Long-Term Results of Autologous Tooth Bone Grafting in Alveolar Cleft Reconstruction: A Retrospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Selection
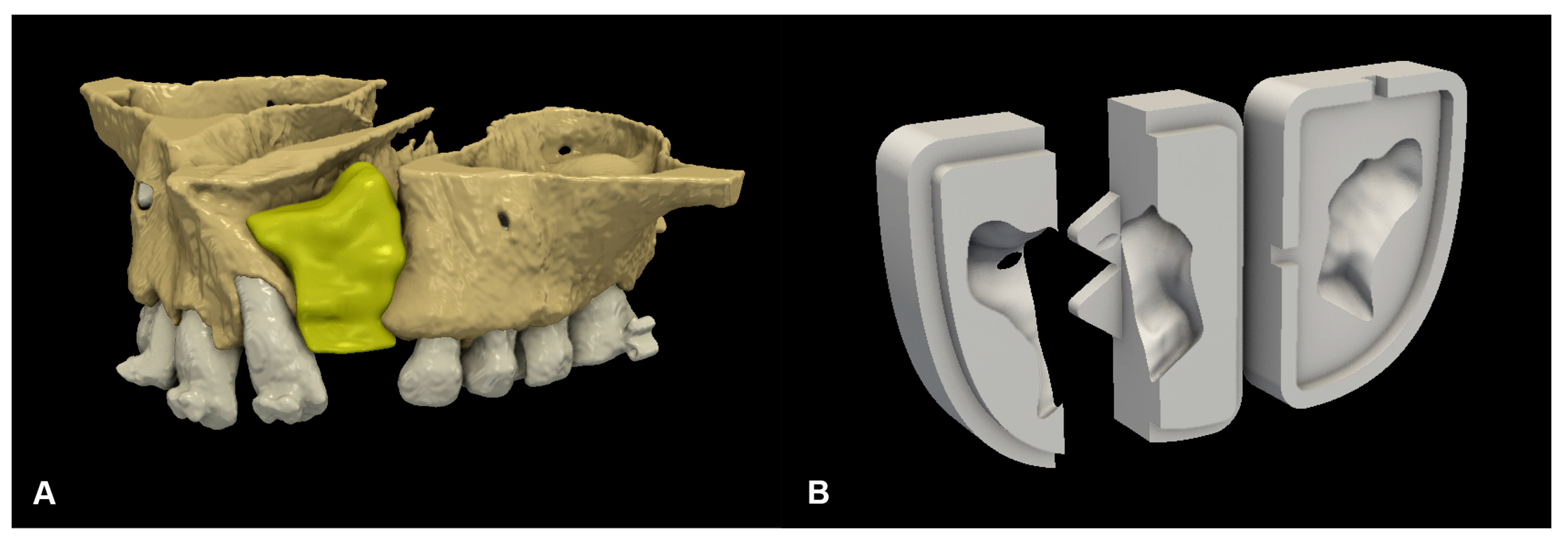
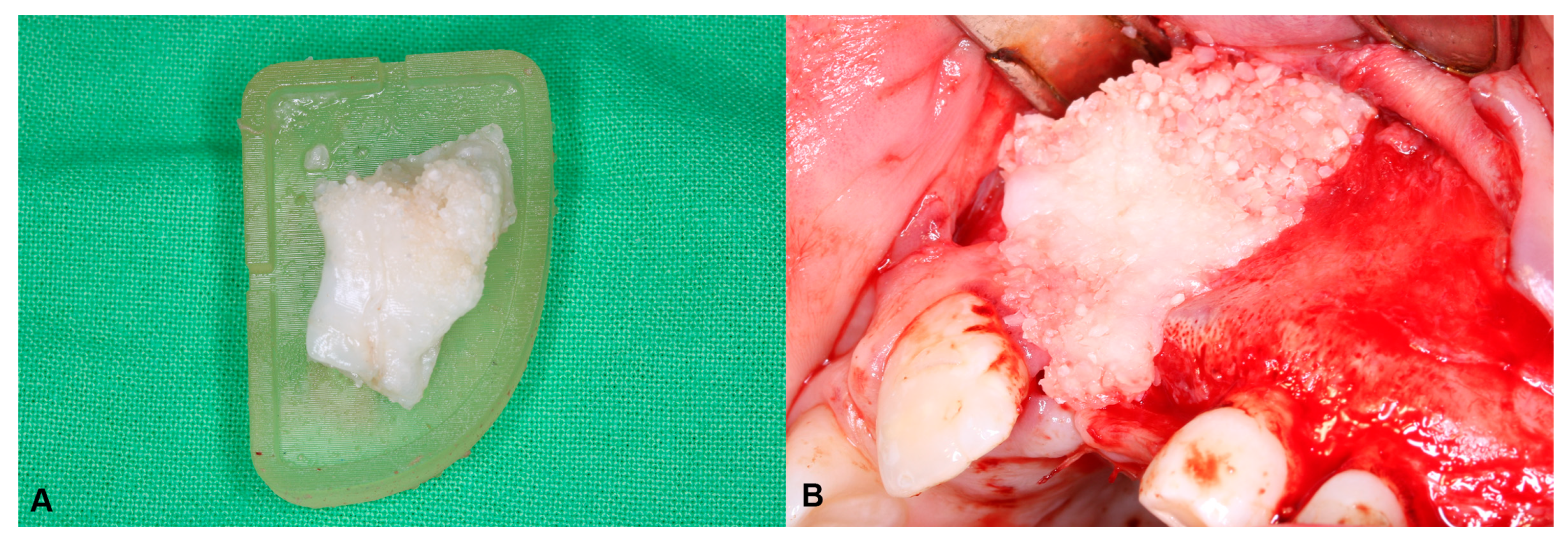
2.2. Surgical Protocol
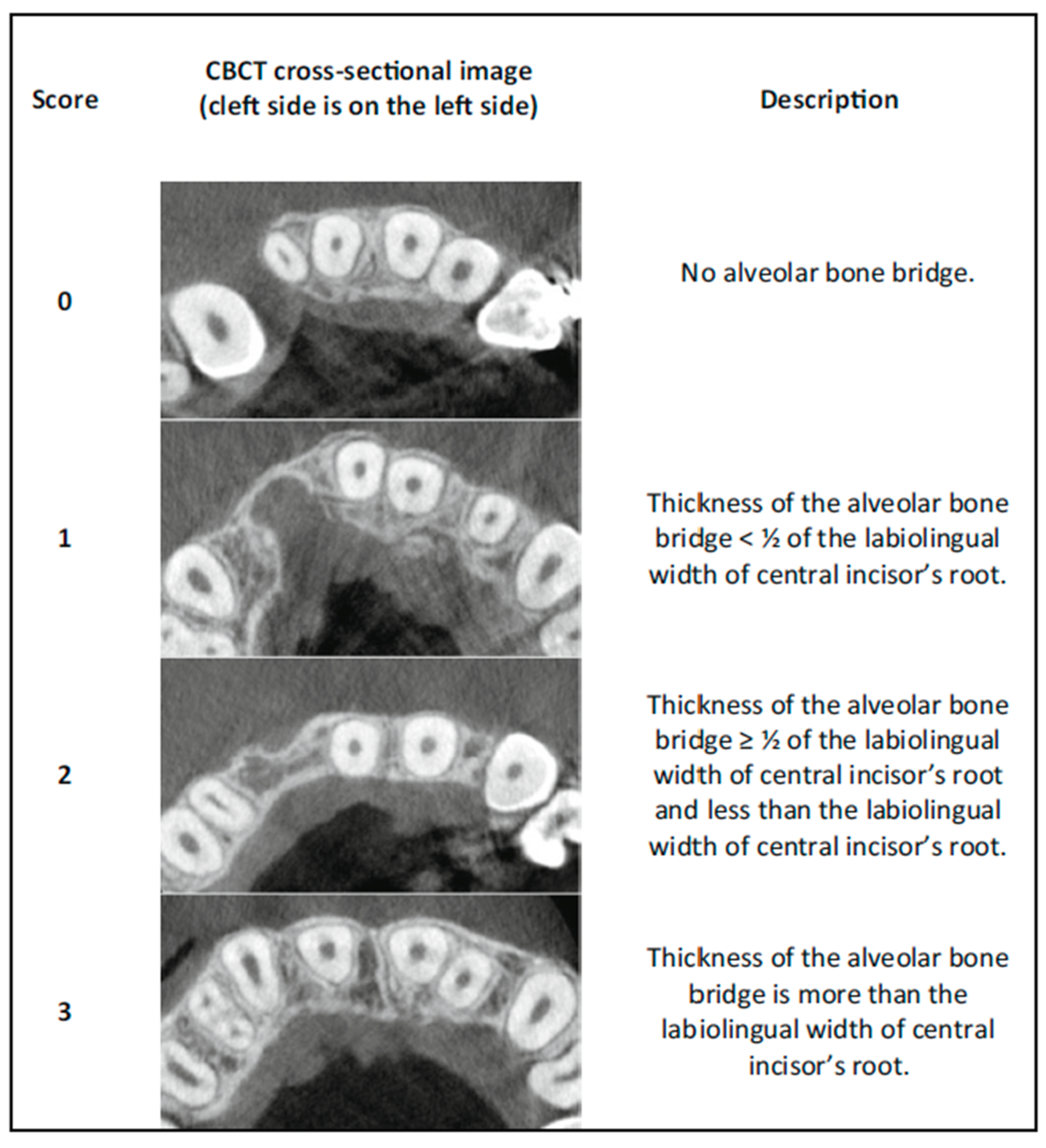
2.3. Radiographic Image Acquisition and Assessment of Surgical Outcomes
- 0 = No alveolar bone bridge;
- 1 = The thickness of the alveolar bone bridge < ½ of the labiolingual width of the central incisor’s root;
- 2 = The thickness of the alveolar bone bridge ≥ ½ of the labiolingual width of the central incisor’s root and less than the labiolingual width of the central incisor’s root;
- 3 = The thickness of the alveolar bone bridge is at least the labiolingual width of the central incisor’s root (Figure 3).
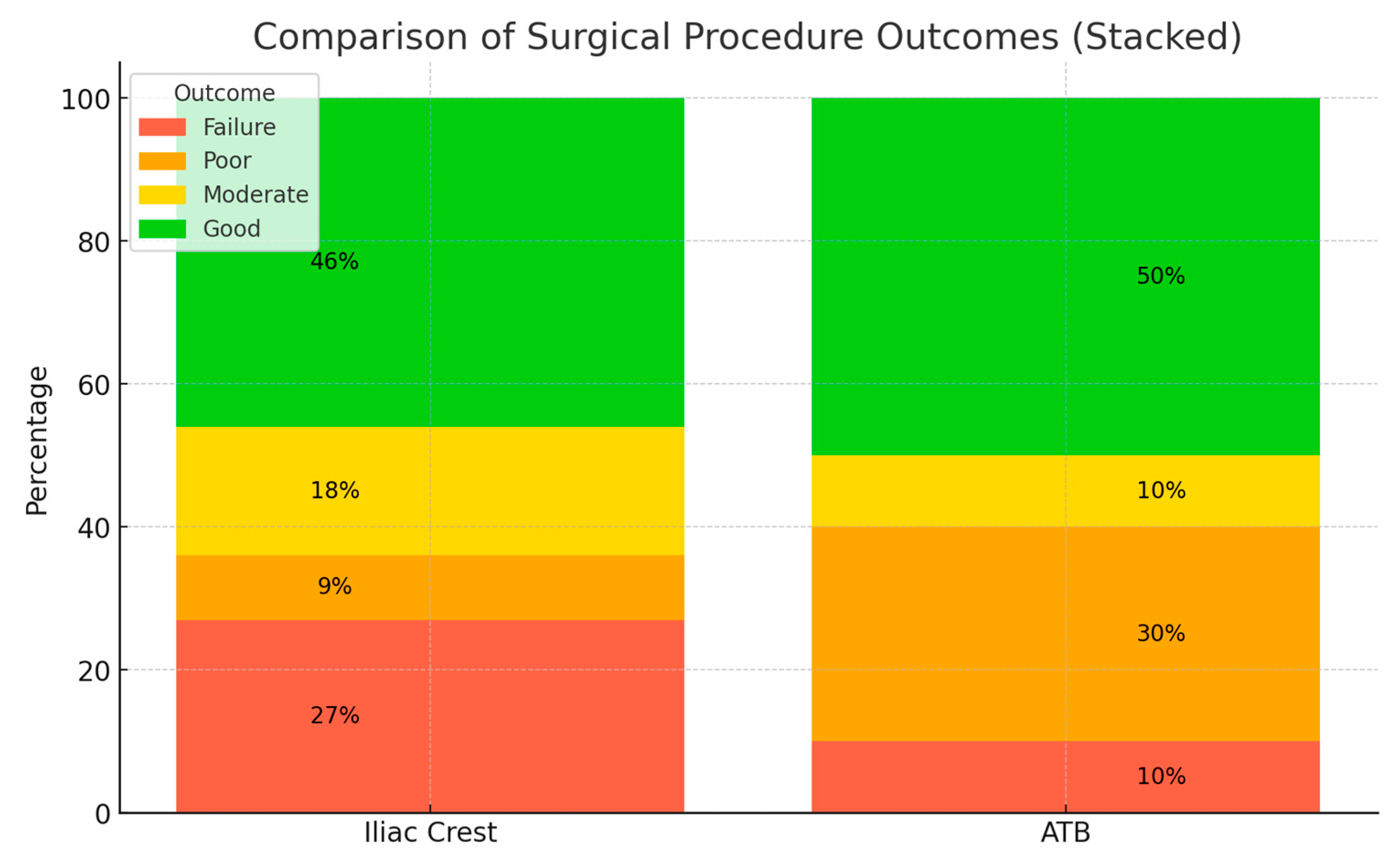
- 0 = Failure;
- 1–4 = Poor outcome;
- 5–8 = Moderate outcome;
- 9–12 = Good outcome.
2.4. Statistical Analysis
3. Results
3.1. Patient Demographics and Descriptive Statistics
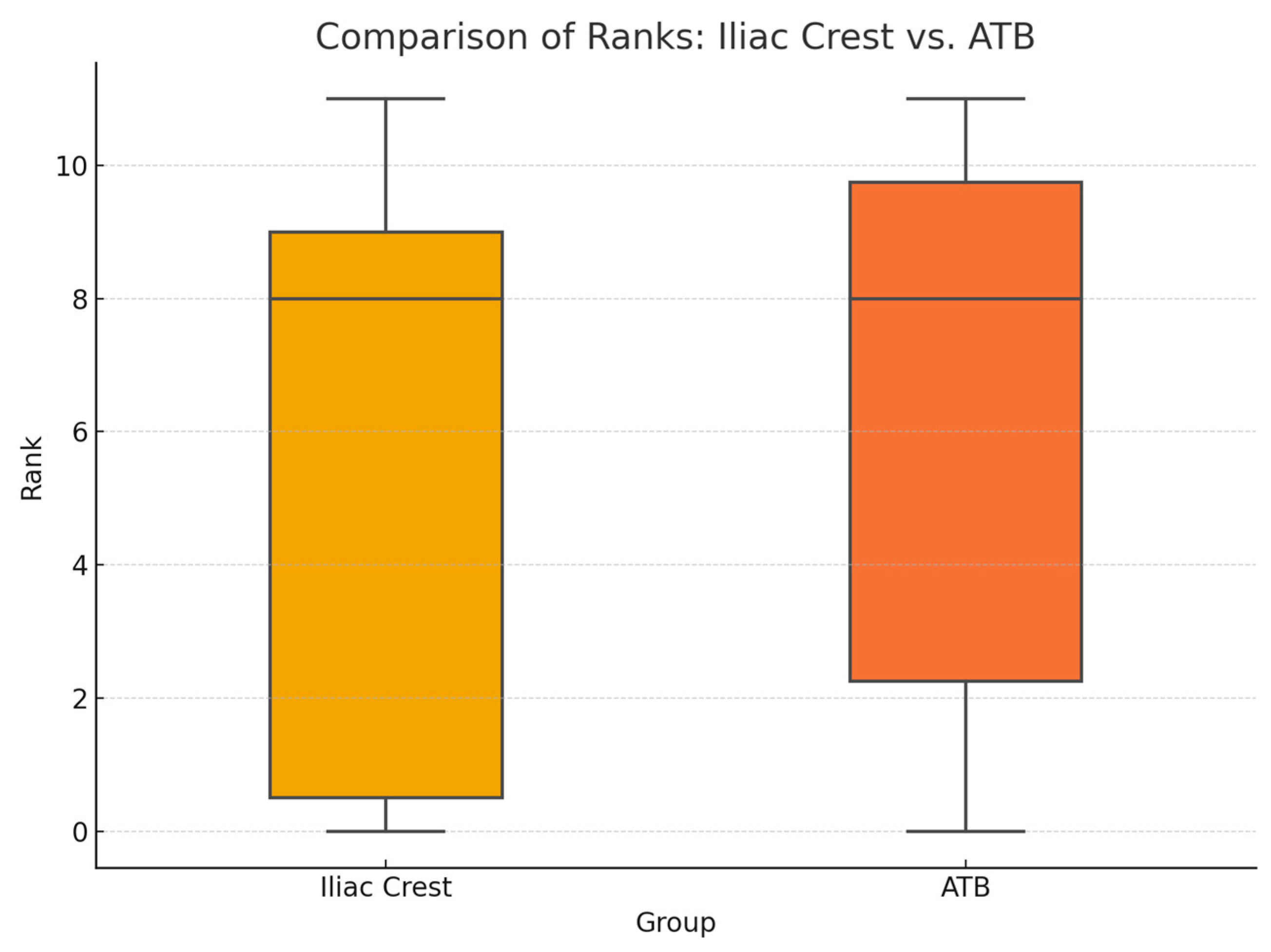
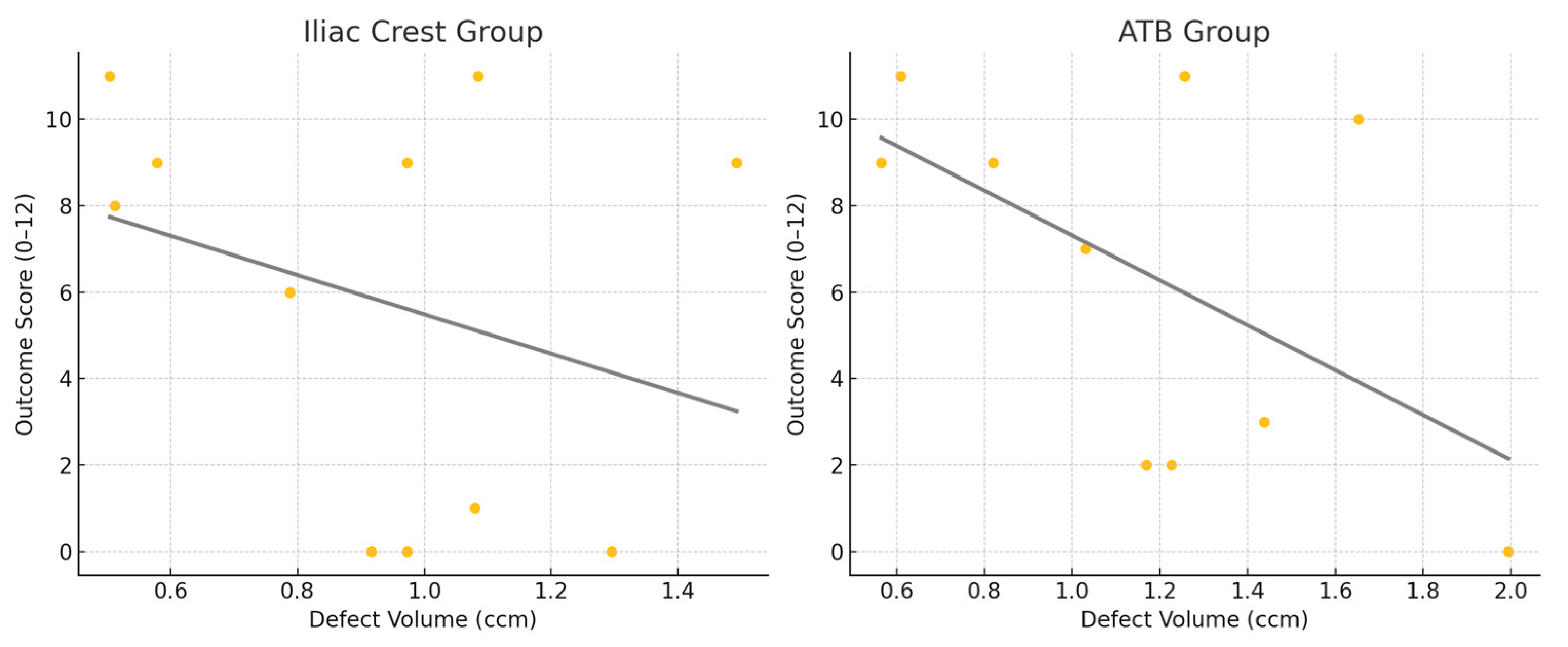
3.2. Radiographical Assessment
3.3. Statistical Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CLP | Cleft lip and palate |
| ABG | Alveolar bone grafting |
| ATB | Auto-tooth bone |
| PRP | Platelet-rich plasma |
| L-PRF | Leukocyte–platelet rich fibrin |
| BMP | Bone morphogenic protein |
| HA | Hydroxyapatite |
| CT | Computed tomography |
| CBCT | Cone-beam computed tomography |
| UCLP | Unilateral cleft lip and palate |
| STL | Standard tessellation language |
| CAD | Computer-aided design |
| SLA | Stereolithography |
| CEJ | Cementoenamel junction |
References
- Acs, L.; Nemes, B.; Nagy, K.; Acs, M.; Banhidy, F.; Rozsa, N. Maternal factors in the origin of cleft lip/cleft palate: A population-based case-control study. Orthod. Craniofacial Res. 2024, 27 (Suppl. S1), 6–13. [Google Scholar] [CrossRef] [PubMed]
- Vandersluis, Y.R.; Fisher, D.M.; Stevens, K.; Tompson, B.D.; Lou, W.; Suri, S. Comparison of dental outcomes in patients with nonsyndromic complete unilateral cleft lip and palate who receive secondary alveolar bone grafting before or after emergence of the permanent maxillary canine. Am. J. Orthod. Dentofac. Orthop. 2020, 157, 668–679. [Google Scholar] [CrossRef] [PubMed]
- Fahradyan, A.; Tsuha, M.; Wolfswinkel, E.M.; Mitchell, K.S.; Hammoudeh, J.A.; Magee, W., 3rd. Optimal Timing of Secondary Alveolar Bone Grafting: A Literature Review. J. Oral. Maxillofac. Surg. 2019, 77, 843–849. [Google Scholar] [CrossRef] [PubMed]
- Åbyholm, F.E.; Olav, B.; Semb, G. Secondary Bone Grafting of Alveolar Clefts: A Surgical/Orthodontic Treatment Enabling a Non-prosthodontic Rehabilitation in Cleft Lip and Palate Patients. Scand. J. Plast. Reconstr. Surg. 1981, 15, 127–140. [Google Scholar] [CrossRef] [PubMed]
- Boyne, P.J.; Sands, N.R. Secondary bone grafting of residual alveolar and palatal clefts. J. Oral Surg. 1972, 30, 87–92. [Google Scholar] [PubMed]
- Dimitriou, R.; Mataliotakis, G.I.; Angoules, A.G.; Kanakaris, N.K.; Giannoudis, P.V. Complications following autologous bone graft harvesting from the iliac crest and using the RIA: A systematic review. Injury 2011, 42 (Suppl. S2), S3–S15. [Google Scholar] [CrossRef] [PubMed]
- Brezulier, D.; Chaigneau, L.; Jeanne, S.; Lebullenger, R. The Challenge of 3D Bioprinting of Composite Natural Polymers PLA/Bioglass: Trends and Benefits in Cleft Palate Surgery. Biomedicines 2021, 9, 1553. [Google Scholar] [CrossRef] [PubMed]
- Ellapakurthi, P.; Reddy, G.S.P. The effectiveness of mineralized plasmatic matrix in the closure of alveolar clefts with volumetric assessment. Regen. Med. Res. 2021, 9, 1. [Google Scholar] [CrossRef] [PubMed]
- Janssen, N.G.; Weijs, W.L.; Koole, R.; Rosenberg, A.J.; Meijer, G.J. Tissue engineering strategies for alveolar cleft reconstruction: A systematic review of the literature. Clin. Oral. Investig. 2014, 18, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.; Pan, W.; Feng, C.; Su, Z.; Duan, Z.; Zheng, Q.; Hua, C.; Li, C. Grafting materials for alveolar cleft reconstruction: A systematic review and best-evidence synthesis. Int. J. Oral. Maxillofac. Surg. 2018, 47, 345–356. [Google Scholar] [CrossRef] [PubMed]
- Leal, C.R.; de Carvalho, R.M.; Ozawa, T.O.; de Almeida, A.M.; da Silva Dalben, G.; da Cunha Bastos, J.C., Jr.; Garib, D.G. Outcomes of Alveolar Graft With Rhbmp-2 in CLP: Influence of Cleft Type and Width, Canine Eruption, and Surgeon. Cleft Palate Craniofacial J. 2019, 56, 383–389. [Google Scholar] [CrossRef] [PubMed]
- Hussain, A.A.; Al-Quisi, A.F.; Abdulkareem, A.A. Efficacy of Autogenous Dentin Biomaterial on Alveolar Ridge Preservation: A Randomized Controlled Clinical Trial. Biomed Res. Int. 2023, 2023, 7932432. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.K.; Kim, S.G.; Yun, P.Y.; Yeo, I.S.; Jin, S.C.; Oh, J.S.; Kim, H.J.; Yu, S.K.; Lee, S.Y.; Kim, J.S.; et al. Autogenous teeth used for bone grafting: A comparison with traditional grafting materials. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2014, 117, e39–e45. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.K.; Kim, S.G.; Byeon, J.H.; Lee, H.J.; Um, I.U.; Lim, S.C.; Kim, S.Y. Development of a novel bone grafting material using autogenous teeth. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2010, 109, 496–503. [Google Scholar] [CrossRef] [PubMed]
- Lorenzoni, D.C.; Janson, G.; Bastos, J.C.; Carvalho, R.M.; Bastos, J.C., Jr.; de Cassia Moura Carvalho Lauris, R.; Henriques, J.F.; Ozawa, T.O. Evaluation of secondary alveolar bone grafting outcomes performed after canine eruption in complete unilateral cleft lip and palate. Clin. Oral Investig. 2017, 21, 267–273. [Google Scholar] [CrossRef] [PubMed]
- Lemberger, M.; Benchimol, D.; Pegelow, M.; Jacobs, R.; Karsten, A. Validation and comparison of 2D grading scales and 3D volumetric measurements for outcome assessment of bone-grafted alveolar clefts in children. Eur. J. Orthod. 2024, 46, cjae002. [Google Scholar] [CrossRef] [PubMed]
- Major, M.; Meszaros, B.; Wursching, T.; Polyak, M.; Kammerhofer, G.; Nemeth, Z.; Szabo, G.; Nagy, K. Evaluation of a Structured Light Scanner for 3D Facial Imaging: A Comparative Study with Direct Anthropometry. Sensors 2024, 24, 5286. [Google Scholar] [CrossRef] [PubMed]
- Wursching, T.; Kesztyus, A.; Pottel, L.; Swennen, G.; Nagy, K. Comparison of two methods for segmentation of the nasoalveolar defect and design of a three-dimensional surgical template in patients with cleft lip and palate: A retrospective study. Int. J. Oral Maxillofac. Surg. 2025. [Google Scholar] [CrossRef] [PubMed]
- Fabian, Z.; Kadar, K.; Patonay, L.; Nagy, K. Application of 3D Printed Biocompatible Plastic Surgical Template for the Reconstruction of a Nasoalveolar Cleft with Preoperative Volume Analysis. Mater. Plast. 2019, 56, 413–415. [Google Scholar] [CrossRef]
- Molnar, B.; Wursching, T.; Solyom, E.; Palvolgyi, L.; Radoczy-Drajko, Z.; Palkovics, D.; Nagy, K. Alveolar cleft reconstruction utilizing a particulate autogenous tooth graft and a novel split-thickness papilla curtain flap—A retrospective study. J. Cranio-Maxillofac. Surg. 2024, 52, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Kesztyus, A.; Wursching, T.; Nemes, B.; Palvolgyi, L.; Nagy, K. Evaluation of 3D visualization, planning and printing techniques in alveolar cleft repair, and their effect on patients’ burden. J. Stomatol. Oral Maxillofac. Surg. 2022, 123, 484–489. [Google Scholar] [CrossRef] [PubMed]
- Stasiak, M.; Wojtaszek-Slominska, A.; Racka-Pilszak, B. A novel method for alveolar bone grafting assessment in cleft lip and palate patients: Cone-beam computed tomography evaluation. Clin. Oral Investig. 2021, 25, 1967–1975. [Google Scholar] [CrossRef] [PubMed]
- Radoczy-Drajko, Z.; Windisch, P.; Svidro, E.; Tajti, P.; Molnar, B.; Gerber, G. Clinical, radiographical and histological evaluation of alveolar ridge preservation with an autogenous tooth derived particulate graft in EDS class 3–4 defects. BMC Oral Health 2021, 21, 63. [Google Scholar] [CrossRef] [PubMed]
- Solyom, E.; Szalai, E.; Czumbel, M.L.; Szabo, B.; Vancsa, S.; Mikulas, K.; Radoczy-Drajko, Z.; Varga, G.; Hegyi, P.; Molnar, B.; et al. The use of autogenous tooth bone graft is an efficient method of alveolar ridge preservation—Meta-analysis and systematic review. BMC Oral Health 2023, 23, 226. [Google Scholar] [CrossRef] [PubMed]
- Jeong, K.-I.; Lee, J.; Kim, K.-W.; Um, I.-W.; Hara, S.; Mitsugi, M.; Kim, Y.-K. Alveolar Cleft Reconstruction Using Chin Bone and Autogenous Tooth Bone Graft Material: Reports of 5 Cases. J. Korean Dent. Sci. 2013, 6, 13–21. [Google Scholar] [CrossRef]
- Datarkar, A.; Bhawalkar, A. Utility of tooth as an autogenous graft material in the defects of alveolar cleft—A novel case report. J. Oral Biol. Craniofacial Res. 2020, 10, 470–473. [Google Scholar] [CrossRef] [PubMed]
- Hara, S.; Mitsugi, M.; Kanno, T.; Tatemoto, Y. Bone transport and bone graft using auto-tooth bone for alveolar cleft repair. J. Craniofacial Surg. 2013, 24, e65–e68. [Google Scholar] [CrossRef] [PubMed]
- Brudnicki, A.; Regulski, P.A.; Sawicka, E.; Fudalej, P.S. Alveolar Volume Following Different Timings of Secondary Bone Grafting in Patients with Unilateral Cleft Lip and Palate. A Pilot Study. J. Clin. Med. 2021, 10, 3524. [Google Scholar] [CrossRef] [PubMed]
- Yu, X.; Huang, Y.; Li, W. Correlation between alveolar cleft morphology and the outcome of secondary alveolar bone grafting for unilateral cleft lip and palate. BMC Oral Health 2022, 22, 251. [Google Scholar] [CrossRef] [PubMed]
- Jahanbin, A.; Kamyabnezhad, E.; Raisolsadat, M.A.; Farzanegan, F.; Bardideh, E. Long-Term Stability of Alveolar Bone Graft in Cleft Lip and Palate Patients: Systematic Review and Meta-Analysis. J. Craniofacial Surg. 2022, 33, e194–e200. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Batra, P.; Sharma, K.; Raghavan, S.; Talwar, A.; Srivastava, A.; Sood, S.C. A Three-Dimensional Scale for the Qualitative and Quantitative Assessments of Secondary Alveolar Bone Grafting (SABG) in Unilateral Cleft Lip and Palate Patients Using Cone-Beam Computed Tomography (CBCT). Indian. J. Plast. Surg. 2022, 56, 138–146. [Google Scholar] [CrossRef] [PubMed]
- Shaheen, E.; Danneels, M.; Doucet, K.; Dormaar, T.; Verdonck, A.; Cadenas de Llano-Perula, M.; Willems, G.; Politis, C.; Jacobs, R. Validation of a 3D methodology for the evaluation and follow-up of secondary alveolar bone grafting in unilateral cleft lip and palate patients. Orthod. Craniofacial Res. 2022, 25, 377–383. [Google Scholar] [CrossRef] [PubMed]
- Suomalainen, A.; Aberg, T.; Rautio, J.; Hurmerinta, K. Cone beam computed tomography in the assessment of alveolar bone grafting in children with unilateral cleft lip and palate. Eur. J. Orthod. 2014, 36, 603–611. [Google Scholar] [CrossRef] [PubMed]

| Iliac Crest | Vdefect (cm3) | Dehiscence | Fistula | Canine | Stasiak Score | Age at Surgery (years) | Follow-Up (months) |
|---|---|---|---|---|---|---|---|
| Patient 1 | 1.085 | no | no | erupted | 11 | 9 | 58 |
| Patient 2 | 1.492 | yes | fistula | erupted | 9 | 14 | 24 |
| Patient 3 | 0.973 | no | no | erupted | 0 | 14 | 41 |
| Patient 4 | 0.578 | no | no | erupted | 9 | 12 | 36 |
| Patient 5 | 0.504 | yes | no | erupted | 11 | 13 | 14 |
| Patient 6 | 0.916 | no | no | erupted | 0 | 10 | 49 |
| Patient 7 | 0.973 | no | no | erupted | 9 | 8 | 18 |
| Patient 8 | 0.788 | no | fistula | erupted | 6 | 10 | 24 |
| Patient 9 | 0.512 | no | no | erupted | 8 | 9 | 52 |
| Patient 10 | 1.295 | no | no | erupted | 0 | 10 | 12 |
| Patient 11 | 1.079 | yes | no | erupted | 1 | 11 | 56 |
| ATB | Vdefect (cm3) | Dehiscence | Fistula | Canine | Stasiak Score | Age at Surgery (years) | Follow-Up (months) |
|---|---|---|---|---|---|---|---|
| Patient 12 | 1.994 | no | no | not erupted | 0 | 10 | 28 |
| Patient 13 | 0.819 | no | no | erupted | 9 | 9 | 25 |
| Patient 14 | 1.653 | yes | no | erupted | 10 | 8 | 20 |
| Patient 15 | 1.03 | no | no | erupted | 7 | 11 | 20 |
| Patient 16 | 1.226 | yes | 21 perio | erupted | 2 | 11 | 26 |
| Patient 17 | 0.609 | no | no | erupted | 11 | 11 | 28 |
| Patient 18 | 1.438 | no | no | not erupted | 3 | 8 | 29 |
| Patient 19 | 1.256 | no | no | erupted | 11 | 10 | 25 |
| Patient 20 | 1.169 | no | fistula | erupted | 2 | 11 | 25 |
| Patient 21 | 0.565 | no | no | erupted | 9 | 10 | 23 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Würsching, T.; Mészáros, B.; Sólyom, E.; Molnár, B.; Bogdán, S.; Németh, Z.; Nagy, K. Long-Term Results of Autologous Tooth Bone Grafting in Alveolar Cleft Reconstruction: A Retrospective Cohort Study. Biomedicines 2025, 13, 1735. https://doi.org/10.3390/biomedicines13071735
Würsching T, Mészáros B, Sólyom E, Molnár B, Bogdán S, Németh Z, Nagy K. Long-Term Results of Autologous Tooth Bone Grafting in Alveolar Cleft Reconstruction: A Retrospective Cohort Study. Biomedicines. 2025; 13(7):1735. https://doi.org/10.3390/biomedicines13071735
Chicago/Turabian StyleWürsching, Tamás, Bence Mészáros, Eleonóra Sólyom, Bálint Molnár, Sándor Bogdán, Zsolt Németh, and Krisztián Nagy. 2025. "Long-Term Results of Autologous Tooth Bone Grafting in Alveolar Cleft Reconstruction: A Retrospective Cohort Study" Biomedicines 13, no. 7: 1735. https://doi.org/10.3390/biomedicines13071735
APA StyleWürsching, T., Mészáros, B., Sólyom, E., Molnár, B., Bogdán, S., Németh, Z., & Nagy, K. (2025). Long-Term Results of Autologous Tooth Bone Grafting in Alveolar Cleft Reconstruction: A Retrospective Cohort Study. Biomedicines, 13(7), 1735. https://doi.org/10.3390/biomedicines13071735






