MicroRNAs Associated with Parenchymal Hematoma After Endovascular Mechanical Reperfusion for Acute Ischemic Stroke in Rats
Abstract
1. Introduction
2. Materials and Methods
2.1. MCAO Model with Hemorrhagic Transformation After Mechanical Reperfusion
2.2. Primary Cultures of Neurons, Astrocytes, Microglia, BMECs, and Pericytes
2.3. OGD/R Model
2.4. RNA Extraction and Quantitative RT-PCR
2.5. Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) Pathway Analyses
2.6. Construction of miRNA-mRNA Regulatory Network of PH
2.7. Statistical Analysis
3. Results
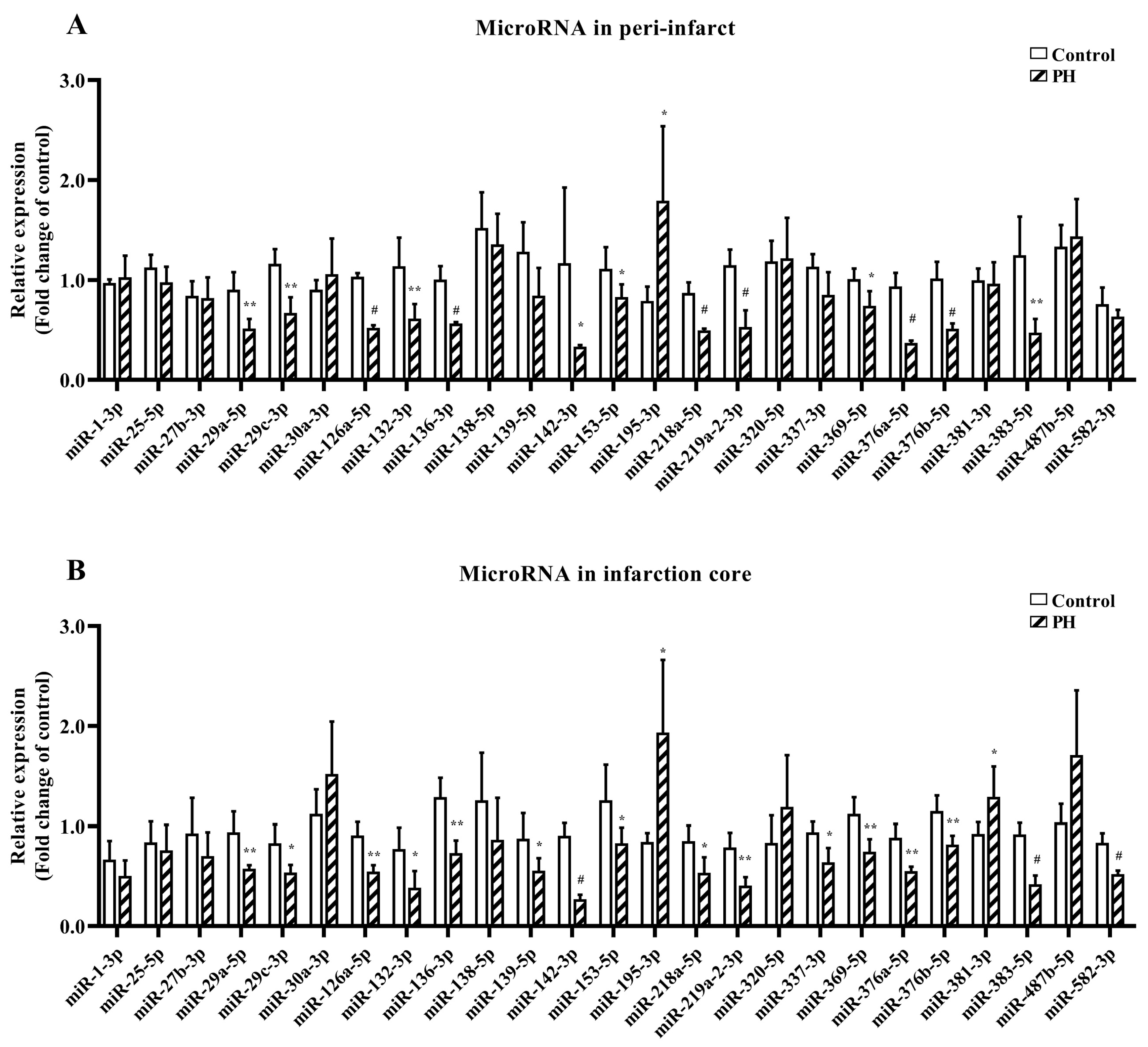
3.1. MiRNAs in Rat Ischemic Brain with PH After Mechanical Reperfusion
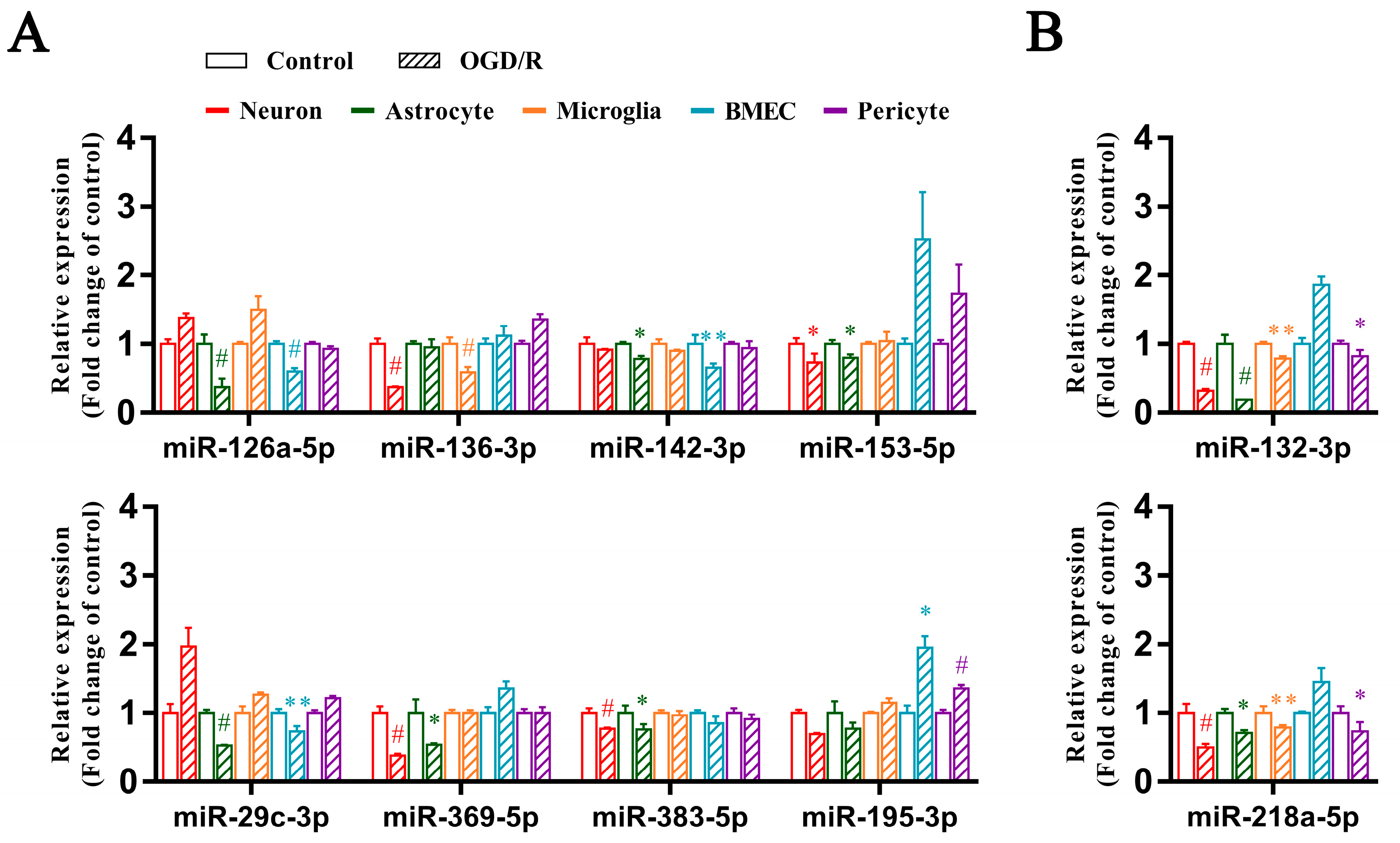
3.2. Differential Expression of PH-Related miRNAs in the OGD/R Model
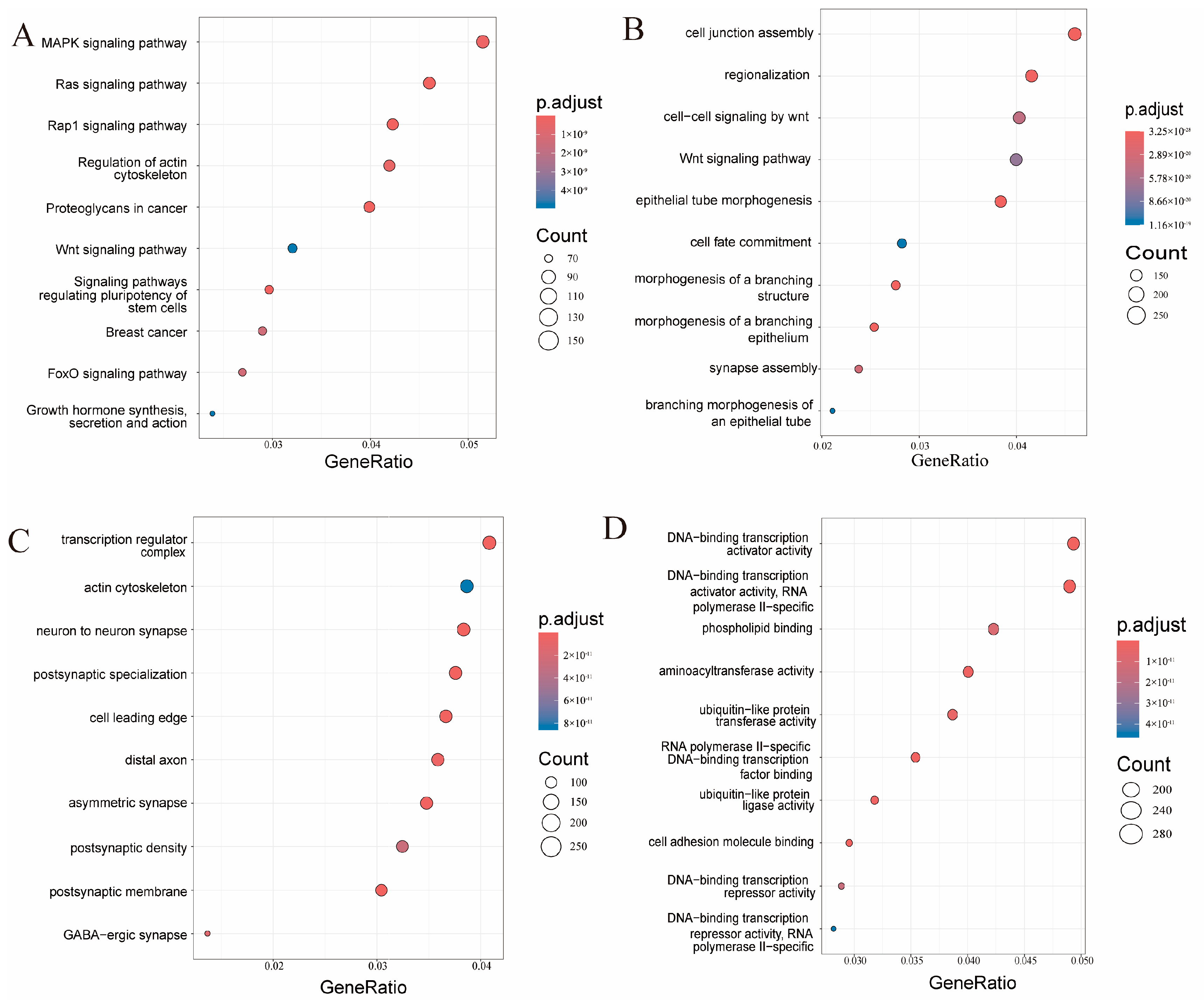
3.3. KEGG Pathway and GO Analysis of Differentially Expressed miRNAs Associated with PH
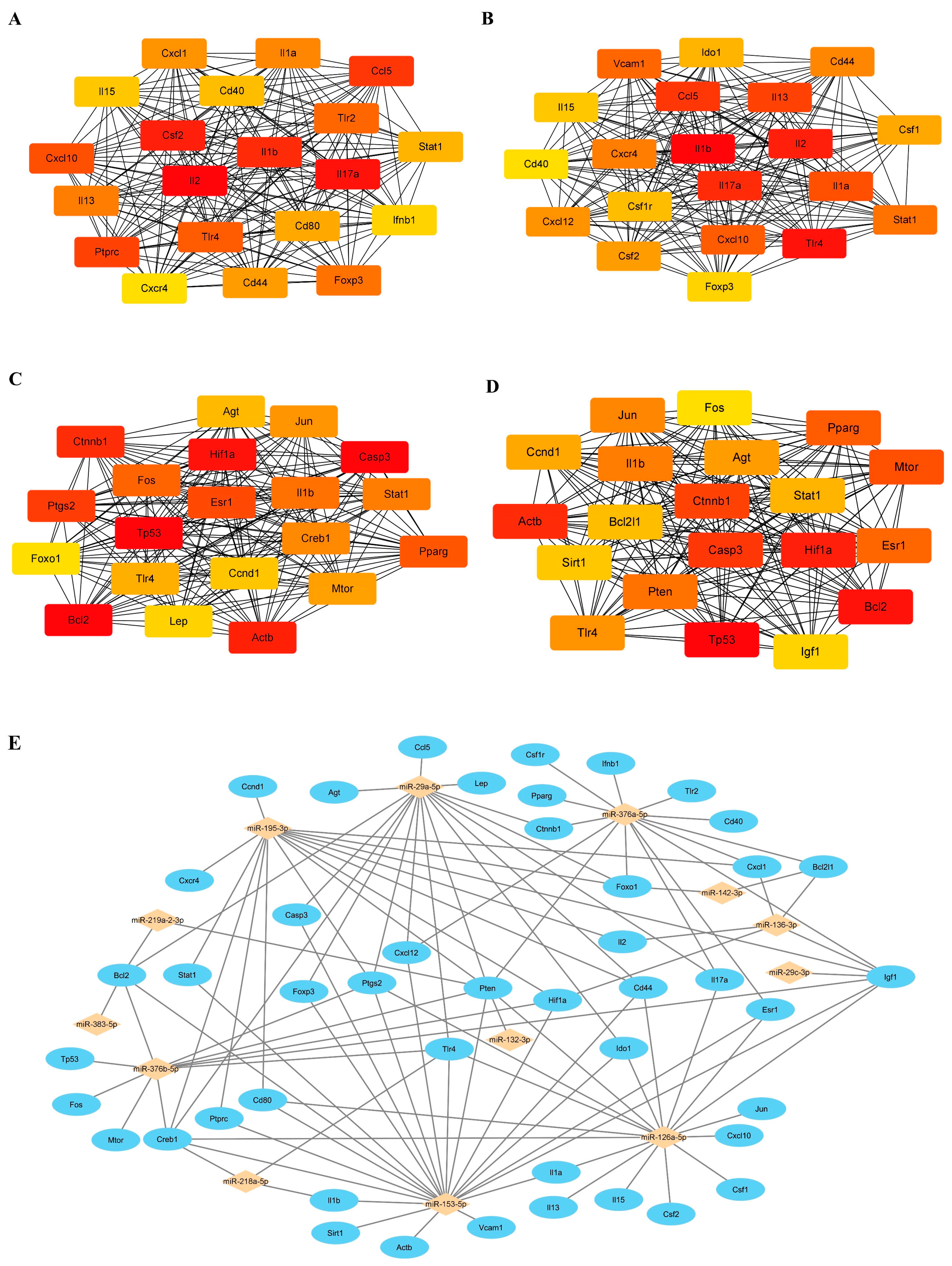
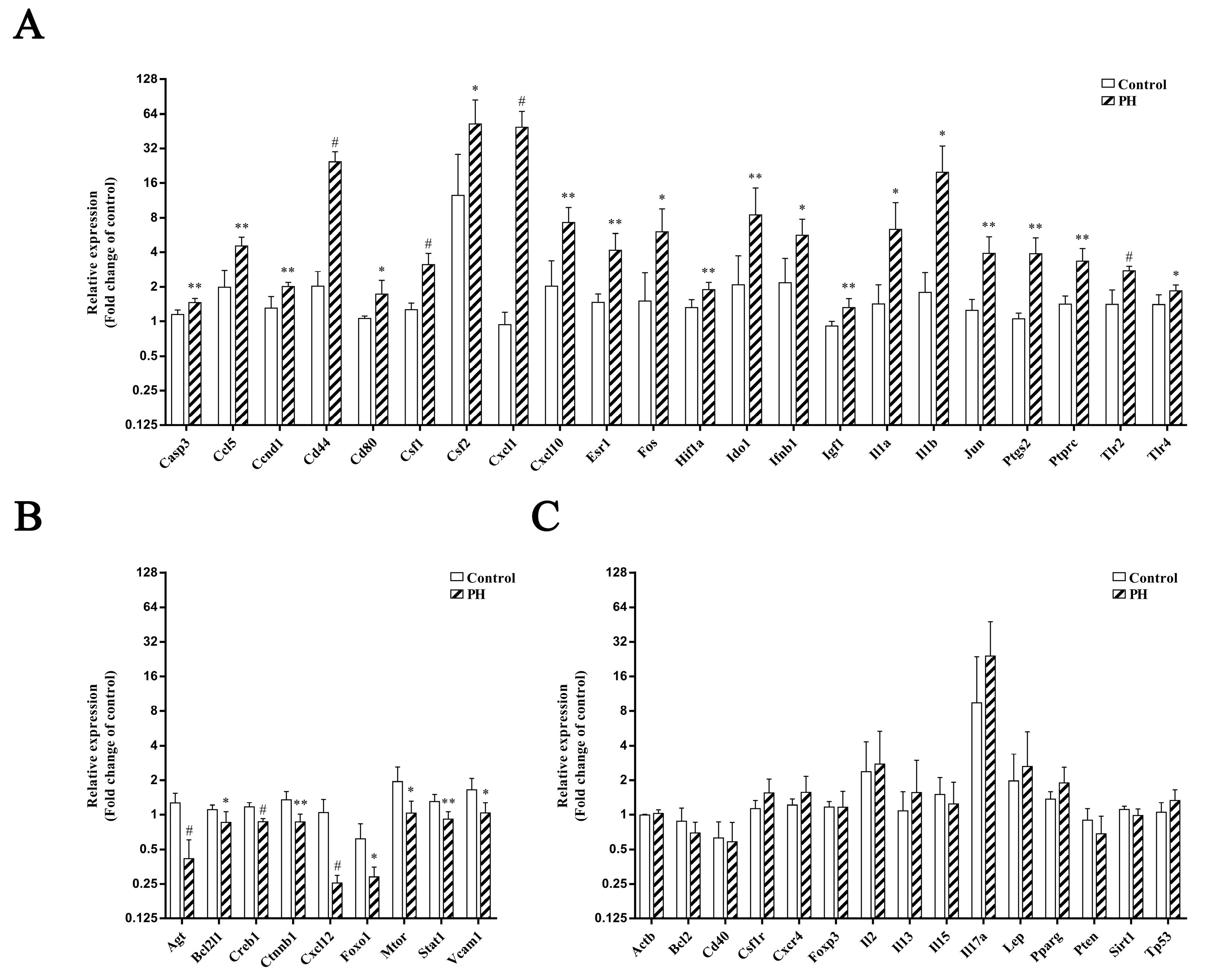
3.4. Differential Expression of Predicted Target Genes in the Rat PH Model
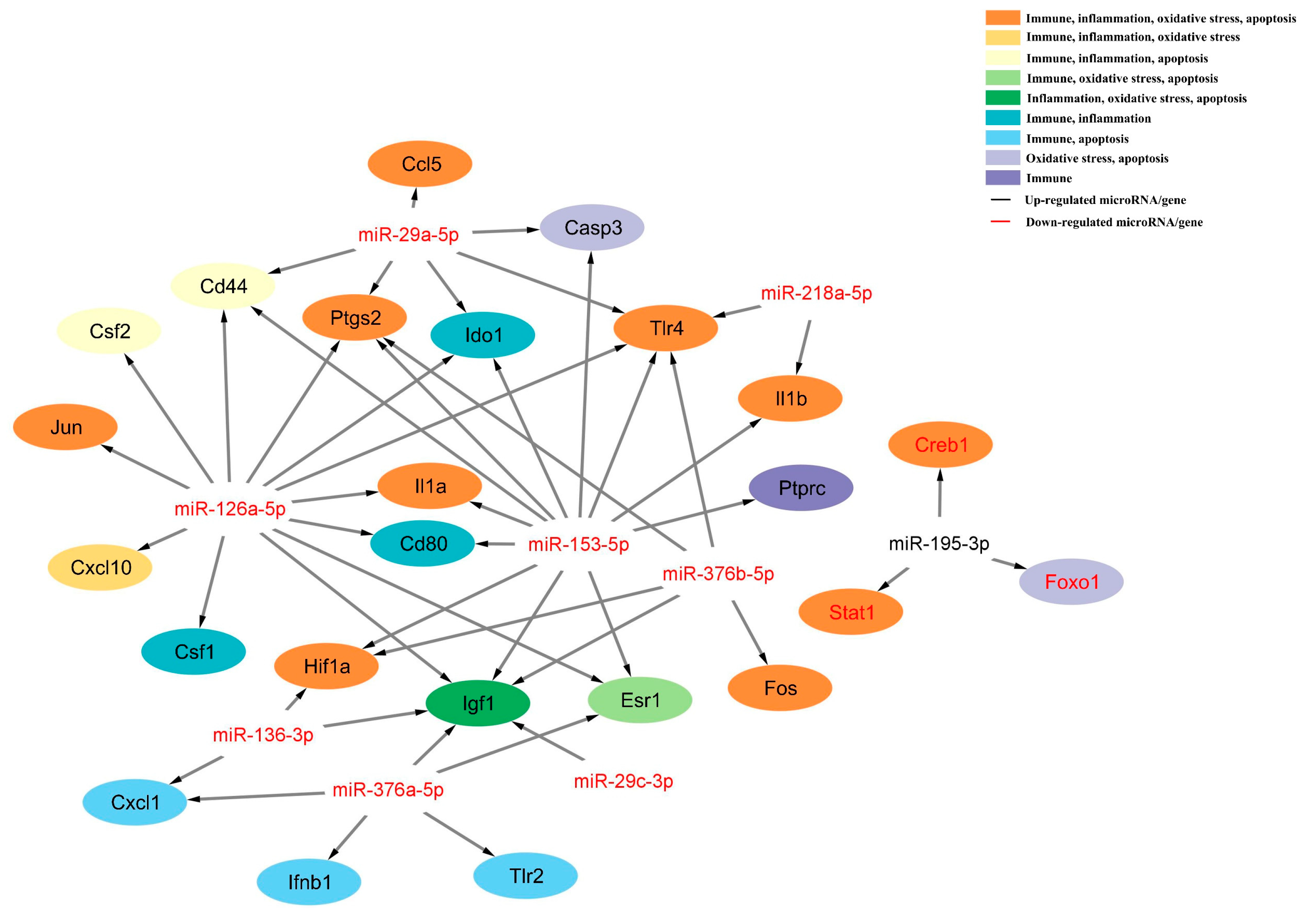
3.5. The miRNA-mRNA Regulatory Network of PH
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fischer, U.; Kaesmacher, J.; Strbian, D.; Eker, O.; Cognard, C.; Plattner, P.S.; Bütikofer, L.; Mordasini, P.; Deppeler, S.; Pereira, V.M.; et al. Thrombectomy alone versus intravenous alteplase plus thrombectomy in patients with stroke: An open-label, blinded-outcome, randomised non-inferiority trial. Lancet 2022, 400, 104–115. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, P.J.; Yan, B.; Churilov, L.; Dowling, R.J.; Bush, S.J.; Bivard, A.; Huo, X.C.; Wang, G.; Zhang, S.Y.; Ton, M.D.; et al. Endovascular thrombectomy versus standard bridging thrombolytic with endovascular thrombectomy within 4.5 h of stroke onset: An open-label, blinded-endpoint, randomised non-inferiority trial. Lancet 2022, 400, 116–125. [Google Scholar] [CrossRef] [PubMed]
- LeCouffe, N.E.; Kappelhof, M.; Treurniet, K.M.; Rinkel, L.A.; Bruggeman, A.E.; Berkhemer, O.A.; Wolff, L.; van Voorst, H.; Tolhuisen, M.L.; Dippel, D.W.; et al. A randomized trial of intravenous alteplase before endovascular treatment for stroke. N. Engl. J. Med. 2021, 385, 1833–1844. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, K.; Matsumaru, Y.; Takeuchi, M.; Morimoto, M.; Kanazawa, R.; Takayama, Y.; Kamiya, Y.; Shigeta, K.; Okubo, S.; Hayakawa, M.; et al. Effect of mechanical thrombectomy without vs. with intravenous thrombolysis on functional outcome among patients with acute ischemic stroke: The SKIP randomized clinical trial. JAMA 2021, 325, 244–253. [Google Scholar] [CrossRef]
- Zi, W.; Qiu, Z.; Li, F.; Sang, H.; Wu, D.; Luo, W.; Liu, S.; Yuan, J.; Song, J.; Shi, Z.; et al. Effect of endovascular treatment alone vs intravenous alteplase plus endovascular treatment on functional independence in patients with acute ischemic stroke: The DEVT randomized clinical trial. JAMA 2021, 325, 234–243. [Google Scholar] [CrossRef]
- Yang, P.; Zhang, Y.; Zhang, L.; Zhang, Y.; Treurniet, K.M.; Chen, W.; Peng, Y.; Han, H.; Wang, J.; Wang, S.; et al. Endovascular thrombectomy with or without intravenous alteplase in acute stroke. N. Engl. J. Med. 2020, 382, 1981–1993. [Google Scholar] [CrossRef]
- Nogueira, R.G.; Jadhav, A.P.; Haussen, D.C.; Bonafe, A.; Budzik, R.F.; Bhuva, P.; Yavagal, D.R.; Ribo, M.; Cognard, C.; Hanel, R.A.; et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N. Engl. J. Med. 2018, 378, 11–21. [Google Scholar] [CrossRef]
- Huo, X.; Ma, G.; Tong, X.; Zhang, X.; Pan, Y.; Nguyen, T.N.; Yuan, G.; Han, H.; Chen, W.; Wei, M.; et al. Trial of endovascular therapy for acute ischemic stroke with large infarct. N. Engl. J. Med. 2023, 388, 1272–1283. [Google Scholar] [CrossRef] [PubMed]
- Sarraj, A.; Hassan, A.E.; Abraham, M.G.; Ortega-Gutierrez, S.; Kasner, S.E.; Hussain, M.S.; Chen, M.; Blackburn, S.; Sitton, C.W.; Churilov, L.; et al. Trial of endovascular thrombectomy for large ischemic strokes. N. Engl. J. Med. 2023, 388, 1259–1271. [Google Scholar] [CrossRef]
- van Kranendonk, K.R.; Treurniet, K.M.; Boers, A.M.M.; Berkhemer, O.A.; Berg, L.A.v.D.; Chalos, V.; Lingsma, H.F.; van Zwam, W.H.; van der Lugt, A.; van Oostenbrugge, R.J.; et al. Hemorrhagic transformation is associated with poor functional outcome in patients with acute ischemic stroke due to a large vessel occlusion. J. NeuroInterv. Surg. 2019, 11, 464–468. [Google Scholar] [CrossRef]
- Boisseau, W.; Fahed, R.; Lapergue, B.; Desilles, J.-P.; Zuber, K.; Khoury, N.; Garcia, J.; Maïer, B.; Redjem, H.; Ciccio, G.; et al. Predictors of parenchymal hematoma after mechanical thrombectomy: A multicenter study. Stroke 2019, 50, 2364–2370. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.; Zhou, Y.; Ospel, J.; Yao, F.; Liu, Y.; Wang, H.; Li, B.; Hui, P.; Yang, P.; Zhang, Y.; et al. Intracranial hemorrhage in large vessel occlusion patients receiving endovascular thrombectomy with or without intravenous alteplase: A secondary analysis of the DIRECT-MT trial. J. NeuroInterv. Surg. 2022, 15, 977–982. [Google Scholar] [CrossRef]
- Jickling, G.C.; Liu, D.; Stamova, B.; Ander, B.P.; Zhan, X.; Lu, A.; Sharp, F.R. Hemorrhagic transformation after ischemic stroke in animals and humans. J. Cereb. Blood Flow Metab. 2014, 34, 185–199. [Google Scholar] [CrossRef]
- Hong, J.M.; Kim, D.S.; Kim, M. Hemorrhagic transformation after ischemic stroke: Mechanisms and management. Front. Neurol. 2021, 12, 703258. [Google Scholar] [CrossRef]
- Zubair, A.S.; Sheth, K.N. Hemorrhagic conversion of acute ischemic stroke. Neurotherapeutics 2023, 20, 705–711. [Google Scholar] [CrossRef] [PubMed]
- Shi, Z.; Duckwiler, G.R.; Jahan, R.; Tateshima, S.; Szeder, V.; Saver, J.L.; Kim, D.; Sharma, L.K.; Vespa, P.M.; Salamon, N.; et al. Early blood-brain barrier disruption after mechanical thrombectomy in acute ischemic stroke. J. Neuroimaging 2018, 28, 283–288. [Google Scholar] [CrossRef]
- Mizuma, A.; You, J.S.; Yenari, M.A. Targeting reperfusion injury in the age of mechanical thrombectomy. Stroke 2018, 49, 1796–1802. [Google Scholar] [CrossRef]
- Zhou, Y.; He, Y.; Yan, S.; Chen, L.; Zhang, R.; Xu, J.; Hu, H.; Liebeskind, D.S.; Lou, M. Reperfusion injury is associated with poor outcome in patients with recanalization after thrombectomy. Stroke 2023, 54, 96–104. [Google Scholar] [CrossRef]
- Wang, S.-W.; Liu, Z.; Shi, Z.-S. Non-coding RNA in acute ischemic stroke: Mechanisms, biomarkers and therapeutic targets. Cell Transplant. 2018, 27, 1763–1777. [Google Scholar] [CrossRef]
- Zheng, L.; Xiong, Y.; Liu, J.; Yang, X.; Wang, L.; Zhang, S.; Liu, M.; Wang, D. MMP-9-related microRNAs as prognostic markers for hemorrhagic transformation in cardioembolic stroke patients. Front. Neurol. 2019, 10, 945. [Google Scholar] [CrossRef]
- Han, R.; Zhang, P.; Li, H.; Chen, Y.; Hao, Y.; Guo, Q.; Zhang, A.; Li, D. Differential expression and correlation analysis of global transcriptome for hemorrhagic transformation after acute ischemic stroke. Front. Neurosci. 2022, 16, 889689. [Google Scholar] [CrossRef]
- Todoran, R.; Falcione, S.R.; Clarke, M.; Joy, T.; Boghozian, R.; Jickling, G.C. microRNA as a therapeutic for ischemic stroke. Neurochem. Int. 2023, 163, 105487. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Tuo, Y.-H.; Chen, J.-W.; Wang, Q.-Y.; Li, S.; Li, M.-C.; Dai, G.; Wang, J.-S.; Zhang, Y.-L.; Feng, L.; et al. NADPH oxidase inhibitor regulates microRNAs with improved outcome after mechanical reperfusion. J. NeuroInterv. Surg. 2017, 9, 702–706. [Google Scholar] [CrossRef] [PubMed]
- Tuo, Y.-H.; Liu, Z.; Chen, J.-W.; Wang, Q.-Y.; Li, S.-L.; Li, M.-C.; Dai, G.; Wang, J.-S.; Zhang, Y.-L.; Feng, L.; et al. NADPH oxidase inhibitor improves outcome of mechanical reperfusion by suppressing hemorrhagic transformation. J. NeuroInterv. Surg. 2017, 9, 492–498. [Google Scholar] [CrossRef] [PubMed]
- Lu, A.; Clark, J.F.; Broderick, J.P.; Pyne-Geithman, G.J.; Wagner, K.R.; Khatri, P.; Tomsick, T.; Sharp, F.R. Mechanical reperfusion is associated with post-ischemic hemorrhage in rat brain. Exp Neurol. 2009, 216, 407–412. [Google Scholar] [CrossRef] [PubMed]
- Sutherland, B.A.; Neuhaus, A.A.; Couch, Y.; Balami, J.S.; DeLuca, G.C.; Hadley, G.; Harris, S.L.; Grey, A.N.; Buchan, A.M. The transient intraluminal filament middle cerebral artery occlusion model as a model of endovascular thrombectomy in stroke. J. Cereb. Blood Flow Metab. 2016, 36, 363–369. [Google Scholar] [CrossRef]
- Zhang, W.; Liu, J.; Hu, X.; Li, P.; Leak, R.K.; Gao, Y.; Chen, J. N-3 polyunsaturated fatty acids reduce neonatal hypoxic/ischemic brain injury by promoting phosphatidylserine formation and akt signaling. Stroke 2015, 46, 2943–2950. [Google Scholar] [CrossRef] [PubMed]
- Qin, A.-P.; Liu, C.-F.; Qin, Y.-Y.; Hong, L.-Z.; Xu, M.; Yang, L.; Liu, J.; Qin, Z.-H.; Zhang, H.-L. Autophagy was activated in injured astrocytes and mildly decreased cell survival following glucose and oxygen deprivation and focal cerebral ischemia. Autophagy 2010, 6, 738–753. [Google Scholar] [CrossRef]
- Gao, C.; Jia, W.; Xu, W.; Wu, Q.; Wu, J. Downregulation of cd151 restricts VCAM-1 mediated leukocyte infiltration to reduce neurobiological injuries after experimental stroke. J. Neuroinflamm. 2021, 18, 118. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Wang, J.; Fang, Y.; Liu, Y.; Chen, T.; Sun, H.; Zhou, X.-F.; Liao, H. Nafamostat mesilate improves function recovery after stroke by inhibiting neuroinflammation in rats. Brain Behav. Immun. 2016, 56, 230–245. [Google Scholar] [CrossRef]
- Redzic, Z.B.; Rabie, T.; Sutherland, B.A.; Buchan, A.M. Differential effects of paracrine factors on the survival of cells of the neurovascular unit during oxygen glucose deprivation. Int. J. Stroke 2015, 10, 407–414. [Google Scholar] [CrossRef] [PubMed]
- Ashwal, S.; Tone, B.; Tian, H.R.; Cole, D.J.; Pearce, W.J. Core and penumbral nitric oxide synthase activity during cerebral ischemia and reperfusion. Stroke 1998, 29, 1037–1047. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.; Zhao, H.; Wang, R.; Wang, P.; Tao, Z.; Gao, L.; Yan, F.; Liu, X.; Yu, S.; Ji, X.; et al. MicroRNA-424 protects against focal cerebral ischemia and reperfusion injury in mice by suppressing oxidative stress. Stroke 2015, 46, 513–519. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.; Hu, E.; Xu, S.; Chen, M.; Guo, P.; Dai, Z.; Feng, T.; Zhou, L.; Tang, W.; Zhan, L.; et al. clusterProfiler 4.0: A universal enrichment tool for interpreting omics data. Innovation 2021, 2, 100141. [Google Scholar] [CrossRef] [PubMed]
- Ouyang, Y.-B.; Stary, C.M.; White, R.E.; Giffard, R.G. The use of microRNAs to modulate redox and immune response to stroke. Antioxid. Redox Signal. 2015, 22, 187–202. [Google Scholar] [CrossRef] [PubMed]
- Uhlmann, S.; Mracsko, E.; Javidi, E.; Lamble, S.; Teixeira, A.; Hotz-Wagenblatt, A.; Glatting, K.-H.; Veltkamp, R. Genome-wide analysis of the circulating miRNome after cerebral ischemia reveals a reperfusion-induced microRNA cluster. Stroke 2017, 48, 762–769. [Google Scholar] [CrossRef]
- Neag, M.-A.; Mitre, A.-O.; Burlacu, C.-C.; Inceu, A.-I.; Mihu, C.; Melincovici, C.-S.; Bichescu, M.; Buzoianu, A.-D. MiRNA involvement in cerebral ischemia-reperfusion injury. Front. Neurosci. 2022, 16, 901360. [Google Scholar] [CrossRef] [PubMed]
- Pan, J.; Qu, M.; Li, Y.; Wang, L.; Zhang, L.; Wang, Y.; Tang, Y.; Tian, H.-L.; Zhang, Z.; Yang, G.-Y. MicroRNA-126-3p/-5p overexpression attenuates blood-brain barrier disruption in a mouse model of middle cerebral artery occlusion. Stroke 2020, 51, 619–627. [Google Scholar] [CrossRef] [PubMed]
- Song, X.; Liu, J.; Wang, Y.; Zheng, L.; Liu, M. Serum microRNA miR-491-5p/miR-206 is correlated with poor outcomes/spontaneous hemorrhagic transformation after ischemic stroke: A case control study. Brain Sci. 2022, 12, 999. [Google Scholar] [CrossRef]
- Suofu, Y.; Wang, X.; He, Y.; Li, F.; Zhang, Y.; Carlisle, D.L.; Friedlander, R.M. Mir-155 knockout protects against ischemia/reperfusion-induced brain injury and hemorrhagic transformation. Neuroreport 2020, 31, 235–239. [Google Scholar] [CrossRef]
- Qiu, L.; Cai, Y.; Geng, Y.; Yao, X.; Wang, L.; Cao, H.; Zhang, X.; Wu, Q.; Kong, D.; Ding, D.; et al. Mesenchymal stem cell-derived extracellular vesicles attenuate tPA-induced blood–brain barrier disruption in murine ischemic stroke models. Acta Biomater. 2022, 154, 424–442. [Google Scholar] [CrossRef] [PubMed]
- Geng, L.; Zheng, L.-Z.; Kang, Y.-F.; Pan, C.-L.; Wang, T.; Xie, C.; Liang, B.; Liao, H.-L. Zhilong Huoxue Tongyu Capsule attenuates hemorrhagic transformation through the let-7f/TLR4 signaling pathway. J. Ethnopharmacol. 2023, 312, 116521. [Google Scholar] [CrossRef] [PubMed]
- Tang, N.; Gong, X.-R.; Huang, H.; Meng, Q. Activated neutrophil-derived exosomes contribute to blood–brain barrier damage and hemorrhagic transformation after cerebral ischemia/reperfusion. Brain Res. 2023, 1810, 148374. [Google Scholar] [CrossRef]
- Deng, L.; Zhang, J.; Chen, S.; Wu, Y.; Fan, X.; Zuo, T.; Hu, Q.; Jiang, L.; Yang, S.; Dong, Z. miR-671-5p upregulation attenuates blood-brain barrier disruption in the ischemia stroke model via the NF-кB/MMP-9 signaling pathway. Mol. Neurobiol. 2023, 60, 3824–3838. [Google Scholar] [CrossRef] [PubMed]
- Qin, C.; Yang, S.; Chu, Y.-H.; Zhang, H.; Pang, X.-W.; Chen, L.; Zhou, L.-Q.; Chen, M.; Tian, D.-S.; Wang, W. Signaling pathways involved in ischemic stroke: Molecular mechanisms and therapeutic interventions. Signal Transduct. Target. Ther. 2022, 7, 215. [Google Scholar] [CrossRef] [PubMed]
- Lv, W.; Jiang, J.; Xu, Y.; Chen, Z.; Wang, Z.; Xing, A.; Zheng, X.; Qu, T.; Wan, Q. Re-exploring the inflammation-related core genes and modules in cerebral ischemia. Mol. Neurobiol. 2023, 60, 3439–3451. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Bonilla, L.; Shahanoor, Z.; Sciortino, R.; Nazarzoda, O.; Racchumi, G.; Iadecola, C.; Anrather, J. Analysis of brain and blood single-cell transcriptomics in acute and subacute phases after experimental stroke. Nat. Immunol. 2024, 25, 357–370. [Google Scholar] [CrossRef]
- Spronk, E.; Sykes, G.; Falcione, S.; Munsterman, D.; Joy, T.; Kamtchum-Tatuene, J.; Jickling, G.C. Hemorrhagic transformation in ischemic stroke and the role of inflammation. Front. Neurol. 2021, 12, 661955. [Google Scholar] [CrossRef]
- Hu, Q.; Manaenko, A.; Bian, H.; Guo, Z.; Huang, J.-L.; Guo, Z.-N.; Yang, P.; Tang, J.; Zhang, J.H. Hyperbaric oxygen reduces infarction volume and hemorrhagic transformation through ATP/NAD+/Sirt1 pathway in hyperglycemic middle cerebral artery occlusion rats. Stroke 2017, 48, 1655–1664. [Google Scholar] [CrossRef] [PubMed]
- Merino-Zamorano, C.; Hernández-Guillamon, M.; Jullienne, A.; Le Béhot, A.; Bardou, I.; Parés, M.; Fernández-Cadenas, I.; Giralt, D.; Carrera, C.; Ribó, M.; et al. NURR1 involvement in recombinant tissue-type plasminogen activator treatment complications after ischemic strokee. Stroke 2015, 46, 477–484. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Li, M.; Wang, Y.; Wang, Z.; Zhang, W.; Guan, F.; Chen, Q.; Wang, J. GSK-3β as a target for protection against transient cerebral ischemia. Int. J. Med. Sci. 2017, 14, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Ostrowski, R.P.; Zhou, C.; Tang, J.; Zhang, J.H. Suppression of hypoxia-inducible factor-1alpha and its downstream genes reduces acute hyperglycemia-enhanced hemorrhagic transformation in a rat model of cerebral ischemia. J. Neurosci. Res. 2010, 88, 2046–2055. [Google Scholar] [CrossRef]
- Chen, H.; Guan, B.; Chen, S.; Yang, D.; Shen, J. Peroxynitrite activates NLRP3 inflammasome and contributes to hemorrhagic transformation and poor outcome in ischemic stroke with hyperglycemia. Free. Radic. Biol. Med. 2021, 165, 171–183. [Google Scholar] [CrossRef]
- Yang, Z.; Huang, C.; Wen, X.; Liu, W.; Huang, X.; Li, Y.; Zang, J.; Weng, Z.; Lu, D.; Tsang, C.K.; et al. Circular RNA circ-FoxO3 attenuates blood-brain barrier damage by inducing autophagy during ischemia/reperfusion. Mol. Ther. 2022, 30, 1275–1287. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.; Yang, Y.; DeMars, K.M.; Rosenberg, G.A.; Candelario-Jalil, E. Genetic deletion or pharmacological inhibition of cyclooxygenase-2 reduces blood-brain barrier damage in experimental ischemic stroke. Front. Neurol. 2020, 11, 887. [Google Scholar] [CrossRef] [PubMed]
- Gliem, M.; Mausberg, A.K.; Lee, J.; Simiantonakis, I.; van Rooijen, N.; Hartung, H.; Jander, S. Macrophages prevent hemorrhagic infarct transformation in murine stroke models. Ann. Neurol. 2012, 71, 743–752. [Google Scholar] [CrossRef]
- Chen, H.; Guan, B.; Wang, B.; Pu, H.; Bai, X.; Chen, X.; Liu, J.; Li, C.; Qiu, J.; Yang, D.; et al. Glycyrrhizin prevents hemorrhagic transformation and improves neurological outcome in ischemic stroke with delayed thrombolysis through targeting peroxynitrite-mediated HMGB1 signaling. Transl. Stroke Res. 2020, 11, 967–982. [Google Scholar] [CrossRef]
- Yao, Y.; Liu, F.; Gu, Z.; Wang, J.; Xu, L.; Yu, Y.; Cai, J.; Ren, R. Emerging diagnostic markers and therapeutic targets in post-stroke hemorrhagic transformation and brain edema. Front. Mol. Neurosci. 2023, 16, 1286351. [Google Scholar] [CrossRef]
- Xia, X.; Niu, H.; Ma, Y.; Qu, B.; He, M.; Yu, K.; Wang, E.; Zhang, L.; Gu, J.; Liu, G. LncRNA CCAT1 protects astrocytes against OGD/R-induced damage by targeting the miR-218/NFAT5-signaling axis. Cell. Mol. Neurobiol. 2020, 40, 1383–1393. [Google Scholar] [CrossRef]
- Yang, Y.; Zhao, F.; Yuan, Z.; Wang, C.; Chen, K.; Xiao, W. Inhibition of miR-218-5p reduces myocardial ischemia–reperfusion injury in a Sprague-Dawley rat model by reducing oxidative stress and inflammation through MEF2C/NF-κB pathway. Int. Immunopharmacol. 2021, 101, 108299. [Google Scholar] [CrossRef]
- Ren, X.; Wang, Z.; Guo, C. MiR-195-5p ameliorates cerebral ischemia-reperfusion injury by regulating the PTEN-AKT signaling pathway. Neuropsychiatr. Dis. Treat. 2021, 17, 1231–1242. [Google Scholar] [CrossRef]
- Wu, X.; Fu, S.; Liu, Y.; Luo, H.; Li, F.; Wang, Y.; Gao, M.; Cheng, Y.; Xie, Z. NDP-MSH binding melanocortin-1 receptor ameliorates neuroinflammation and BBB disruption through CREB/Nr4a1/NF-κB pathway after intracerebral hemorrhage in mice. J. Neuroinflamm. 2019, 16, 192. [Google Scholar] [CrossRef]
- Wang, Y.; Yang, R.; Yan, F.; Jin, Y.; Liu, X.; Wang, T. Medicarpin protects cerebral microvascular endothelial cells against oxygen-glucose deprivation/reoxygenation-induced injury via the PI3K/Akt/FoxO pathway: A study of network pharmacology analysis and experimental validation. Neurochem. Res. 2022, 47, 347–357. [Google Scholar] [CrossRef]
- Tao, W.; Zhang, G.; Liu, C.; Jin, L.; Li, X.; Yang, S. Low-dose LPS alleviates early brain injury after SAH by modulating microglial M1/M2 polarization via USP19/FOXO1/IL-10/IL-10R1 signaling. Redox Biol. 2023, 66, 102863. [Google Scholar] [CrossRef] [PubMed]
- Hafez, S.; Abdelsaid, M.; Fagan, S.C.; Ergul, A. Peroxynitrite-induced tyrosine nitration contributes to matrix metalloprotease-3 activation: Relevance to hyperglycemic ischemic brain injury and tissue plasminogen activator. Neurochem. Res. 2018, 43, 259–266. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.-X.; Sun, Z.-Y.; Wang, F.-J.; Guo, H.; Chen, L.; Chai, L.-J.; Li, R.-L.; Hu, L.-M.; Wang, H. Shuxuetong injection protects cerebral microvascular endothelial cells against oxygen-glucose deprivation reperfusion. Neural Regen. Res. 2019, 14, 783–793. [Google Scholar] [CrossRef]
- Liu, C.; Tian, Q.; Wang, J.; He, P.; Han, S.; Guo, Y.; Yang, C.; Wang, G.; Wei, H.; Li, M. Blocking P2RX7 attenuates ferroptosis in endothelium and reduces HG-induced hemorrhagic transformation after MCAO by inhibiting ERK1/2 and P53 signaling pathways. Mol. Neurobiol. 2023, 60, 460–479. [Google Scholar] [CrossRef]


| MicroRNAs | In Vivo Stroke Model | In-Vitro OGD/R Model | ||||||
|---|---|---|---|---|---|---|---|---|
| Peri-Infarct | Infarction Core | Neuron | Astrocyte | Microglia | BMEC | Pericyte | ||
| 1 | miR-1-3p | NS | NS | - | - | - | - | - |
| 2 | miR-25-5p | NS | NS | - | - | - | - | - |
| 3 | miR-27b-3p | NS | NS | - | - | - | - | - |
| 4 | miR-29a-5p | Down | Down | NS | Down | NS | NS | NS |
| 5 | miR-29c-3p | Down | Down | Up | Down | Up | Down | Up |
| 6 | miR-30a-3p | NS | NS | - | - | - | - | - |
| 7 | miR-126a-5p | Down | Down | NS | Down | Up | Down | NS |
| 8 | miR-132-3p | Down | Down | Down | Down | Down | Up | Down |
| 9 | miR-136-3p | Down | Down | Down | NS | Down | NS | Up |
| 10 | miR-138-5p | NS | NS | - | - | - | - | - |
| 11 | miR-139-5p | NS | Down | - | - | - | - | - |
| 12 | miR-142-3p | Down | Down | NS | Down | NS | Down | NS |
| 13 | miR-153-5p | Down | Down | Down | Down | NS | Up | Up |
| 14 | miR-195-3p | Up | Up | Down | NS | NS | Up | Up |
| 15 | miR-218a-5p | Down | Down | Down | Down | Down | Up | Down |
| 16 | miR-219a-2-3p | Down | Down | Up | Down | NS | NS | NS |
| 17 | miR-320-5p | NS | NS | - | - | - | - | - |
| 18 | miR-337-3p | NS | Down | - | - | - | - | - |
| 19 | miR-369-5p | Down | Down | Down | Down | NS | NS | NS |
| 20 | miR-376a-5p | Down | Down | Down | NS | NS | NS | NS |
| 21 | miR-376b-5p | Down | Down | Down | NS | Up | NS | Up |
| 22 | miR-381-3p | NS | Up | - | - | - | - | - |
| 23 | miR-383-5p | Down | Down | Down | Down | NS | NS | NS |
| 24 | miR-487b-5p | NS | NS | - | - | - | - | - |
| 25 | miR-582-3p | NS | Down | - | - | - | - | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhuang, J.-K.; Huang, Z.-R.; Qin, W.; Li, C.-L.; Li, Q.; Xiang, C.; Tuo, Y.-H.; Liu, Z.; Chen, Q.-Y.; Shi, Z.-S. MicroRNAs Associated with Parenchymal Hematoma After Endovascular Mechanical Reperfusion for Acute Ischemic Stroke in Rats. Biomedicines 2025, 13, 449. https://doi.org/10.3390/biomedicines13020449
Zhuang J-K, Huang Z-R, Qin W, Li C-L, Li Q, Xiang C, Tuo Y-H, Liu Z, Chen Q-Y, Shi Z-S. MicroRNAs Associated with Parenchymal Hematoma After Endovascular Mechanical Reperfusion for Acute Ischemic Stroke in Rats. Biomedicines. 2025; 13(2):449. https://doi.org/10.3390/biomedicines13020449
Chicago/Turabian StyleZhuang, Jin-Kun, Zhong-Run Huang, Wang Qin, Chang-Luo Li, Qi Li, Chun Xiang, Yong-Hua Tuo, Zhong Liu, Qian-Yu Chen, and Zhong-Song Shi. 2025. "MicroRNAs Associated with Parenchymal Hematoma After Endovascular Mechanical Reperfusion for Acute Ischemic Stroke in Rats" Biomedicines 13, no. 2: 449. https://doi.org/10.3390/biomedicines13020449
APA StyleZhuang, J.-K., Huang, Z.-R., Qin, W., Li, C.-L., Li, Q., Xiang, C., Tuo, Y.-H., Liu, Z., Chen, Q.-Y., & Shi, Z.-S. (2025). MicroRNAs Associated with Parenchymal Hematoma After Endovascular Mechanical Reperfusion for Acute Ischemic Stroke in Rats. Biomedicines, 13(2), 449. https://doi.org/10.3390/biomedicines13020449







