Targeting p70S6K1 Inhibits Glycated Albumin-Induced Triple-Negative Breast Cancer Cell Invasion and Overexpression of Galectin-3, a Potential Prognostic Marker in Diabetic Patients with Invasive Breast Cancer
Abstract
1. Introduction
2. Materials and Methods
2.1. Bioinformatics
2.2. Generation of Glycated Albumin
2.3. MDA-MB-231 Cell Culture and Treatment
2.4. p70S6K1 Knockdown Using siRNA Technology
2.5. Cell Lysate Preparation and Western Blot Technology
2.6. Cell Invasion Assay
2.7. Oncology Protein Array
2.8. Statistical Analysis
3. Results
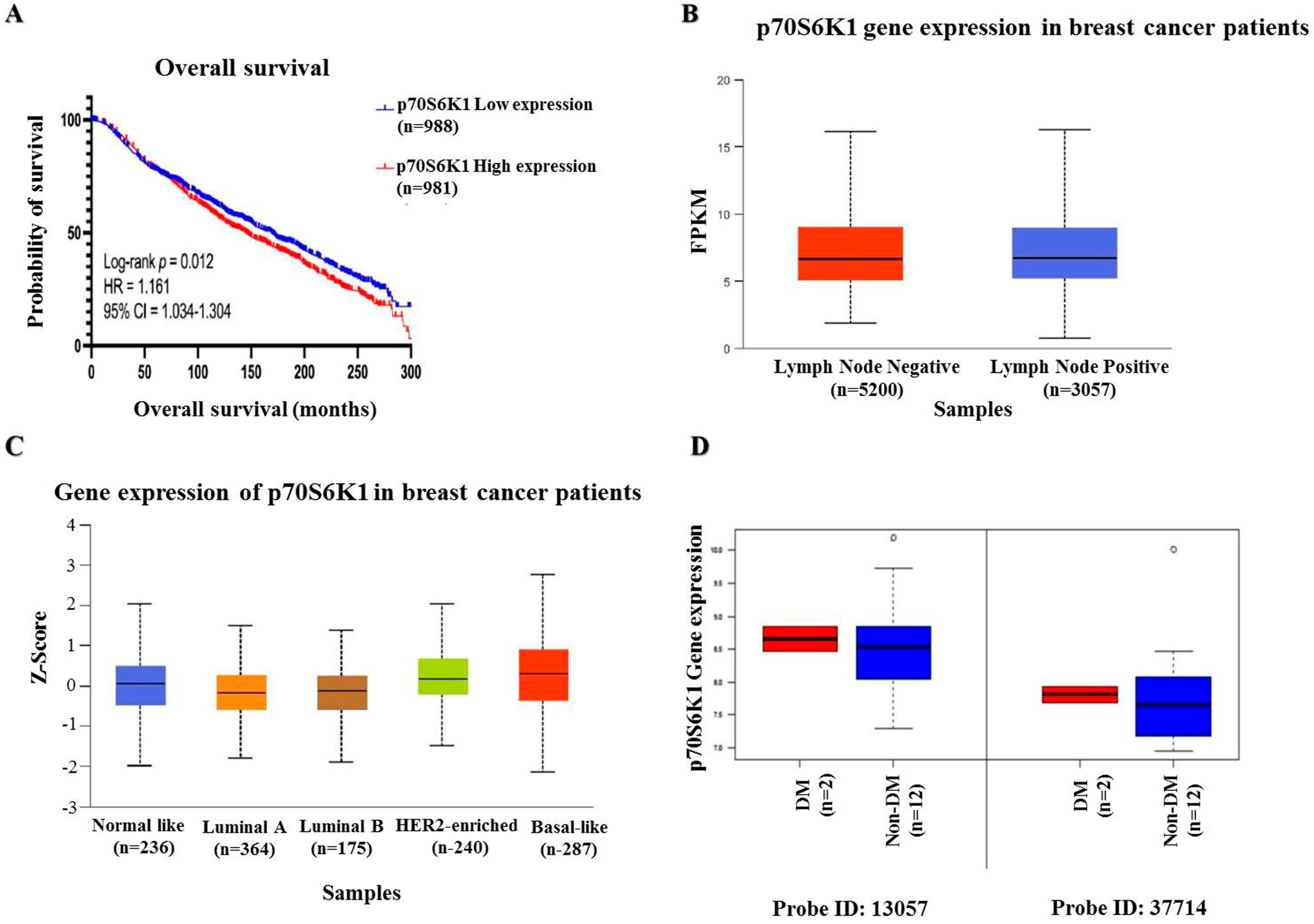
3.1. Prognostic Impact of p70S6K1 Expression Levels on BC Patient Overall Survival
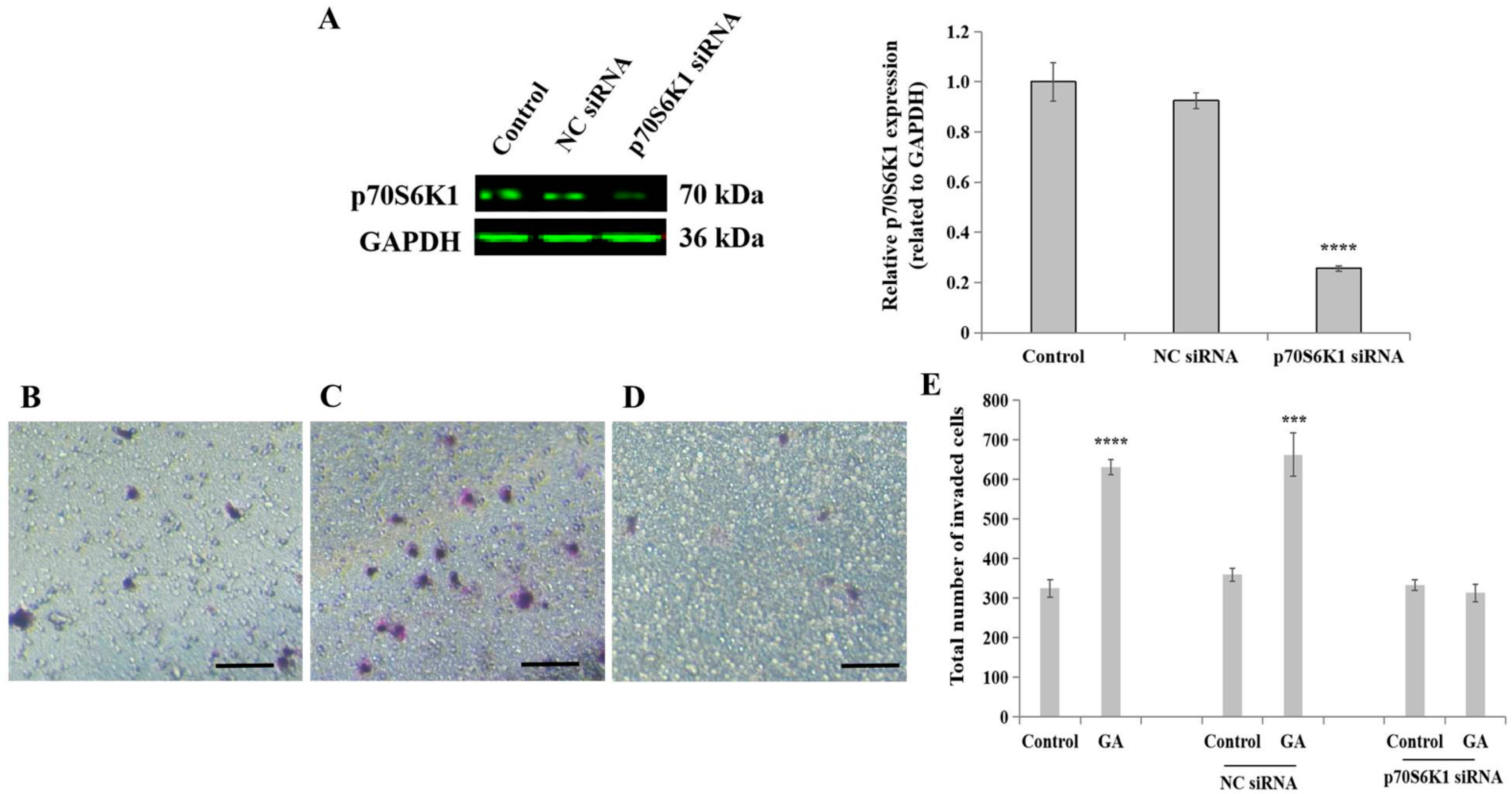
3.2. Knockdown of p70S6K1 Inhibits GA-Induced MDA-MB-231 Cell Invasion
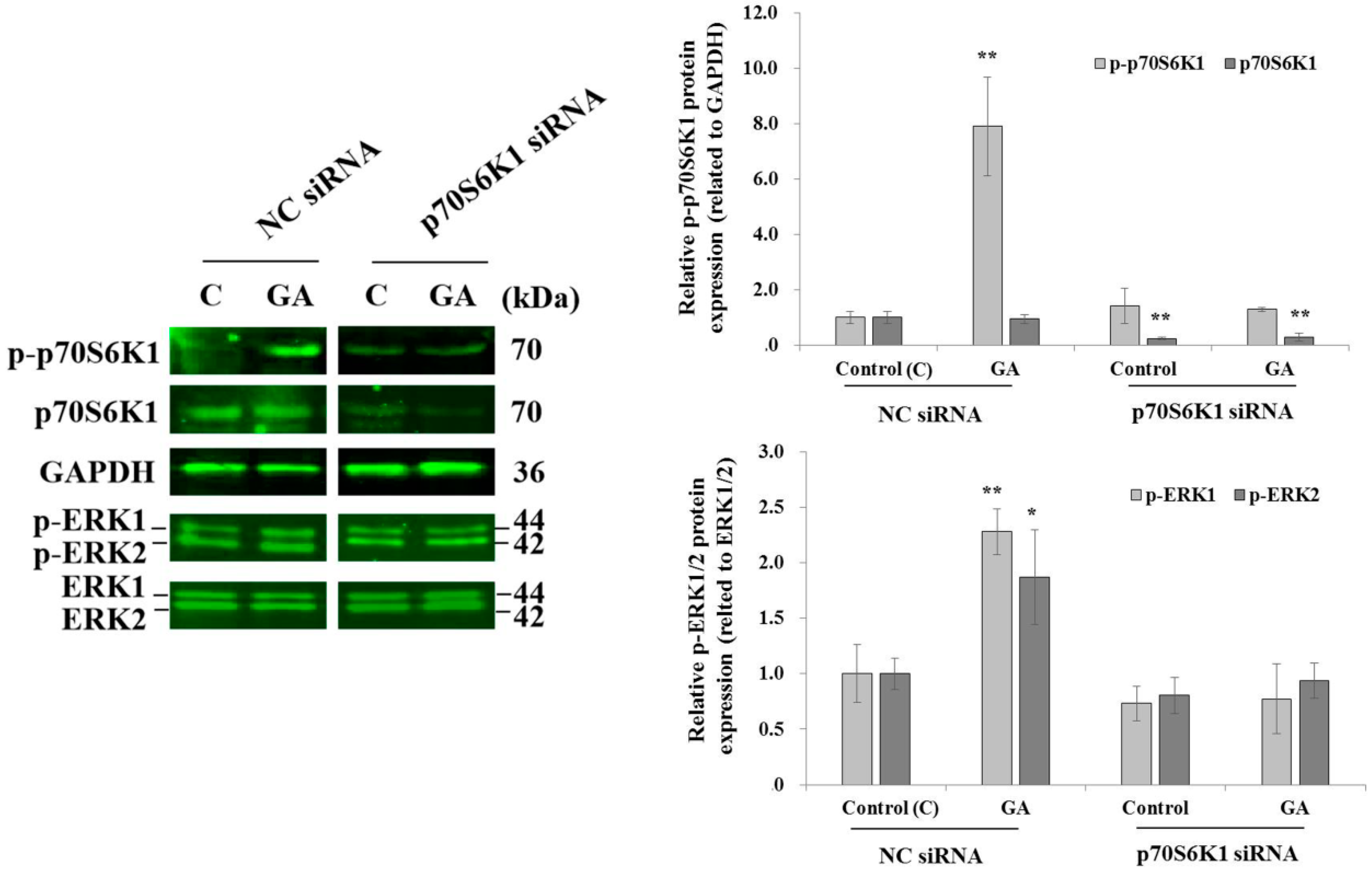
3.3. Knockdown of p70S6K1 Inhibits GA-Induced p70S6K1 and ERK1/2 Phosphorylation in MDA-MB-231 Cells
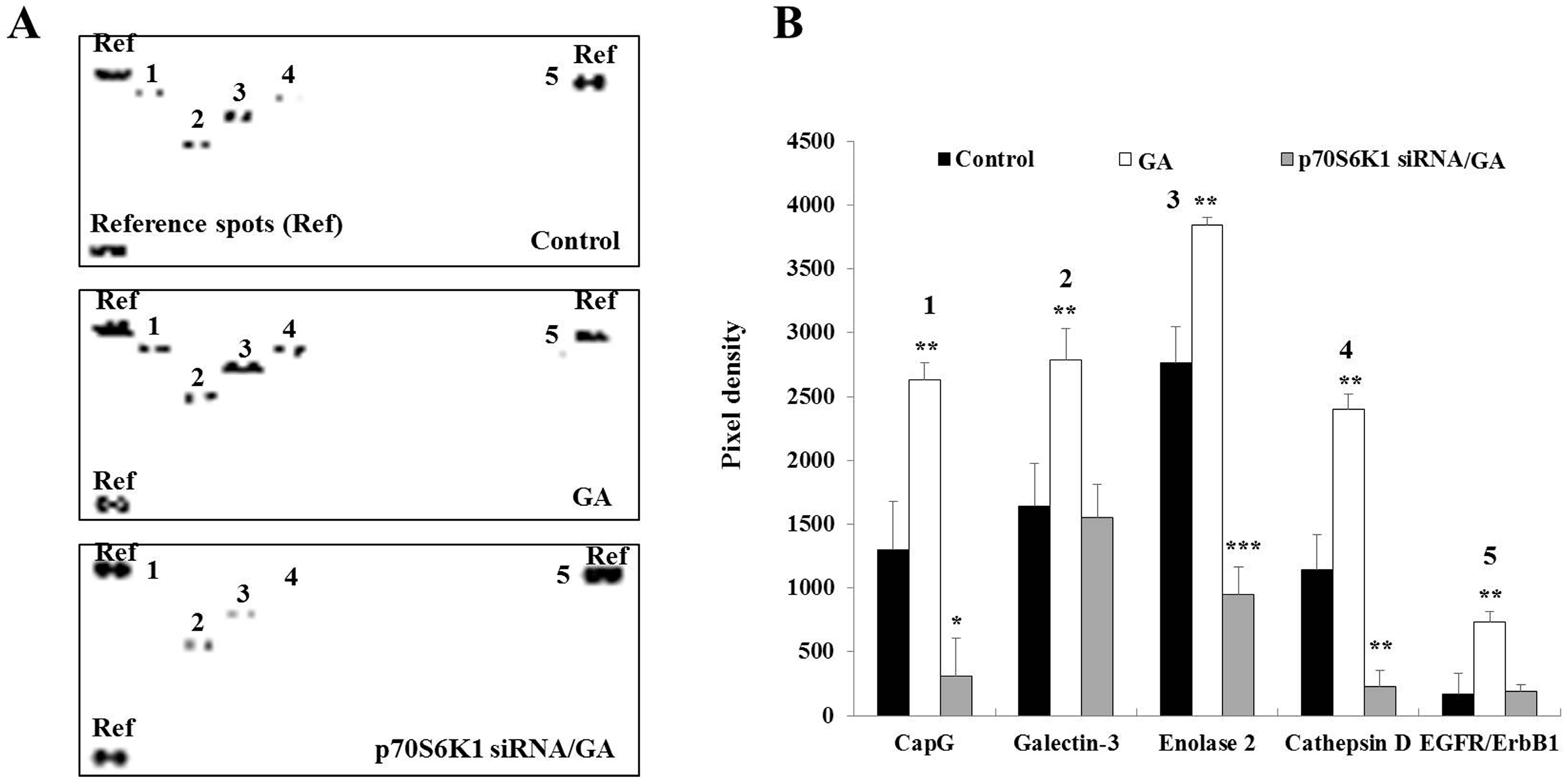
3.4. Knockdown of p70S6K1 Suppresses GA-Upregulated Cancer-Related Protein Expression in MDA-MB-231 Cells
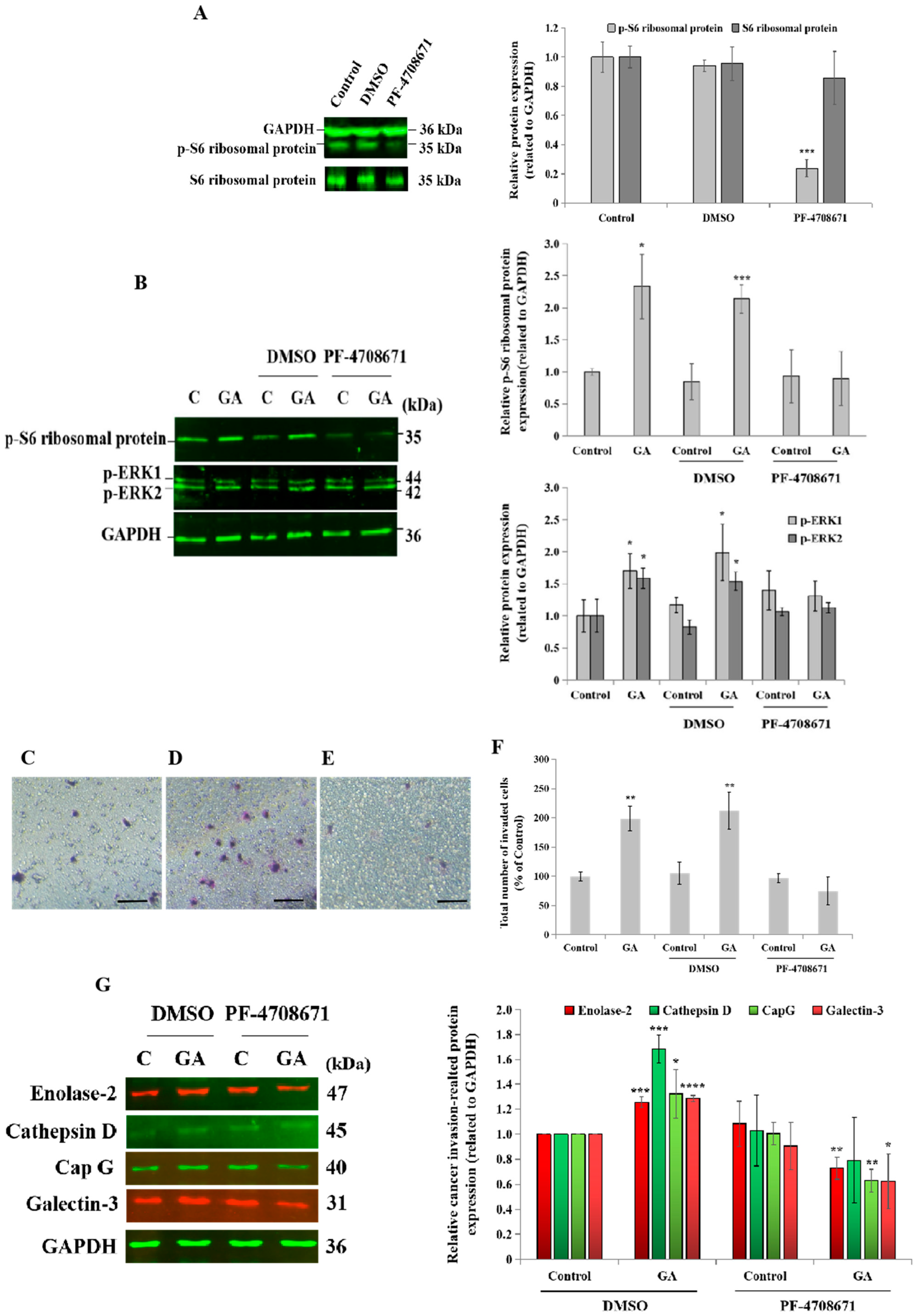
3.5. Blockade of p70S6K1 Pathway Using PF-4708671 Inhibits GA-Induced MDA-MB-231 Cell Invasion, Ribosomal Protein S6, ERK1/2 Phosphorylation, and Cancer-Related Protein Expression
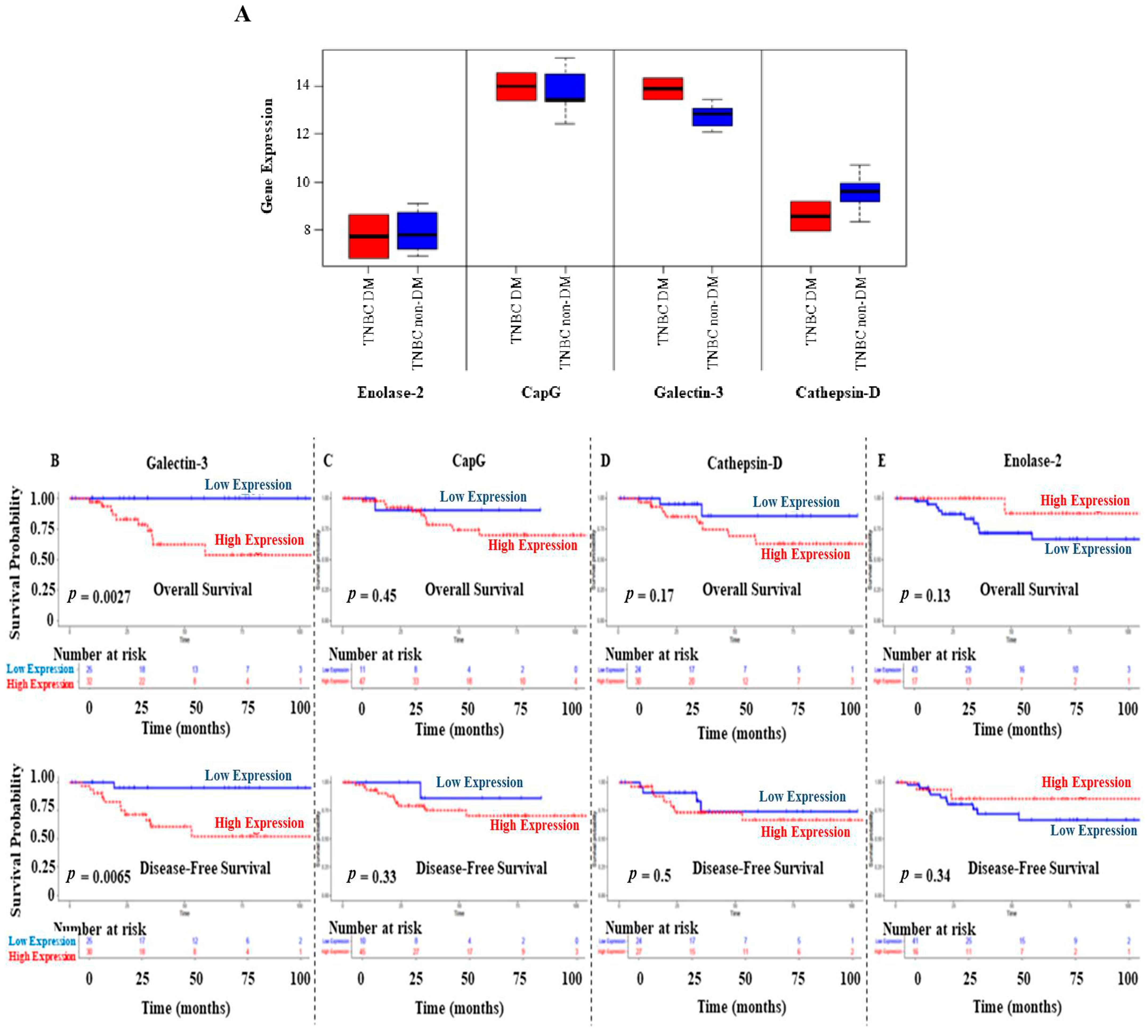
3.6. Prognostic Values of GA-Induced Cancer-Related Proteins on OS and DFS of BC Patients
4. Discussion
5. Conclusions and Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Antar, S.A.; Ashour, N.A.; Sharaky, M.; Khattab, M.; Ashour, N.A.; Zaid, R.T.; Roh, E.J.; Elkamhawy, A.; Al-Karmalawy, A.A. Diabetes mellitus: Classification, mediators, and complications; a gate to identify potential targets for the development of new effective treatments. Biomed. Pharmacother. 2023, 168, 115734. [Google Scholar] [CrossRef] [PubMed]
- Lu, X.; Xie, Q.; Pan, X.; Zhang, R.; Zhang, X.; Peng, G.; Zhang, Y.; Shen, S.; Tong, N. Type 2 diabetes mellitus in adults: Pathogenesis, prevention and therapy. Signal Transduct. Target. Ther. 2024, 9, 262. [Google Scholar] [CrossRef]
- Cuadros, D.F.; Li, J.; Musuka, G.; Awad, S.F. Spatial epidemiology of diabetes: Methods and insights. World J. Diabetes 2021, 12, 1042–1056. [Google Scholar] [CrossRef]
- Yee, L.D.; Mortimer, J.E.; Natarajan, R.; Dietze, E.C.; Seewaldt, V.L. Metabolic health, insulin, and breast cancer: Why oncologists should care about insulin. Front. Endocrinol. 2020, 11, 58. [Google Scholar] [CrossRef]
- Mao, X.; Omeogu, C.; Karanth, S.; Joshi, A.; Meernik, C.; Wilson, L.; Clark, A.; Deveaux, A.; He, C.; Johnson, T.; et al. Association of reproductive risk factors and breast cancer molecular subtypes: A systematic review and meta-analysis. BMC Cancer 2023, 23, 644. [Google Scholar] [CrossRef]
- Miller, M.E.; Bell, M.; Holland, P.; Ibrahim, V.; Jacobsen, M.S. The impact of race and glycemic control on triple negative breast cancer in type 2 diabetics. Cancer Epidemiol. Biomark. Prev. 2022, 31, 56–57, Abstract nr A069. [Google Scholar] [CrossRef]
- Vuger, A.T.; Šeparović, R.; Vazdar, L.P.; Pavlović, M.; Lepetić, P.; Šitić, S.; Bajić, Ž.; Šarčević, B.; Vrbanec, D. Characteristics and Prognosis of triple-negative breast cancer patient: A Croatian single institution retrospective cohort study. Acta Clin. Croat. 2020, 59, 97–108. [Google Scholar]
- Khalid, M.; Petroianu, G.; Adem, A. Advanced glycation end products and diabetic mellitus: Mechanisms and perspectives. Biomolecules 2022, 12, 542. [Google Scholar] [CrossRef]
- Sharaf, H.; Matou-Nasri, S.; Wang, Q.; Rabhan, Z.; Al-Eidi, H.; Alabdulrahman, A.; Ahmed, N. Advanced glycation endproducts increase proliferation, migration and invasion of the breast cancer cell line MDA-MB-231. Biochim. Biophys. Acta 2015, 1852, 429–441. [Google Scholar] [CrossRef]
- Artemenko, M.; Zhong, S.S.W.; To, S.K.Y.; Wong, A.S.T. p70S6 kinase as a therapeutic target in cancers: More than just an mTOR effector. Cancer Lett. 2022, 535, 215593. [Google Scholar] [CrossRef]
- Lu, Y.; Hajjar, A.; Cryns, V.L.; Trentham-Dietz, A.; Gangnon, R.E.; Heckman-Stoddard, B.M.; Alagoz, O. Breast cancer risk for women with diabetes and the impact of metformin: A meta-analysis. Cancer Med. 2023, 12, 11703–11718. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Cook, L.S.; Tang, M.C.; Hill, D.A.; Wiggins, C.L.; Li, C.I. Relationship between diabetes and diabetes medications and risk of different molecular subtypes of breast cancer. Cancer Epidemiol. Biomark. Prev. 2019, 28, 1802–1808. [Google Scholar] [CrossRef] [PubMed]
- Garczorz, W.; Kosowska, A.; Francuz, T. Antidiabetic drugs in breast cancer patients. Cancers 2024, 16, 299. [Google Scholar] [CrossRef]
- Matou-Nasri, S.; Aldawood, M.; Alanazi, F.; Khan, A.L. Updates on triple-negative breast cancer in type 2 diabetes mellitus patients: From risk factors to diagnosis, biomarkers and therapy. Diagnostics 2023, 13, 2390. [Google Scholar] [CrossRef]
- Durrani, I.A.; John, P.; Bhatti, A.; Khan, J.S. Network medicine based approach for identifying the type 2 diabetes, osteoarthritis and triple negative breast cancer interactome: Finding the hub of hub genes. Heliyon 2024, 10, e36650. [Google Scholar] [CrossRef] [PubMed]
- Ennis, C.S.; Llevenes, P.; Qiu, Y.; Dries, R.; Denis, G.V. The crosstalk within the breast tumor microenvironment in type II diabetes: Implications for cancer disparities. Front. Endocrinol. 2022, 13, 1044670. [Google Scholar] [CrossRef]
- Dong, R.; Wang, J.; Guan, R.; Sun, J.; Shen, J. Role of oxidative stress in the occurrence, development, and treatment of breast cancer. Antioxidants 2025, 14, 104. [Google Scholar] [CrossRef]
- Wu, X.; Tan, X.; Bao, Y.; Yan, W.; Zhang, Y. Landscape of metabolic alterations and treatment strategies in breast cancer. Genes Dis. 2025, 12, 101521. [Google Scholar] [CrossRef]
- Lipscombe, L.L.; Fischer, H.D.; Austin, P.C.; Fu, L.; Jaakkimainem, R.L.; Ginsburg, O.; Rochon, P.A.; Narod, S.; Paszat, L. The association between diabetes and breast cancer stage at diagnosis: A population-based study. Breast Cancer Res. Treat. 2015, 150, 613–620. [Google Scholar] [CrossRef]
- Màrmol, J.M.; Carlsson, M.; Raun, S.H.; Grand, M.K.; Sørensen, J.; Lehrskov, L.L.; Richter, E.A.; Norgaard, O.; Sylow, L. Insulin resistance in patients with cancer: A systematic review and meta-analysis. Acta Oncol. 2023, 62, 364–371. [Google Scholar] [CrossRef]
- Park, Y.M.; Bookwalter, D.B.; O'Brien, K.M.; Jackson, C.L.; Weinberg, C.R.; Sandler, D.P. A prospective study of type 2 diabetes, metformin use, and risk of breast cancer. Ann. Oncol. 2021, 32, 351–359. [Google Scholar] [CrossRef] [PubMed]
- Asiri, A.; Al Qarni, A.; Bakillah, A. The interleukin metabolic association between type 2 diabetes mellitus and cancer: Molecular mechanisms and therapeutic insights. Diagnostics 2024, 14, 2132. [Google Scholar] [CrossRef]
- Browne, I.M.; André, F.; Chandarlapaty, S.; Carey, L.A.; Turner, N.C. Optimal targeting of PI3K-AKT and mTOR in advanced oestrogen receptor-positive breast cancer. Lancet Oncol. 2024, 25, e139–e151. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Chen, F.; Sun, S.; Xv, L.; Wang, X.; Wang, M.; Zhao, S.; Zhao, Z.; Li, M. mTOR inhibitor introduce disitamab vedotin (RC48-ADC) rechallenge microtubule-chemotherapy resistance in HER2-low MBC patients with PI3K mutation. Front. Oncol. 2024, 14, 1312634. [Google Scholar] [CrossRef]
- Cerami, E.; Gao, J.; Dogrusoz, U.; Gross, B.E.; Sumer, S.O.; Aksoy, B.A.; Jacobsen, A.; Byrne, C.J.; Heuer, M.L.; Larsson, E.; et al. The cBio cancer genomics portal: An open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2012, 2, 401–404. [Google Scholar] [CrossRef]
- Barnes, C.N.; Johnson, B.P.; Leacock, S.W.; Ceballos, R.M.; Hensley, L.L.; Reyna, N.S. Gene expresion and data analysis pipeline using cancer BioPortal in the classroom. J. Microbiol. Biol. Educ. 2021, 22, 10–1128. [Google Scholar] [CrossRef] [PubMed]
- Pereira, B.; Chin, S.F.; Rueda, O.M.; Vollan, H.K.; Provenzano, E.; Bardwell, H.A.; Pugh, M.; Jones, L.; Russell, R.; Sammut, S.J.; et al. The somatic mutation profiles of 2433 breast cancers refines their genomic and transcriptomic landscapes. Nat. Commun. 2016, 7, 11479. [Google Scholar] [CrossRef]
- Rueda, O.M.; Sammut, S.J.; Seoane, J.A.; Chin, S.F.; Caswell-Jin, J.L.; Callari, M.; Batra, R.; Pereira, B.; Bruna, A.; Ali, H.R.; et al. Dynamics of breast-cancer relapse reveal late-recurring ER-positive genomic subgroups. Nature 2019, 567, 399–404. [Google Scholar] [CrossRef]
- Yu, T.J.; Ma, D.; Liu, Y.Y.; Xiao, Y.; Gong, Y.; Jiang, Y.Z.; Shao, Z.M.; Hu, X.; Di, G.H. Bulk and single-cell transcriptome profiling reveal the metabolic heterogeneity in human breast cancers. Mol. Ther. 2021, 29, 2350–2365. [Google Scholar] [CrossRef]
- Cancer Genome Atlas Research Network; Weinstein, J.N.; Collisson, E.A.; Mills, G.B.; Shaw, K.R.; Ozenberger, B.A.; Ellrott, K.; Shmulevich, I.; Sander, C.; Stuart, J.M. The Cancer Genome Atlas Pan-Cancer analysis project. Nat. Genet. 2013, 45, 1113–1120. [Google Scholar] [CrossRef]
- Varambally, S.; Karthikeyan, S.K.; Chandrashekar, D.; Sahai, S.; Shrestha, S.; Aneja, R.; Singh, R.; Kleer, C.; Kumar, S.; Qin, Z.; et al. MammOnc-DB, an integrative breast cancer data analysis platform for target discovery. Res. Square 2024, 26, rs.3.rs-4926362. [Google Scholar]
- Staaf, J.; Häkkinen, J.; Hegardt, C.; Saal, L.H.; Kimbung, S.; Hedenfalk, I.; Lien, T.; Sørlie, T.; Naume, B.; Russnes, H.; et al. RNA sequencing-based single sample predictors of molecular subtype and risk of recurrence for clinical assessment of early-stage breast cancer. NPJ Breast Cancer 2022, 8, 94. [Google Scholar] [CrossRef]
- Goncalves, A.; Finetti, P.; Birnbaum, D.; Bertucci, F. The CINSARC signature predicts the clinical outcome in patients with luminal B breast cancer. NPJ Breast Cancer 2021, 7, 48. [Google Scholar] [CrossRef] [PubMed]
- Tamez-Peña, J.G.; Rodriguez-Rojas, J.A.; Gomez-Rueda, H.; Celaya-Padilla, J.M.; Rivera-Prieto, R.A.; Palacios-Corona, R.; Garza-Montemayor, M.; Cardona-Huerta, S.; Treviño, V. Radiogenomics analysis identifies correlations of digital mammography with clinical molecular signatures in breast cancer. PLoS ONE 2018, 13, e0193871. [Google Scholar] [CrossRef] [PubMed]
- Matou-Nasri, S.; Sharaf, H.; Wang, Q.; Almobadel, N.; Rabhan, Z.; Al-Eidi, H.; Yahya, W.B.; Trivilegio, T.; Ali, R.; Al-Shanti, N.; et al. Biological impact of advanced glycation endproducts on estrogen receptor-positive MCF-7 breast cancer cells. Biochim. Biophys. Acta Mol. Basis Dis. 2017, 1863, 2808–2820. [Google Scholar] [CrossRef]
- Glaviano, A.; Foo, A.S.C.; Lam, H.Y.; Yap, K.C.H.; Jacot, W.; Jones, R.H.; Eng, H.; Nair, M.G.; Makvandi, P.; Geoerger, B.; et al. PI3K/AKT/mTOR signaling transduction pathway and targeted therapies in cancer. Mol. Cancer 2023, 22, 138. [Google Scholar] [CrossRef] [PubMed]
- Majeed, S.T.; Majeed, R.; Shah, G.; Andrabi, K.I. S6 kinase: A compelling prospect for therapeutic interventions. In Homeostasis: An Integrated Vision; IntechOpen: London, UK, 2019. [Google Scholar] [CrossRef]
- Maashi, Y.; Almutairi, S.; Aldawood, M.; Al-Eidi, H.; AlRoshody, R.; Alghamdi, H.A.; Bahattab, S.; Alsaleh, A.A.; Alkadi, H.; Alghamdi, S.; et al. In vitro oncogenic effects of glycated albumin in human colorectal cancer cell lines HT29 and SW620 revealing EpCAM and galectin-3 upregulation in type 2 diabetic colorectal cancer tissues as potential biomarkers. J. Oncol. Res. Ther. 2024, 9, 10227. [Google Scholar]
- Shum, M.; Houde, V.P.; Bellemare, V.; Moreira, R.J.; Bellmann, K.; St-Pierre, P.; Viollet, B.; Foretz, M.; Marette, A. Inhibition of mitochondrial complex 1 by the S6K1 inhibitor PF-4708671 partly contributes to its glucose metabolic effects in muscle and liver cells. J. Biol. Chem. 2019, 294, 12250–12260. [Google Scholar] [CrossRef]
- Haythorne, E.; Liloyd, M.; Walsby-Tickle, J.; Tarasov, A.I.; Sandbrink, J.; Portillo, I.; Exposito, R.T.; Sachse, G.; Cyranka, M.; Rohm, M.; et al. Altered glycolysis triggers impaired mitochondrial metabolism and mTORC1 activation in diabetic b-cells. Nat. Commun. 2022, 13, 6754. [Google Scholar] [CrossRef]
- Khotskaya, Y.; Goverdhan, A.; Shen, J.; Ponz-Sarvise, M.; Chang, S.S.; Hsu, M.C.; Wei, Y.; Xia, W.; Yu, D.; Hung, M.C. S6K1 promotes invasiveness of breast cancer cells in a model of metastasis of triple-negative breast cancer. Am. J. Transl. Res. 2014, 6, 361–376. [Google Scholar]
- Spirrison, A.N.; Lannigan, D. RSK1 and RSK2 as therapeutic targets: An up-to-date snapshot of emerging data. Expert. Opin. Ther. Targets 2024, 28, 1047–1059. [Google Scholar] [CrossRef] [PubMed]
- Jafari, N.; Zheng, Q.; Li, L.; Li, W.; Qi, L.; Xiao, J.; Gao, T.; Huang, C. p70S6K1 (S6K1)-mediated phosphorylation regulates phosphatidylinositol 4-phosphate 5-kinase type Iγ degradation and cell invasion. J. Biol. Chem. 2016, 291, 25729–25741. [Google Scholar] [CrossRef]
- Li, B.K.; Guo, K.; Li, C.Y.; Li, H.L.; Zhao, P.P.; Chen, K.; Liu, C.X. Influence of suppression of CapG gene expression by siRNA on the growth and metastasis of human prostate cancer cells. Genet. Mol. Res. 2015, 14, 15769–15778. [Google Scholar] [CrossRef]
- Tsai, T.J.; Lim, Y.P.; Chao, W.Y.; Chen, C.C.; Chen, Y.J.; Lin, C.Y.; Lee, Y.R. Capping actin protein overexpression in human colorectal carcinoma and its contributed tumor migration. Anal. Cell Pathol. 2018, 2018, 8623937. [Google Scholar] [CrossRef]
- Ajani, J.A.; Estrella, J.S.; Chen, Q.; Correa, A.M.; Lang, M.; Scott, A.W.; Jin, J.; Liu, B.; Xie, M.; Sudo, K.; et al. Galectin-3 expression is prognostic in diffuse type gastric adenocarcinoma, confers aggressive phenotype, and can be targeted by YAP1/BET inhibitors. Br. J. Cancer 2018, 118, 52–61. [Google Scholar] [CrossRef] [PubMed]
- Ram, T.J.; Lekshmi, A.; Darvin, P.; Rajappan, P.; Jagathnath Krishna, K.M.; Anoop, T.M.; Augustine, P.; Mathew, A.P.; Cherian, K.; Bhargavan, R.V.; et al. Co-expression of galectin-3 and vimentin in triple negative breast cancer cells promotes tumor progression, metastasis and survival. Tumour Biol. 2023, 45, 31–54. [Google Scholar]
- Jia, J.; Abudu, Y.P.; Claude-Taupin, A.; Gu, Y.; Kumar, S.; Choi, S.W.; Peters, R.; Mudd, M.H.; Allers, L.; Salemi, M.; et al. Galectins control mTOR in response to endomembrane damage. Mol. Cell 2018, 70, 120–135. [Google Scholar] [CrossRef]
- Shafiq, A.; Moore, J.; Suleman, A.; Faiz, S.; Farooq, O.; Arshad, A.; Tehseen, M.; Zafar, A.; Ali, S.H.; Din, N.U.; et al. Elevated soluble galectin-3 as a marker of chemotherapy efficacy in breast cancer patients: A prospective study. Int. J. Breast Cancer 2020, 2020, 4824813. [Google Scholar] [CrossRef] [PubMed]
- Raiter, A.; Barhum, Y.; Lipovetsky, J.; Menachem, C.; Elgavish, S.; Ruppo, S.; Birger, Y.; Ezraeli, S.; Steinberg-Shemer, O.; Yerushalmi, R. Galectin-3 secreted by triple-negative breast cancer cells regulates T cell function. Neoplasia 2025, 60, 101117. [Google Scholar] [CrossRef]
- Lin, D.; Hong, X.; Sun, K.; Zhang, X.; Lian, H.; Wang, J.; Mao, N.; Zhang, X.; Ren, M.; Yan, L.; et al. Galectin-3/adiponectin as a new biological indicator for assessing the risk of type 2 diabetes: A cross-sectional study in a community population. Aging 2021, 13, 15433–15443. [Google Scholar] [CrossRef]
- Petrovic, I.; Pejnovic, N.; Ljujic, B.; Pavlovic, S.; Miletic Kovacevic, M.; Jeftic, I.; Djukic, A.; Draginic, N.; Andjic, M.; Arsenijevic, N.; et al. Overexpression of galectin 3 in pancreatic β cells amplifies β-cell apoptosis and islet inflammation in type-2 diabetes in mice. Front. Endocrinol. 2020, 11, 30. [Google Scholar] [CrossRef] [PubMed]
- Da Costa, G.G.; Gomig, T.H.; Kaviski, R.; Sousa, K.S.; Kukolj, C.; De Lima, R.S.; De Andrade Urban, C.; Cavalli, I.J.; Ribeiro, E.M. Comparative proteomics of tumor and paired normal breast tissue highlights potential biomarkers in breast cancer. Cancer Genom. Proteom. 2015, 12, 251–261. [Google Scholar]
- Vizin, T.; Kos, J. Gamma-enolase: A well-known tumour marker, with a less-known role in cancer. Radiol. Oncol. 2015, 49, 217–226. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, F.; Emad, S.; Waraich, R.S.; Ghani, R.; Shah, K.; Ali, N.N.; Qazi, S.; Jibran, S.; Rohilla, A.R. Investigating neuron-specific enolase as a diagnostic marker for earlt detection of diabetic peripheral neuropathy in patients with type II diabetes mellitus. J. Popul. Ther. Clin. Pharmacol. 2024, 31, 1209–1219. [Google Scholar]
- Alhudiri, I.; Nolan, C.; Ellis, I.; Elzagheid, A.; Green, A.; Chapman, C. Expression of cathepsin D in early-stage breast cancer and its prognostic and predictive value. Breast Cancer Res. Treat. 2024, 206, 143–153. [Google Scholar] [CrossRef]
- Desroys du Roure, P.; David, T.; Mallavialle, A.; Laurent-Matha, V.; Roger, P.; Guiu, S.; Chardès, T.; Liaudet-Coopman, E. Antibodies against the multifaceted cathepsin D protein open new avenues for TNBC immunotherapy. J. Immunother. Cancer 2025, 13, e009548. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alanazi, F.; Alsaleh, A.A.; Alamoudi, M.K.; Alasiri, A.; Haymond, A.; Matou-Nasri, S. Targeting p70S6K1 Inhibits Glycated Albumin-Induced Triple-Negative Breast Cancer Cell Invasion and Overexpression of Galectin-3, a Potential Prognostic Marker in Diabetic Patients with Invasive Breast Cancer. Biomedicines 2025, 13, 612. https://doi.org/10.3390/biomedicines13030612
Alanazi F, Alsaleh AA, Alamoudi MK, Alasiri A, Haymond A, Matou-Nasri S. Targeting p70S6K1 Inhibits Glycated Albumin-Induced Triple-Negative Breast Cancer Cell Invasion and Overexpression of Galectin-3, a Potential Prognostic Marker in Diabetic Patients with Invasive Breast Cancer. Biomedicines. 2025; 13(3):612. https://doi.org/10.3390/biomedicines13030612
Chicago/Turabian StyleAlanazi, Fatimah, Abdulmonem A. Alsaleh, Mariam K. Alamoudi, Abdulrahman Alasiri, Amanda Haymond, and Sabine Matou-Nasri. 2025. "Targeting p70S6K1 Inhibits Glycated Albumin-Induced Triple-Negative Breast Cancer Cell Invasion and Overexpression of Galectin-3, a Potential Prognostic Marker in Diabetic Patients with Invasive Breast Cancer" Biomedicines 13, no. 3: 612. https://doi.org/10.3390/biomedicines13030612
APA StyleAlanazi, F., Alsaleh, A. A., Alamoudi, M. K., Alasiri, A., Haymond, A., & Matou-Nasri, S. (2025). Targeting p70S6K1 Inhibits Glycated Albumin-Induced Triple-Negative Breast Cancer Cell Invasion and Overexpression of Galectin-3, a Potential Prognostic Marker in Diabetic Patients with Invasive Breast Cancer. Biomedicines, 13(3), 612. https://doi.org/10.3390/biomedicines13030612





