Left Ventricular Assist Device (LVAD)-Related Major Adverse Events Account for a Low Number of Emergency Room Admissions in HeartMate 3™ Patients—A 10-Year Retrospective Study
Abstract
1. Introduction
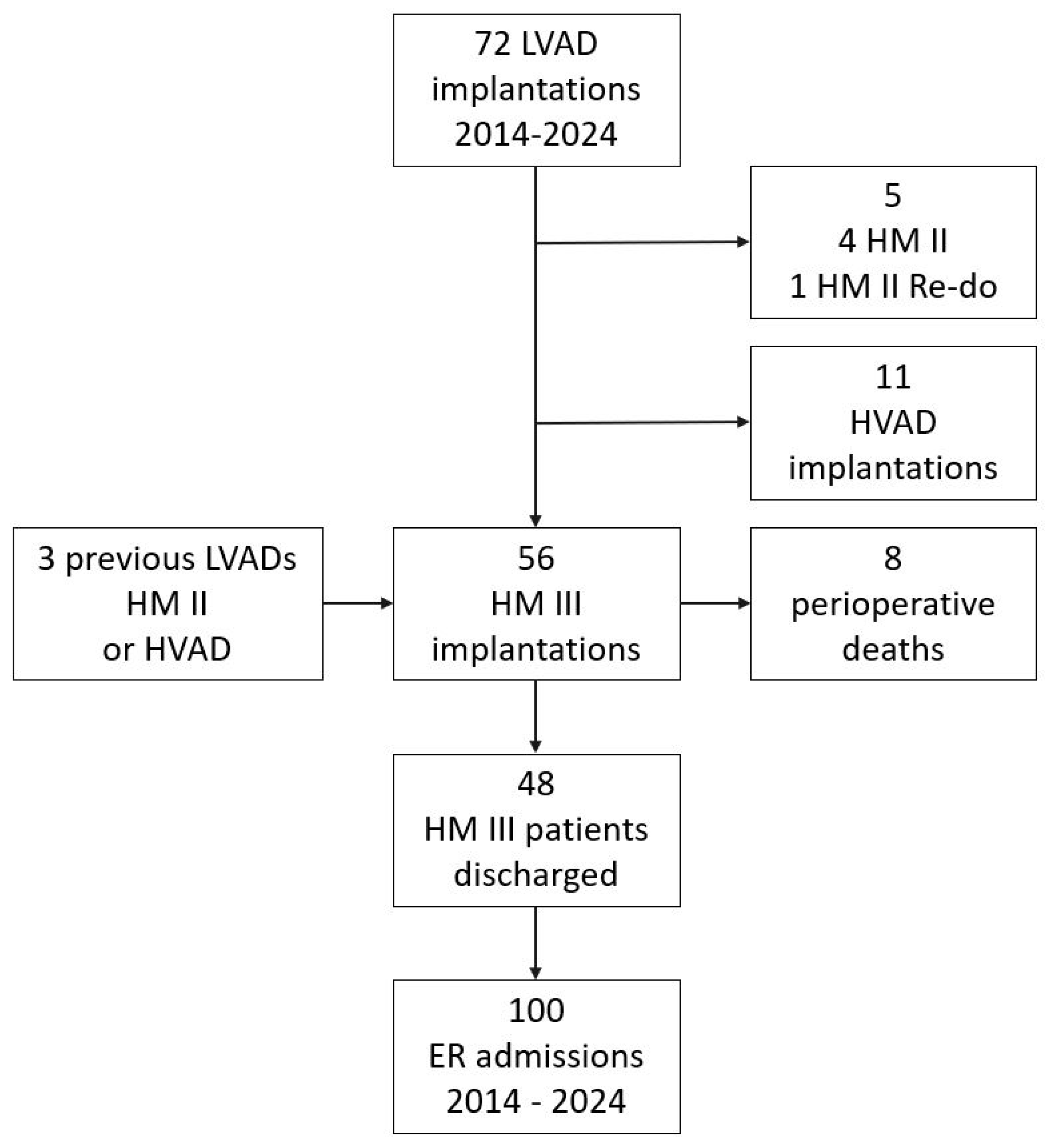
2. Materials and Methods
2.1. Study Design
2.2. Metrics
2.3. Statistics
3. Results
3.1. Baseline Characteristics
3.2. Emergency Room Admissions
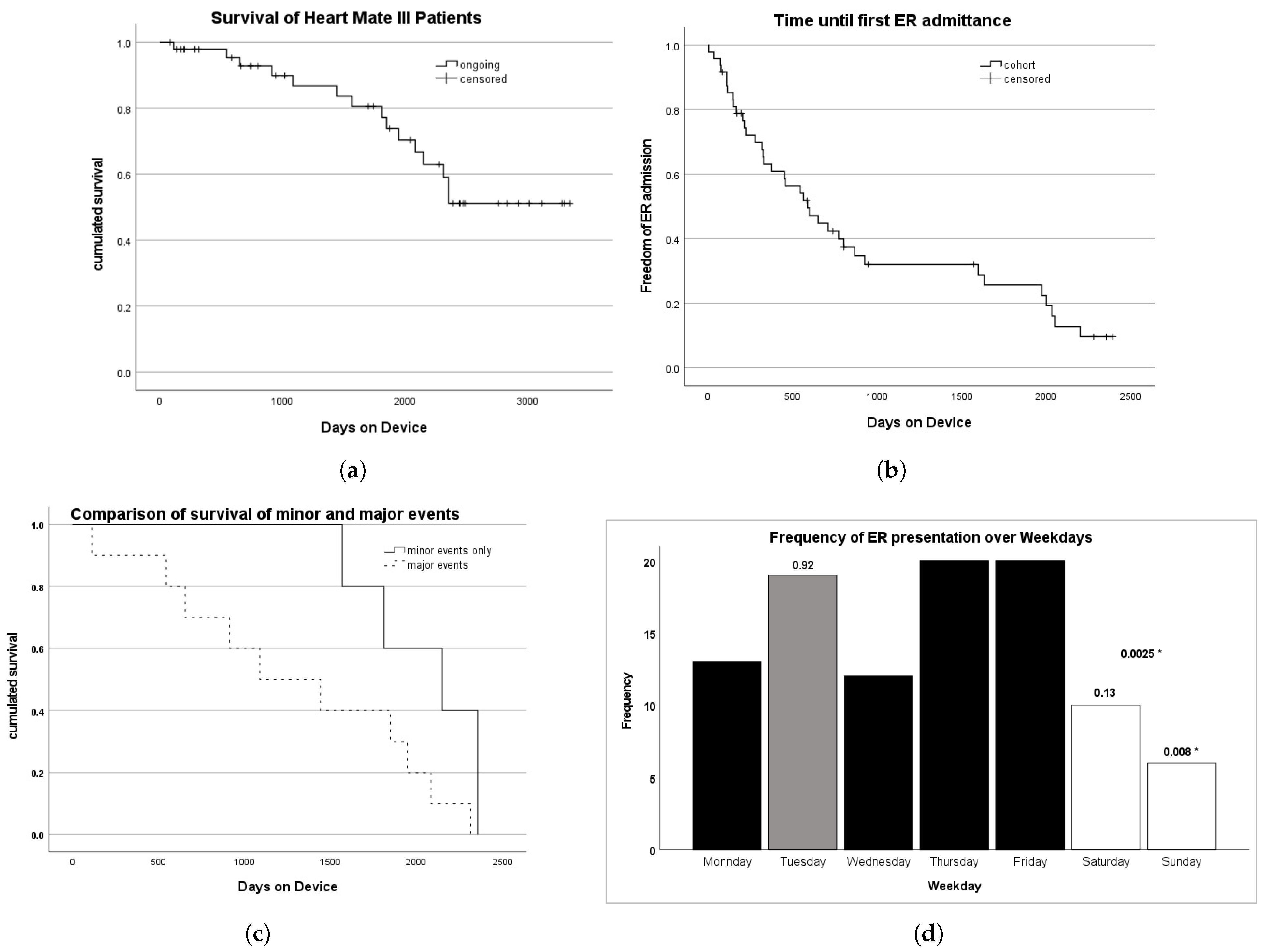
3.3. Survival and Freedom from Emergency Room Admission
3.4. LVAD-RelatedAdmissions to the Emergency Room
3.4.1. Causes of Death
General Causes of All Deaths
Death After Emergency Room Admittance
4. Discussion
4.1. Principal Findings and Clinical Interpretation
4.2. Role of LVAD Clinics and Temporal Presentation Patterns
4.3. Integration with Existing Literature
4.4. Recommendations for Emergency Care
- Do not assume an LVAD-related pathology; initial evaluation should follow standard emergency workups.
- Mental status, vital signs, and primary complaints should guide triage decisions.
- Contact the LVAD patient reference center when necessary, but avoid unnecessary delays in treatment.
- Check for anticoagulation, battery status, and LVAD alarms.
4.5. Limitations and Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Schmitto, J.D.; Hanke, J.S.; Rojas, S.V.; Avsar, M.; Haverich, A. First implantation in man of a new magnetically levitated left ventricular assist device (HeartMate III). J. Heart Lung Transplant. 2015, 34, 858–860. [Google Scholar] [CrossRef] [PubMed]
- Dembitsky, W.P.; Tector, A.J.; Park, S.; Moskowitz, A.J.; Gelijns, A.C.; Ronan, N.S.; Piccione, W.; Holman, W.L.; Furukawa, S.; Weinberg, A.D.; et al. Left Ventricular Assist Device Performance with Long-Term Circulatory Support: Lessons from the REMATCH Trial. Ann. Thorac. Surg. 2004, 78, 2123–2130. [Google Scholar] [CrossRef] [PubMed]
- Estep, J.D.; Starling, R.C.; Horstmanshof, D.A.; Milano, C.A.; Selzman, C.H.; Shah, K.B.; Loebe, M.; Moazami, N.; Long, J.W.; Stehlik, J.; et al. Risk Assessment and Comparative Effectiveness of Left Ventricular Assist Device and Medical Management in Ambulatory Heart Failure Patients Results from the ROADMAP Study. J. Am. Coll. Cardiol. 2015, 66, 1747–1761. [Google Scholar] [CrossRef] [PubMed]
- Mehra, M.R.; Uriel, N.; Naka, Y.; Cleveland, J.C.; Yuzefpolskaya, M.; Salerno, C.T.; Walsh, M.N.; Milano, C.A.; Patel, C.B.; Hutchins, S.W.; et al. A Fully Magnetically Levitated Left Ventricular Assist Device—Final Report. N. Engl. J. Med. 2019, 380, 1618–1627. [Google Scholar] [CrossRef] [PubMed]
- Schmitto, J.D.; Shaw, S.; Garbade, J.; Gustafsson, F.; Morshuis, M.; Zimpfer, D.; Lavee, J.; Pya, Y.; Berchtold-Herz, M.; Wang, A.; et al. Fully magnetically centrifugal left ventricular assist device and long-term outcomes: The ELEVATE registry. Eur. Heart J. 2023, 45, 613–625. [Google Scholar] [CrossRef] [PubMed]
- Finch, A.S.; Mohseni, M.M.; Simon, L.V.; Finch, J.G.; Gordon-Hackshaw, L.E.; Klassen, A.B.; Mullan, A.F.; Barbara, D.W.; Sandefur, B.J. Characteristics and Outcomes of Patients in the Emergency Department with Left Ventricular Assist Devices. West. J. Emerg. Med. Integr. Emerg. Care Popul. Health 2023, 24, 1018–1024. [Google Scholar] [CrossRef] [PubMed]
- Milicic, D.; Avraham, B.B.; Chioncel, O.; Barac, Y.D.; Goncalvesova, E.; Grupper, A.; Altenberger, J.; Frigeiro, M.; Ristic, A.; Jonge, N.D.; et al. Heart Failure Association of the European Society of Cardiology position paper on the management of left ventricular assist device-supported patients for the non-left ventricular assist device specialist healthcare provider: Part 2: At the emergency department. ESC Heart Fail. 2021, 8, 4409–4424. [Google Scholar] [CrossRef] [PubMed]
- Reza, N.; Edwards, J.J.; Katcoff, H.; Mondal, A.; Griffis, H.; Rossano, J.W.; Lin, K.Y.; Holzhauser, H.L.; Wald, J.W.; Owens, A.T.; et al. Sex Differences in Left Ventricular Assist Device-related Emergency Department Encounters in the United States. J. Card. Fail. 2022, 28, 1445–1455. [Google Scholar] [CrossRef] [PubMed]
- Pokrajac, N.; Cantwell, L.M.; Murray, J.M.; Dykes, J.C. Characteristics and Outcomes of Pediatric Patients with a Ventricular Assist Device Presenting to the Emergency Department. Pediatr. Emerg. Care 2022, 38, e924–e928. [Google Scholar] [CrossRef] [PubMed]
- Bowles, C.T.; Hards, R.; Wrightson, N.; Lincoln, P.; Kore, S.; Marley, L.; Dalzell, J.R.; Raj, B.; Baker, T.A.; Goodwin, D.; et al. Algorithms to guide ambulance clinicians in the management of emergencies in patients with implanted rotary left ventricular assist devices. Emerg. Med. J. 2017, 34, 842. [Google Scholar] [CrossRef]
- Hockstein, M.A. Continuous-flow left ventricular assist devices: Management in the emergency department. J. Am. Coll. Emerg. Physicians Open 2020, 1, 362–370. [Google Scholar] [CrossRef]
- Kilic, A.; Acker, M.A.; Atluri, P. Dealing with surgical left ventricular assist device complications. J. Thorac. Dis. 2015, 7, 2158–2164. [Google Scholar] [CrossRef] [PubMed]
- Chaudhry, A.; Berberian, J.; Ghandi, N. Emergency Department Approach to LVAD Patients. 2024. Available online: https://www.emra.org/emresident/article/lvad (accessed on 26 May 2025).
- Pilarczyk, K.; Panholzer, B.; Haneya, A.; Cremer, J.; Haake, N. Notfallmanagement bei Patienten mit linksventrikulärem Unterstützungssystem. Z. Herz-Thorax-GefäßChirurgie 2017, 31, 406–414. [Google Scholar] [CrossRef]
- Pilarczyk, K.; Boeken, U.; Beckmann, A.; Markewitz, A.; Schulze, P.C.; Pin, M.; Gräff, I.; Schmidt, S.; Runge, B.; Busch, H.J.; et al. Empfehlungen zum Notfallmanagement von Patienten mit permanenten Herzunterstützungssystemen. Kardiologe 2020, 14, 168–181. [Google Scholar] [CrossRef]
| Parameter | n = 48 |
|---|---|
| Gender [m] | 40 (83.3%) |
| Age [y] | 61.2 +/− 11.1 |
| Implant age [y] | 56.8 +/− 10.9 |
| Follow-up [y] | 4.3 +/− 2.7 |
| Indication | |
| Ischemic cardiomyopathy | 24 (50%) |
| Dilative cardiomyopathy | 20 (41.7%) |
| Myocarditis | 4 (8.3%) |
| Therapy objective | |
| Bridge to transplant | 33 (68.75%) |
| Destination therapy | 11 (22.92%) |
| Bridge to decision | 3 (6.25%) |
| Bridge to recovery | 1 (2.08%) |
| LVAD Relation | Minor | Major | LVAD Relation |
|---|---|---|---|
| No | 71 | 21 | 92 |
| Yes | 6 | 2 | 8 |
| severity | 77 | 23 | 100 |
| Cause | Counts | Patients |
|---|---|---|
| Arrhythmia | 24 | 11 |
| Infection | 15 | 10 |
| Gastrointestinal | 13 | 8 |
| Bleeding | 7 | 7 |
| Drive Line Infection | 7 | 6 |
| Neurologic | 6 | 6 |
| Metabolic | 5 | 3 |
| Musculosceletal | 5 | 4 |
| Trauma | 5 | 4 |
| Heart Failure | 4 | 4 |
| Oncologic | 2 | 2 |
| Urologic | 2 | 2 |
| Acute coronary syndrome | 1 | 1 |
| COVID-19 | 1 | 1 |
| Pain | 1 | 1 |
| Psychiatric | 1 | 1 |
| Unknown | 1 | 1 |
| Sum | 100 | 72 |
| ER Presentation Causes | Non-LVAD-Related | LVAD-Related | Sum |
|---|---|---|---|
| Minor | 71 | 6 | 77 |
| Arrhythmia | 21 | 21 | |
| Gastrointestinal | 10 | 1 | 11 |
| Infection | 9 | 9 | |
| Drive Line Infection | 5 | 5 | |
| Metabolic | 5 | 5 | |
| Musculosceletal | 5 | 5 | |
| Trauma | 5 | 5 | |
| Neurologic | 4 | 4 | |
| Bleeding | 3 | 3 | |
| Heart Failure | 2 | 2 | |
| Oncologic | 2 | 2 | |
| Urologic | 2 | 2 | |
| COVID-19 | 1 | 1 | |
| Pain | 1 | 1 | |
| Psychiatric | 1 | 1 | |
| Major | 21 | 2 | 23 |
| Infection | 6 | 6 | |
| Bleeding | 4 | 4 | |
| Arrhythmia | 3 | 3 | |
| Drive Line Infection | 2 | 2 | |
| Gastrointestinal | 2 | 2 | |
| Heart Failure | 2 | 2 | |
| Neurologic | 2 | 2 | |
| Acute coronary syndrome | 1 | 1 | |
| Unknown | 1 | 1 | |
| Sum | 92 | 8 | 100 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salewski, C.; Rustenbach, C.J.; Marinos, S.L.; Sandoval Boburg, R.; Schlensak, C.; Radwan, M. Left Ventricular Assist Device (LVAD)-Related Major Adverse Events Account for a Low Number of Emergency Room Admissions in HeartMate 3™ Patients—A 10-Year Retrospective Study. Biomedicines 2025, 13, 1702. https://doi.org/10.3390/biomedicines13071702
Salewski C, Rustenbach CJ, Marinos SL, Sandoval Boburg R, Schlensak C, Radwan M. Left Ventricular Assist Device (LVAD)-Related Major Adverse Events Account for a Low Number of Emergency Room Admissions in HeartMate 3™ Patients—A 10-Year Retrospective Study. Biomedicines. 2025; 13(7):1702. https://doi.org/10.3390/biomedicines13071702
Chicago/Turabian StyleSalewski, Christoph, Christian Jörg Rustenbach, Spiros Lukas Marinos, Rodrigo Sandoval Boburg, Christian Schlensak, and Medhat Radwan. 2025. "Left Ventricular Assist Device (LVAD)-Related Major Adverse Events Account for a Low Number of Emergency Room Admissions in HeartMate 3™ Patients—A 10-Year Retrospective Study" Biomedicines 13, no. 7: 1702. https://doi.org/10.3390/biomedicines13071702
APA StyleSalewski, C., Rustenbach, C. J., Marinos, S. L., Sandoval Boburg, R., Schlensak, C., & Radwan, M. (2025). Left Ventricular Assist Device (LVAD)-Related Major Adverse Events Account for a Low Number of Emergency Room Admissions in HeartMate 3™ Patients—A 10-Year Retrospective Study. Biomedicines, 13(7), 1702. https://doi.org/10.3390/biomedicines13071702









