Abstract
Background: Over the past few decades, the prevalence of obesity has significantly increased worldwide, particularly among children. This trend represents a global health challenge. Considering the pivotal role of obesity in the development of metabolic disorders, the identification and characterization of pathogenic gene variants in children with severe forms of obesity are key priorities in fundamental endocrinology. Methods: We performed whole-exome sequencing (WES) in 163 Russian children with morbid obesity and identified 96 pathogenic or likely pathogenic variants in 61 genes. These variants were clinically significant in 64 children (38.79% of the cohort). Results: Notably, 42 of the identified variants have not been previously described in the literature or reported in existing databases. Conclusions: The findings of this study will enable a more personalized approach to the diagnosis and treatment of patients with syndromic and polygenic forms of obesity. Moreover, these results advance our understanding of the genetic architecture of obesity in the Russian population.
1. Introduction
The World Health Organization (WHO) predicts that, by 2030, 250 million children and adolescents aged 5–19 years will be affected by obesity. This projection highlights the significance of the issue as a global health challenge with extensive consequences. A large-scale study on the prevalence of overweight among children in the Russian Federation examined 13,700 children aged 6–18 years, with a mean age of 13 years. The study identified overweight in 5.5% to 11.8% of cases and obesity in 5.5% of children living in rural areas and 8.5% of those in urban areas [1]. A study conducted in Moscow between 2017 and 2018 as part of the COSI (Childhood Obesity Surveillance Initiative) program included 2166 seven-year-old children. The study reported overweight in 27% of boys and 22% of girls, while obesity was observed in 10% and 6%, respectively [2]. DNA diagnostics is essential for understanding the underlying molecular mechanisms and improving diagnosis, prognosis, and treatment.
Advances in genomic technologies have led to the identification of numerous genetic loci associated with this condition. These studies range from severe early-onset cases and include common multifactorial polygenic forms. Methods such as whole-exome sequencing (WES) and whole-genome sequencing facilitate the identification of novel genes and biological pathways involved in syndromic and monogenic forms of obesity. However, the molecular architecture of severe childhood obesity remains poorly characterized, necessitating further investigation of causal genes. This will optimize diagnostic approaches and facilitate the development of novel therapeutic agents targeting gene products and related biochemical pathways.
Objective: The aim of this study is to identify and characterize causal gene variants in children with severe obesity using whole-exome sequencing.
2. Materials and Methods
This study included 163 unrelated patients diagnosed with severe early-onset obesity, who were examined at the Endocrinology Research Centre. Written informed consent was obtained from each patient or their legal representative. This study was approved by the Bioethics Committee of the Endocrinology Research Centre (protocol №18, dated 10 October 2022). A detailed description of the study cohort is presented in Table 1.

Table 1.
Characteristics of the study cohort.
Inclusion criteria: Girls and boys with obesity onset before the age of 7 years and a BMI SDS (standard deviation score) greater than 3.5. Exclusion criteria: The presence of organic central nervous system pathology.
The study protocol included a clinical examination of patients, a detailed collection of family history, a physical examination, and an assessment of phenotypic features and anthropometric parameters. Height SDS and BMI SDS were calculated using the Auxology 1.0 software (Pfizer, USA). Laboratory diagnostics included analysis of glycated hemoglobin (HbA1c), hemoglobin, total and ionized calcium, phosphorus, fasting blood glucose, triglycerides (TG), total cholesterol, low-density lipoproteins (LDL), high-density lipoproteins (HDL), alanine aminotransferase (ALT), and aspartate aminotransferase (AST). Hormonal profiling included the measurement of insulin levels, thyroid-stimulating hormone (TSH), free thyroxine (FT4), parathyroid hormone (PTH), insulin-like growth factor 1 (IGF-1), calcitonin, and 25-hydroxyvitamin D (25-OH vitamin D). Instrumental diagnostics included ultrasound examination of the abdominal organs, kidneys, and thyroid gland, as well as X-ray imaging of the hands and wrist joints.
Food intake was recorded using a meal frequency questionnaire. A questionnaire proposed by Dykens et al. was used to assess polyphagy [3]. Subsequently, the dietitian assessed the actual nutrition according to a diary filled in by the patient’s parents for 7 days. To assess basal metabolic rate at rest, indirect calorimetry was performed in some patients (patients over 5 years old without neurological diseases). Subsequently, the diet was adjusted taking into account the individual characteristics of the patient and the results of examinations.
Genomic DNA was extracted from peripheral blood lymphocytes using the MagPure Blood DNA Kit (Magen, Guangzhou, China). Quantitative and qualitative analysis of the extracted DNA was performed using a Nanodrop 2000 spectrophotometer (Thermo Fisher Scientific, Waltham, MA, USA) and a Qubit 2.0 fluorometer (Invitrogen, Carlsbad, CA, USA) with the Qubit dsDNA HS Assay Kit. Whole-exome libraries were prepared using the KAPA HyperPlus Kit (Roche, Basel, Switzerland) according to the manufacturer’s protocol. The prepared libraries were enriched using the KAPA HyperExome Kit (Roche, Basel, Switzerland). Sequencing was performed on the Novaseq 6000 platform (Illumina, San Diego, CA, USA), using the Novaseq 6000 S4 Reagent Kit v1.5 (200 cycles) with paired-end sequencing at 2 × 100 bp. Result validation was performed using specific primers designed for the targeting of fragments of genes by Sanger sequencing on an AB3500 platform (Applied Biosystems, Waltham, MA, USA).
NGS sequencing data were processed using an automated algorithm that included alignment to the human reference genome (GRCh38), post-alignment processing, variant calling, quality filtering, and annotation of identified variants for all known transcripts of each gene from the RefSeq database. Pathogenicity prediction was performed using computational algorithms in accordance with the recommendations of the American College of Medical Genetics and Genomics (ACMG) [4].
3. Results
As a result of the conducted studies, 72 children (out of 163 examined) with morbid obesity (43.63%) were found to have various variants of pathogenic and likely pathogenic clinical significance. In eight patients, the identified variants were classified as ‘incidental’ findings associated with heterozygous carriage of pathogenic variants linked to the following diseases: thiamine-responsive megaloblastic anemia (OMIM: 249270)—c.1223+1G>A (SLC19A2), cortisone reductase deficiency type 1—c.787G>A, p.Val263Ile (H6PD), malignant hyperthermia—c.356G>A, p.Arg119His (CACNA1S), combined pituitary hormone deficiency type 3—c.1018C>T, p.Pro340Ser (LHX3), absorptive hypercalciuria—c.2535_2537 (rs767527947, ADCY10), Alström syndrome—c.8380C>G, p.Gln2794Glu (ALMS1), MEN type IV—rs755225286 (CDKN1B), and Wolman disease/cholesteryl ester storage disease—c.894G>A (LIPA).
After excluding incidental findings, the cohort with identified variants was reduced to 64 children (38.79% of the total number of examined children), in whom 96 pathogenic or likely pathogenic variants were identified in 61 genes (ABCC8, ADCY3, ADNP, ADRB2, ALMS1, ANKRD17, ARID1B, ASH1L, AVPR2, BAP1, BBS1, BBS10, CEP290, CREB3L3, CREBBP, CYFIP2, DYRK1B, ENPP1, FAT1, FGFR1, GCK, GNAS, GPR12, KCNJ11, KCNJ15, KIDINS220, KSR2, LEP, LEPR, LIPE, MAPK8IP1, MC3R, MC4R, METTL5, MLC1, MYT1L, NAA10, NEXMIF, NTRK2, ODC1, PACS1, PCSK1, PDE11A, PDE4D, PHIP, PLIN1, POMC, RPL13, SIM1, SLC2A2, SOS1, SPEN, SPTAN1, STAG1, TNPO2, TRAPPC9, TRIP12, TUB, WDR11, WFS1, ZMYND11, three large deletions, and one duplication). Variants in three genes—ADCY3, GCK, and POMC—co-occurred with autosomal dominant mutations in key genes associated with both diabetes and obesity.
The identified pool of genes can be categorized into three groups (Figure 1):
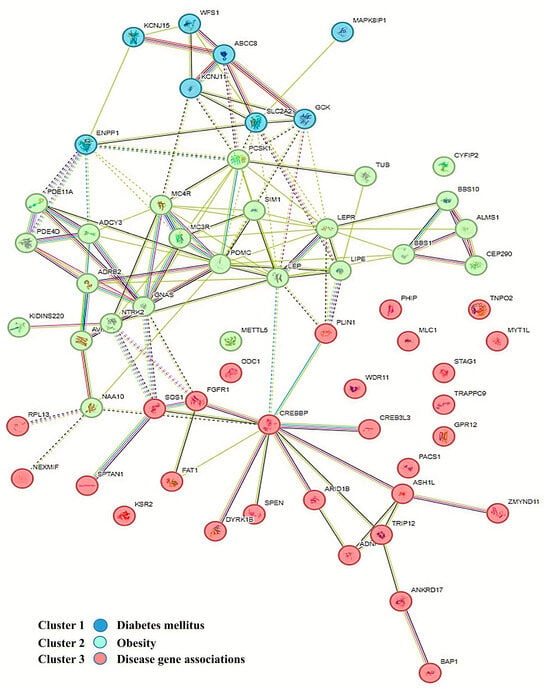
Figure 1.
Network illustrating the clustering of protein products of genes associated with diabetes, obesity, and rare syndromes, based on genotype–phenotype correlation databases and using the k-means clustering algorithm in the STRING version 10 software.
- Associated with obesity;
- Associated with diabetes and insulin resistance;
- Associated with other comorbid conditions, typically intellectual developmental disorders.
During screening for glucose metabolism disorders in our patient cohort, normoglycemia was observed in 80% of cases, while 13% of patients exhibited impaired fasting glucose or impaired glucose tolerance. Type 2 diabetes mellitus (T2DM) was confirmed in 7% of patients. To differentiate between autoimmune and non-autoimmune forms of diabetes, specific pancreatic autoantibodies (anti-GAD, anti-insulin, ICA, and IA2 autoantibodies) were assessed in all patients. The autoantibody titers were within the reference range in all cases, suggesting a non-autoimmune etiology and supporting the diagnosis of T2DM.
Dyslipidemia was identified in 42% of cases based on national clinical guidelines. Non-alcoholic fatty liver disease (NAFLD), manifesting as hepatic steatosis, was diagnosed in 45% of patients, and 25% had steatohepatitis. The remaining 30% of patients had normal liver enzyme levels and no abnormalities were detected on ultrasound examination.
Calcium and phosphate levels, along with parathyroid hormone (PTH) and calcitonin, were assessed in patients with suspected pseudohypoparathyroidism. All patients had elevated PTH levels and increased calcitonin concentrations. In rare cases, calcium levels were within the reference range at the time of examination; however, most patients exhibited hypocalcemia and hyperphosphatemia. Additionally, patients with pseudohypoparathyroidism exhibited TSH resistance, characterized by elevated TSH levels with normal free T4 concentrations. These patients were treated with calcitriol and levothyroxine sodium.
Kidney ultrasound was performed in this patient subgroup to detect renal microcalcifications, identifying renal microliths in 75% of cases [5].
Thyroid function was also assessed in patients with other forms of obesity. Euthyroidism was observed in 92% of cases, while subclinical hypothyroidism (TSH < 10 mIU/L) was diagnosed in 8% of cases. Levothyroxine sodium therapy was not indicated for these patients due to the mild nature of thyroid dysfunction.
Serum 25-hydroxyvitamin D levels were measured in all patients. Vitamin D deficiency of varying severity was diagnosed in 87% of cases, and cholecalciferol supplementation was prescribed to restore adequate vitamin D levels.
The first group included 29 patients (43.94%), in whom 36 pathogenic/likely pathogenic variants were identified in 21 genes, as well as two large chromosomal duplications/deletions on chromosomes 17 and 15, respectively (Table 2). The second group included 7 patients (13.64%) with 11 pathogenic/likely pathogenic variants identified in 9 genes (Table 3). The third group included 28 patients (42.42%) with 36 pathogenic/likely pathogenic variants identified in 34 genes, as well as two large chromosomal deletions on chromosomes 6 and 22 (Table 4).

Table 2.
Nucleotide sequence variations in genes associated with obesity.

Table 3.
Nucleotide sequence variations in genes associated with diabetes mellitus and insulin resistance.

Table 4.
Nucleotide sequence variations in genes associated with rare syndromes.
Recessive forms of severe obesity were identified, caused by homozygous or compound heterozygous mutations in the following genes: LEP (leptin), LEPR (leptin receptor), BBS1 and BBS10 (Bardet–Biedl syndrome), and POMC (pro-opiomelanocortin). These genes are well-studied, and their roles in the development of severe obesity in children are well-established. Approximately half of the identified variants had not been previously reported in the literature (Table 1). Heterozygous carriage of recessive mutations was observed in the ADCY3 (adenylate cyclase 3), CEP290 (centrosomal protein), and TUB (Tubby-like protein) genes, which are involved in obesity pathogenesis. However, no second pathogenic variant was detected. Variants were identified in the following genes: MC3R and MC4R (neuronal melanocortin receptors), DYRK1B (dual-specificity tyrosine-phosphorylation-regulated kinase), GPR12 (G-protein-coupled receptor 12), SIM1 (transcription factor), GNAS (stimulatory G-protein alpha subunit), NTRK2 (neurotrophic factor receptor), and KSR2 (kinase suppressor of Ras 2). These variants are associated with dominant forms of obesity in patients with a family history of the condition. Additionally, a previously unreported structural variation, a large deletion on chromosome 15, was identified with approximate boundaries chr15:22786711-28720475 (15q11.2-q13.1), spanning 5,933,764 base pairs. This deletion includes exons 1–5 of the NIPA1 gene and fully encompasses the genes MKRN3, MAGEL2, imprinted genes NDN and SNRPN, and UBE3A, GABRB3, GABRA5, OCA2, and HERC2. Heterozygous deletions in the 15q11.2-q13 region with loss of the paternal copy have been described in Prader–Willi syndrome. A large duplication in a heterozygous state on chromosome 17 was also identified, with approximate boundaries chr17:6819193-7498210, spanning 679,017 base pairs. This duplication includes the genes TEKT1, ALOX12P2, ALOX12-AS1, RNASEK, C17orf49, MIR497HG, MIR195, MIR497, BCL6B, SLC16A13, SLC16A11, CLEC10A, ASGR2, RPL7AP64, ASGR1, DLG4, ACADVL, MIR324, DVL2, PHF23, GABARAP, CTDNEP1, ELP5, CLDN7, RNA, SLC2A4, YBX2, EIF5A, GPS2, NEURL4, ACAP1, KCTD11, TMEM95, TNK1, PLSCR3, TMEM256, NLGN2, SPEM1, SPEM2, SPEM3, TMEM102, FGF11, CHRNB1, ZBTB4, and SLC35G6. Duplications of this region with similar sizes have been described as pathogenic or likely pathogenic in the Decipher database in patients with developmental delays, obesity, short stature, and other phenotypic features. All protein products of the identified genes cluster into two subgroups: one directly involved in the development of obesity, and the other involved in lipolysis regulation in adipocytes (Figure 2).
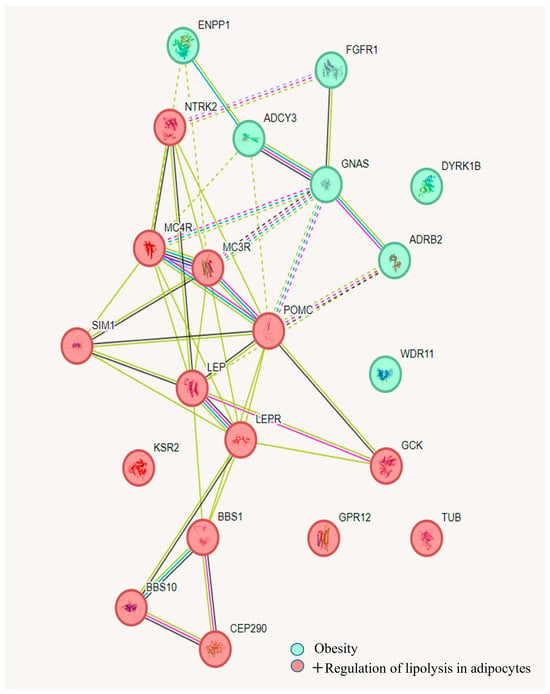
Figure 2.
Network illustrating the clustering of protein products of genes associated with obesity and the regulation of lipolysis in adipocytes, based on gene-phenotype correlation databases and analyzed using k-means clustering algorithms in the String 10 software.
Pathogenic variants were also identified in genes associated with MODY (maturity-onset diabetes of the young), including ABCC8, GCK, KCNJ11, and WFS1. Variants were additionally found in genes linked to nephrogenic diabetes insipidus type 1 (AVPR2), the SLC2A2 gene encoding the GLUT2 protein, which plays a key role in glucose metabolism, and the MAPK8IP1 gene encoding a regulator of pancreatic beta-cell function (Table 4). In one case, a mutation in the ABCC8 gene co-occurred with a pathogenic variant in the POMC gene, while, in another case, a pathogenic variant in the KCNJ11 gene was found alongside a mutation in the ADCY3 gene, which encodes adenylate cyclase type 3, a protein that converts ATP to cAMP and is associated with obesity. It is known that insulin exerts a dominant anabolic effect on adipocytes by reducing the circulating concentrations of various metabolic components, stimulating glucose uptake by tissues, suppressing the release of fatty acids from adipose tissue, inhibiting ketone production in the liver, and promoting fat and glycogen storage. Accordingly, elevated insulin levels are predictably associated with weight gain [6]. Figure 3 illustrates the clustering of these genes into two subclasses: those associated with type 2 diabetes and those interacting with vasopressin and corticotropin-releasing factor. In the adenohypophysis, vasopressin, together with corticotropin-releasing hormone, stimulates the secretion of adrenocorticotropic hormone (ACTH), which is involved in stimulating lipolysis. This further suggests the involvement of the identified gene variants in the development of obesity in children.
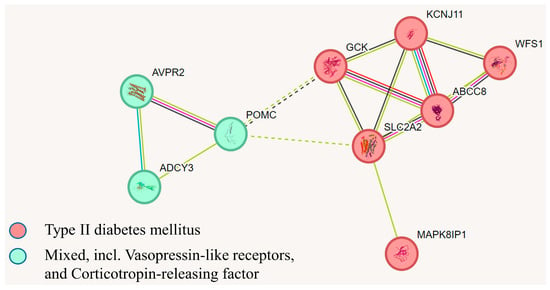
Figure 3.
A network demonstrating the clustering of protein products of genes associated with type 2 diabetes and their interactions with vasopressin and corticotropin-releasing factors, according to gene-phenotype correlation databases, based on k-means algorithms using the String 10 software.
The third group of nucleotide sequence variations in genes associated with rare syndromes is characterized as the most heterogeneous, comprising the largest number of distinct genes, primarily linked to intellectual developmental disorders (Table 4). Two cases of lipodystrophy warrant particular attention, both accompanied by various metabolic disorders, including insulin resistance, specific diabetes mellitus (lipoatrophic diabetes), hepatic steatosis, steatohepatitis, lipid metabolism disorders, and arterial hypertension. Both cases were reported for the first time.
Additionally, five patients in the third group harbored multiple molecular defects: three patients had pathogenic variants in two genes, one patient had variants in three genes, and another in four genes. This underscores the complexity of the genetic architecture of obesity associated with intellectual disabilities.
Information on the prevalence and clinical significance of the identified variants according to ACMG criteria and in silico pathogenicity assessment is presented in Table 5.

Table 5.
Prevalence frequencies and clinical significance of identified variants according to ACMG criteria and in silico pathogenicity assessment in predictive programs.
The identification of a large number of previously unreported variants emphasizes the distinctiveness of the genetic architecture of severe obesity in Russian children and highlights the need for functional studies to determine their clinical significance. This study represents the first attempt to summarize and systematize the results of whole-exome sequencing in a sufficiently large cohort of children with severe forms of obesity. Further analysis and detailed characterization of the clinical course of the disease are planned, considering the identified gene variants, family history, ethnic background, and region of residence. Additionally, dynamic monitoring of patients and their families will be performed using advanced, clinical genetic and molecular tools.
4. Discussion
Our study identified three groups of children with severe obesity, whose condition is likely associated with different pathogenic mechanisms. This stratification facilitates differentiation between syndromic/monogenic forms of obesity, primarily represented in the first group of children with mutations in obesity-associated genes, and the second group, where the disease likely developed due to carbohydrate metabolism disorders or complex molecular interactions of pathogenic gene variants related to lipid and carbohydrate metabolism. The third, heterogeneous group comprises children whose obesity appears to have developed due to severe disruptions in genes associated with higher nervous system development, congenital anomalies, rare syndromes, and lipid metabolism disorders. Our study identified a significant number of previously unreported variants, further increasing the value of the obtained data. Future research can focus on these variants to uncover previously unknown complex pathogenic pathways of obesity in rare syndromes or conditions that were not previously associated with severe obesity in children.
The results highlight the complexity of interpreting genetic testing results in clinical practice. Genetic obesity can be classified into two forms: syndromic, which is typically associated with chromosomal abnormalities (e.g., Prader–Willi, Fragile X, Alström, Cohen, Down syndrome, and pseudohypoparathyroidism), and non-syndromic, which includes both monogenic and polygenic obesity [7]. Monogenic obesity results from alterations in a single gene sequence or changes in chromosomal copy number due to small or large chromosomal deletions or duplications, typically inherited in a Mendelian manner. A history of early-onset obesity in children under the age of 10 serves as a basis for conducting molecular genetic testing, the choice of which depends on clinical manifestations and family history. The types of identified variants vary and include single nucleotide substitutions leading to amino acid sequence changes, substitutions resulting in protein loss of function due to frameshifts, premature stop codons, or splicing disruptions. Structural rearrangements, large deletions, or duplications affecting multiple genes, present only in the proband, can also underlie obesity [6,8]. Many of the variants identified in our study, in genes with a proven association with obesity, align with the characteristics of monogenic and syndromic forms, as well as those associated with insulin resistance disorders. On the other hand, patients with cognitive impairments represent a broad group that requires increased attention due to the established link between obesity and intellectual spectrum disorders [9].
Various forms of nonsyndromic monogenic childhood obesity exist and occur in less than 2% of children [10]. As morbid obesity is a heterogeneous condition, severe forms of the disease, including nonsyndromic early-onset forms, are likely caused by highly penetrant rare genetic variants [11]. The variants of unknown significance identified in our study, not previously reported in the literature, could potentially be associated with obesity due to a pathogenic effect. This effect could arise from high penetrance in heterozygous carriers.
Most studies have focused on the MC4R, POMC, LEP, LEPR, and BBS genes. Mutations in the melanocortin-4 receptor (MC4R) gene are the most common, accounting for approximately 4–6% of monogenic obesity cases. Mutations in the leptin receptor (LEPR) gene account for approximately 3% of cases. Mutations in other genes, such as POMC (pro-opiomelanocortin), LEP (leptin), PCSK1 (proprotein convertase subtilisin/kexin type 1), NTRK2 (neurotrophic receptor tyrosine kinase type 2), BDNF (brain-derived neurotrophic factor), and SIM1 (single-minded family bHLH transcription factor 1), are even rarer causes of monogenic obesity [12].
In recent years, the widespread use of next-generation sequencing technologies for investigating the causes of monogenic forms of obesity has led to the identification of numerous variants of unknown clinical significance, whose relevance remains unclear [13,14]. Many authors have studied monogenic forms of obesity by analyzing a limited number of genes using custom gene panels. For example, Nordang et al. (2017) analyzed a Norwegian cohort of patients with severe obesity, including children under 12 years of age. Their gene panel included LEP, LEPR, MC4R, PCSK1, and POMC, and they identified four cases (0.8%) with pathogenic or likely pathogenic variants in the MC4R gene [15].
In a Turkish study involving 105 children with early-onset obesity and analysis of 41 genes, approximately 10.5% of the variants were found in the SIM1, POMC, PCSK1, MC4R, and LEPR genes [16]. Additionally, in a study of 25 patients with obesity from Guadeloupe, five heterozygous variants were identified in the MC4R, NTRK2, SH2B1, and SIM1 genes, with a frequency of approximately 10% [17]. A study in Italy that screened 209 patients with obesity for mutations in the MC4R, LEP, and LEPR genes identified only one novel pathogenic frameshift variant in the MC4R gene, which disrupted gene signaling [18]. The highest prevalence of monogenic obesity was observed in a Pakistani population, where 30% of children with obesity carried pathogenic variants in the LEP, LEPR, and MC4R genes [19].
In 2023, Mohammed et al. conducted targeted sequencing of a panel of 52 genes (ADCY3, ALMS1, ARL6, BBIP1, BBS1, BBS10, BBS12, BBS2, BBS4, BBS5, BBS7, BBS9, BDNF, CEP290, CFAP418, CPE, CUL4B, DYRK1B, GNAS, IFT172, IFT27, IFT74, KSR2, LEP, LEPR, LZTFL1, MAGEL2, MC3R, MC4R, MCHR1, MKKS, MKS1, MRAP2, NCOA1, NR0B2, NTRK2, PCSK1, PHF6, POMC, PPARG, RAB23, RAI1, SDCCAG8, SH2B1, SIM1, TMEM67, TRIM32, TTC8, TUB, UCP3, VPS13B, WDPCP) in 243 patients with severe early-onset obesity (ages from 3 months to 10 years) observed at the Endocrinology Clinic at Sidra Medicine in Qatar. They identified 30 rare variants potentially associated with obesity in 36 of the 243 children across 15 candidate genes (LEP, LEPR, POMC, MC3R, MC4R, MRAP2, SH2B1, BDNF, NTRK2, DYRK1B, SIM1, GNAS, ADCY3, RAI1, and BBS2). Twenty-three of the identified variants had not been previously described in the literature at the time of this study. In this cohort, variants in the MC4R gene were the most common cause of obesity, with the variant c.485C>T, p.T162I being the most frequently observed mutation in five patients [20].
In Chandigarh, India, next-generation sequencing in children with obesity identified one pathogenic variant in the MC4R gene, one likely pathogenic variant each in the LEPR, NTRK2, and LEP genes, as well as variants of uncertain significance in the POMC and LEPR genes [12].
Interesting findings were reported by the group led by Petra Lloyd, who, in 2022, published results of a custom-designed panel for targeted exome sequencing in genes previously associated with copy number variations (CNVs) linked to severe childhood obesity. The authors identified 13 rare heterozygous variants of uncertain significance in 12 genes in 11 children. Two rare missense variants (p.Pro405Arg and p.Tyr232Cys) were identified in the SORCS1 gene, which is highly expressed in the brain and has been associated with diabetes risk. Four rare variants were identified in genes within the 16p11.2 region (a frameshift variant in TAOK2 and missense variants in SEZ6L2, ALDOA, and KIF22), and three rare missense variants were found in the 22q11.21 region in the AIFM3, ARVCF, and KLHL22 genes.
Our study presents a range of novel findings, including the identification of 42 variants not previously reported in the literature. A duplication on chromosome 17 revealed two gene clusters, one of which is associated with the regulation of lipolysis in adipocytes. This cluster includes the genes ENPP1, ADCY3, FGFR1, GNAS, ADRB2, DYRK1B, and WDR11. Additionally, a previously unreported large deletion on chromosome 15 was identified, encompassing the genes NIPA1, MKRN3, and MAGEL2, the imprinted genes NDN and SNRPN, as well as UBE3A, GABRB, GABRA5, OCA2, and HERC2, which is of particular scientific interest. The genes NDN, SNRPN, and UBE3A are known for their association with Prader–Willi syndrome; GABRB and GABRA5 are associated with encephalopathies; OCA2 and HERC2 are linked to skin pigmentation. In two patients, two distinct pathogenic variants in the ABCC8 gene were identified, consistent with the pathogenic model of obesity development under insulin resistance induced by hyperinsulinemia. In one child, sequencing revealed two likely pathogenic variants not previously described. One of these variants, ADCY3 c.3380C>G, is involved in the development of obesity, while the other, KCNJ11 c.628A>G, is associated with type 2 diabetes and neonatal diabetes. A study published in Nature Genetics reported a direct association between pathogenic variants in the ADCY3 gene and severe obesity in children from consanguineous Pakistani families [21], which further supports the significance of our identified variant. The combination of two previously undescribed variants located in conserved coding regions of key genes involved in energy homeostasis and receptor system regulation suggests a potential synergistic pathogenic effect. This combination may contribute to an increased risk of early-onset morbid obesity in infancy, especially given that whole-exome sequencing did not identify any other significant pathogenic variants in the patient. In one patient from the second group, nephrogenic diabetes insipidus, obesity, pronounced lentiginosis, and hypogonadotropic hypogonadism were diagnosed. Exome sequencing revealed a previously described hemizygous variant, c.262G>T, in exon 3 of the AVPR2 gene, leading to an amino acid substitution of valine to leucine at position 88 of the protein. Vasopressin is primarily known for its role in water reabsorption through urine concentration. However, adipose tissue is also a source of metabolic water, raising the possibility that vasopressin may contribute to fat accumulation [22]. Given the impaired function of the vasopressin receptor caused by the identified pathogenic variants, disruption of these mechanisms in individuals with nephrogenic diabetes insipidus can be hypothesized. This, in part, may suggest a potential link between obesity and nephrogenic diabetes in the context of AVPR2 gene mutations.
An intriguing finding concerns another patient from the second group, who was diagnosed with a combination of diabetes mellitus, severe obesity, optic nerve atrophy, and possibly diabetes insipidus. The patient’s brother has diabetes mellitus, obesity, and sensorineural hearing loss. Whole-exome sequencing identified two causal variants in the WFS1 (wolframin) gene, found in a compound heterozygous state. One of these variants, c.1943G>A in exon 8, in a heterozygous state, has been previously described in the literature. Genome-wide association studies have identified WFS1 variants associated with type 2 diabetes (T2D) and metabolic traits [23]. Functional studies on model animals demonstrated that mice carrying WFS1 mutations exhibit reduced insulin response and increased cellular stress due to heightened sensitivity to a high-fat diet [24].
Heterozygous mutations in the WFS1 gene have been associated with insulin-independent diabetes mellitus (OMIM:125853), Wolfram-like syndrome (OMIM:614296), deafness (OMIM:600965), and cataracts (OMIM:116400), following an autosomal dominant inheritance pattern. These findings strongly support the identification of causal variants in the patient, correlating with their described phenotypes.
The results of our study suggest that the pathogenesis of morbid obesity in Russian children is complex and exhibits diverse genetic architecture. The numerous variants identified in our study, many of unknown significance or probable pathogenicity, point to unexplored factors contributing to obesity.
5. Conclusions
Molecular genetic analysis of Russian children with morbid obesity has revealed several previously unreported genetic variants potentially associated with comorbid conditions such as obesity, insulin resistance, and syndromic forms. These findings warrant further functional studies, which may provide insights into the intricate genetic architecture of obesity. Obesity is characterized by a multifaceted metabolic imbalance that affects the regulation of energy balance, glucose homeostasis, lipid metabolism, and interactions between the central and peripheral nervous systems and adipose tissue. Many patients with diabetes and obesity meet the criteria for metabolic syndrome, which includes central obesity, dyslipidemia, and insulin resistance. However, it is often unclear which genes and causal factors contribute to the risk of obesity in such patients, as pathogenic variants are not always detected in the suspected genes. Our study brings us closer to understanding this problem. The results may serve as a guide for improving existing panels for targeted sequencing. Furthermore, previously unreported variants may help bridge the gaps in our understanding of the mechanisms underlying insulin resistance in childhood morbid obesity.
Author Contributions
Conceptualization: I.R.M. and R.I.K.; methodology, R.R.S.; formal analysis: B.I.Y., D.A.K., R.M.G. and O.V.V.; investigation: I.R.M. and R.I.K.; resources: N.G.M. and O.V.V.; data curation: V.A.P.; writing—original draft preparation: I.R.M. and R.I.K.; writing—review and editing: B.I.Y., I.R.M., R.I.K. and R.R.S.; visualization: B.I.Y.; supervision: N.G.M.; project administration: N.G.M. and V.A.P.; funding acquisition: N.G.M. and V.A.P. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Ministry of Science and Higher Education of the Russian Federation (agreement No. 075-15-2022-310 from 20 April 2022).
Institutional Review Board Statement
This study was approved by the Bioethics Committee of the Endocrinology Research Centre (protocol №18, dated 10 October 2022).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Vasyukova, O.V. Obesity in Children and Adolescents: Diagnosis Criteria. Obes. Metab. 2019, 16, 70–73. [Google Scholar] [CrossRef]
- WHO Latest Data Shows Southern European Countries Have Highest Rate of Childhood Obesity. Available online: https://dev-cms.who.int/europe/news/item/24-05-2018-latest-data-shows-southern-european-countries-have-highest-rate-of-childhood-obesity (accessed on 20 January 2025).
- Dykens, E.M.; Maxwell, M.A.; Pantino, E.; Kossler, R.; Roof, E. Assessment of hyperphagia in Prader-Willi syndrome. Obesity 2007, 15, 1816–1826. [Google Scholar] [CrossRef] [PubMed]
- Richards, S.; Aziz, N.; Bale, S.; Bick, D.; Das, S.; Gastier-Foster, J.; Grody, W.W.; Hegde, M.; Lyon, E.; Spector, E.; et al. Standards and Guidelines for the Interpretation of Sequence Variants: A Joint Consensus Recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet. Med. 2015, 17, 405–424. [Google Scholar] [CrossRef] [PubMed]
- Kopytina, D.A.; Vasyukova, O.V.; Salakhov, R.R.; Okorokov, P.L.; Kopytina, E.V.; Nagaeva, E.V.; Khusainova, R.I.; Minniakhmetov, I.R.; Popov, S.V.; Bezlepkina, O.B.; et al. Identification of Novel Pathogenic Variants in the Gnas Gene in Children with Morbid Obesity and Pseudohypoparathyroidism. Obes. Metab. 2024, 21, 412–424. [Google Scholar] [CrossRef]
- Ludwig, D.S.; Ebbeling, C.B. The Carbohydrate-Insulin Model of Obesity: Beyond “Calories in, Calories Out”. JAMA Intern. Med. 2018, 178, 1098–1103. [Google Scholar] [CrossRef]
- Singh, R.K.; Kumar, P.; Mahalingam, K. Molecular Genetics of Human Obesity: A Comprehensive Review. Comptes Rendus Biol. 2017, 340, 87–108. [Google Scholar] [CrossRef]
- Keller, M.; Svensson, S.I.A.; Rohde-Zimmermann, K.; Kovacs, P.; Böttcher, Y. Genetics and Epigenetics in Obesity: What Do We Know so Far? Curr. Obes. Rep. 2023, 12, 482–501. [Google Scholar] [CrossRef]
- Martins, L.B.; Monteze, N.M.; Calarge, C.; Ferreira, A.V.M.; Teixeira, A.L. Pathways Linking Obesity to Neuropsychiatric Disorders. Nutrition 2019, 66, 16–21. [Google Scholar] [CrossRef]
- Kelly, A.S.; Barlow, S.E.; Rao, G.; Inge, T.H.; Hayman, L.L.; Steinberger, J.; Urbina, E.M.; Ewing, L.J.; Daniels, S.R. Severe Obesity in Children and Adolescents: Identification, Associated Health Risks, and Treatment Approaches: A Scientific Statement from the American Heart Association. Circulation 2013, 128, 1689–1712. [Google Scholar] [CrossRef]
- Serra-Juhé, C.; Martos-Moreno, G.; Bou de Pieri, F.; Flores, R.; Chowen, J.A.; Pérez-Jurado, L.A.; Argente, J. Heterozygous Rare Genetic Variants in Non-Syndromic Early-Onset Obesity. Int. J. Obes. 2020, 44, 830–841. [Google Scholar] [CrossRef]
- George, A.; Navi, S.; Nanda, P.M.; Daniel, R.; Anand, K.; Banerjee, S.; Panigrahi, I.; Dayal, D. Clinical and Molecular Characterisation of Children with Monogenic Obesity: A Case Series. Pediatr. Endocrinol. Diabetes Metab. 2024, 30, 104–109. [Google Scholar] [CrossRef] [PubMed]
- Kernohan, K.D.; Boycott, K.M. The Expanding Diagnostic Toolbox for Rare Genetic Diseases. Nat. Rev. Genet. 2024, 25, 401–415. [Google Scholar] [CrossRef] [PubMed]
- Roberts, K.J.; Chaves, E.; Ariza, A.J.; Thaker, V.V.; Cho, C.C.; Binns, H.J. Exploring Genetic Testing for Rare Disorders of Obesity: Experience and Perspectives of Pediatric Weight Management Providers. Child. Obes. 2024, 20, 451–458. [Google Scholar] [CrossRef]
- Nordang, G.B.N.; Busk, Ø.L.; Tveten, K.; Hanevik, H.I.; Fell, A.K.M.; Hjelmesæth, J.; Holla, Ø.L.; Hertel, J.K. Next-Generation Sequencing of the Monogenic Obesity Genes LEP, LEPR, MC4R, PCSK1 and POMC in a Norwegian Cohort of Patients with Morbid Obesity and Normal Weight Controls. Mol. Genet. Metab. 2017, 121, 51–56. [Google Scholar] [CrossRef]
- Akıncı, A.; Turkkahraman, D.; Tekedereli, I.; Ozer, L.; Evren, B.; Şahin, I.; Kalkan, T.; Curek, Y.; Camtosun, E.; Döğer, E.; et al. Novel Mutations in Obesity-Related Genes in Turkish Children with Non-Syndromic Early Onset Severe Obesity: A Multicentre Study. J. Clin. Res. Pediatr. Endocrinol. 2019, 11, 341–349. [Google Scholar] [CrossRef]
- Foucan, L.; Larifla, L.; Durand, E.; Rambhojan, C.; Armand, C.; Michel, C.T.; Billy, R.; Dhennin, V.; De Graeve, F.; Rabearivelo, I.; et al. High Prevalence of Rare Monogenic Forms of Obesity in Obese Guadeloupean Afro-Caribbean Children. J. Clin. Endocrinol. Metab. 2018, 103, 539–545. [Google Scholar] [CrossRef]
- Trevellin, E.; Granzotto, M.; Host, C.; Grisan, F.; De Stefani, D.; Grinzato, A.; Lefkimmiatis, K.; Pagano, C.; Rizzuto, R.; Vettor, R. A Novel Loss of Function Melanocortin-4-Receptor Mutation (MC4R-F313Sfs∗29) in Morbid Obesity. J. Clin. Endocrinol. Metab. 2021, 106, 736–749. [Google Scholar] [CrossRef]
- Saeed, S.; Bonnefond, A.; Manzoor, J.; Shabir, F.; Ayesha, H.; Philippe, J.; Durand, E.; Crouch, H.; Sand, O.; Ali, M.; et al. Genetic Variants in LEP, LEPR, and MC4R Explain 30% of Severe Obesity in Children from a Consanguineous Population. Obesity 2015, 23, 1687–1695. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, I.; Haris, B.; Al-Barazenji, T.; Vasudeva, D.; Tomei, S.; Al Azwani, I.; Dauleh, H.; Shehzad, S.; Chirayath, S.; Mohamadsalih, G.; et al. Understanding the Genetics of Early-Onset Obesity in a Cohort of Children from Qatar. J. Clin. Endocrinol. Metab. 2023, 108, 3201–3213. [Google Scholar] [CrossRef]
- Saeed, S.; Bonnefond, A.; Tamanini, F.; Mirza, M.U.; Manzoor, J.; Janjua, Q.M.; Din, S.M.; Gaitan, J.; Milochau, A.; Durand, E.; et al. Loss-of-Function Mutations in ADCY3 Cause Monogenic Severe Obesity. Nat. Genet. 2018, 50, 175–179. [Google Scholar] [CrossRef]
- Andres-Hernando, A.; Jensen, T.J.; Kuwabara, M.; Orlicky, D.J.; Cicerchi, C.; Li, N.; Roncal-Jimenez, C.A.; Garcia, G.E.; Ishimoto, T.; Maclean, P.S.; et al. Vasopressin Mediates Fructose-Induced Metabolic Syndrome by Activating the V1b Receptor. JCI Insight 2021, 6, e140848. [Google Scholar] [CrossRef] [PubMed]
- Fawcett, K.A.; Wheeler, E.; Morris, A.P.; Ricketts, S.L.; Hallmans, G.; Rolandsson, O.; Daly, A.; Wasson, J.; Permutt, A.; Hattersley, A.T.; et al. Detailed Investigation of the Role of Common and Low-Frequency WFS1 Variants in Type 2 Diabetes Risk. Diabetes 2010, 59, 741–746. [Google Scholar] [CrossRef] [PubMed]
- Ivask, M.; Volke, V.; Raasmaja, A.; Kõks, S. High-Fat Diet Associated Sensitization to Metabolic Stress in Wfs1 Heterozygous Mice. Mol. Genet. Metab. 2021, 134, 203–211. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).