Effectiveness of Humidified High Flow Nasal Cannula Versus Continuous Nasal Positive Airway Pressure in Managing Respiratory Failure in Preterm Infants: An Emergency Department Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Enrolment
2.2. Patient Selection and Grouping
2.3. Training Session
2.4. Data Collection
2.5. Data Analysis
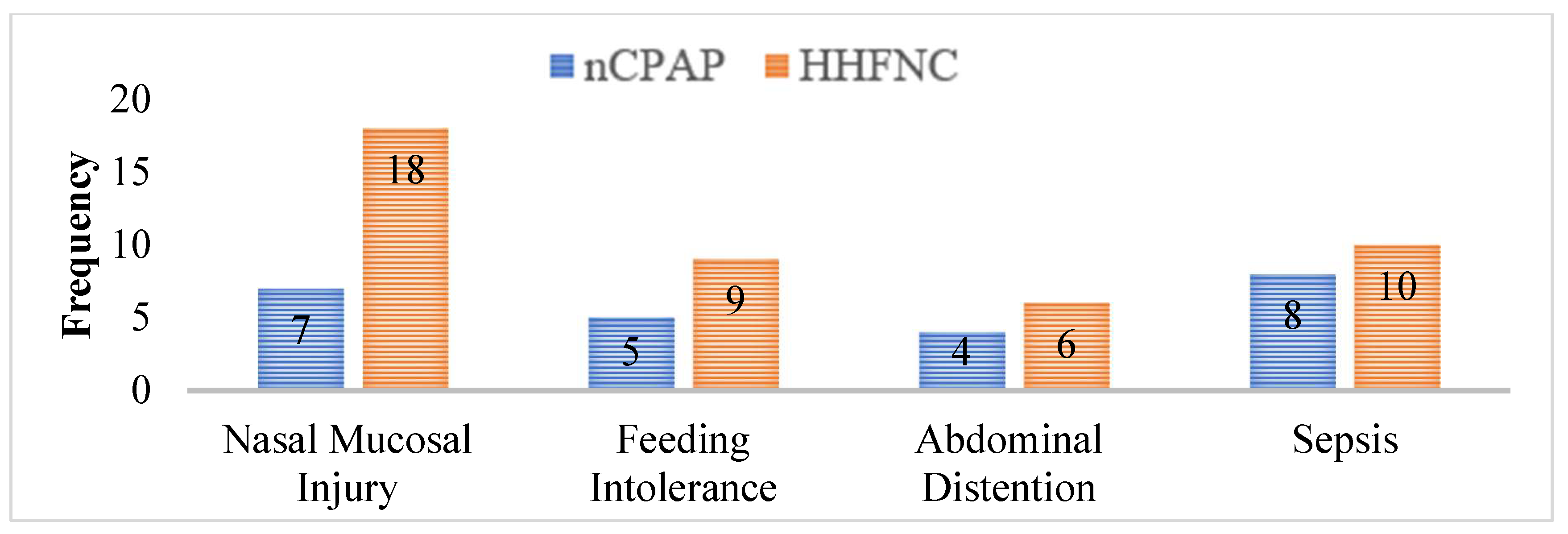
3. Results
3.1. Baseline Characteristics of Study Sample
3.2. Comparison of Duration of Application of Non-Invasive Ventilatory Support (Hours) and Hospital Stay Between the Groups
3.3. Comparison of Treatment Failure in Both Groups
3.4. Comparison of Duration of Neonatal Outcome Between the Groups
3.5. Comparison of Arterial pH Levels Between HHFNC and nCPAP Groups
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- De Luca, D. Respiratory distress syndrome in preterm neonates in the era of precision medicine: A modern critical care-based approach. Pediatr. Neonatol. 2021, 62, S3–S9. [Google Scholar] [CrossRef]
- Ramaswamy, V.V.; More, K.; Roehr, C.C.; Bandiya, P.; Nangia, S. Efficacy of noninvasive respiratory support modes for primary respiratory support in preterm neonates with respiratory distress syndrome: Systematic review and network meta-analysis. Pediatr. Pulmonol. 2020, 55, 2940–2963. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Lin, Y.; Du, L.; Kang, M.; Chi, X.; Wang, Z.; Chen, Y. The comparison of HHHFNC and NCPAP in extremely low-birth-weight preterm infants after extubation: A single-center randomized controlled trial. Front. Pediatr. 2020, 8, 250. [Google Scholar] [CrossRef] [PubMed]
- Malakian, A.; Aramesh, M.R.; Agahin, M.; Dehdashtian, M. Non-invasive duo positive airway pressure ventilation versus nasal continuous positive airway pressure in preterm infants with respiratory distress syndrome: A randomized controlled trial. BMC Pediatr. 2021, 21, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Kenner, C.; Boykova, M.V. Neonatal Nursing Care Handbook: An Evidence-Based Approach to Conditions and Procedures; Springer Publishing Company: Berlin/Heidelberg, Germany, 2021. [Google Scholar]
- Campbell, D.E. Continuing Care of the Infant After Transfer From Neonatal Intensive Care. In Neonatology for Primary Care; American Academy of Pediatrics: Itasca, IL, USA, 2020. [Google Scholar]
- Sjöblom, A. Clinical and Physiological Consequences of Preoxygenation Using High-Flow Nasal Oxygen in Emergency Anaesthesia; Karolinska Institutet: Stockholm, Sweden, 2023. [Google Scholar]
- Çetinkaya, M.; Atasay, B.; Perk, Y. Turkish Neonatal Society guideline on the transfusion principles in newborns. Turk. Arch. Pediatr. Türk Pediatri Arşivi 2018, 53 (Suppl. S1), S101–S108. [Google Scholar] [CrossRef] [PubMed]
- Dunn, M.S.; Kaempf, J.; de Klerk, A.; de Klerk, R.; Reilly, M.; Howard, D.; Ferrelli, K.; O’Conor, J.; Soll, R.F. Randomized trial comparing 3 approaches to the initial respiratory management of preterm neonates. Pediatrics 2011, 128, e1069–e1076. [Google Scholar] [CrossRef] [PubMed]
- Murki, S.; Singh, J.; Khant, C.; Dash, S.K.; Oleti, T.P.; Joy, P.; Kabra, N.S. High-flow nasal cannula versus nasal continuous positive airway pressure for primary respiratory support in preterm infants with respiratory distress: A randomized controlled trial. Neonatology 2018, 113, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.-J.; Chiang, L.-L.; Chen, K.-Y.; Feng, P.-H.; Su, C.-L.; Hsu, H.-S. High-Flow Nasal Cannula versus Noninvasive Positive Pressure Ventilation in Patients with Heart Failure after Extubation: An Observational Cohort Study. Can. Respir. J. 2020, 1, 6736475. [Google Scholar] [CrossRef]
- Sreenan, C.; Lemke, R.P.; Hudson-Mason, A.; Osiovich, H. High-flow nasal cannulae in the management of apnea of prematurity: A comparison with conventional nasal continuous positive airway pressure. Pediatrics 2001, 107, 1081–1083. [Google Scholar] [CrossRef]
- Lee, C.C.; Mankodi, D.; Shaharyar, S.; Ravindranathan, S.; Danckers, M.; Herscovici, P.; Moor, M.; Ferrer, G. High flow nasal cannula versus conventional oxygen therapy and non-invasive ventilation in adults with acute hypoxemic respiratory failure: A systematic review. Respir. Med. 2016, 121, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Dumpa, V.; Avulakunta, I.; Bhandari, V. Respiratory management in the premature neonate. Expert. Rev. Respir. Med. 2023, 17, 155–170. [Google Scholar] [CrossRef] [PubMed]
- Yoder, B.A.; Stoddard, R.A.; Li, M.; King, J.; Dirnberger, D.R.; Abbasi, S. Heated, humidified high-flow nasal cannula versus nasal CPAP for respiratory support in neonates. Pediatrics 2013, 131, e1482–e1490. [Google Scholar] [CrossRef]
- Madar, J.; Roehr, C.C.; Ainsworth, S.; Ersdal, H.; Morley, C.; Rüdiger, M.; Skåre, C.; Szczapa, T.; Pas, A.T.; Trevisanuto, D.; et al. European Resuscitation Council Guidelines 2021: Newborn resuscitation and support of transition of infants at birth. Resuscitation 2021, 161, 291–326. [Google Scholar] [CrossRef]
- De Paoli, A.G.; Morley, C.; Davis, P.G. Nasal CPAP for neonates: What do we know in 2003? Arch. Dis. Child.-Fetal Neonatal Ed. 2003, 88, F168–F172. [Google Scholar] [CrossRef] [PubMed]
- Manley, B.J. A Trial Comparing Noninvasive Ventilation Strategies in Preterm Infants. In 50 Studies Every Neonatologist Should Know; Oxford Academic: New York, NY, USA, 2024; pp. 103–108. [Google Scholar]
- Shi, Y.; Muniraman, H.; Biniwale, M.; Ramanathan, R. A review on non-invasive respiratory support for management of respiratory distress in extremely preterm infants. Front. Pediatr. 2020, 8, 270. [Google Scholar] [CrossRef] [PubMed]
- Abadesso, C.; Nunes, P.; Silvestre, C.; Matias, E.; Loureiro, H.; Almeida, H. Non-invasive ventilation in acute respiratory failure in children. Pediatr. Rep. 2012, 4, e16. [Google Scholar] [CrossRef] [PubMed]
- De Luca, D.; Tingay, D.G.; van Kaam, A.H.; Courtney, S.E.; Kneyber, M.C.J.; Tissieres, P.; Tridente, A.; Rimensberger, P.C.; Pillow, J.J. Epidemiology of neonatal acute respiratory distress syndrome: Prospective, multicenter, international cohort study. Pediatr. Crit. Care Med. 2022, 23, 524–534. [Google Scholar] [CrossRef] [PubMed]
- Townsel, C.D.; Emmer, S.F.; Campbell, W.A.; Hussain, N. Gender differences in respiratory morbidity and mortality of preterm neonates. Front. Pediatr. 2017, 5, 6. [Google Scholar] [CrossRef]
- Sarkar, M.; Sinha, R.; Roychowdhoury, S.; Mukhopadhyay, S.; Ghosh, P.; Dutta, K.; Ghosh, S. Comparative study between noninvasive continuous positive airway pressure and hot humidified high-flow nasal cannulae as a mode of respiratory support in infants with acute bronchiolitis in pediatric intensive care unit of a tertiary care hospital. Indian J. Crit. Care Med. Peer-Rev. Off. Publ. Indian Soc. Crit. Care Med. 2018, 22, 85. [Google Scholar]
- Sharma, D.; Kaur, A.; Farahbakhsh, N.; Agarwal, S. To compare nasal mask with binasal prongs in delivering continuous positive airway pressure for reducing need of invasive ventilation: Randomized controlled trial. J. Matern. Fetal Neonatal Med. 2021, 34, 1890–1896. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.; Park, K.; Lee, E.H.; Choi, B.M. Humidified high flow nasal cannula versus nasal continuous positive airway pressure as an initial respiratory support in preterm infants with respiratory distress: A randomized, controlled non-inferiority trial. J. Korean Med. Sci. 2017, 32, 650. [Google Scholar] [CrossRef]
- Foglia, E.E.; Carper, B.; Gantz, M.; DeMauro, S.B.; Lakshminrusimha, S.; Walsh, M.; Schmidt, B.; Caplan, M.S.; Laptook, A.R.; Keszler, M.; et al. Association between policy changes for oxygen saturation alarm settings and neonatal morbidity and mortality in infants born very preterm. J. Pediatr. 2019, 209, 17–22. [Google Scholar] [CrossRef]
- Sarker, S.K.; Choudhury, U.K.; Mohsin, M.; Mondal, S.K.; Begum, M. Diagnostic validity of ratio between differences of central venous to arterial CO2 and arterial to central venous O2 content in diagnosis of anaerobic metabolism among septic patients. J. Curr. Adv. Med. Res. 2021, 8, 34–38. [Google Scholar] [CrossRef]
- Cristea, A.I.; Ren, C.L.; Amin, R.; Eldredge, L.C.; Levin, J.C.; Majmudar, P.P.; May, A.E.; Rose, R.S.; Tracy, M.C.; Watters, K.F.; et al. Outpatient respiratory management of infants, children, and adolescents with post-prematurity respiratory disease: An official American Thoracic Society clinical practice guideline. Am. J. Respir. Crit. Care Med. 2021, 204, e115–e133. [Google Scholar] [CrossRef]
- Wu, C.; Chen, X.; Cai, Y.; Xia, J.; Zhou, X.; Xu, S.; Huang, H.; Zhang, L.; Zhou, X.; Du, C.; et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern. Med. 2020, 180, 934–943. [Google Scholar] [CrossRef]
- Friedman, M.L.; Nitu, M.E. Acute respiratory failure in children. Pediatr. Ann. 2018, 47, e268–e273. [Google Scholar] [CrossRef] [PubMed]
- Luo, J.; Duke, T.; Chisti, M.J.; Kepreotes, E.; Kalinowski, V.; Li, J. Efficacy of high-flow nasal cannula vs standard oxygen therapy or nasal continuous positive airway pressure in children with respiratory distress: A meta-analysis. J. Pediatr. 2019, 215, 199–208. [Google Scholar] [CrossRef]
- Huang, H.-W.; Sun, X.-M.; Shi, Z.-H.; Chen, G.-Q.; Chen, L.; Friedrich, J.O.; Zhou, J.-X. Effect of high-flow nasal cannula oxygen therapy versus conventional oxygen therapy and noninvasive ventilation on reintubation rate in adult patients after extubation: A systematic review and meta-analysis of randomized controlled trials. J. Intensive Care Med. 2018, 33, 609–623. [Google Scholar] [CrossRef]
- Ann Skariah, T.; Dias, L.; Edward Lewis, L. Comparison of the Heated Humidified High-flow Nasal Cannula with Nasal Continuous Positive Airway Pressure as Primary Respiratory Support for Preterm Neonates: A Prospective Observational Study. Iran. J. Neonatol. 2019, 10, 51–57. [Google Scholar]
- Shaaban, H.A.; Aly, H.H.; Ramadan, M.A.; Gad, T.M. The Effect of Ventilatory Supports on Oxidative Stress Biomarkers in Preterm Respiratory Distress. Ain Shams Med. J. 2024, 75, 988–998. [Google Scholar] [CrossRef]
- Asseri, A.A.; AlQahtani, Y.A.; Alhanshani, A.A.; Ali, G.H.; Alhelali, I. Indications and safety of high flow nasal cannula in pediatric intensive care unit: Retrospective single center experience in Saudi Arabia. Pediatr. Health Med. Ther. 2021, 12, 431–437. [Google Scholar] [CrossRef]
- Awad, A.H.; El-Farrash, A.R.; Shinkar, D.M.; Aly, Y.A.F.; Soliman, N.; Alhassanin, A.H. A study of heated, humidified high flow nasal cannula as an initial respiratory support in preterm neonates. QJM An. Int. J. Med. 2021, 114 (Suppl. S1), hcab113.010. [Google Scholar] [CrossRef]
- Jose, D.; Parameswaran, N. Advances in management of respiratory failure in children. Indian J. Pediatr. 2023, 90, 470–480. [Google Scholar] [CrossRef] [PubMed]


| Characteristics | Group A (n = 128) | Group B (n = 128) | p-Value |
|---|---|---|---|
| Age (1–28 days) | 14.72 ± 8.45 | 15.07 ± 8.02 | 0.796 a |
| Gender | |||
| Male | 44 (40.0%) | 49 (44.5%) | 0.495 b |
| Female | 66 (60.0%) | 61 (55.5%) | |
| Gestational Age (week) | 32.71 ± 2.52 | 32.45 ± 2.94 | 0.472 a |
| APGAR Score at 5 min | 5.98 + 0.88 | 5.46 + 0.81 | 0.971 a |
| SPO2 (%) | 69.69 ± 18.2 | 70.43 ± 17.38 | 0.735 a |
| Respiratory Rate (bpm) | 52.29 ± 11.23 | 55.75 ± 11.66 | 0.028 a |
| HR Rate (bpm) | 134.28 ± 18.69 | 133.46 ± 17/83 | 0.765 a |
| Arterial pH | 7.26 ± 1.37 | 7.09 ± 1.41 | 0.301 a |
| PCO2 (mmHg) | 63.31 ± 12.1 | 63.02 ± 11.5 | 0.941 a |
| PO2 (mmHg) | 40.56 ± 5.42 | 39.87 ± 5.23 | 0.344 a |
| Duration of Application of Non-Invasive Ventilatory Support (Hours) | |||
|---|---|---|---|
| Study Group | Mean | Std. Deviation | p-Value |
| nCPAP (A) | 72.29 | 20.7 | 0.013 a |
| HHFNC (B) | 65.20 | 15.9 | |
| Hospital stays in days | |||
| nCPAP (A) | 24.25 | 6.07 | 0.000 a |
| HHFNC (B) | 20.14 | 3.50 | |
| Neonatal Outcome | Groups | Total | p-Value | |
|---|---|---|---|---|
| nCPAP | HHFNC | |||
| Discharged without the need for intubation | 100 (90.9%) | 94 (85.5%) | 194 (88.2%) | a 0.224 |
| Expired | 5 (4.5%) | 4 (3.6%) | 9 (4.1%) | |
| Intubated | 5 (4.5%) | 12 (10.9%) | 17 (7.7%) | |
| Total | 110 | 110 | 220 | |
| Variable | B | SE | Wald | p-Value | Hazard Ratio (Exp B) | 95% CI for Exp (B) |
|---|---|---|---|---|---|---|
| Treatment Group (nCPAP vs. HHFNC) | −1.526 | 0.295 | 26.806 | 0.000 | 0.217 | (0.123–0.382) |
| Sepsis | −0.707 | 0.326 | 4.697 | 0.03 | 0.493 | (0.257–0.947) |
| Treatment Failure | 0.120 | 0.326 | 0.136 | 0.71 | 1.128 | (0.588–2.163) |
| Arterial pH | Groups | Total | p-Value | |
|---|---|---|---|---|
| nCPAP | HHFNC | |||
| <7.2 | 59 (53.6%) | 63 (57.3%) | 122 (55.5%) | a 0.58 |
| >7.2 | 51 (46.4%) | 47 (42.7%) | 98 (44.5%) | |
| Total | 110 | 110 | 220 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yousof Mahboob, D.; Hassan, A.; Naheed, F.; Ali Shah, A.; Fareed Siddiqui, M. Effectiveness of Humidified High Flow Nasal Cannula Versus Continuous Nasal Positive Airway Pressure in Managing Respiratory Failure in Preterm Infants: An Emergency Department Study. Biomedicines 2025, 13, 602. https://doi.org/10.3390/biomedicines13030602
Yousof Mahboob D, Hassan A, Naheed F, Ali Shah A, Fareed Siddiqui M. Effectiveness of Humidified High Flow Nasal Cannula Versus Continuous Nasal Positive Airway Pressure in Managing Respiratory Failure in Preterm Infants: An Emergency Department Study. Biomedicines. 2025; 13(3):602. https://doi.org/10.3390/biomedicines13030602
Chicago/Turabian StyleYousof Mahboob, Duaa, Amber Hassan, Faiza Naheed, Arshad Ali Shah, and Maria Fareed Siddiqui. 2025. "Effectiveness of Humidified High Flow Nasal Cannula Versus Continuous Nasal Positive Airway Pressure in Managing Respiratory Failure in Preterm Infants: An Emergency Department Study" Biomedicines 13, no. 3: 602. https://doi.org/10.3390/biomedicines13030602
APA StyleYousof Mahboob, D., Hassan, A., Naheed, F., Ali Shah, A., & Fareed Siddiqui, M. (2025). Effectiveness of Humidified High Flow Nasal Cannula Versus Continuous Nasal Positive Airway Pressure in Managing Respiratory Failure in Preterm Infants: An Emergency Department Study. Biomedicines, 13(3), 602. https://doi.org/10.3390/biomedicines13030602







