Neuronal and immunological basis of action of antidepressants in chronic pain—Clinical and experimental studies. Pharmacol. Rep. 2013, 65, 1611–1621. [Google Scholar] [CrossRef]
- Sluka, K.A.; Clauw, D.J. Neurobiology of fibromyalgia and chronic widespread pain. Neuroscience 2016, 338, 114–129. [Google Scholar] [CrossRef] [PubMed]
- Julien, N.; Goffaux, P.; Arsenault, P.; Marchand, S. Widespread pain in fibromyalgia is related to a deficit of endogenous pain inhibition. Pain 2005, 114, 295–302. [Google Scholar] [CrossRef] [PubMed]
- Vaishnavi, S.N.; Nemeroff, C.B.; Plott, S.J.; Rao, S.G.; Kranzler, J.; Owens, M.J. Milnacipran: A comparative analysis of human monoamine uptake and transporter binding affinity. Biol. Psychiatry 2004, 55, 320–322. [Google Scholar] [CrossRef] [PubMed]
- Mestres, J.; Seifert, S.A.; Oprea, T.I. Linking pharmacology to clinical reports: Cyclobenzaprine and its possible association with serotonin syndrome. Clin. Pharmacol. Ther. 2011, 90, 662–665. [Google Scholar] [CrossRef] [PubMed]
- Roth, B.L.; Driscol, J. PDSP Ki Database. In Psychoactive Drug Screening Program (PDSP); United States National Institute of Mental Health, University of North Carolina: Chapel Hill, NC, USA, 2011. [Google Scholar]
- Koch, S.; Perry, K.W.; Nelson, D.L.; Conway, R.G.; Threlkeld, P.G.; Bymaster, F.P. R-fluoxetine increases extracellular DA, NE, as well as 5-HT in rat prefrontal cortex and hypothalamus: An in vivo microdialysis and receptor binding study. Neuropsychopharmacology 2002, 27, 949–959. [Google Scholar] [CrossRef]
- Dekeyne, A.; Millan, M.J. Discriminative stimulus properties of the atypical antidepressant, mirtazapine, in rats: A pharmacological characterization. Psychopharmacology 2009, 203, 329–341. [Google Scholar] [CrossRef] [PubMed]
- Murai, N.; Aoki, T.; Tamura, S.; Sekizawa, T.; Kakimoto, S.; Tsukamoto, M.; Oe, T.; Enomoto, R.; Hamakawa, N.; Matsuoka, N. AS1069562, the (+)-isomer of indeloxazine, exerts analgesic effects in a rat model of neuropathic pain with unique characteristics in spinal monoamine turnover. J. Pharmacol. Exp. Ther. 2014, 348, 372–382. [Google Scholar] [CrossRef] [PubMed]
- Mahaney, P.E.; Vu, A.T.; McComas, C.C.; Zhang, P.; Nogle, L.M.; Watts, W.L.; Sarkahian, A.; Leventhal, L.; Sullivan, N.R.; Uveges, A.J.; et al. Synthesis and activity of a new class of dual acting norepinephrine and serotonin reuptake inhibitors: 3-(1H-indol-1-yl)-3-arylpropan-1-amines. Bioorg. Med. Chem. 2006, 14, 8455–8466. [Google Scholar] [CrossRef] [PubMed]
- Bymaster, F.P.; Dreshfield-Ahmad, L.J.; Threlkeld, P.G.; Shaw, J.L.; Thompson, L.; Nelson, D.L.; Hemrick-Luecke, S.K.; Wong, D.T. Comparative affinity of duloxetine and venlafaxine for serotonin and norepinephrine transporters in vitro and in vivo, human serotonin receptor subtypes, and other neuronal receptors. Neuropsychopharmacology 2001, 25, 871–880. [Google Scholar] [CrossRef]
- Koch, S.; Hemrick-Luecke, S.K.; Thompson, L.K.; Evans, D.C.; Threlkeld, P.G.; Nelson, D.L.; Perry, K.W.; Bymaster, F.P. Comparison of effects of dual transporter inhibitors on monoamine transporters and extracellular levels in rats. Neuropharmacology 2003, 45, 935–944. [Google Scholar] [CrossRef]
- Marks, D.M.; Shah, M.J.; Patkar, A.A.; Masand, P.S.; Park, G.Y.; Pae, C.U. Serotonin-norepinephrine reuptake inhibitors for pain control: Premise and promise. Curr. Neuropharmacol. 2009, 7, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Owens, J.M.; Knight, D.L.; Nemeroff, C.B. Second generation SSRIs: Human monoamine transporter binding profile of escitalopram and R-fluoxetine. Encephale 2002, 28, 350–355. [Google Scholar] [CrossRef]
- Smith, J.A.; Bourdet, D.L.; Daniels, O.T.; Ding, Y.S.; Gallezot, J.D.; Henry, S.; Kim, K.H.; Kshirsagar, S.; Martin, W.J.; Obedencio, G.P.; et al. Preclinical to clinical translation of CNS transporter occupancy of TD-9855, a novel norepinephrine and serotonin reuptake inhibitor. Int. J. Neuropsychopharmacol. 2014, 18, pyu027. [Google Scholar] [CrossRef] [PubMed]
- Micó, J.A.; Ardid, D.; Berrocoso, E.; Eschalier, A. Antidepressants and pain. Trends Pharmacol. Sci. 2006, 27, 348–354. [Google Scholar] [CrossRef] [PubMed]
- Mason, P. Deconstructing endogenous pain modulations. J. Neurophysiol. 2005, 94, 1659–1663. [Google Scholar] [CrossRef] [PubMed]
- Deurveilher, S.; Kazue, S. Reciprocal connections between the suprachiasmatic nucleus and the midbrain raphe nuclei: A putative role in the circadian control of behavioral states. In Serotonin and Sleep: Molecular, Functional and Clinical Aspects; Monti, J.M., Pandi-Perumal, S.R., Jacobs, B.L., Nutt, D.J., Eds.; Birkhäuser: Basel, Switzerland, 2008; pp. 103–131. [Google Scholar]
- Benarroch, E.E. The locus ceruleus norepinephrine system: Functional organization and potential clinical significance. Neurology 2009, 73, 1699–1704. [Google Scholar] [CrossRef] [PubMed]
- Ramos, B.P.; Arnsten, A.F. Adrenergic pharmacology and cognition: Focus on the prefrontal cortex. Pharmacol. Ther. 2007, 113, 523–536. [Google Scholar] [CrossRef] [PubMed]
- Nekovarova, T.; Yamamotova, A.; Vales, K.; Stuchlik, A.; Fricova, J.; Rokyta, R. Common mechanisms of pain and depression: Are antidepressants also analgesics? Front. Behav. Neurosci. 2014, 8, 99. [Google Scholar] [CrossRef] [PubMed]
- Sawynok, J.; Esser, M.J.; Reid, A.R. Antidepressants as analgesics: An overview of central and peripheral mechanisms of action. J. Psychiatry Neurosci. 2001, 26, 21–29. [Google Scholar] [PubMed]
- Carette, S.; Oakson, G.; Guimont, C.; Steriade, M. Sleep electroencephalography and the clinical response to amitriptyline in patients with fibromyalgia. Arthritis Rheum. 1995, 9, 1211–1217. [Google Scholar] [CrossRef]
- Ginsberg, F.; Mancaux, A.; Joos, E.; Vanhove, P.; Famaey, J.P. A randomized placebo-controlled trial of sustained-release amitriptyline in primary fibromyalgia. J. Musculoskelet. Pain 1996, 4, 37–47. [Google Scholar] [CrossRef]
- Goldenberg, D.; Felson, D.; Dinerman, H. A randomized, controlled trial of amitriptyline and naproxen in the treatment of patients with fibromyalgia. Arthritis Rheum. 1986, 29, 1371–1377. [Google Scholar] [CrossRef] [PubMed]
- Goldenberg, D.; Mayskiy, M.; Mossey, C.; Ruthazer, R.; Schmid, C. A randomized, double-blind crossover trial of fluoxetine and amitriptyline in the treatment of fibromyalgia. Arthritis Rheum. 1996, 39, 1852–1859. [Google Scholar] [CrossRef] [PubMed]
- Hannonen, P.; Malminiemi, K.; Yli-Kerttula, U.; Isomeri, R.; Roponen, P. A randomized, double-blind, placebo-controlled study of moclobemide and amitriptyline in the treatment of fibromyalgia in females without psychiatric disorder. Br. J. Rheumatol. 1998, 37, 1279–1286. [Google Scholar] [CrossRef] [PubMed]
- Heymann, R.E.; Helfenstein, M.; Feldman, D. A double-blind, randomized controlled study of amitriptyline, nortriptyline and placebo in patients with fibromyalgia. An analysis of outcome measures. Clin. Exp. Rheumatol. 2001, 19, 697–702. [Google Scholar] [PubMed]
- Capaci, K.; Hepguler, S. Comparison of the effects of amitriptyline and paroxetine in the treatment of fibromyalgia syndrome. Pain Clinic 2002, 14, 223–228. [Google Scholar] [CrossRef]
- Gulec, H.; Capkin, E.; Sayar, K.; Ak, I. The evaluation of the effectiveness of amitriptyline versus venlafaxine in female patients diagnosed with fibromyalgia syndrome. Klinik Psikofarmakol. Bulteni 2007, 17, 68–73. [Google Scholar]
- Konuk, N.; Ortancil, O.; Bostanci, B.; Kiran, S.; Sapmaz, P. A comparison of reboxetine and amitryptilline in the treatment of fibromyalgia syndrome with co-morbid depressive symptoms: An open-label preliminary study. Klinik Psikofarmakol. Bulteni 2010, 20, 29–37. [Google Scholar]
- Calandre, E.P.; Rico-Villademoros, F.; Galan, J.; Molina-Barea, R.; Vilchez, J.S.; Rodriguez-Lopez, C.M.; Hidalgo-Tallon, J.; Morillas-Arques, P. Quetiapine extended-release (Seroquel-XR) versus amitriptyline monotherapy for treating patients with fibromyalgia: A 16-week, randomized, flexible-dose, open-label trial. Psychopharmacology 2014, 231, 2525–2531. [Google Scholar] [CrossRef] [PubMed]
- Gur, A.; Karakoc, M.; Nas, K.; Cevik, R.; Sarac, J.; Ataoglu, S. Effects of low power laser and low dose amitriptyline therapy on clinical symptoms and quality of life in fibromyalgia: A single-blind, placebo-controlled trial. Rheumatol. Int. 2002, 22, 188–193. [Google Scholar] [PubMed]
- Azad, K.A.; Alam, M.N.; Haq, S.A.; Nahar, S.; Chowdhury, M.A.; Ali, S.M.; Ullah, A.K. Vegetarian diet in the treatment of fibromyalgia. Bangladesh Med. Res. Counc. Bull. 2000, 26, 41–47. [Google Scholar] [PubMed]
- Vlainich, R.; Issy, A.M.; Sakata, R.K. Effect of intravenous lidocaine associated with amitriptyline on pain relief and plasma serotonin, norepinephrine, and dopamine concentrations in fibromyalgia. Clin. J. Pain 2011, 27, 285–288. [Google Scholar] [CrossRef] [PubMed]
- Anderberg, U.M.; Marteinsdottir, I.; von Knorring, L. Citalopram in patients with fibromyalgia—A randomized, double-blind, placebo-controlled study. Eur. J. Pain 2000, 4, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Moldofsky, H.; Harris, H.W.; Archambault, W.T.; Kwong, T.; Lederman, S. Effects of bedtime very low dose cyclobenzaprine on symptoms and sleep physiology in patients with fibromyalgia syndrome: A double-blind randomized placebo-controlled study. J. Rheumatol. 2011, 38, 2653–2663. [Google Scholar] [CrossRef] [PubMed]
- Bennett, R.M.; Gatter, R.A.; Campbell, S.M.; Andrews, R.P.; Clark, S.R.; Scarola, J.A. A comparison of cyclobenzaprine and placebo in the management of fibrositis: A double blind controlled study. Arthritis Rheum. 1988, 31, 1535–1542. [Google Scholar] [CrossRef] [PubMed]
- Carette, S.; Bell, M.J.; Reynolds, W.J.; Haraoui, B.; McCain, G.A.; Bykerk, V.P. A comparison of amitriptyline, cyclobenzaprine and placebo in the treatment of fibromyalgia: A randomized, double-blind clinical trial. Arthritis Rheum. 1994, 37, 32–40. [Google Scholar] [CrossRef] [PubMed]
- Quimby, L.G.; Gratwick, G.M.; Whitney, C.D.; Block, S.R. A randomized trial of cyclobenzaprine for the treatment of fibromyalgia. J. Rheumatol. 1989, 16, 140–143. [Google Scholar]
- Reynolds, W.J.; Moldofsky, H.; Saskin, P.; Lue, F.A. The effects of cyclobenzaprine on sleep physiology and symptoms in patients with fibromyalgia. J. Rheumatol. 1991, 19, 452–454. [Google Scholar]
- Arnold, L.M.; Lu, Y.; Crofford, L.J.; Wohlreich, M.; Detke, M.J.; Iyengar, S.; Goldstein, D.J. A double-blind, multicenter trial comparing duloxetine with placebo in the treatment of fibromyalgia patients with or without major depressive disorder. Arthritis Rheum. 2004, 50, 2974–2984. [Google Scholar] [CrossRef] [PubMed]
- Chappell, A.S.; Bradley, L.A.; Wiltse, C.; Detke, M.J.; D’Souza, D.N.; Spaeth, M. A six-month double-blind, placebo-controlled, randomized clinical trial of duloxetine for the treatment of fibromyalgia. Int. J. Gen. Med. 2008, 30, 91–102. [Google Scholar] [CrossRef]
- Arnold, L.M.; Clauw, D.J.; Wohlreich, M.M.; Wang, F.; Ahl, J.; Gaynor, P.J.; Chappell, A.S. Efficacy of duloxetine in patients with fibromyalgia: Pooled analysis of 4 placebo-controlled clinical trials. Prim. Care Companion J. Clin. Psychiatry 2009, 11, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Arnold, L.M.; Zhang, S.; Pangallo, B.A. Efficacy and safety of duloxetine 30 mg/d in patients with fibromyalgia: A randomized, double-blind, placebo-controlled study. Clin. J. Pain 2012, 28, 775–781. [Google Scholar] [CrossRef] [PubMed]
- Bradley, L.A.; Bennett, R.; Russell, I.J.; Wohlreich, M.M.; Chappell, A.S.; Wang, F.; D’Souza, D.N.; Moldofsky, H. Effect of duloxetine in patients with fibromyalgia: Tiredness subgroups. Arthritis Res. Ther. 2010, 12, R141. [Google Scholar] [CrossRef] [PubMed]
- Murakami, M.; Osada, K.; Mizuno, H.; Ochiai, T.; Alev, L.; Nishioka, K. A randomized, double-blind, placebo-controlled phase III trial of duloxetine in Japanese fibromyalgia patients. Arthritis Res. Ther. 2015, 17, 224. [Google Scholar] [CrossRef] [PubMed]
- Russell, I.J.; Mease, P.J.; Smith, T.R.; Kajdasz, D.K.; Wohlreich, M.M.; Detke, M.J.; Walker, D.J.; Chappell, A.S.; Arnold, L.M. Efficacy and safety of duloxetine for treatment of fibromyalgia in patients with or without major depressive disorder: Results from a 6-month, randomized, double-blind, placebo-controlled, fixed-dose trial. Pain 2008, 136, 432–444. [Google Scholar] [CrossRef] [PubMed]
- Arnold, L.M.; Wang, F.; Ahl, J.; Gaynor, P.J.; Wohlreich, M.M. Improvement in multiple dimensions of fatigue in patients with fibromyalgia treated with duloxetine: Secondary analysis of a randomized, placebo-controlled trial. Arthritis Res. Ther. 2011, 13, R86. [Google Scholar] [CrossRef] [PubMed]
- Arnold, L.M.; Rosen, A.; Pritchett, Y.L.; D'Souza, D.N.; Goldstein, D.J.; Iyengar, S.; Wernicke, J.F. A randomized, double-blind, placebo-controlled trial of duloxetine in the treatment of women with fibromyalgia with or without major depressive disorder. Pain 2005, 119, 5–15. [Google Scholar] [CrossRef] [PubMed]
- Arnold, L.M.; Hirsch, I.; Sanders, P.; Ellis, A.; Hughes, B. Safety and efficacy of esreboxetine in patients with fibromyalgia: A fourteen-week, randomized, double-blind, placebo-controlled, multicenter clinical trial. Arthritis Rheum. 2012, 64, 2387–2397. [Google Scholar] [CrossRef] [PubMed]
- Arnold, L.M.; Hess, E.V.; Hudson, J.I.; Welge, J.A.; Berno, S.E.; Keck, P.E. A randomized, placebo-controlled, double-blind, flexible-dose study of fluoxetine in the treatment of women with fibromyalgia. Am. J. Med. 2002, 112, 191–197. [Google Scholar] [CrossRef]
- Clauw, D.J.; Mease, P.; Palmer, R.H.; Gendreau, R.M.; Wang, Y. Milnacipran for the treatment of fibromyalgia in adults: A 15-week, multicentre, randomized, double-blind, placebo-controlled, multiple-dose clinical trial. Clin. Ther. 2008, 30, 1988–2004. [Google Scholar] [CrossRef] [PubMed]
- Gendreau, R.M.; Thorn, M.D.; Gendreau, J.F.; Kranzler, J.D.; Ribeiro, S.; Gracely, R.H.; Williams, D.A.; Mease, P.J.; McLean, S.A.; Clauw, D.J. Efficacy of milnacipran in patients with fibromyalgia. J. Rheumatol. 2005, 32, 1975–1985. [Google Scholar] [PubMed]
- Vitton, O.; Gendreau, M.; Gendreau, J.; Kranzler, J.; Rao, S.G. A double-blind placebo-controlled trial of milnacipran in the treatment of fibromyalgia. Hum. Psychopharmacol. 2004, 19, S27–S35. [Google Scholar] [CrossRef] [PubMed]
- Goldenberg, D.L.; Clauw, D.J.; Palmer, R.H.; Mease, P.; Chen, W.; Gendreau, R.M. Durability of therapeutic response to milnacipran treatment for fibromyalgia. Results of a randomized, double-blind, monotherapy 6-month extension study. Pain Med. 2010, 11, 180–194. [Google Scholar] [CrossRef] [PubMed]
- Arnold, L.M.; Gendreau, R.M.; Palmer, R.H.; Gendreau, J.F.; Wang, Y. Efficacy and safety of milnacipran 100 mg/day in patients with fibromyalgia: Results of a randomized, double-blind, placebo-controlled trial. Arthritis Rheum. 2010, 62, 2745–2756. [Google Scholar] [CrossRef] [PubMed]
- Patkar, A.A.; Masand, P.S.; Krulewicz, S.; Mannelli, P.; Peindl, K.; Beebe, K.L.; Jiang, W. A randomized, controlled, trial of controlled release paroxetine in fibromyalgia. Am. J. Med. 2007, 120, 448–454. [Google Scholar] [CrossRef] [PubMed]
- Pae, C.U.; Masand, P.S.; Marks, D.M.; Krulewicz, S.; Peindl, K.; Mannelli, P.; Patkar, A.A. History of depressive and/or anxiety disorders as a predictor of treatment response: A post hoc analysis of a 12-week, randomized, double-blind, placebo-controlled trial of paroxetine controlled release in patients with fibromyalgia. Prog. Neuropsychopharmacol. Biol. Psychiatry 2009, 31, 996–1002. [Google Scholar] [CrossRef] [PubMed]
- González-Viejo, M.A.; Avellanet, M.; Hernández-Morcuende, M.I. A comparative study of fibromyalgia treatment: Ultrasonography and physiotherapy versus sertraline treatment. Ann. Readapt. Med. Phys. 2005, 48, 610–615. [Google Scholar] [CrossRef] [PubMed]
- TD-9855. Available online: http://www.theravance.com/search?words=fibromyalgia (accessed on 8 March 2017).
- Morillas-Arques, P.; Rodriguez-Lopez, C.M.; Molina-Barea, R.; Rico-Villademoros, F.; Calandre, E.P. Trazodone for the treatment of fibromyalgia: An open-label, 12-week study. BMC Musculoskelet. Disord. 2010, 11, 204. [Google Scholar] [CrossRef] [PubMed]
- Sayar, K.; Aksu, G.; Ak, I.; Tosun, M. Venlafaxine treatment of fibromyalgia. Ann. Pharmacother. 2003, 37, 1561–1565. [Google Scholar] [CrossRef] [PubMed]
- Sindrup, S.H.; Otto, M.; Finnerup, N.B.; Jensen, T.S. Antidepressants in the treatment of neuropathic pain. Basic Clin. Pharmacol. Toxicol. 2005, 96, 399–409. [Google Scholar] [CrossRef] [PubMed]
- Jasmin, L.; Tien, D.; Weinshenker, D.; Palmiter, R.D.; Green, P.G.; Janni, G.; Ohara, P.T. The NK1 receptor mediates both the hyperalgesia and the resistance to morphine in mice lacking noradrenaline. Proc. Natl. Acad. Sci. USA 2002, 99, 1029–1034. [Google Scholar] [CrossRef] [PubMed]
- Sawynok, J. Topical and peripherally acting analgesics. Pharmacol. Rev. 2003, 55, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Reid, A.R.; Sawynok, J. Spinal serotonin 5-HT7 and adenosine A1 receptors, as well as peripheral adenosine A1 receptors, are involved in antinociception by systemically administered amitriptyline. Eur. J. Pharmacol. 2013, 698, 213–219. [Google Scholar] [CrossRef] [PubMed]
- Teitelbaum, J.; Johnson, C.; St Cyr, J. The use of d-ribose in chronic fatigue syndrome and fibromyalgia: A pilot study. J. Altern. Complement. Med. 2006, 12, 857–862. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, I.J.; Miller, R.J. Tricyclic antidepressants block N-methyl-d-aspartate receptors: Similarities to the action of zinc. Br. J. Pharmacol. 1988, 95, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Cai, Z.; McCaslin, P.P. Amitriptyline, desipramine, cyproheptadine and carbamazepine, in concentrations used therapeutically, reduce kainate- and N-methyl-d-aspartate-induced intracellular Ca2+ levels in neuronal culture. Eur. J. Pharmacol. 1992, 14, 53–57. [Google Scholar] [CrossRef]
- Ceko, M.; Bushnell, M.C.; Gracely, R.H. Neurobiology underlying fibromyalgia symptoms. Pain Res. Treat. 2012, 2012, 585419. [Google Scholar] [CrossRef] [PubMed]
- Wattiez, A.S.; Libert, F.; Privat, A.M.; Loiodice, S.; Fialip, J.; Eschalier, A.; Courteix, C. Evidence for a differential opioidergic involvement in the analgesic effect of antidepressants: Prediction for efficacy in animal models of neuropathic pain? Br. J. Pharmacol. 2011, 163, 792–803. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.K.; Russell, C.; Wang, S.Y. State-dependent block of voltage-gated Na+ channels by amitriptyline via the local anesthetic receptor and its implication for neuropathic pain. Pain 2004, 110, 166–174. [Google Scholar] [CrossRef] [PubMed]
- Galeotti, N.; Ghelardini, C.; Bartolini, A. Involvement of potassium channels in amitriptyline and clomipramine analgesia. Neuropharmacology 2001, 40, 75–78. [Google Scholar] [CrossRef]
- Tsantoulas, C.; McMahon, S.B. Opening paths to novel analgesics: The role of potassium channels in chronic pain. Trends Neurosci. 2014, 37, 146–158. [Google Scholar] [CrossRef] [PubMed]
- Raffa, R.B.; Pergolizzi, J.V., Jr. The evolving understanding of the analgesic mechanism of action of flupirtine. J. Clin. Pharm. Ther. 2012, 37, 4–6. [Google Scholar] [CrossRef] [PubMed]
- Wood, P.B.; Schweinhardt, P.; Jaeger, E.; Dagher, A.; Hakyemez, H.; Rabiner, E.A.; Bushnell, M.C.; Chizh, B.A. Fibromyalgia patients show an abnormal dopamine response to pain. Eur. J. Neurosci. 2007, 25, 3576–3582. [Google Scholar] [CrossRef] [PubMed]
- Horst, W.D.; Preskorn, S.H. Mechanisms of action and clinical characteristics of three atypical antidepressants: Venlafaxine, nefazodone, bupropion. J. Affect. Disord. 1998, 51, 237–254. [Google Scholar] [CrossRef]
- Gummersheimer, A.; Todd, T.; Herndon, C.M. Bupropion use for adjuvant analgesia in a patient with fibromyalgia: A case report. Fibrom. Open Access 2016, 1, 106. [Google Scholar]
- Palangio, M.; Flores, J.A.; Joyal, S.V. Treatment of fibromyalgia with sibutramine hydrochloride monohydrate: Comment on the article by Goldenberg et al. Arthritis Rheum. 2002, 46, 2545–2546. [Google Scholar] [CrossRef] [PubMed]
- Arnold, L.M.; Gebke, K.B.; Choy, E.H. Fibromyalgia: Management strategies for primary care providers. Int. J. Clin. Pract. 2016, 70, 99–112. [Google Scholar] [CrossRef] [PubMed]
- Luciano, J.V.; Forero, C.G.; Cerdà-Lafont, M.; Peñarrubia-María, M.T.; Fernández-Vergel, R.; Cuesta-Vargas, A.I.; Ruíz, J.M.; Rozadilla-Sacanell, A.; Sirvent-Alierta, E.; Santo-Panero, P.; et al. Functional status, quality of life, and costs associated with fibromyalgia subgroups: A latent profile analysis. Clin. J. Pain 2016, 32, 829–840. [Google Scholar] [CrossRef] [PubMed]
- Woodcock, J.; Witter, J.; Dionne, R.A. Stimulating the development of mechanism-based, individualized pain therapies. Nat. Rev. Drug Discov. 2007, 6, 703–710. [Google Scholar] [CrossRef] [PubMed]
| Drug | NET | SERT | DAT | Receptors | References | |||
|---|---|---|---|---|---|---|---|---|
| Adrenergic | Muscarinic | Histamine | 5-HT | |||||
| Ki/IC50 nM | Ki/IC50 nM | Ki/IC50 nM | IC50 nM | IC50 nM | IC50 nM | IC50 nM | ||
| Amitriptyline | 13.3–63 | 3.13–67 | 2580–7500 | 24–690 | 7.2–26 | 1.1(H1), 1000(H3), 33.6(H4) | 450(1A), 40(1B), 4(2A), 40(2B), 6(2C), 89–103(6), 126–398(7) | [10,11,12] |
| Citalopram | 4870–>10,000 | 1.13–19.0 | >10,000 | 560–1211 | 1430 | 180–286 | 617–6000(2) | [10,13,14] |
| Cyclobenzaprine | 126 | 251 | 7943 | 10–110 | 8–30 | 1–6 | 20(2A), 200(2B), 62(2C), 40(6), 69(7) | [11] |
| Duloxetine | 1.17–42 | 0.07–13 | 200–439 | 8300–8600 | 3000 | 2300 | 504(2A), 419(6) | [10,15,16,17,18,19] |
| Fluoxetine | 563–1021 | 1.0–10 | 4180 | 3000 | 870–2700 | 3250 | 200(2A), 5000(2B), 73(2C) | [12,16,18,20] |
| Milnacipran | 22–200 | 8.4–151 | >100,000 | >10,000 | >10,000 | >10,000 | >10,000 | [10,16,18,19] |
| Nortriptyline | 1.49–8.3 | 16.5–317 | 1200–5000 | 55–2030 | 40–110 | 15.1(H1) | 294(1A), 5(2A), 8.5(2C), 148(6) | [10,12] |
| Paroxetine | 100–156 | 0.34–2 | 963 | 2741 | 72–340 | >10,000 | 9034(2C) | [12,14,16,20] |
| Reboxetine | 3–13.4 | 242–274 | >10,000 | >10000 | 6700 | 312 | 457(2C) | [12,14,16] |
| Sertraline | 715–925 | 0.9–2.8 | 315 | 188 | 427 | 6578 | 2298(2C) | [18,20] |
| TD-9855 | 2–4 | 3–10 | 160–200 | N/A | N/A | N/A | N/A | [21] |
| Trazodone | >10,000 | 367 | >7000 | 153–728 | >10,000 | 220(H1), 3290(H2) | 118(1A), 106(1D), 36(2A), 78(2B), 224(2C), 1780(7) | [12] |
| Venlafaxine | 538–2483 | 7.8–145 | 3070–7647 | >10,000 | >10,000 | >10,000 | 2000(2), 2800(6) | [10,13,16,17,18,19] |
| Drug | Dose (mg/day) | FIQ | Patient’s Global Assessment | Symptoms | References | |||
|---|---|---|---|---|---|---|---|---|
| Pain | Fatigue | Sleep | Anxiety and Depression | |||||
| Amitriptyline | 10–100 | −13 to −19 | −0.5 to −3.8 87% # | −0.4 to −5.3 | −2.2 to 3.5 80−93% # | −1.1 to −3.9 63−100% # | HDRS −9.9 to −10.4 BDI −6.2 to −7.0 50% # | [29,30,31,32,33,34,35,36,37,38,39,40,41] |
| Citalopram | 20–40 | 52.9% # | −1.2 | −0.59 | MADRS −4.0 | [42] | ||
| Cyclobenzaprine (TNX102SL) | 10 VLD 1–4 | −0.9 | No effect | Parameters improved 12.3−38.5% | Improved 24.1% | [43,44,45,46,47] | ||
| Duloxetine | 30–120 | −7.96 to −18.4 | −2.79 to −3.43 | −1.6 to −2.4 | −0.33 to −3.8 | −2.67 to −2.69 Caused insomnia | BDI −3.32 to −5.47 HDRS −2.04 to −7.8 | [48,49,50,51,52,53,54,55,56] |
| Esreboxetine | 4–10 | −3.9 to −7.2 | 40−42.6% # | −0.4 to −0.76 | −0.59 to −0.64 | Caused insomnia | [57] | |
| Fluoxetine | 10–80 | −10.9 to −11.5 | −1.77 | −2.3 to −2.4 | −1.6 | −0.86 | No effect | [32,58] |
| Milnacipran | 30–200 | −12.3 to −26 | 35−51% # | −1.6 to −3.5 | −4.3 to −7.3 | No effect | BDI −2.1 to −4.9 | [59,60,61,62,63] |
| Paroxetine | 12.5–62.5 | −6.6 to −6.8 | 45−55% # | −0.95 | −4.6 to −4.9 | BDI −4.6 to −5.8 | [64,65] | |
| Sertraline | 50 | 83% # | −4.2 | MOS Score −15 | [66] | |||
| TD-9855 | 20 | −16.2 | 48% # | −1.4 | Caused insomnia | [67] | ||
| Trazodone | 50–300 | −9.6 to −13.4 | −0.52 to −1.41 | −0.72 to −1.17 | −4.2 to −5.0 | HDRS −1.4 to −2.0 HAM-A −1.5 to −2.4 BDI −5.5 to −8.9 | [68] | |
| Venlafaxine | 75–300 | −9.0 to −19.9 | 51% # | −1.87 to −2.14 | 35% # | HDRS −3.6 to −4.65 HAM-A −7.14 to −13.5 BAI −8.5 BDI −7.9 | [34,69] | |
© 2017 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lawson, K. A Brief Review of the Pharmacology of Amitriptyline and Clinical Outcomes in Treating Fibromyalgia. Biomedicines 2017, 5, 24. https://doi.org/10.3390/biomedicines5020024
Lawson K. A Brief Review of the Pharmacology of Amitriptyline and Clinical Outcomes in Treating Fibromyalgia. Biomedicines. 2017; 5(2):24. https://doi.org/10.3390/biomedicines5020024
Chicago/Turabian StyleLawson, Kim. 2017. "A Brief Review of the Pharmacology of Amitriptyline and Clinical Outcomes in Treating Fibromyalgia" Biomedicines 5, no. 2: 24. https://doi.org/10.3390/biomedicines5020024
APA StyleLawson, K. (2017). A Brief Review of the Pharmacology of Amitriptyline and Clinical Outcomes in Treating Fibromyalgia. Biomedicines, 5(2), 24. https://doi.org/10.3390/biomedicines5020024







