Effect of Levosimendan Use on All-Cause Mortality in Out-of-Hospital Cardiac Arrest Survivors After Extracorporeal Cardiopulmonary Resuscitation
Abstract
1. Introduction
2. Materials and Methods
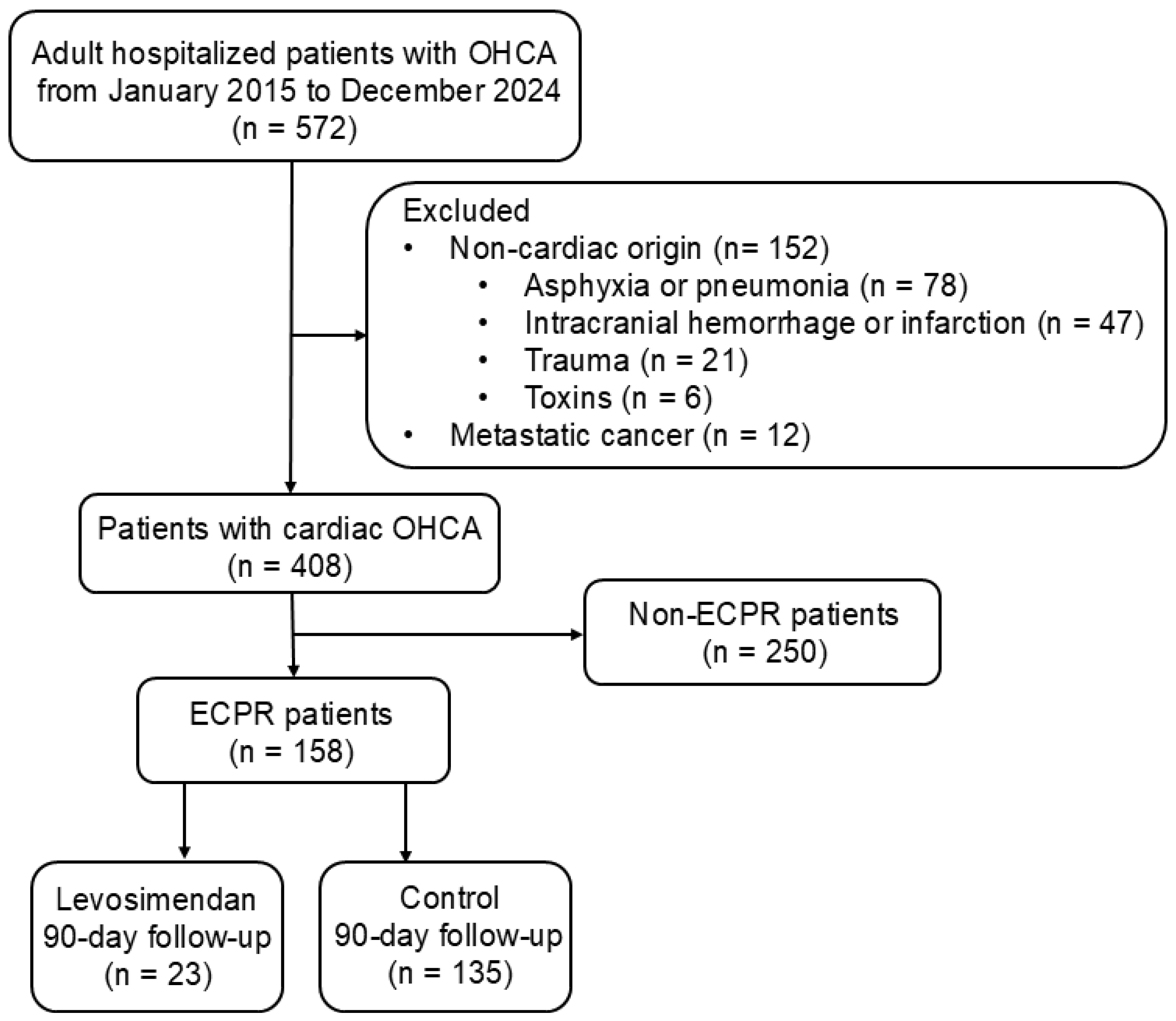
2.1. Study Design and Population
2.2. Vasopressors (Epinephrine, Norepinephrine, and Vasopressin)
2.3. Inotropes (Dopamine, Dobutamine, Milrinone, and Levosimendan)
2.4. VIS and SCAI Staging at Admission
2.5. Left Ventricular Function Test at 24 h After OHCA
2.6. Levosimendan Use Within 72 h of ECPR
2.7. Statistical Analysis
3. Results
3.1. Baseline Clinical Characteristics
3.2. Follow-Up of Laboratory Tests on the Day of Admission
3.3. Analyses of Sequential Organ Failure Assessment (SOFA), Length of Stay, Clinical Outcomes, and Cerebral Performance Category (CPC)
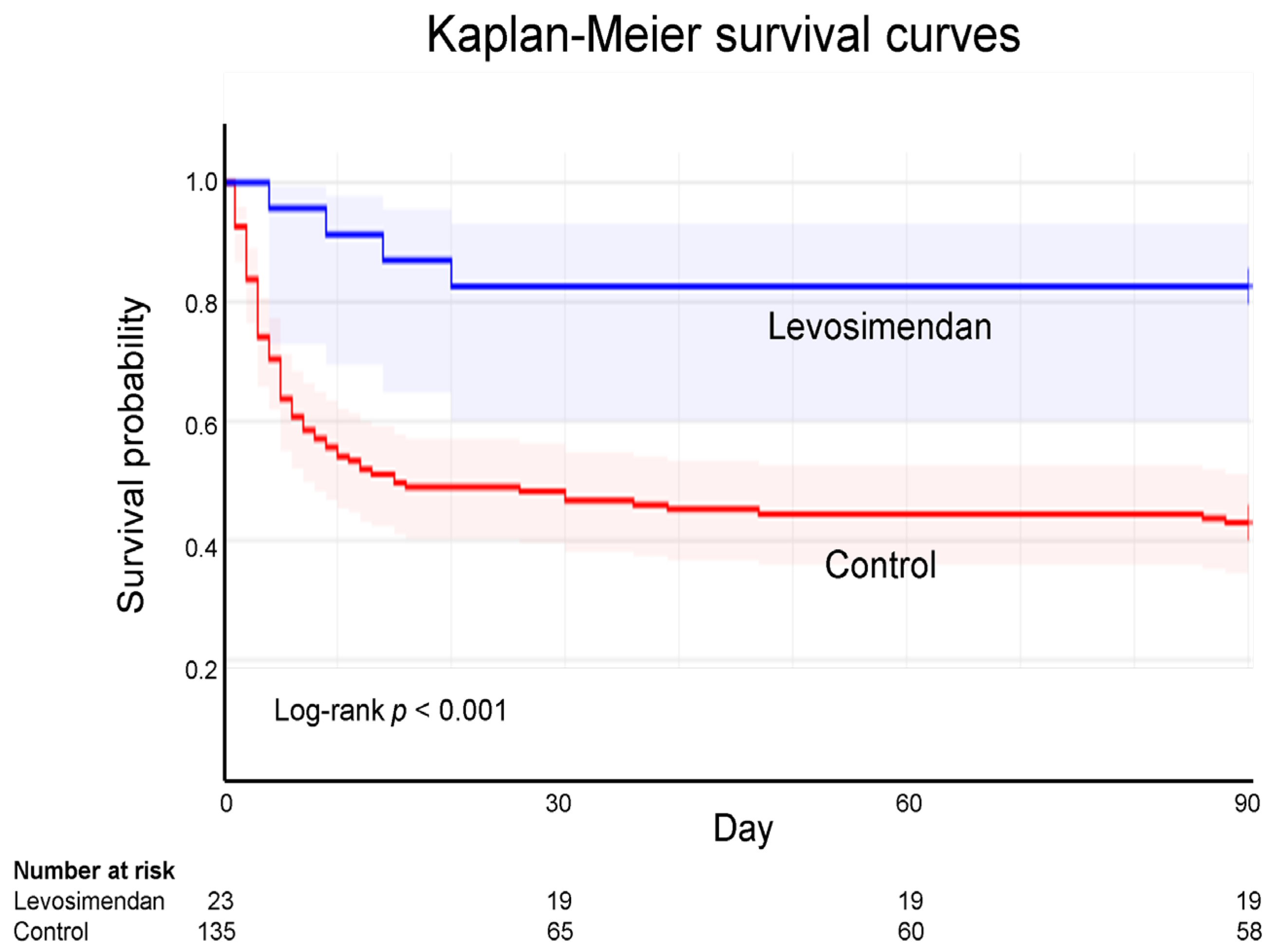
3.4. Kaplan–Meier Survival Curves of ECPR
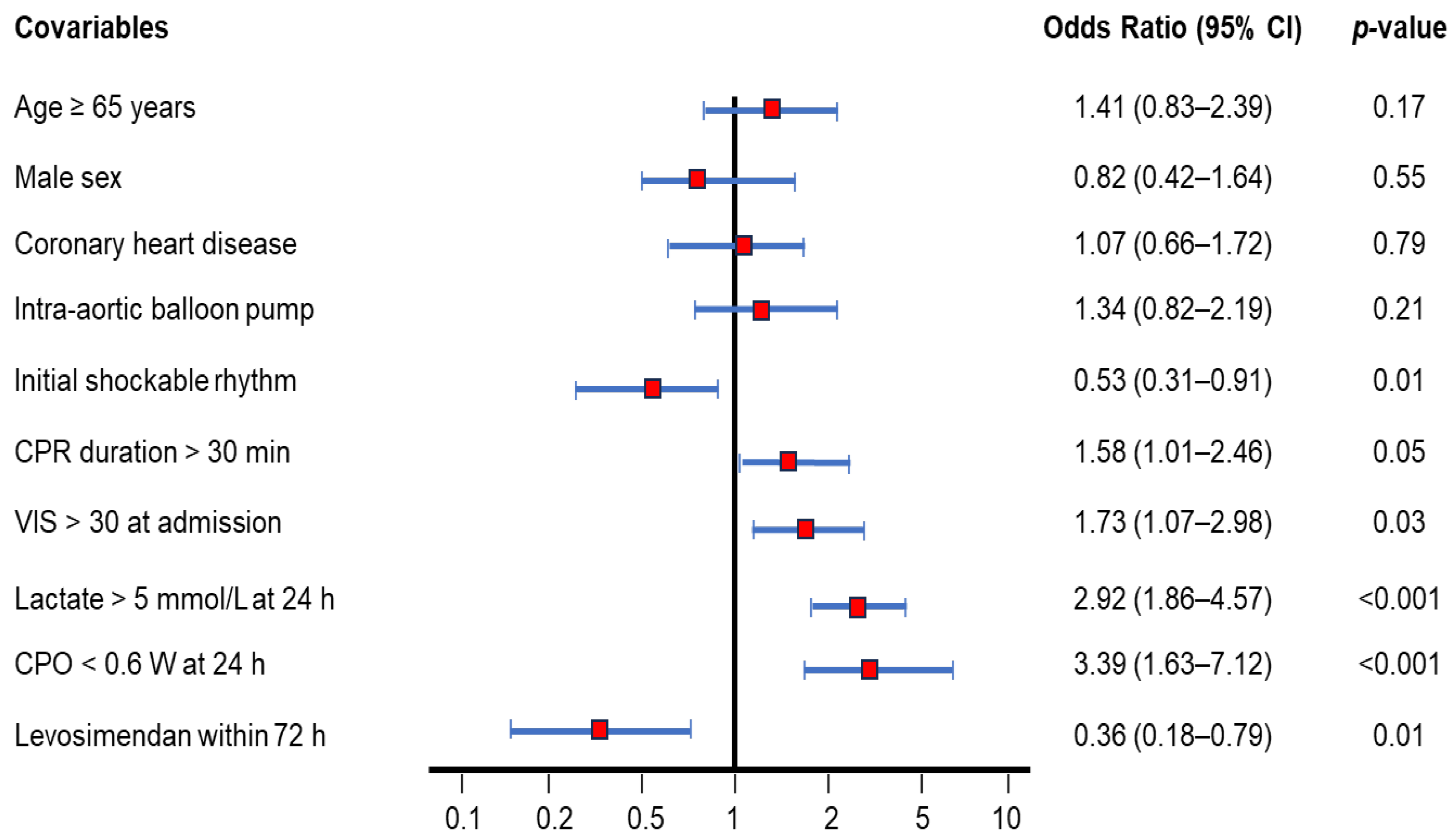
3.5. Ninety-Day Mortality Rate-Adjusted Covariables Using Cox Regression Model
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CAHP | Cardiac arrest hospital prognosis |
| CI | Confidence interval |
| CPC | Cerebral performance category |
| CPO | Cardiac power output |
| CPR | Cardiopulmonary resuscitation |
| ECPR | Extracorporeal cardiopulmonary resuscitation |
| ECMO | Extracorporeal membrane oxygenation |
| LVEF | Left ventricular ejection fraction |
| LVCI | Left ventricular cardiac index |
| OHCA | Out-of-hospital cardiac arrest |
| SCAI | Society for cardiovascular angiography and interventions |
| SOFA | Sequential organ failure assessment |
| VIS | Vasoactive-inotropic score |
References
- Zheng, J.; Lv, C.; Zheng, W.; Zhang, G.; Tan, H.; Ma, Y.; Zhu, Y.; Li, C.; Han, X.; Yan, S.; et al. Incidence, process of care, and outcomes of out-of-hospital cardiac arrest in China: A prospective study of the BASIC-OHCA registry. Lancet Public Health 2023, 8, e923–e932. [Google Scholar] [CrossRef] [PubMed]
- Kondo, T.; Araki, T.; Imaizumi, T.; Sumita, Y.; Nakai, M.; Tanaka, A.; Okumura, T.; Butt, J.H.; Petrie, M.C.; McMurray, J.J.; et al. Prognosis in Patients with Cardiogenic Shock Who Received Temporary Mechanical Circulatory Support. JACC Asia 2022, 3, 122–134. [Google Scholar] [CrossRef] [PubMed]
- Yan, S.; Gan, Y.; Jiang, N.; Wang, R.; Chen, Y.; Luo, Z.; Zong, Q.; Chen, S.; Lv, C. The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: A systematic review and meta-analysis. Crit. Care 2020, 24, 61. [Google Scholar] [CrossRef]
- Kim, M.W.; Kim, T.H.; Song, K.J.; Shin, S.D.; Kim, C.H.; Lee, E.J.; Kim, K. Comparison between dispatcher-assisted bystander CPR and self-led bystander CPR in out-of-hospital cardiac arrest (OHCA). Resuscitation 2021, 158, 64–70. [Google Scholar] [CrossRef]
- Narducci, M.L.; Pedicino, D. A new defibrillation strategy for refractory ventricular fibrillation during out-of-hospital cardiac arrest: Are two better than one? Eur. Heart J. 2023, 44, 919–920. [Google Scholar] [CrossRef]
- Mandigers, L.; Boersma, E.; Uil, C.A.D.; Gommers, D.; Bělohlávek, J.; Belliato, M.; Lorusso, R.; Miranda, D.d.R. Systematic review and meta-analysis comparing low-flow duration of extracorporeal and conventional cardiopulmonary resuscitation. Interact. Cardiovasc. Thorac. Surg. 2022, 35, ivac219. [Google Scholar] [CrossRef]
- Miraglia, D.; Almanzar, C.; Rivera, E.; Alonso, W. Extracorporeal cardiopulmonary resuscitation for refractory cardiac arrest: A scoping review. J. Am. Coll. Emerg. Physicians Open 2021, 2, e12380. [Google Scholar] [CrossRef]
- Inoue, A.; Hifumi, T.; Sakamoto, T.; Kuroda, Y. Extracorporeal Cardiopulmonary Resuscitation for Out-of-Hospital Cardiac Arrest in Adult Patients. J. Am. Heart Assoc. 2020, 9, e015291. [Google Scholar] [CrossRef]
- Low, C.J.W.; Ramanathan, K.; Ling, R.R.; Ho, M.J.C.; Chen, Y.; Lorusso, R.; MacLaren, G.; Shekar, K.; Brodie, D. Extracorporeal cardiopulmonary resuscitation vs. conventional cardiopulmonary resuscitation in adults with cardiac arrest: A comparative meta-analysis and trial sequential analysis. Lancet Respir. Med. 2023, 11, 883–893. [Google Scholar] [CrossRef]
- Low, C.J.W.; Ling, R.R.; Ramanathan, K.; Chen, Y.; Rochwerg, B.; Kitamura, T.; Iwami, T.; Ong, M.E.H.; Okada, Y. Extracorporeal cardiopulmonary resuscitation vs. conventional CPR in cardiac arrest: An updated meta-analysis and trial sequential analysis. Crit. Care 2024, 28, 57. [Google Scholar] [CrossRef]
- Suverein, M.M.; Delnoij, T.S.; Lorusso, R.; Bruinsma, G.J.B.B.; Otterspoor, L.; Kraemer, C.V.E.; Vlaar, A.P.; van der Heijden, J.J.; Scholten, E.; Uil, C.D.; et al. Early Extracorporeal CPR for Refractory Out-of-Hospital Cardiac Arrest. N. Engl. J. Med. 2023, 388, 299–309. [Google Scholar] [CrossRef] [PubMed]
- Yannopoulos, D.; Bartos, J.; Raveendran, G.; Walser, E.; Connett, J.; Murray, T.A.; Collins, G.; Zhang, L.; Kalra, R.; Kosmopoulos, M.; et al. Advanced reperfusion strategies for patients with out-of-hospital cardiac arrest and refractory ventricular fibrillation (ARREST): A phase 2, single centre, open-label, randomised controlled trial. Lancet 2020, 396, 1807–1816. [Google Scholar] [CrossRef] [PubMed]
- Heringlake, M.; Alvarez, J.; Bettex, D.; Bouchez, S.; Fruhwald, S.; Girardis, M.; Grossini, E.; Guarracino, F.; Herpain, A.; Toller, W.; et al. An update on levosimendan in acute cardiac care: Applications and recommendations for optimal efficacy and safety. Expert Rev. Cardiovasc. Ther. 2021, 19, 325–335. [Google Scholar] [CrossRef] [PubMed]
- Girardis, M.; Bettex, D.; Bojan, M.; Demponeras, C.; Fruhwald, S.; Gál, J.; Groesdonk, H.V.; Guarracino, F.; Guerrero-Orriach, J.L.; Heringlake, M.; et al. Levosimendan in intensive care and emergency medicine: Literature update and expert recommendations for optimal efficacy and safety. J. Anesthesia, Analg. Crit. Care 2022, 2, 4. [Google Scholar] [CrossRef]
- Luo, J.-C.; Zheng, W.-H.; Meng, C.; Zhou, H.; Xu, Y.; Tu, G.-W.; Luo, Z.; Huang, H.-B. Levosimendan to Facilitate Weaning from Cardiorespiratory Support in Critically Ill Patients: A Meta-Analysis. Front. Med. 2021, 8, 741108. [Google Scholar] [CrossRef]
- Tabi, M.; Burstein, B.J.; Ahmed, A.; Dezfulian, C.; Kashani, K.B.; Jentzer, J.C. Shock Severity and Hospital Mortality in Out of Hospital Cardiac Arrest Patients Treated with Targeted Temperature Management. Shock 2021, 55, 48–54. [Google Scholar] [CrossRef]
- Belletti, A.; Lerose, C.C.; Zangrillo, A.; Landoni, G. Vasoactive-Inotropic Score: Evolution, Clinical Utility, and Pitfalls. J. Cardiothorac. Vasc. Anesthesia 2021, 35, 3067–3077. [Google Scholar] [CrossRef]
- Na, S.J.; Chung, C.R.; Cho, Y.H.; Jeon, K.; Suh, G.Y.; Ahn, J.H.; Yang, J.H. Vasoactive inotropic score as a predictor of mortality in adult patients with cardiogenic shock: Medical therapy vs. ECMO. Rev. Esp. Cardiol. 2019, 72, 40. [Google Scholar] [CrossRef]
- Kapur, N.K.; Kanwar, M.; Sinha, S.S.; Thayer, K.L.; Garan, A.R.; Hernandez-Montfort, J.; Zhang, Y.; Li, B.; Baca, P.; Dieng, F.; et al. Criteria for Defining Stages of Cardiogenic Shock Severity. J. Am. Coll. Cardiol. 2022, 80, 185–198. [Google Scholar] [CrossRef]
- Tehrani, B.N.; Truesdell, A.G.; Sherwood, M.; Desai, S.; Tran, H.A.; Epps, K.C.; Singh, R.; Psotka, M.; Shah, P.; Cooper, L.B.; et al. Standardized Team-Based Care for Cardiogenic Shock. J. Am. Coll. Cardiol. 2019, 73, 1659–1669. [Google Scholar] [CrossRef]
- Pashkovetsky, E.; Gupta, C.A.; Aronow, W.S. Use of levosimendan in acute and advanced heart failure: Short review on available real-world data. Ther. Clin. Risk Manag. 2019, 15, 765–772. [Google Scholar] [CrossRef] [PubMed]
- Papp, Z.; Agostoni, P.; Alvarez, J.; Bettex, D.; Bouchez, S.; Brito, D.; Černý, V.; Comin-Colet, J.; Crespo-Leiro, M.G.; Delgado, J.F.; et al. Levosimendan Efficacy and Safety: 20 Years of SIMDAX in Clinical Use. J. Cardiovasc. Pharmacol. 2020, 76, 4–22. [Google Scholar] [CrossRef] [PubMed]
- Desai, H.N.; Sangurima, L.; Malik, M.M.; Ganatra, N.; Siby, R.; Kumar, S.; Khan, S.; Jayaprakasan, S.K.; Cheriachan, D.; Mohammed, L. Therapeutic Development of Levosimendan in Acute and Advanced Heart Failure: A Systematic Review. Cureus 2023, 15, 37844. [Google Scholar] [CrossRef] [PubMed]
- Glinka, L.; Mayzner-Zawadzka, E.; Onichimowski, D.; Jalali, R.; Glinka, M. Levosimendan in the modern treatment of patients with acute heart failure of various aetiologies. Arch. Med. Sci. 2019, 17, 296–303. [Google Scholar] [CrossRef]
- Susilo, H.; Aldian, F.M.; Wungu, C.D.K.; Alsagaff, M.Y.; Sutanto, H.; Multazam, C.E.C.Z. Levosimendan, a Promising Pharmacotherapy in Cardiogenic Shock: A Comprehensive Review. Eur. Cardiol. Rev. 2025, 19, e21. [Google Scholar] [CrossRef]
- Brahmbhatt, D.H.; Daly, A.L.; Luk, A.C.; Fan, E.; Billia, F. Liberation from Venoarterial Extracorporeal Membrane Oxygenation: A Review. Circ. Heart Fail. 2021, 14, 823–836. [Google Scholar] [CrossRef]
- Lüsebrink, E.; Stremmel, C.; Stark, K.; Joskowiak, D.; Czermak, T.; Born, F.; Kupka, D.; Scherer, C.; Orban, M.; Petzold, T.; et al. Update on Weaning from Veno-Arterial Extracorporeal Membrane Oxygenation. J. Clin. Med. 2020, 9, 992. [Google Scholar] [CrossRef]
- Quintero-Altare, A.; Flórez-Navas, C.; Robayo-Amortegui, H.; Rojas-Arrieta, M.; Tuta-Quintero, E.; Bastidas-Goyes, A.; Martínez-Delgado, L.; Casallas-Barrera, J.O.; Poveda-Henao, C.; Buitrago-Bernal, R. Boosting the Beat: A Critical Showdown of Levosimendan and Milrinone in Surgical and Non-Surgical Scenarios: A Narrative Review. J. Cardiovasc. Pharmacol. Ther. 2024, 29, 6431. [Google Scholar] [CrossRef]
- Zeitouni, M.; Dorvillius, E.; Sulman, D.; Procopi, N.; Beaupré, F.; Devos, P.; Barthélémy, O.; Rouanet, S.; Ferrante, A.; Chommeloux, J.; et al. Levosimendan in Patients with Cardiogenic Shock Refractory to Dobutamine Weaning. Am. J. Cardiovasc. Drugs 2024, 25, 249–258. [Google Scholar] [CrossRef]
- Bertini, P.; Paternoster, G.; Landoni, G.; Falcone, M.; Nocci, M.; Costanzo, D.; Brizzi, G.; Romani, M.; Esposito, A.; Guarracino, F. Beneficial effects of levosimendan to wean patients from VA-ECMO: A systematic review and meta-analysis. Minerva Cardioangiol. 2023, 71, 564–574. [Google Scholar] [CrossRef]
- Gaisendrees, C.; Schlachtenberger, G.; Gerfer, S.; Krasivskyi, I.; Djordjevic, I.; Sabashnikov, A.; Kosmopoulos, M.; Jaeger, D.; Luehr, M.; Kuhn, E.; et al. The impact of levosimendan on survival and weaning from ECMO after extracorporeal cardiopulmonary resuscitation. Artif. Organs 2023, 47, 1351–1360. [Google Scholar] [CrossRef] [PubMed]
- Ellouze, O.; Faure, A.S.; Radhouani, M.; Abou-Arab, O.; Besnier, E.; Moussa, M.; Cransac, A.; Ksiazek, E.; Fischer, M.; Mertes, P.M.; et al. Levosimendan in venoarterial ECMO weaning. Rational and design of a randomized double blind multicentre trial. ESC Heart Fail. 2021, 8, 3339–3347. [Google Scholar] [CrossRef] [PubMed]
- Kaddoura, R.; Omar, A.S.; Ibrahim, M.I.M.; Alkhulaifi, A.; Lorusso, R.; Elsherbini, H.; Soliman, O.; Caliskan, K. The Effectiveness of Levosimendan on Veno-Arterial Extracorporeal Membrane Oxygenation Management and Outcome: A Systematic Review and Meta-Analysis. J. Cardiothorac. Vasc. Anesthesia 2021, 35, 2483–2495. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Zhang, L.; Yao, Y.; Li, Y.; Qin, W.; Li, Y.; Xue, W.; Li, P.; Chen, Y.; Chen, X.; et al. Effects of levosimendan on the outcome of veno-arterial extracorporeal membrane oxygenation: A systematic review and meta-analysis. Clin. Res. Cardiol. 2024, 113, 509–521. [Google Scholar] [CrossRef]
- Deppe, A.C.; Wahlers, T.C.W.; Weber, C.; Esser, M.; Eghbalzadeh, K.; Sabashnikov, A.; Djordjevic, I.; Maier, J.; Merkle, J.; Choi, Y.-H.; et al. Levosimendan Reduces Mortality and Low Cardiac Output Syndrome in Cardiac Surgery. Thorac. Cardiovasc. Surg. 2020, 68, 401–409. [Google Scholar] [CrossRef]
- Hau, M.; Fong, K.-M.; Au, S.-Y. Levosimendan’s effect on venoarterial extracorporeal membrane oxygenation weaning. Int. J. Artif. Organs 2022, 45, 571–579. [Google Scholar] [CrossRef]
- Mastoris, I.; Tonna, J.E.; Hu, J.; Sauer, A.J.; Haglund, N.A.; Rycus, P.; Wang, Y.; Wallisch, W.J.; Abicht, T.O.; Danter, M.R.; et al. Use of Extracorporeal Membrane Oxygenation as Bridge to Replacement Therapies in Cardiogenic Shock: Insights from the Extracorporeal Life Support Organization. Circ. Heart Fail. 2022, 15, e008777. [Google Scholar] [CrossRef]
- Hyun, J.; Kim, A.-R.; Lee, S.E.; Hong, J.A.; Kang, P.J.; Jung, S.-H.; Kim, M.-S. Vasoactive-Inotropic Score as a Determinant of Timely Initiation of Venoarterial Extracorporeal Membrane Oxygenation in Patients with Cardiogenic Shock. Circ. J. 2022, 86, 687–694. [Google Scholar] [CrossRef]
- Kaddoura, R.; Orabi, B.; Omar, A.S.; Ibrahim, M.I.M.; Alyafei, S.A.; Alkhulaifi, A.; Shehatta, A.L. The Role of Levosimendan in Extracorporeal Membrane Oxygenation for Refractory Cardiac Arrest. J. Cardiothorac. Vasc. Anesthesia 2025, 39, 957–966. [Google Scholar] [CrossRef]
- Tian, X.; Wang, L.; Li, C.; Shao, J.; Jia, M.; Wang, H.; Hou, X. Combining the vasoactive-inotropic score with lactate levels to predict mortality in post-cardiotomy patients supported with venoarterial extracorporeal membrane oxygenation. Eur. J. Cardio-Thoracic Surg. 2024, 66, ezae334. [Google Scholar] [CrossRef]
- Burstein, B.; Anand, V.; Ternus, B.; Tabi, M.; Anavekar, N.S.; Borlaug, B.A.; Barsness, G.W.; Kane, G.C.; Oh, J.K.; Jentzer, J.C. Noninvasive echocardiographic cardiac power output predicts mortality in cardiac intensive care unit patients. Am. Heart J. 2021, 245, 149–159. [Google Scholar] [CrossRef] [PubMed]
- Tholén, M.; Ricksten, S.-E.; Lannemyr, L. Effects of levosimendan on renal blood flow and glomerular filtration in patients with acute kidney injury after cardiac surgery: A double blind, randomized placebo-controlled study. Crit. Care 2021, 25, 207. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-W.; Lee, W.-C.; Wu, P.-J.; Fang, H.-Y.; Fang, Y.-N.; Chen, H.-C.; Tong, M.-S.; Sung, P.-H.; Lee, C.-H.; Chung, W.-J. Early Levosimendan Administration Improved Weaning Success Rate in Extracorporeal Membrane Oxygenation in Patients with Cardiogenic Shock. Front. Cardiovasc. Med. 2022, 9, 912321. [Google Scholar] [CrossRef] [PubMed]
- Guilherme, E.; Jacquet-Lagrèze, M.; Pozzi, M.; Achana, F.; Armoiry, X.; Fellahi, J.-L. Can levosimendan reduce ECMO weaning failure in cardiogenic shock?: A cohort study with propensity score analysis. Crit. Care 2020, 24, 442. [Google Scholar] [CrossRef]
- Paulo, N.; Kimmoun, A.; Hajage, D.; Hubert, P.; Levy, D.; de Chambrun, M.P.; Chommeloux, J.; Saura, O.; Del Marmol, G.; Moyon, Q.; et al. Does Levosimendan hasten veno-arterial ECMO weaning? A propensity score matching analysis. Ann. Intensiv. Care 2025, 15, 48. [Google Scholar] [CrossRef]
| Levosimendan (n = 23) | Control (n = 135) | p-Value | ||
|---|---|---|---|---|
| Age (y), mean ± SD | 54.1 ± 12.9 | 54.3 ± 14.1 | 0.96 | |
| Male sex, n (%) | 21 (91.3) | 117 (86.7) | 0.54 | |
| BMI (kg/m2), mean ± SD | 27.7 ± 4.1 | 26.8 ± 4.8 | 0.34 | |
| Medical history, n (%) | Hypertension | 13 (56.5) | 52 (38.5) | 0.11 |
| Hyperlipidemia | 9 (39.1) | 49 (36.3) | 0.66 | |
| Diabetes mellitus | 5 (21.7) | 28 (20.7) | 0.91 | |
| Chronic heart failure | 4 (17.4) | 20 (14.8) | 0.75 | |
| Coronary artery disease | 4 (17.4) | 26 (19.3) | 0.83 | |
| End-stage renal disease | 1 (4.3) | 7 (5.2) | 0.87 | |
| Cerebrovascular disease | 1 (4.3) | 3 (2.2) | 0.55 | |
| Chronic obstructive pulmonary disease | 1 (4.3) | 1 (0.7) | 0.15 | |
| Witnessed cardiac arrest, n (%) | 17 (74.3) | 92 (68.2) | 0.48 | |
| Bystander CPR, n (%) | 12 (52.2) | 57 (42.2) | 0.29 | |
| Initial shockable rhythm, n (%) | 2 (91.3) | 98 (72.6) | 0.05 | |
| No-flow time (min), mean ± SD | 4.6 ± 1.5 | 4.9 ± 0.4 | 0.51 | |
| CPR duration (min), mean ± SD | 30.7 ± 13.7 | 35.5 ± 25.3 | 0.37 | |
| Initial arterial pH,mean ± SD | 7.04 ± 0.16 | 7.01 ± 0.19 | 0.39 | |
| Total Epinephrine while CPR (mg), mean ± SD | 9.3 ± 5.7 | 9.3 ± 7.1 | 0.98 | |
| CAHP score, mean ± SD | 140.3 ± 26.7 | 153.8 ± 7.1 | 0.13 | |
| CHD, n (%) | Coronary angiography | 15 (65.2) | 92 (68.1) | 0.78 |
| Left main disease | 6 (26.1) | 17 (12.6) | 0.09 | |
| Triple-vessel disease | 9 (39.1) | 47 (34.8) | 0.69 | |
| AMI, n (%) | Percutaneous coronary intervention | 14 (60.9) | 85 (63.0) | 0.85 |
| ST-elevation myocardial infarction | 12 (52.2) | 55 (40.7) | 0.31 | |
| Intra-aortic balloon pump, n (%) | 11 (47.8) | 38 (28.1) | 0.06 | |
| Targeted temperature management, n (%) | 17 (73.9) | 96 (71.1) | 0.78 | |
| Cardiogenic shock, n (%) | SCAI Stage C | 3 (13.0) | 24 (17.8) | 0.58 |
| SCAI Stage D | 9 (39.1) | 50 (37.0) | 0.85 | |
| SCAI Stage E | 11 (47.8) | 61 (45.2) | 0.82 | |
| VISat admission, mean ± SD | 34.9 ± 23.6 | 32.6 ± 27.6 | 0.72 | |
| Norepinephrine (μg/kg/min), mean ± SD | 0.3 ± 0.2 | 0.2 ± 0.2 | ||
| Dopamine (μg/kg/min), mean ± SD | 6.3 ± 7.7 | 8.1 ± 9.3 | ||
| Dobutamine (μg/kg/min), mean ± SD | 0.5 ± 1.5 | 0.2 ± 0.9 | ||
| LVEF at 24 h (%), mean ± SD | 31.2 ± 12.2 | 31.0 ± 15.4 | 0.97 | |
| LVCI at 24 h (L/min/M2), mean ± SD | 1.73 ± 0.83 | 1.60 ± 1.02 | 0.56 | |
| CPO at 24 h (W), mean ± SD | 0.54 ± 0.26 | 0.48 ± 0.35 | 0.41 | |
| Levosimendan (n = 23) | Control (n = 135) | p-Value | |
|---|---|---|---|
| Blood counts | |||
| WBC (K/μL) at 6 h, mean ± SD | 14.0 ± 6.8 | 13.9 ± 6.0 | 0.98 |
| WBC (K/μL) at 24 h, mean ± SD | 14.4 ± 7.8 | 15.5 ± 7.0 | 0.51 |
| Neutrophils (K/μL) at 6 h, mean ± SD | 7.6 ± 5.8 | 7.9 ± 5.0 | 0.78 |
| Neutrophils (K/μL) at 24 h, mean ± SD | 12.4 ± 7.4 | 13.2 ± 6.5 | 0.57 |
| Hemoglobin (%) at 6 h, mean ± SD | 13.2 ± 2.4 | 12.5 ± 2.6 | 0.05 |
| Hemoglobin (%) at 24 h, mean ± SD | 12.1 ± 1.9 | 11.0 ± 2.5 | 0.06 |
| Platelet (K/μL) at 6 h, mean ± SD | 182.5 ± 74.8 | 189.3 ± 140.8 | 0.82 |
| Platelet (K/μL) at 24 h, mean ± SD | 123.5 ± 53.3 | 134.6 ± 72.0 | 0.48 |
| Biochemical indices | |||
| Troponin-I (ng/mL) at 6 h, mean ± SD | 6.9 ± 5.7 | 4.3 ± 3.8 | 0.08 |
| Troponin-I (ng/mL) at 24 h, mean ± SD | 110.2 ± 100.3 | 80.1 ± 80.8 | 0.11 |
| AST (U/L) at 6 h, mean ± SD | 249.6 ± 198.8 | 305.4 ± 311.4 | 0.46 |
| AST (U/L) at 24 h, mean ± SD | 577.6 ± 287.7 | 812.6 ± 1872.8 | 0.58 |
| ALT (U/L) at 6 h, mean ± SD | 125.2 ± 105.4 | 150.8 ± 177.6 | 0.53 |
| ALT (U/L) at 24 h, mean ± SD | 232.6 ± 180.3 | 272.7 ± 566.0 | 0.74 |
| BUN (mg/dL) at 6 h, mean ± SD | 21.0 ± 7.7 | 24.8 ± 20.6 | 0.41 |
| BUN (mg/dL) at 24 h, mean ± SD | 26.2 ± 6.1 | 28.9 ± 17.6 | 0.47 |
| Creatinine (mg/dL) at 6 h, mean ± SD | 1.5 ± 0.4 | 2.0 ± 2.0 | 0.22 |
| Creatinine (mg/dL) at 24 h, mean ± SD | 1.7 ± 0.4 | 2.0 ± 1.5 | 0.29 |
| Lactate (mmol/L) at 6 h, mean ± SD | 14.0 ± 6.3 | 16.0 ± 6.8 | 0.21 |
| Lactate (mmol/L) at 24 h, mean ± SD | 5.1 ± 2.8 | 7.2 ± 6.2 | 0.12 |
| Levosimendan (n = 23) | Control (n = 135) | p-Value | |
|---|---|---|---|
| SOFA on day 1, mean ± SD | 14.1 ± 1.9 | 14.4 ± 2.5 | 0.64 |
| SOFA on day 3, mean ± SD | 13.4 ± 2.6 | 15.8 ± 5.2 | 0.03 |
| SOFA on day 5, mean ± SD | 12.7 ± 3.3 | 16.0 ± 6.2 | 0.01 |
| SOFA on day 7, mean ± SD | 11.6 ± 3.4 | 16.2 ± 7.0 | 0.003 |
| Hospital stay (days), mean ± SD | 38.0 ± 21.7 | 24.5 ± 26.0 | 0.02 |
| ECMO weaning failure, n (%) | 3 (13.0) | 71 (52.6) | <0.001 |
| 90-day mortality, n (%) | 4 (17.4) | 77 (57.0) | <0.001 |
| 90-day poor neurological outcomes, n (%) | 11 (47.8) | 97 (71.8) | 0.06 |
| CPC sub-analyses at 90-day follow-up | |||
| CPC 1, n (%) | 6 (26.1) | 27 (20.0) | |
| CPC 2, n (%) | 6 (26.1) | 11 (8.1) | |
| CPC 3, n (%) | 5 (21.7) | 7 (5.2) | |
| CPC 4, n (%) | 2 (8.7) | 13 (9.6) | |
| CPC 5, n (%) | 4 (17.4) | 77 (57.0) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, D.-L.; Lin, Y.-K.; Wang, G.-J.; Chang, K.-C. Effect of Levosimendan Use on All-Cause Mortality in Out-of-Hospital Cardiac Arrest Survivors After Extracorporeal Cardiopulmonary Resuscitation. Biomedicines 2025, 13, 955. https://doi.org/10.3390/biomedicines13040955
Chen D-L, Lin Y-K, Wang G-J, Chang K-C. Effect of Levosimendan Use on All-Cause Mortality in Out-of-Hospital Cardiac Arrest Survivors After Extracorporeal Cardiopulmonary Resuscitation. Biomedicines. 2025; 13(4):955. https://doi.org/10.3390/biomedicines13040955
Chicago/Turabian StyleChen, Da-Long, Yu-Kai Lin, Guei-Jane Wang, and Kuan-Cheng Chang. 2025. "Effect of Levosimendan Use on All-Cause Mortality in Out-of-Hospital Cardiac Arrest Survivors After Extracorporeal Cardiopulmonary Resuscitation" Biomedicines 13, no. 4: 955. https://doi.org/10.3390/biomedicines13040955
APA StyleChen, D.-L., Lin, Y.-K., Wang, G.-J., & Chang, K.-C. (2025). Effect of Levosimendan Use on All-Cause Mortality in Out-of-Hospital Cardiac Arrest Survivors After Extracorporeal Cardiopulmonary Resuscitation. Biomedicines, 13(4), 955. https://doi.org/10.3390/biomedicines13040955






