A Meta-Analysis of Clinical and Echocardiographic Outcomes of Physiological Versus Conventional Pacing
Abstract
1. Introduction
2. Materials and Methods
- “yes” indicates the number of positive responses fully meeting a given criterion (2 points),
- “partials” indicates the number of responses partially meeting a given criterion (1 point),
- “N/A” indicates questions deemed not applicable to a given study and excluded from the denominator.
3. Results
3.1. Effects on Left Ventricular Ejection Fraction (LVEF)
3.2. Effects on Left Ventricular End-Diastolic Volume (LVEDV)
3.3. Effects on Left Ventricular End-Systolic Volume (LVESV)
3.4. Effects on QRS Duration
3.5. Effects on NYHA Functional Class
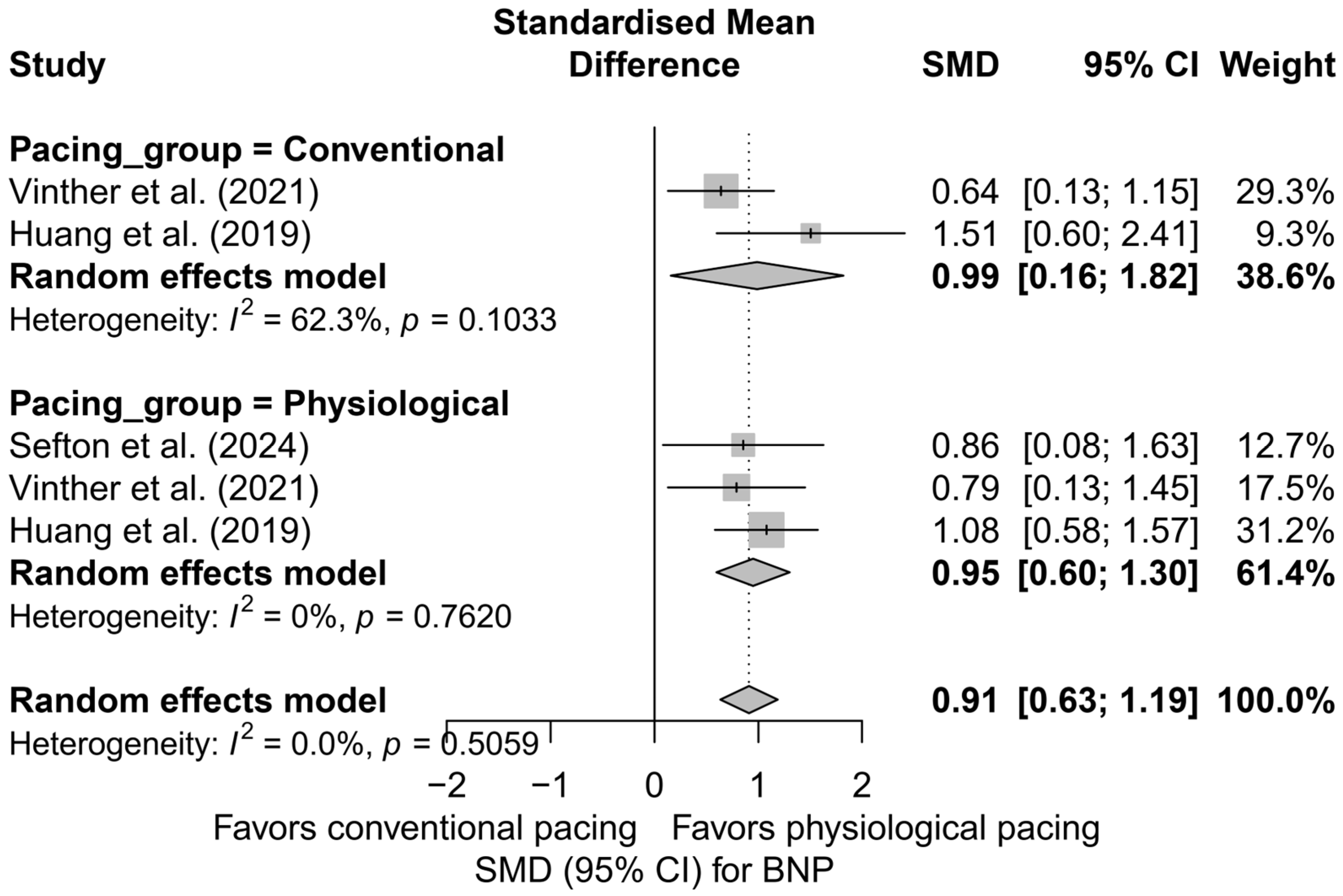
3.6. Effects on Brain Natriuretic Peptide (BNP) Levels
3.7. Effects on R-Wave Amplitude
3.8. Effects on Pacing Thresholds
3.9. Secondary and Summary Analyses
- Head-to-head comparisons limited to multi-arm studies,
- Synthetic comparisons of CSP versus conventional pacing for each clinical parameter,
- Meta-regressions assessing the impact of follow-up duration,
- Assessment of publication bias using Egger’s test and the trim-and-fill method.
3.9.1. Consolidated Head-to-Head Comparisons Across Parameters
3.9.2. Summary: Physiological vs. Classical Pacing Across Outcomes
3.9.3. Meta-Regressions Summary Table
3.9.4. Influence of Follow-Up Duration Across Parameters
3.9.5. Summary of Publication Bias Across All Outcomes
- Egger’s test: no funnel plot asymmetry detected for LVEF, BNP, QRS, or NYHA;
- Trim-and-fill: no imputed studies were added, supporting the robustness of the results.
4. Discussion
- In candidates for CRT in whom implantation of a coronary sinus lead is unsuccessful (Class IIa recommendation);
- With a backup ventricular lead in patients with rapidly conducted supraventricular arrhythmias undergoing a “pace-and-ablate” strategy (Class IIb recommendation);
- As an alternative to RVP in patients with atrioventricular block (AVB) and an LVEF > 40%, who are expected to require >20% ventricular pacing (Class IIb recommendation).
- In patients with an LVEF of 36–50% and an anticipated high percentage of RVP > 20–40% (Class I recommendation);
- In patients with pacing-induced cardiomyopathy (PICM), defined as a decline in LVEF or the onset of HF symptoms associated with a high percentage of RVP (Class I recommendation).
5. Limitations, Strengths, and Future Directions
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AF | atrial fibrillation |
| AVB | atrioventricular block |
| AVJ | atrioventricular junction |
| AVNA | atrioventricular node ablation |
| BNP | Brain Natriuretic Peptide |
| BVP | biventricular pacing |
| CI | Confidence Interval |
| CSP | conduction system pacing |
| CRT | cardiac resynchronization therapy |
| EF | ejection fraction |
| FSN | Fail-Safe N |
| HBP | His bundle pacing |
| HF | heart failure |
| HFH | heart failure hospitalization |
| HFrEF | heart failure with reduced ejection fraction |
| LBBAP | left bundle branch area pacing |
| LBBB | left bundle branch block |
| LVEDD | left ventricular end-diastolic diameter |
| LVEDV | left ventricular end-diastolic volume |
| LVEF | left ventricular ejection fraction |
| LVESV | left ventricular end-systolic volume |
| NMA | network meta-analysis |
| NT-proBNP | N-terminal pro–B-type natriuretic peptide |
| NYHA | New York Heart Association functional class |
| PICM | pacemaker-induced cardiomyopathy |
| RBBB | right bundle branch block |
| RCT | Randomized Controlled Trial |
| RVP | right ventricular pacing |
| SE | Standard Errors |
| SMD | standardized mean difference |
| SND | sinus node dysfunction |
References
- Aktaa, S.; Abdin, A.; Arbelo, E.; Burri, H.; Vernooy, K.; Blomström-Lundqvist, C.; Boriani, G.; Defaye, P.; Deharo, J.-C.; Drossart, I.; et al. European Society of Cardiology Quality Indicators for the Care and Outcomes of Cardiac Pacing: Developed by the Working Group for Cardiac Pacing Quality Indicators in Collaboration with the European Heart Rhythm Association of the European Society of Cardiology. EP Eur. 2022, 24, 165–172. [Google Scholar] [CrossRef]
- Oida, M.; Mizutani, T.; Hasumi, E.; Fujiu, K.; Goto, K.; Kani, K.; Oshima, T.; Matsubara, T.J.; Shimizu, Y.; Oguri, G.; et al. Prediction of Pacemaker-Induced Cardiomyopathy Using a Convolutional Neural Network Based on Clinical Findings Prior to Pacemaker Implantation. Sci. Rep. 2024, 14, 6916. [Google Scholar] [CrossRef] [PubMed]
- Yu, C.; Fang, F.; Luo, X.; Zhang, Q.; Azlan, H.; Razali, O. Long-term Follow-up Results of the Pacing to Avoid Cardiac Enlargement (PACE) Trial. Eur. J. Heart Fail. 2014, 16, 1016–1025. [Google Scholar] [CrossRef] [PubMed]
- Moss, A.J.; Hall, W.J.; Cannom, D.S.; Klein, H.; Brown, M.W.; Daubert, J.P.; Estes, N.A.M.; Foster, E.; Greenberg, H.; Higgins, S.L.; et al. Cardiac-Resynchronization Therapy for the Prevention of Heart-Failure Events. N. Engl. J. Med. 2009, 361, 1329–1338. [Google Scholar] [CrossRef]
- Tang, A.S.L.; Wells, G.A.; Talajic, M.; Arnold, M.O.; Sheldon, R.; Connolly, S.; Hohnloser, S.H.; Nichol, G.; Birnie, D.H.; Sapp, J.L.; et al. Cardiac-Resynchronization Therapy for Mild-to-Moderate Heart Failure. N. Engl. J. Med. 2010, 363, 2385–2395. [Google Scholar] [CrossRef]
- Curtis, A.B.; Worley, S.J.; Adamson, P.B.; Chung, E.S.; Niazi, I.; Sherfesee, L.; Shinn, T.; St. John Sutton, M. Biventricular Pacing for Atrioventricular Block and Systolic Dysfunction. N. Engl. J. Med. 2013, 368, 1585–1593. [Google Scholar] [CrossRef]
- Cleland, J.G.F.; Daubert, J.-C.; Erdmann, E.; Freemantle, N.; Gras, D.; Kappenberger, L.; Tavazzi, L. The Effect of Cardiac Resynchronization on Morbidity and Mortality in Heart Failure. N. Engl. J. Med. 2005, 352, 1539–1549. [Google Scholar] [CrossRef]
- Bristow, M.R.; Saxon, L.A.; Boehmer, J.; Krueger, S.; Kass, D.A.; De Marco, T.; Carson, P.; DiCarlo, L.; DeMets, D.; White, B.G.; et al. Cardiac-Resynchronization Therapy with or without an Implantable Defibrillator in Advanced Chronic Heart Failure. N. Engl. J. Med. 2004, 350, 2140–2150. [Google Scholar] [CrossRef]
- Naqvi, S.Y.; Jawaid, A.; Goldenberg, I.; Kutyifa, V. Non-Response to Cardiac Resynchronization Therapy. Curr. Heart Fail. Rep. 2018, 15, 315–321. [Google Scholar] [CrossRef]
- Chairs, T.F.; Daubert, J.-C.; Saxon, L.; Adamson, P.B.; Auricchio, A.; Berger, R.D.; Beshai, J.F.; Breithard, O.; Brignole, M.; Cleland, J.; et al. 2012 EHRA/HRS Expert Consensus Statement on Cardiac Resynchronization Therapy in Heart Failure: Implant and Follow-up Recommendations and Management: A Registered Branch of the European Society of Cardiology (ESC), and the Heart Rhythm Society; and in Collaboration with the Heart Failure Society of America (HFSA), the American Society of Echocardiography (ASE), the American Heart Association (AHA), the European Association of Echocardiography (EAE) of the ESC and the Heart Failure Association of the ESC (HFA). * Endorsed by the Governing Bodies of AHA, ASE, EAE, HFSA, HFA, EHRA, and HRS. Europace 2012, 14, 1236–1286. [Google Scholar] [CrossRef]
- Prinzen, F.W.; Vernooy, K.; Auricchio, A. Cardiac Resynchronization Therapy: State-of-the-Art of Current Applications, Guidelines, Ongoing Trials, and Areas of Controversy. Circulation 2013, 128, 2407–2418. [Google Scholar] [CrossRef] [PubMed]
- Scherlag, B.J.; Kosowsky, B.D.; Damato, A.N. A Technique for Ventricular Pacing from the His Bundle of the Intact Heart. J. Appl. Physiol. 1967, 22, 584–587. [Google Scholar] [CrossRef] [PubMed]
- Deshmukh, P.; Casavant, D.A.; Romanyshyn, M.; Anderson, K. Permanent, Direct His-Bundle Pacing: A Novel Approach to Cardiac Pacing in Patients With Normal His-Purkinje Activation. Circulation 2000, 101, 869–877. [Google Scholar] [CrossRef] [PubMed]
- Catanzariti, D.; Maines, M.; Cemin, C.; Broso, G.; Marotta, T.; Vergara, G. Permanent Direct His Bundle Pacing Does Not Induce Ventricular Dyssynchrony Unlike Conventional Right Ventricular Apical Pacing: An Intrapatient Acute Comparison Study. J. Interv. Card. Electrophysiol. 2006, 16, 81–92. [Google Scholar] [CrossRef]
- Abdelrahman, M.; Subzposh, F.A.; Beer, D.; Durr, B.; Naperkowski, A.; Sun, H.; Oren, J.W.; Dandamudi, G.; Vijayaraman, P. Clinical Outcomes of His Bundle Pacing Compared to Right Ventricular Pacing. J. Am. Coll. Cardiol. 2018, 71, 2319–2330. [Google Scholar] [CrossRef]
- Huang, W.; Su, L.; Wu, S.; Xu, L.; Xiao, F.; Zhou, X.; Ellenbogen, K.A. A Novel Pacing Strategy With Low and Stable Output: Pacing the Left Bundle Branch Immediately Beyond the Conduction Block. Can. J. Cardiol. 2017, 33, 1736.e1–1736.e3. [Google Scholar] [CrossRef]
- Zhuo, W.; Zhong, X.; Liu, H.; Yu, J.; Chen, Q.; Hu, J.; Xiong, Q.; Hong, K. Pacing Characteristics of His Bundle Pacing vs. Left Bundle Branch Pacing: A Systematic Review and Meta-Analysis. Front. Cardiovasc. Med. 2022, 9, 849143. [Google Scholar] [CrossRef]
- Prinzen, F.W.; Hunter, W.C.; Wyman, B.T.; McVeigh, E.R. Mapping of Regional Myocardial Strain and Work during Ventricular Pacing: Experimental Study Using Magnetic Resonance Imaging Tagging. J. Am. Coll. Cardiol. 1999, 33, 1735–1742. [Google Scholar] [CrossRef]
- Mariani, M.V.; Piro, A.; Forleo, G.B.; Della Rocca, D.G.; Natale, A.; Miraldi, F.; Vizza, C.D.; Lavalle, C. Clinical, Procedural and Lead Outcomes Associated with Different Pacing Techniques: A Network Meta-Analysis. Int. J. Cardiol. 2023, 377, 52–59. [Google Scholar] [CrossRef]
- Herweg, B.; Sharma, P.S.; Cano, Ó.; Ponnusamy, S.S.; Zanon, F.; Jastrzebski, M.; Zou, J.; Chelu, M.G.; Vernooy, K.; Whinnett, Z.I.; et al. Arrhythmic Risk in Biventricular Pacing Compared With Left Bundle Branch Area Pacing: Results From the I-CLAS Study. Circulation 2024, 149, 379–390. [Google Scholar] [CrossRef]
- Vijayaraman, P.; Naperkowski, A.; Subzposh, F.A.; Abdelrahman, M.; Sharma, P.S.; Oren, J.W.; Dandamudi, G.; Ellenbogen, K.A. Permanent His-Bundle Pacing: Long-Term Lead Performance and Clinical Outcomes. Heart Rhythm 2018, 15, 696–702. [Google Scholar] [CrossRef] [PubMed]
- Mirmaksudov, M.; Ross, S.; Kongsgård, E.; Edvardsen, T. Enhancing Cardiac Pacing Strategies: A Review of Conduction System Pacing Compared with Right and Biventricular Pacing and Their Influence on Myocardial Function. Eur. Heart J.-Cardiovasc. Imaging 2024, 25, 879–887. [Google Scholar] [CrossRef] [PubMed]
- Hua, J.; Wang, C.; Kong, Q.; Zhang, Y.; Wang, Q.; Xiong, Z.; Hu, J.; Li, J.; Chen, Q.; Hong, K. Comparative Effects of Left Bundle Branch Area Pacing, His Bundle Pacing, Biventricular Pacing in Patients Requiring Cardiac Resynchronization Therapy: A Network Meta-analysis. Clin. Cardiol. 2022, 45, 214–223. [Google Scholar] [CrossRef] [PubMed]
- Domenichini, G.; Le Bloa, M.; Teres Castillo, C.; Graf, D.; Carroz, P.; Ascione, C.; Porretta, A.P.; Pascale, P.; Pruvot, E. Conduction System Pacing versus Conventional Biventricular Pacing for Cardiac Resynchronization Therapy: Where Are We Heading? J. Clin. Med. 2023, 12, 6288. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Haddaway, N.R.; Page, M.J.; Pritchard, C.C.; McGuinness, L.A. PRISMA2020: An R Package and Shiny App for Producing PRISMA 2020-compliant Flow Diagrams, with Interactivity for Optimised Digital Transparency and Open Synthesis. Campbell Syst. Rev. 2022, 18, e1230. [Google Scholar] [CrossRef]
- Kmet, L.M.; Cook, L.S.; Lee, R.C. Standard Quality Assessment Criteria for Evaluating Primary Research Papers from a Variety of Fields 2004. Available online: https://era.library.ualberta.ca/items/48b9b989-c221-4df6-9e35-af782082280e/view/a1cffdde-243e-41c3-be98-885f6d4dcb29/standard_quality_assessment_criteria_for_evaluating_primary_research_papers_from_a_variety_of_fields.pdf (accessed on 29 April 2025).
- Higgins, J.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.; Velch, V. Cochrane Handbook for Systematic Reviews of Interventions Version 6.5 (Updated August 2024). Available online: https://training.cochrane.org/handbook (accessed on 29 April 2025).
- Akl, E.; Mustafa, R.; Wiercioch, N.; Schünemann, H.; Brożek, J.; Guyatt, G. GRADE Handbook; GRADEpro: Gurugram, India, 2013; Available online: https://gdt.gradepro.org/app/handbook/handbook.html (accessed on 29 April 2025).
- Chaumont, C.; Auquier, N.; Milhem, A.; Mirolo, A.; Al Arnaout, A.; Popescu, E.; Viart, G.; Godin, B.; Gillibert, A.; Savouré, A.; et al. Can Permanent His Bundle Pacing Be Safely Started by Operators New to This Technique? Data from a Multicenter Registry. Cardiovasc. Electrophysiol. 2021, 32, 417–427. [Google Scholar] [CrossRef]
- Chaumont, C.; Azincot, M.; Savouré, A.; Auquier, N.; Hamoud, R.A.; Popescu, E.; Viart, G.; Mirolo, A.; Eltchaninoff, H.; Anselme, F. His Bundle Pacing versus Left Bundle Branch Area Pacing in Patients Undergoing Atrioventricular Node Ablation: A Prospective and Comparative Study. Arch. Cardiovasc. Dis. 2024, 117, 505–513. [Google Scholar] [CrossRef]
- Chen, X.; Ye, Y.; Wang, Z.; Jin, Q.; Qiu, Z.; Wang, J.; Qin, S.; Bai, J.; Wang, W.; Liang, Y.; et al. Cardiac Resynchronization Therapy via Left Bundle Branch Pacing vs. Optimized Biventricular Pacing with Adaptive Algorithm in Heart Failure with Left Bundle Branch Block: A Prospective, Multi-Centre, Observational Study. EP Eur. 2022, 24, 807–816. [Google Scholar] [CrossRef]
- Chen, Z.; Xu, Y.; Jiang, L.; Zhang, R.; Zhao, H.; Liu, R.; Zhang, L.; Li, Y.; Liu, X. Left Bundle Branch Area Pacing versus Right Ventricular Pacing in Patients with Atrioventricular Block: An Observational Cohort Study. Cardiovasc. Ther. 2023, 2023, 6659048. [Google Scholar] [CrossRef]
- Chen, X.; Jin, Q.; Qiu, Z.; Qian, C.; Liang, Y.; Wang, J.; Qin, S.; Bai, J.; Wang, W.; Chen, H.; et al. Outcomes of Upgrading to LBBP in CRT Nonresponders. JACC Clin. Electrophysiol. 2024, 10, 108–120. [Google Scholar] [CrossRef] [PubMed]
- Ezzeddine, F.M.; Pistiolis, S.M.; Pujol-Lopez, M.; Lavelle, M.; Wan, E.Y.; Patton, K.K.; Robinson, M.; Lador, A.; Tamirisa, K.; Karim, S.; et al. Outcomes of Conduction System Pacing for Cardiac Resynchronization Therapy in Patients with Heart Failure: A Multicenter Experience. Heart Rhythm 2023, 20, 863–871. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Li, L.; Xiao, G.; Ye, T.; Huang, X.; Meng, F.; Li, Q.; Chen, S.; Cai, B. Remarkable Response to Cardiac Resynchronization Therapy via Left Bundle Branch Pacing in Patients with True Left Bundle Branch Block. Clin. Cardiol. 2020, 43, 1460–1468. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.; Su, L.; Wu, S.; Xu, L.; Xiao, F.; Zhou, X.; Mao, G.; Vijayaraman, P.; Ellenbogen, K.A. Long-Term Outcomes of His Bundle Pacing in Patients with Heart Failure with Left Bundle Branch Block. Heart 2019, 105, 137–143. [Google Scholar] [CrossRef]
- Huang, W.; Wu, S.; Vijayaraman, P.; Su, L.; Chen, X.; Cai, B.; Zou, J.; Lan, R.; Fu, G.; Mao, G.; et al. Cardiac Resynchronization Therapy in Patients With Nonischemic Cardiomyopathy Using Left Bundle Branch Pacing. JACC Clin. Electrophysiol. 2020, 6, 849–858. [Google Scholar] [CrossRef]
- Ponnusamy, S.S.; Bopanna, D.; Syed, T.; Muthu, G.; Kumar, S. Feasibility, Safety and Outcomes of Left Bundle Branch Pacing in Octogenarians. Indian Heart J. 2021, 73, 117–120. [Google Scholar] [CrossRef]
- Sharma, P.S.; Patel, N.R.; Ravi, V.; Zalavadia, D.V.; Dommaraju, S.; Garg, V.; Larsen, T.R.; Naperkowski, A.M.; Wasserlauf, J.; Krishnan, K.; et al. Clinical Outcomes of Left Bundle Branch Area Pacing Compared to Right Ventricular Pacing: Results from the Geisinger-Rush Conduction System Pacing Registry. Heart Rhythm 2022, 19, 3–11. [Google Scholar] [CrossRef]
- Sefton, C.; Tanaka-Esposito, C.; Dresing, T.; Lee, J.; Chung, R. Outcomes of combined left bundle branch area pacing with atrioventricular nodal ablation in patients with atrial fibrillation and pulmonary disease. Pacing Clin. Electrophis 2024, 47, 946–952. [Google Scholar] [CrossRef]
- Sharma, P.S.; Dandamudi, G.; Naperkowski, A.; Oren, J.W.; Storm, R.H.; Ellenbogen, K.A.; Vijayaraman, P. Permanent His-Bundle Pacing Is Feasible, Safe, and Superior to Right Ventricular Pacing in Routine Clinical Practice. Heart Rhythm 2015, 12, 305–312. [Google Scholar] [CrossRef]
- Sharma, P.S.; Dandamudi, G.; Herweg, B.; Wilson, D.; Singh, R.; Naperkowski, A.; Koneru, J.N.; Ellenbogen, K.A.; Vijayaraman, P. Permanent His-Bundle Pacing as an Alternative to Biventricular Pacing for Cardiac Resynchronization Therapy: A Multicenter Experience. Heart Rhythm 2018, 15, 413–420. [Google Scholar] [CrossRef]
- Sharma, P.S.; Naperkowski, A.; Bauch, T.D.; Chan, J.Y.S.; Arnold, A.D.; Whinnett, Z.I.; Ellenbogen, K.A.; Vijayaraman, P. Permanent His Bundle Pacing for Cardiac Resynchronization Therapy in Patients With Heart Failure and Right Bundle Branch Block. Circ. Arrhythmia Electrophysiol. 2018, 11, e006613. [Google Scholar] [CrossRef] [PubMed]
- Tang, J.; Kong, N.W.; Beaser, A.; Aziz, Z.; Yeshwant, S.; Ozcan, C.; Tung, R.; Upadhyay, G.A. Clinical Outcomes of Conduction System Pacing Compared to Biventricular Pacing in Patients with Mid-Range Ejection Fraction. J. Interv. Card. Electrophysiol. 2025, 68, 111–116. [Google Scholar] [CrossRef] [PubMed]
- Upadhyay, G.A.; Vijayaraman, P.; Nayak, H.M.; Verma, N.; Dandamudi, G.; Sharma, P.S.; Saleem, M.; Mandrola, J.; Genovese, D.; Oren, J.W.; et al. On-Treatment Comparison between Corrective His Bundle Pacing and Biventricular Pacing for Cardiac Resynchronization: A Secondary Analysis of the His-SYNC Pilot Trial. Heart Rhythm 2019, 16, 1797–1807. [Google Scholar] [CrossRef] [PubMed]
- Vazquez, P.M.; Mohamed, U.; Zanon, F.; Lustgarten, D.L.; Atwater, B.; Whinnett, Z.I.; Curila, K.; Dinerman, J.; Molina-Lerma, M.; Wiley, J.; et al. Result of the Physiologic Pacing Registry, an International Multicenter Prospective Observational Study of Conduction System Pacing. Heart Rhythm 2023, 20, 1617–1625. [Google Scholar] [CrossRef]
- Vijayaraman, P.; Ponnusamy, S.; Cano, Ó.; Sharma, P.S.; Naperkowski, A.; Subsposh, F.A.; Moskal, P.; Bednarek, A.; Dal Forno, A.R.; Young, W.; et al. Left Bundle Branch Area Pacing for Cardiac Resynchronization Therapy. JACC Clin. Electrophysiol. 2021, 7, 135–147. [Google Scholar] [CrossRef]
- Vijayaraman, P.; Sharma, P.S.; Cano, Ó.; Ponnusamy, S.S.; Herweg, B.; Zanon, F.; Jastrzebski, M.; Zou, J.; Chelu, M.G.; Vernooy, K.; et al. Comparison of Left Bundle Branch Area Pacing and Biventricular Pacing in Candidates for Resynchronization Therapy. J. Am. Coll. Cardiol. 2023, 82, 228–241. [Google Scholar] [CrossRef]
- Vinther, M.; Risum, N.; Svendsen, J.H.; Møgelvang, R.; Philbert, B.T. A Randomized Trial of His Pacing Versus Biventricular Pacing in Symptomatic HF Patients With Left Bundle Branch Block (His-Alternative). JACC Clin. Electrophysiol. 2021, 7, 1422–1432. [Google Scholar] [CrossRef]
- Wang, Y.; Zhu, H.; Hou, X.; Wang, Z.; Zou, F.; Qian, Z.; Wei, Y.; Wang, X.; Zhang, L.; Li, X.; et al. Randomized Trial of Left Bundle Branch vs Biventricular Pacing for Cardiac Resynchronization Therapy. J. Am. Coll. Cardiol. 2022, 80, 1205–1216. [Google Scholar] [CrossRef]
- Whinnett, Z.I.; Shun-Shin, M.J.; Tanner, M.; Foley, P.; Chandrasekaran, B.; Moore, P.; Adhya, S.; Qureshi, N.; Muthumala, A.; Lane, R.; et al. Effects of Haemodynamically Atrio-ventricular Optimized His Bundle Pacing on Heart Failure Symptoms and Exercise Capacity: The His Optimized Pacing Evaluated for Heart Failure (HOPE-HF) Randomized, Double-blind, Cross-over Trial. Eur. J. Heart Fail. 2023, 25, 274–283. [Google Scholar] [CrossRef]
- Wu, S.; Su, L.; Vijayaraman, P.; Zheng, R.; Cai, M.; Xu, L.; Shi, R.; Huang, Z.; Whinnett, Z.I.; Huang, W. Left Bundle Branch Pacing for Cardiac Resynchronization Therapy: Nonrandomized On-Treatment Comparison With His Bundle Pacing and Biventricular Pacing. Can. J. Cardiol. 2021, 37, 319–328. [Google Scholar] [CrossRef]
- Zanon, F.; Abdelrahman, M.; Marcantoni, L.; Naperkowski, A.; Subzposh, F.A.; Pastore, G.; Baracca, E.; Boaretto, G.; Raffagnato, P.; Tiribello, A.; et al. Long Term Performance and Safety of His Bundle Pacing: A Multicenter Experience. Cardiovasc. Electrophysiol. 2019, 30, 1594–1601. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.; Qin, C.; Du, A.; Wang, Q.; He, C.; Zou, F.; Li, X.; Tao, J.; Wang, C.; Liu, Z.; et al. Comparisons of Long-Term Clinical Outcomes with Left Bundle Branch Pacing, Left Ventricular Septal Pacing, and Biventricular Pacing for Cardiac Resynchronization Therapy. Heart Rhythm 2024, 21, 1342–1353. [Google Scholar] [CrossRef] [PubMed]
- Vijayaraman, P.; Zalavadia, D.; Haseeb, A.; Dye, C.; Madan, N.; Skeete, J.R.; Vipparthy, S.C.; Young, W.; Ravi, V.; Rajakumar, C.; et al. Clinical Outcomes of Conduction System Pacing Compared to Biventricular Pacing in Patients Requiring Cardiac Resynchronization Therapy. Heart Rhythm 2022, 19, 1263–1271. [Google Scholar] [CrossRef] [PubMed]
- Diaz, J.C.; Tedrow, U.B.; Duque, M.; Aristizabal, J.; Braunstein, E.D.; Marin, J.; Niño, C.; Bastidas, O.; Lopez Cabanillas, N.; Koplan, B.A.; et al. Left Bundle Branch Pacing vs Left Ventricular Septal Pacing vs Biventricular Pacing for Cardiac Resynchronization Therapy. JACC Clin. Electrophysiol. 2024, 10, 295–305. [Google Scholar] [CrossRef]
- Ponnusamy, S.S.; Syed, T.; Vijayaraman, P. Pacing Induced Cardiomyopathy: Recognition and Management. Heart 2023, 109, 1407–1415. [Google Scholar] [CrossRef]
- Somma, V.; Ha, F.J.; Palmer, S.; Mohamed, U.; Agarwal, S. Pacing-Induced Cardiomyopathy: A Systematic Review and Meta-Analysis of Definition, Prevalence, Risk Factors, and Management. Heart Rhythm 2023, 20, 282–290. [Google Scholar] [CrossRef]
- Glikson, M.; Nielsen, J.C.; Kronborg, M.B.; Michowitz, Y.; Auricchio, A.; Barbash, I.M.; Barrabés, J.A.; Boriani, G.; Braunschweig, F.; Brignole, M.; et al. 2021 ESC Guidelines on Cardiac Pacing and Cardiac Resynchronization Therapy. Eur. Heart J. 2021, 42, 3427–3520. [Google Scholar] [CrossRef]
- Chung, M.K.; Patton, K.K.; Lau, C.-P.; Dal Forno, A.R.J.; Al-Khatib, S.M.; Arora, V.; Birgersdotter-Green, U.M.; Cha, Y.-M.; Chung, E.H.; Cronin, E.M.; et al. 2023 HRS/APHRS/LAHRS Guideline on Cardiac Physiologic Pacing for the Avoidance and Mitigation of Heart Failure. Heart Rhythm 2023, 20, e17–e91. [Google Scholar] [CrossRef]
- Peng, X.; Chen, Y.; Wang, X.; Hu, A.; Li, X. Safety and Efficacy of His-Bundle Pacing/Left Bundle Branch Area Pacing versus Right Ventricular Pacing: A Systematic Review and Meta-Analysis. J. Interv. Card. Electrophysiol. 2021, 62, 445–459. [Google Scholar] [CrossRef]
- Liu, J.; Sun, F.; Wang, Z.; Sun, J.; Jiang, X.; Zhao, W.; Zhang, Z.; Liu, L.; Zhang, S. Left Bundle Branch Area Pacing vs. Biventricular Pacing for Cardiac Resynchronization Therapy: A Meta-Analysis. Front. Cardiovasc. Med. 2021, 8, 669301. [Google Scholar] [CrossRef]



















| Population (P) | Patients with HF and various indications for pacemaker implantation. |
| Intervention (I) | Application of HBP or LBBAP. |
| Comparison (C) | Application of RVP or BVP. |
| Outcome (O) | LVEF, LVEDV, LVESV, QRS duration, NYHA, NT-proBNP, R-wave, pacing threshold. |
| Variable | SMD < 0 Indicates | SMD > 0 Indicates | Clinical Benefit in the Analysis |
|---|---|---|---|
| LVEF | increase | decrease | SMD < 0 |
| LVEDV, LVESV | increase | decrease | SMD > 0 |
| NYHA | worsening | improvement | SMD > 0 |
| NT-proBNP | increase | decrease | SMD > 0 |
| QRS duration | extending | shortening | SMD > 0 |
| Pacing threshold | decrease | increase | SMD < 0 |
| R-wave amplitude | decrease | increase | SMD > 0 |
| Ref. | Authors (Year) | Total Patients | Summary QualSyst Score | Patient Population Characteristics | Intervention | Follow-Up [Months] |
|---|---|---|---|---|---|---|
| [15] | Abdelrahman et al. (2018) | 765 | 0.79 | Bradycardia | HBP, RVP | 24.00 |
| [30] | Chaumont et al. (2021) | 170 | 0.71 | General indications for pacing | HBP | 11.00 |
| [31] | Chaumont et al. (2024) | 164 | 0.79 | Arrhythmia with ANVA | HBP, LBBAP | 12.00 |
| [32] | Chen et al. (2022) | 100 | 0.75 | HF with LBBB, LVEF ≤ 35% | BVP, LBBAP | 12.00 |
| [33] | Chen et al. (2023) | 1170 | 0.79 | AVB | LBBAP | N/R |
| [34] | Chen et al. (2024) | 145 | 0.75 | CRT nonresponders (Sinus rhythm or AF) | LBBAP, BVP | 24.00 |
| [35] | Ezzeddine et al. (2023) | 238 | 0.75 | CRT nonresponders, HFrEF | BVP, CSP (HBP, LBBAP) | 9.00 |
| [36] | Guo et al. (2020) | 42 | 0.75 | HF with LBBB, LVEF ≤ 35%, NYHA II-IV | LBBAP, BVP | 6.00 |
| [37] | Huang et al. (2019) | 74 | 0.71 | HF with LBBB | HBP, BVP | 12.00 |
| [38] | Huang et al. (2020) | 63 | 0.75 | HF with LBBB, LVEF < 50%, nonischemic cardiomyopathy | LBBAP | 18.00 |
| [39] | Ponnusamy et al. (2021) | 11 | 0.68 | Octogenarians (≥80 years), with AVB, LBBB with low EF, SND. | LBBAP | 7.70 |
| [40] | Sharma et al. (2022) | 50 | 0.71 | Bradycardia | RVP | 22.10 |
| 703 | 0.79 | LBBAP | 16.20 | |||
| [41] | Sefton et al. (2024) | 27 | 0.71 | AF and advanced pulmonary disease, AVNA | LBBAP | 17.30 |
| [42] | Sharma et al. (2015) | 192 | 0.75 | Bradycardia | HBP, RVP | 25.50 |
| [43] | Sharma, Dandamudi, et al. (2018) | 106 | 0.75 | HF and AVB, BBB and high rates of ventricular pacing | HBP | 14.40 |
| [44] | Sharma, Naperkowski, et al. (2018) | 39 | 0.71 | HF with RBBB, LVEF ≤ 50%, NYHA II-IV | HBP | 15.00 |
| [45] | Tang et al. (2025) | 36 | 0.71 | HF, LVEF 35–50% | BVP, CSP (HBP, LBBAP) | 47.00 |
| [46] | Upadhyay et al. (2019) | 41 | 0.89 | HF with LBBB/RBBB, NYHA II–IV | HBP, BVP | 6.20 |
| [47] | Vazquez et al. (2023) | 849 | 0.75 | AVB, HF with wide QRS, HF with frequent dependence on ventricular pacing, AVNA, Ischemic/nonischemic cardiomyopathy | HBP, LBBAP | 5.00 |
| [21] | Vijayaraman et al. (2018) | 192 | 0.75 | Bradycardia | HBP, RVP | 60.00 |
| [48] | Vijayaraman et al. (2021) | 325 | 0.79 | HF with LBBB, LVEF ≤ 50%, NYHA II-IV | LBBAP | 6.00 |
| [49] | Vijayaraman et al. (2023) | 1778 | 0.79 | CRT nonresponders, HFrEF, LVEF ≤ 35% | BVP, LBBAP | 33.00 |
| [50] | Vinther et al. (2021) | 50 | 0.89 | HF with LBBB, LVEF ≤ 35%, NYHA II-IV | HBP, BVP | 6.00 |
| [51] | Wang et al. (2022) | 40 | 0.79 | HF with LBBB, LVEF ≤ 40%, nonischemic cardiomyopathy | BVP, LBBAP | 6.00 |
| [52] | Whinnett et al. (2023) | 167 | 1.00 | HF, LVEF ≤ 40%, AVB 1.degree, QRS ≤ 140 ms or RBBB | HBP | 6.00 |
| [53] | Wu et al. (2021) | 137 | 0.75 | HF with LBBB, LVEF ≤ 40% | HBP, LBBAP, BVP | 12.00 |
| [54] | Zanon et al. (2019) | 844 | 0.75 | AVB, SND, bradycardia with AF, HF | HBP | 3.90 |
| [55] | Zhu et al. (2024) | 259 | 0.79 | HF, AVB, LBBB, RBBB, AF, LVEF < 50% | BVP, LBBAP | 29.00 |
| Endpoint | Comparisons/Patients | Pooled Effect (SMD [95% CI]) | Certainty of Evidence (GRADE) | Downgrading Factors |
|---|---|---|---|---|
| LVEF (benefit SMD < 0) | 34/6102 | −1.38 [−1.69; −1.06] | ⬤⬤◯◯ low | observational studies, I2 > 90% |
| NYHA (benefit SMD > 0) | 19/3418 | 1.94 [1.59; 2.29] | ⬤⬤◯◯ low | observational studies, I2 > 90% |
| NT-proBNP (benefit SMD > 0) | 5/811 | 0.91 [0.63; 1.19] | ⬤⬤◯◯ low | a limited number of studies, observational studies |
| LVESV (benefit SMD > 0) | 13/2047 | 1.14 [0.81; 1.47] | ⬤⬤◯◯ low | heterogeneity, lack of Randomized Controlled Trials |
| Pacing threshold (benefit SMD < 0) | 17/2682 | −0.14 [−0.36; 0.08] | ⬤⬤◯◯ low | non-significant effect, I2 = 81% |
| Parameter | SMD (95%CI) | p-Value | Interpretation |
|---|---|---|---|
| LVEF | −1.49 [−1.85; −1.13] | <0.0001 | Significant improvement following physiological pacing |
| QRS duration | 0.18 [−0.42; 0.79] | 0.55 | No difference observed |
| NYHA | 1.94 [1.43; 2.45] | <0.0001 | Significant improvement |
| NT-proBNP | 0.92 [0.62; 1.22] | <0.0001 | Significant improvement. |
| LVEDV | −0.23 [−0.44; −0.03] | 0.025 | Moderate improvement |
| LVESV | −0.35 [−0.60; −0.09] | 0.0078 | Improvement |
| Pacing threshold | −0.23 [−0.44; −0.03] | 0.025 | Potential benefit of physiological pacing |
| R-wave amplitude | −0.09 [−0.21; 0.03] | 0.13 | No significant difference |
| Parameter | Overall Effect (SMD [CI]) | Overall p-Value | CSP vs. Conventional (p) | Meta-Regression (p) | Trend vs. Follow-Up |
|---|---|---|---|---|---|
| LVEF | −1.49 [−1.85, −1.13] | <0.0001 | 0.987 | <0.01 | Yes |
| QRS duration | 0.18 [−0.42, 0.79] | 0.55 | 0.333 | 0.134 | No |
| NYHA | 1.94 [1.43, 2.45] | <0.0001 | 0.286 | 0.134 | No |
| NT-proBNP | 0.92 [0.62, 1.22] | <0.0001 | 0.891 | 0.445 | No |
| LVEDV | −0.23 [−0.44, −0.03] | 0.025 | 0.134 | 0.134 | No |
| LVESV | −0.35 [−0.60, −0.09] | 0.0078 | 0.134 | 0.134 | No |
| R-wave amplitude | −0.09 [−0.21, 0.03] | 0.13 | 0.445 | 0.445 | No |
| Pacing threshold | −0.23 [−0.44, −0.03] | 0.025 | 0.134 | 0.134 | No |
| Parameter | Number of Studies (k) | β (Regression Coefficient) | 95%CI β | p for Follow-Up | Effect of Follow-Up |
|---|---|---|---|---|---|
| LVEF | 24 | +0.026 | [0.011, 0.041] | <0.01 | Significant |
| QRS duration | 24 | −0.007 | [−0.022, 0.008] | 0.13 | Not significant |
| NYHA | 15 | −0.013 | [−0.038, 0.011] | 0.13 | Not significant |
| NT-proBNP | 4 | −0.004 | [−0.062, 0.054] | 0.89 | Not significant |
| LVEDV | 8 | +0.007 | [−0.006, 0.021] | 0.45 | Not significant |
| LVESV | 11 | +0.013 | [−0.004, 0.031] | 0.13 | Not significant |
| R-wave amplitude | 9 | −0.005 | [−0.018, 0.008] | 0.45 | Not significant |
| Pacing threshold | 11 | +0.012 | [−0.009, 0.033] | 0.13 | Not significant |
| Parameter | k | SMD (95% CI) | Rosenthal Fail-Safe N | p After FSN Adjustment | Interpretation |
|---|---|---|---|---|---|
| LVEF | 34 | −1.38 (−1.69; −1.06) | 512 | 0.0501 | highly robust effect |
| NYHA | 19 | 1.94 (1.59; 2.29) | 410 | 0.0503 | robust |
| LVESV | 13 | 1.14 (0.81; 1.47) | 95 | 0.0506 | moderate robustness |
| LVEDV | 9 | 0.66 (0.25; 1.08) | 11 | 0.0574 | sensitive to publication bias |
| Parameter/Aspect | Limitation | Comment |
|---|---|---|
| general | heterogeneity of the results (high I2 values) | Expected due to population, methodological, and temporal differences; random-effects models, subgroup analyses, and meta-regressions with respect to follow-up were applied. |
| predominance of observational studies | Most of the data originate from non-randomized studies; potential selection bias was minimized through head-to-head analyses and a rigorous assessment of methodological quality (QualSyst). | |
| lack of complete individual patient data | A standard limitation of meta-analyses; the best available aggregated data were used; the results should be confirmed in future individual patient data analyses. | |
| variable follow-up duration (3.9–60 months) | Meta-regression with respect to follow-up duration was applied to assess the impact of time on the outcomes. | |
| potential for publication bias | Assessment performed using Egger’s test and the trim-and-fill method; results were adjusted where necessary. | |
| lack of a standardized definition of CSP | Differences were accounted for in subgroup analyses; results were interpreted with caution. | |
| diversity of implantation protocols (e.g., selective vs. non-selective) | Results were interpreted with caution; detailed protocols should be standardized in future studies. | |
| LVEF | lack of full standardization of assessment methods | Use of SMD; echocardiography was the predominant assessment method, adjusted using the REML model. |
| lack of analysis of mortality and rehospitalization | Consistent with the PICO framework of the study (focused on LVEF); clinical outcomes should be addressed in separate investigations. | |
| potential overlap of patient populations | A mixed-effects analysis with clustering by publication number was applied. | |
| LVEDV and LVESV | small number of studies in certain groups | Results were considered exploratory, with recommendations for further research. |
| lack of raw data for delta analysis | Use of aggregated data, with SMD partially minimizing this limitation. | |
| use of SMD instead of mean differences | Justified by heterogeneity in measurement units and populations; the analysis is standardized. | |
| QRS | possible multiple arms within studies | Separate head-to-head analysis for multi-arm studies; clearly discussed in the text. |
| NYHA | lack of randomized head-to-head studies comparing HBP and LBBAP | The need for future RCTs was emphasized; results were interpreted with caution. |
| NT-proBNP | small number of studies (k = 5) | Results were interpreted with caution; further studies with larger sample sizes are recommended. |
| lack of long-term data | Meta-regression did not demonstrate an impact of follow-up duration; however, the results require confirmation in longer-term observations. | |
| R-Wave Amplitude | heterogeneity of measurement methods | Clear indication of the lack of standardization in the original studies; results were interpreted as preliminary. |
| lack of data on device settings (gain, sensing) | Potential source of technical bias; recommendation for future standardization in clinical studies. | |
| Pacing Threshold | non-random selection of studies | Only complete analyses (Means, Standard Deviation, N) were used; the risk of publication bias is low. |
| lack of data on secondary outcomes | The need for future studies focusing on the technical parameters of the leads was indicated. | |
| small number of comparisons between HBP and LBBAP | Results were presented with caution, emphasizing the need for further studies. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Paluszkiewicz, P.; Martuszewski, A.; Smereka, J.; Gajek, J. A Meta-Analysis of Clinical and Echocardiographic Outcomes of Physiological Versus Conventional Pacing. Biomedicines 2025, 13, 1359. https://doi.org/10.3390/biomedicines13061359
Paluszkiewicz P, Martuszewski A, Smereka J, Gajek J. A Meta-Analysis of Clinical and Echocardiographic Outcomes of Physiological Versus Conventional Pacing. Biomedicines. 2025; 13(6):1359. https://doi.org/10.3390/biomedicines13061359
Chicago/Turabian StylePaluszkiewicz, Patrycja, Adrian Martuszewski, Jacek Smereka, and Jacek Gajek. 2025. "A Meta-Analysis of Clinical and Echocardiographic Outcomes of Physiological Versus Conventional Pacing" Biomedicines 13, no. 6: 1359. https://doi.org/10.3390/biomedicines13061359
APA StylePaluszkiewicz, P., Martuszewski, A., Smereka, J., & Gajek, J. (2025). A Meta-Analysis of Clinical and Echocardiographic Outcomes of Physiological Versus Conventional Pacing. Biomedicines, 13(6), 1359. https://doi.org/10.3390/biomedicines13061359








