Neuroprotective Effects of Dehydroepiandrosterone Sulphate Against Aβ Toxicity and Accumulation in Cellular and Animal Model of Alzheimer’s Disease
Abstract
1. Introduction
2. Materials and Methods
2.1. Cellular Model of AD
2.1.1. Primary Neuronal Culture
2.1.2. Preparation and Characterization of Aβ42 Monomers, Oligomers and Polymers
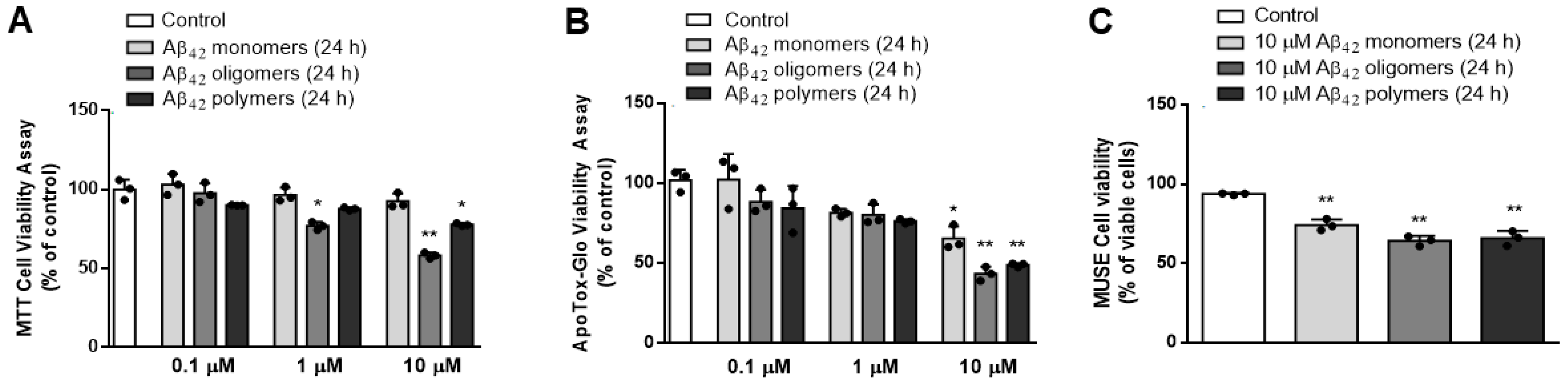
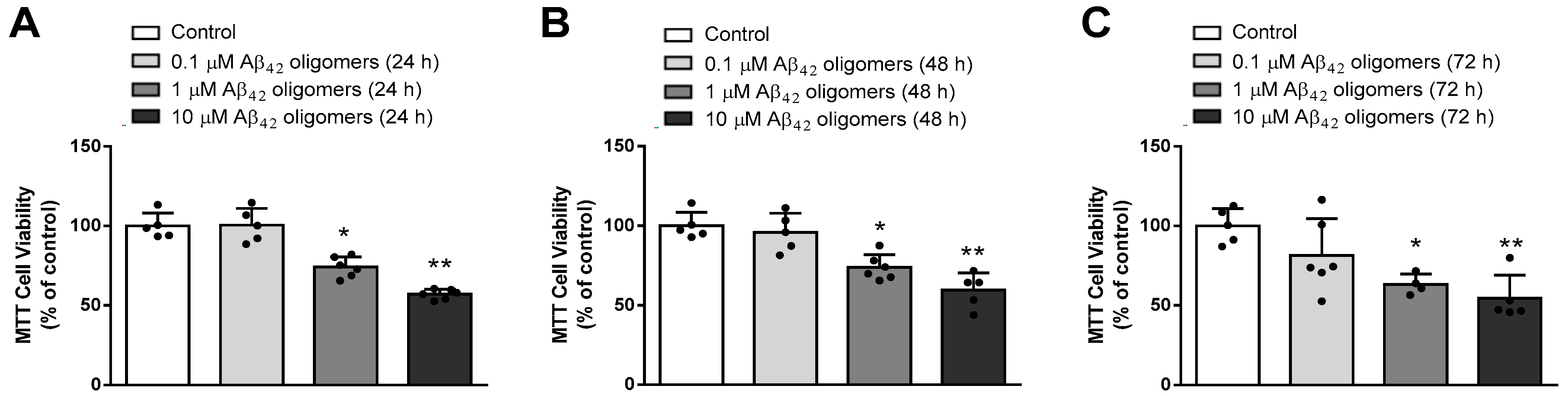
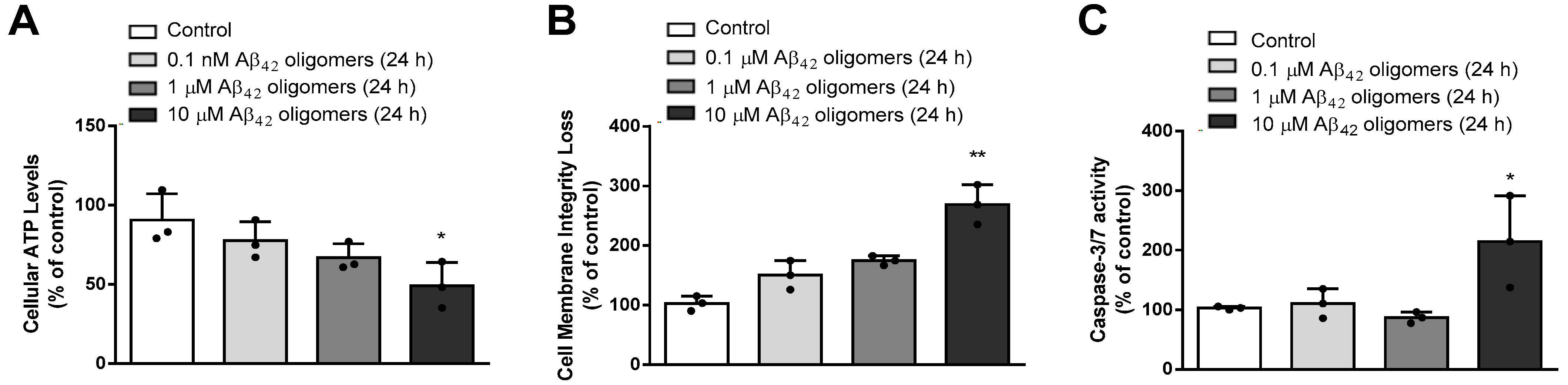
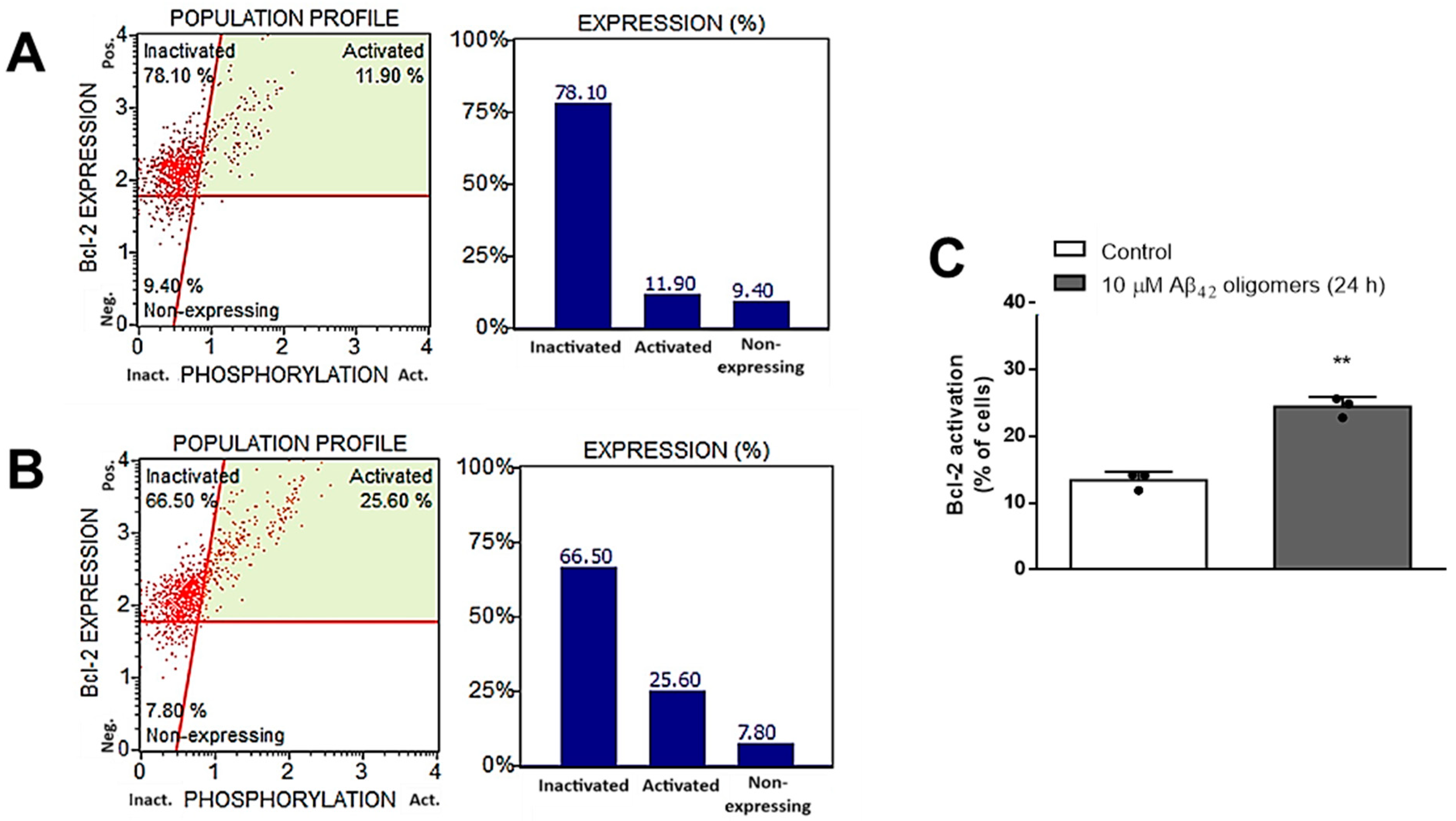
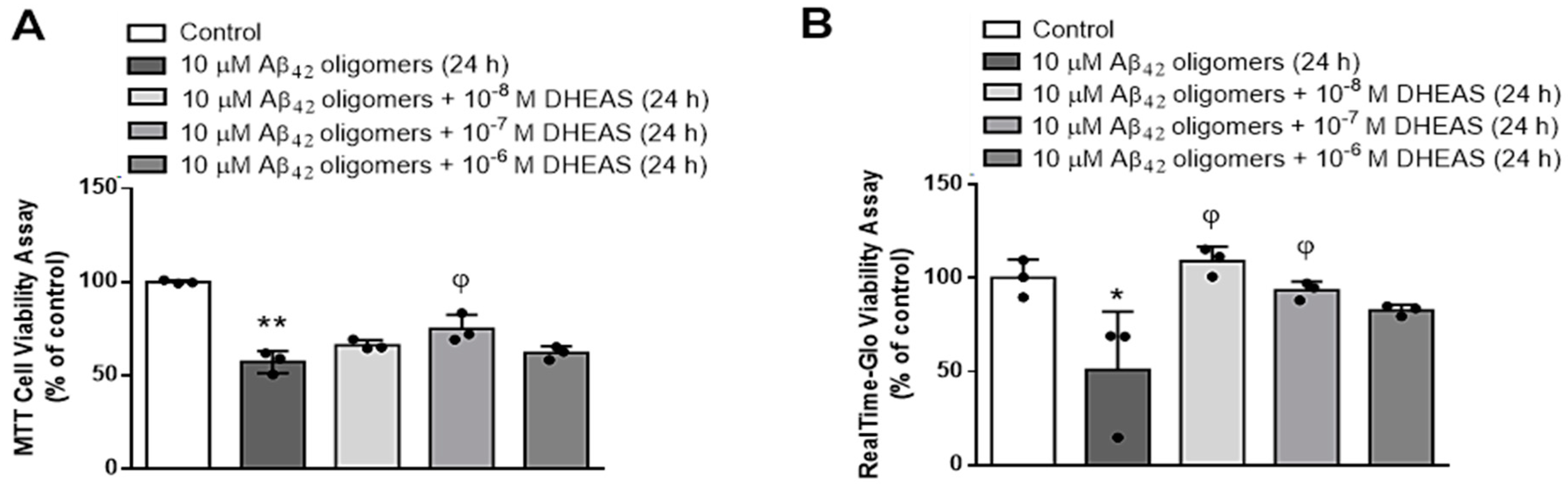
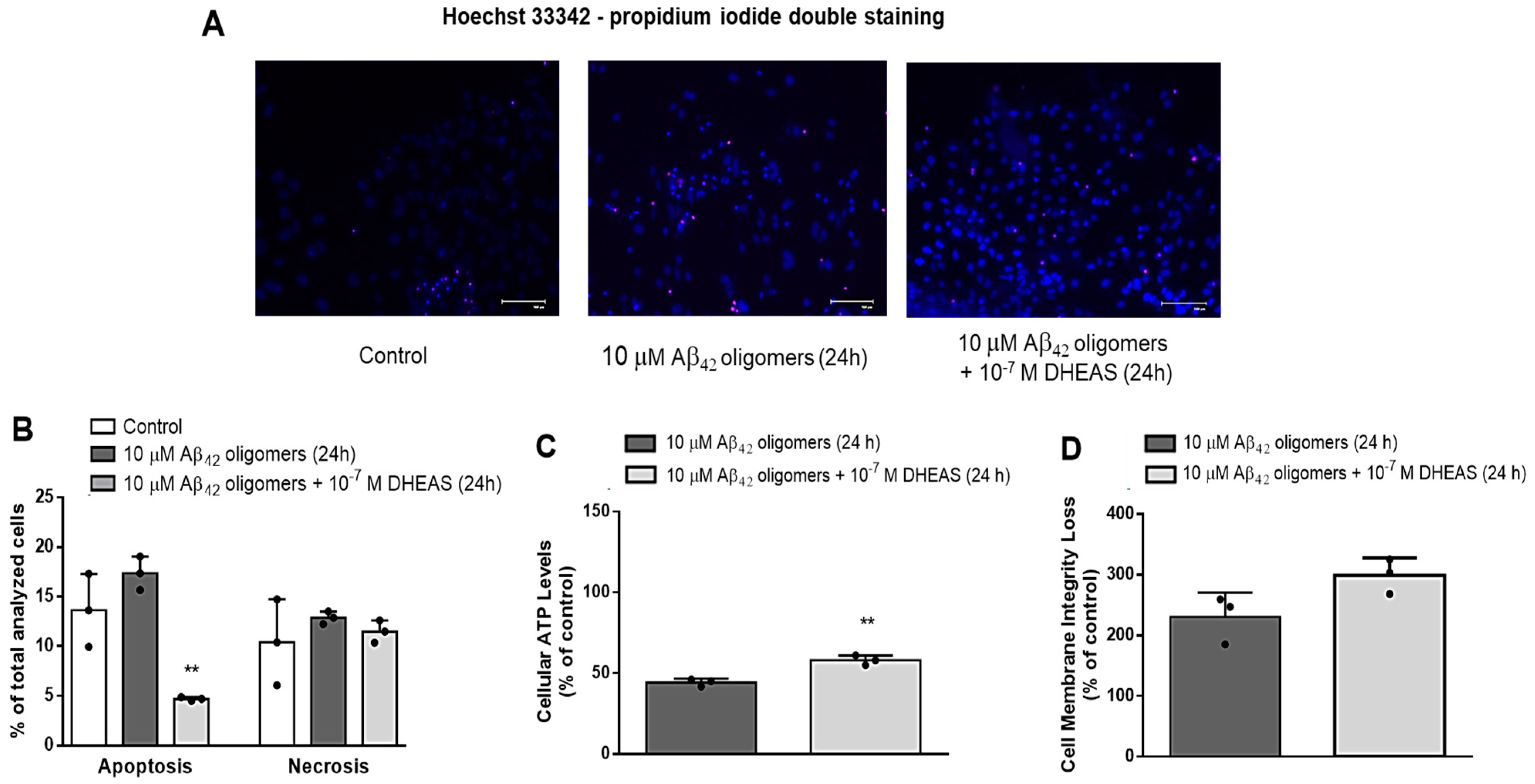
2.1.3. Cell Treatment and Determination of Viability, Cytotoxicity and Apoptosis
2.1.4. RNA Expression Analysis
2.2. Animal Model of AD
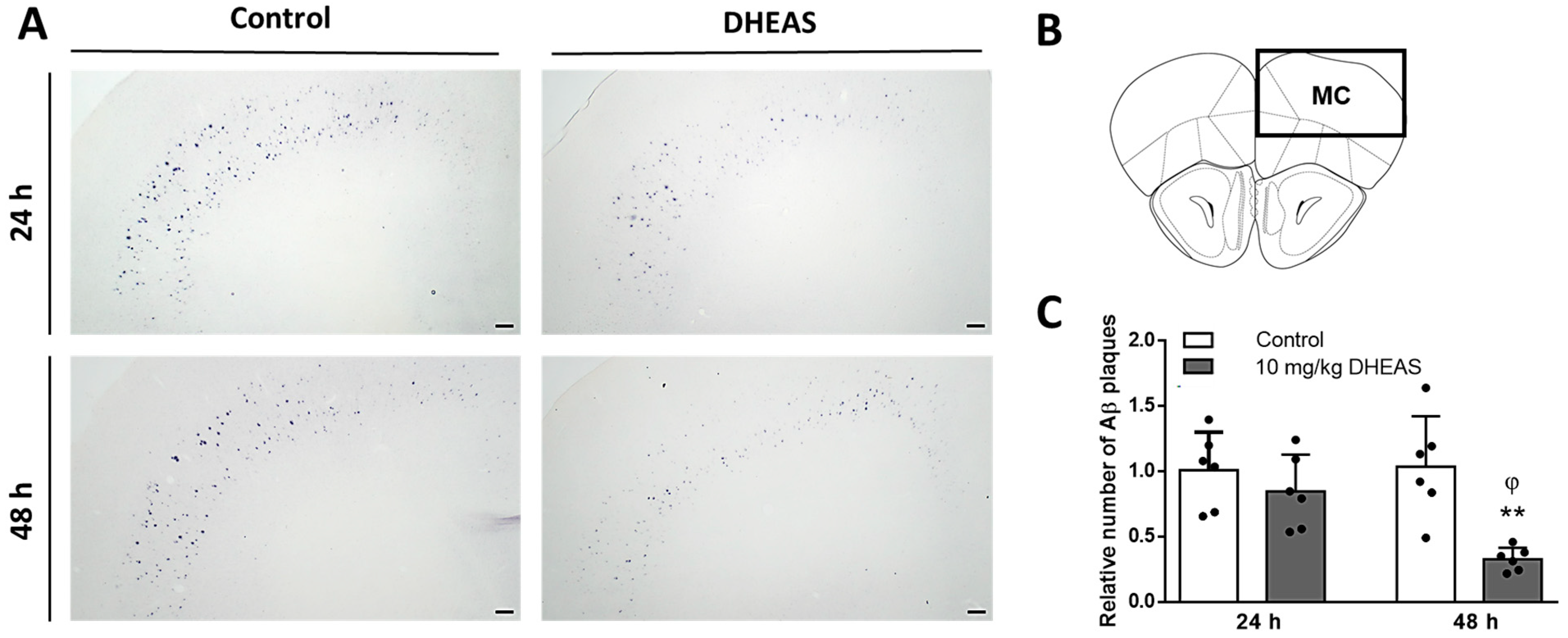
2.2.1. 3xTg-AD Mice
2.2.2. DHEAS Treatment and Brain Tissue Processing

2.2.3. Immunohistochemistry
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Babić, M.; Svob Štrac, D.; Mück-Šeler, D.; Pivac, N.; Stanić, G.; Hof, P.R.; Simić, G. Update on the core and developing cerebrospinal fluid biomarkers for Alzheimer disease. Croat. Med. J. 2014, 55, 347–365. [Google Scholar] [CrossRef]
- Tiwari, S.; Atluri, V.; Kaushik, A.; Yndart, A.; Nair, M. Alzheimer’s disease: Pathogenesis, diagnostics, and therapeutics. Int. J. Nanomed. 2019, 14, 5541–5554. [Google Scholar] [CrossRef] [PubMed]
- Haass, C.; Selkoe, D.J. Soluble protein oligomers in neurodegeneration: Lessons from the Alzheimer’s amyloid beta-peptide. Nat. Rev. Mol. Cell Biol. 2007, 8, 101–112. [Google Scholar] [CrossRef] [PubMed]
- Crouch, P.J.; Harding, S.M.; White, A.R.; Camakaris, J.; Bush, A.I.; Masters, C.L. Mechanisms of A beta mediated neurodegeneration in Alzheimer’s disease. Int. J. Biochem. Cell Biol. 2008, 40, 181–198. [Google Scholar] [CrossRef] [PubMed]
- Breijyeh, Z.; Karaman, R. Comprehensive Review on Alzheimer’s Disease: Causes and Treatment. Molecules 2020, 25, 5789. [Google Scholar] [CrossRef]
- Cummings, J. Anti-Amyloid Monoclonal Antibodies are Transformative Treatments that Redefine Alzheimer’s Disease Therapeutics. Drugs 2023, 83, 569–576. [Google Scholar] [CrossRef]
- Doran, S.J.; Sawyer, R.P. Risk factors in developing amyloid related imaging abnormalities (ARIA) and clinical implications. Front. Neurosci. 2024, 18, 1326784. [Google Scholar] [CrossRef] [PubMed]
- Hunter, P. The controversy around anti-amyloid antibodies for treating Alzheimer’s disease: The European Medical Agency’s ruling against the latest anti-amyloid drugs highlights the ongoing debate about their safety and efficacy. EMBO Rep. 2024, 25, 5227–5231. [Google Scholar] [CrossRef]
- Auchus, R.J. Overview of dehydroepiandrosterone biosynthesis. Semin. Reprod. Med. 2004, 22, 281–288. [Google Scholar] [CrossRef]
- Mueller, J.W.; Gilligan, L.C.; Idkowiak, J.; Arlt, W.; Foster, P.A. The Regulation of Steroid Action by Sulfation and Desulfation. Endocr. Rev. 2015, 36, 526–563. [Google Scholar] [CrossRef]
- Baulieu, E.E.; Robel, P. Dehydroepiandrosterone (DHEA) and dehydroepiandrosterone sulfate (DHEAS) as neuroactive neurosteroids. Proc. Natl. Acad. Sci. USA 1998, 95, 4089–4091. [Google Scholar] [CrossRef] [PubMed]
- Friess, E.; Schiffelholz, T.; Steckler, T.; Steiger, A. Dehydroepiandrosterone--a neurosteroid. Eur. J. Clin. Investig. 2000, 30, 46–50. [Google Scholar] [CrossRef] [PubMed]
- Tannenbaum, C.; Barrett-Connor, E.; Laughlin, G.A.; Platt, R.W. A longitudinal study of dehydroepiandrosterone sulphate (DHEAS) change in older men and women: The Rancho Bernardo Study. Eur. J. Endocrinol. 2004, 151, 717–725. [Google Scholar] [CrossRef][Green Version]
- Berr, C.; Lafont, S.; Debuire, B.; Dartigues, J.F.; Baulieu, E.E. Relationships of dehydroepiandrosterone sulfate in the elderly with functional, psychological, and mental status, and short-term mortality: A French community-based study. Proc. Natl. Acad. Sci. USA 1996, 93, 13410–13415. [Google Scholar] [CrossRef]
- Pan, X.; Wu, X.; Kaminga, A.C.; Wen, S.W.; Liu, A. Dehydroepiandrosterone and Dehydroepiandrosterone Sulfate in Alzheimer’s Disease: A Systematic Review and Meta-Analysis. Front. Aging Neurosci. 2019, 11, 61. [Google Scholar] [CrossRef]
- Wolkowitz, O.M.; Reus, V.I. Neuropsychiatric Effects of Dehydroepiandrosterone (DHEA). In Dehydroepiandrosterone (DHEA): Biochemical, Physiological and Clinical Aspects; Kalimi, M., Regelson, W., Eds.; De Gruyter: Berlin, NY, USA, 2000; pp. 271–298. [Google Scholar]
- Wolf, O.T.; Kirschbaum, C. Actions of dehydroepiandrosterone and its sulfate in the central nervous system: Effects on cognition and emotion in animals and humans. Brain Res. Brain Res. Rev. 1999, 30, 264–288. [Google Scholar] [CrossRef]
- Strac, D.S.; Konjevod, M.; Perkovic, M.N.; Tudor, L.; Erjavec, G.N.; Pivac, N. Dehydroepiandrosterone (DHEA) and its Sulphate (DHEAS) in Alzheimer’s Disease. Curr. Alzheimer Res. 2020, 17, 141–157. [Google Scholar] [CrossRef]
- Maninger, N.; Wolkowitz, O.M.; Reus, V.I.; Epel, E.S.; Mellon, S.H. Neurobiological and neuropsychiatric effects of dehydroepiandrosterone (DHEA) and DHEA sulfate (DHEAS). Front. Neuroendocrinol. 2009, 30, 65–91. [Google Scholar] [CrossRef]
- Pérez-Neri, I.; Montes, S.; Ojeda-López, C.; Ramírez-Bermúdez, J.; Ríos, C. Modulation of neurotransmitter systems by dehydroepiandrosterone and dehydroepiandrosterone sulfate: Mechanism of action and relevance to psychiatric disorders. Prog. Neuropsychopharmacol. Biol. Psychiatry 2008, 32, 1118–1130. [Google Scholar] [CrossRef]
- Clark, B.J.; Prough, R.A.; Klinge, C.M. Mechanisms of Action of Dehydroepiandrosterone. Vitam. Horm. 2018, 108, 29–73. [Google Scholar] [CrossRef]
- Li, L.; Xu, B.; Zhu, Y.; Chen, L.; Sokabe, M.; Chen, L. DHEA prevents Aβ25-35-impaired survival of newborn neurons in the dentate gyrus through a modulation of PI3K-Akt-mTOR signaling. Neuropharmacology 2010, 59, 323–333. [Google Scholar] [CrossRef]
- Mao, X.; Barger, S.W. Neuroprotection by dehydroepiandrosterone-sulfate: Role of an NFkappaB-like factor. Neuroreport 1998, 9, 759–763. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Li Bs Ma, W.; Barker, J.L.; Chang, Y.H.; Zhao, W.; Rubinow, D.R. Dehydroepiandrosterone (DHEA) and its sulfated derivative (DHEAS) regulate apoptosis during neurogenesis by triggering the Akt signaling pathway in opposing ways. Brain Res. Mol. Brain Res. 2002, 98, 58–66. [Google Scholar] [CrossRef] [PubMed]
- Asaba, H.; Hosoya, K.; Takanaga, H.; Ohtsuki, S.; Tamura, E.; Takizawa, T.; Terasaki, T. Blood-brain barrier is involved in the efflux transport of a neuroactive steroid, dehydroepiandrosterone sulfate, via organic anion transporting polypeptide 2. J. Neurochem. 2000, 75, 1907–1916. [Google Scholar] [CrossRef] [PubMed]
- Qaiser, M.Z.; Dolman, D.E.M.; Begley, D.J.; Abbott, N.J.; Cazacu-Davidescu, M.; Corol, D.I.; Fry, J.P. Uptake and metabolism of sulphated steroids by the blood-brain barrier in the adult male rat. J. Neurochem. 2017, 142, 672–685. [Google Scholar] [CrossRef]
- Lapchak, P.A.; Araujo, D.M. Preclinical development of neurosteroids as neuroprotective agents for the treatment of neurodegenerative diseases. Int. Rev. Neurobiol. 2001, 46, 379–397. [Google Scholar] [CrossRef] [PubMed]
- Powrie, Y.S.L.; Smith, C. Central intracrine DHEA synthesis in ageing-related neuroinflammation and neurodegeneration: Therapeutic potential? J. Neuroinflammation 2018, 15, 289. [Google Scholar] [CrossRef] [PubMed]
- Dhatariya, K.K.; Nair, K.S. Dehydroepiandrosterone: Is there a role for replacement? Mayo Clin. Proc. 2003, 78, 1257–1273. [Google Scholar] [CrossRef] [PubMed]
- Olech, E.; Merrill, J.T. DHEA supplementation: The claims in perspective. Cleve Clin. J. Med. 2005, 72, 965–966, 968, 970-1 passim. [Google Scholar] [CrossRef][Green Version]
- Gilad, I.; Shtaif, B.; Eshet, R.; Maayan, R.; Rehavi, M.; Weizman, A. Effect of dehydroepiandrosterone and its sulfate metabolite on neuronal cell viability in culture. Isr. Med. Assoc. J. 2001, 3, 639–643. [Google Scholar] [PubMed]
- Kurata, K.; Takebayashi, M.; Morinobu, S.; Yamawaki, S. beta-estradiol, dehydroepiandrosterone, and dehydroepiandrosterone sulfate protect against N-methyl-D-aspartate-induced neurotoxicity in rat hippocampal neurons by different mechanisms. J. Pharmacol. Exp. Ther. 2004, 311, 237–245. [Google Scholar] [CrossRef] [PubMed]
- Cardounel, A.; Regelson, W.; Kalimi, M. Dehydroepiandrosterone protects hippocampal neurons against neurotoxin-induced cell death: Mechanism of action. Proc. Soc. Exp. Biol. Med. 1999, 222, 145–149. [Google Scholar] [CrossRef] [PubMed]
- El Bitar, F.; Meunier, J.; Villard, V.; Alméras, M.; Krishnan, K.; Covey, D.F.; Maurice, T.; Akwa, Y. Neuroprotection by the synthetic neurosteroid enantiomers ent-PREGS and ent-DHEAS against Aβ25–35 peptide-induced toxicity in vitro and in vivo in mice. Psychopharmacology 2014, 231, 3293–3312. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.Y.; Feng, Y.H.; Kao, T.J.; Chen, H.C.; Chen, G.Y.; Ko, C.Y.; Hsu, T.I. Exploring neuron-specific steroid synthesis and DHEAS therapy in Alzheimer’s disease. J. Steroid Biochem. Mol. Biol. 2024, 243, 106585. [Google Scholar] [CrossRef]
- Edwards, M.A.; Loxley, R.A.; Williams, A.J.; Connor, M.; Phillips, J.K. Lack of functional expression of NMDA receptors in PC12 cells. Neurotoxicology 2007, 28, 876–885. [Google Scholar] [CrossRef] [PubMed]
- LePage, K.T.; Dickey, R.W.; Gerwick, W.H.; Jester, E.L.; Murray, T.F. On the use of neuro-2a neuroblastoma cells versus intact neurons in primary culture for neurotoxicity studies. Crit. Rev. Neurobiol. 2005, 17, 27–50. [Google Scholar] [CrossRef] [PubMed]
- Kovalevich, J.; Langford, D. Considerations for the use of SH-SY5Y neuroblastoma cells in neurobiology. Methods Mol. Biol. 2013, 1078, 9–21. [Google Scholar] [CrossRef]
- Verma, M.; Vats, A.; Taneja, V. Toxic species in amyloid disorders: Oligomers or mature fibrils. Ann. Indian. Acad. Neurol. 2015, 18, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Jarero-Basulto, J.J.; Gasca-Martínez, Y.; Rivera-Cervantes, M.C.; Gasca-Martínez, D.; Carrillo-González, N.J.; Beas-Zárate, C.; Gudiño-Cabrera, G. Cytotoxic Effect of Amyloid-β1-42 Oligomers on Endoplasmic Reticulum and Golgi Apparatus Arrangement in SH-SY5Y Neuroblastoma Cells. NeuroSci 2024, 5, 141–157. [Google Scholar] [CrossRef]
- Ganbat, D.; Jeon, J.K.; Lee, Y.; Kim, S.S. Exploring the Pathological Effect of Aβ42 Oligomers on Neural Networks in Primary Cortical Neuron Culture. Int. J. Mol. Sci. 2023, 24, 6641. [Google Scholar] [CrossRef] [PubMed]
- Chafekar, S.M.; Hoozemans, J.J.; Zwart, R.; Baas, F.; Scheper, W. Abeta 1-42 induces mild endoplasmic reticulum stress in an aggregation state-dependent manner. Antioxid. Redox Signal 2007, 9, 2245–2254. [Google Scholar] [CrossRef]
- Picone, P.; Carrotta, R.; Montana, G.; Nobile, M.R.; San Biagio, P.L.; Di Carlo, M. Abeta oligomers and fibrillar aggregates induce different apoptotic pathways in LAN5 neuroblastoma cell cultures. Biophys. J. 2009, 96, 4200–4211. [Google Scholar] [CrossRef] [PubMed]
- Maurice, T.; Su, T.P.; Privat, A. Sigma1 (σ1) receptor agonists and neurosteroids attenuate B25-35-amyloid peptide-induced amnesia in mice through a common mechanism. Neuroscience 1998, 83, 413–428. [Google Scholar] [CrossRef]
- Belfiore, R.; Rodin, A.; Ferreira, E.; Velazquez, R.; Branca, C.; Caccamo, A.; Oddo, S. Temporal and regional progression of Alzheimer’s disease-like pathology in 3xTg-AD mice. Aging Cell 2019, 18, e12873. [Google Scholar] [CrossRef]
- Oddo, S.; Caccamo, A.; Kitazawa, M.; Tseng, B.P.; LaFerla, F.M. Amyloid deposition precedes tangle formation in a triple transgenic model of Alzheimer’s disease. Neurobiol. Aging 2003, 24, 1063–1070. [Google Scholar] [CrossRef]
- Oddo, S.; Caccamo, A.; Shepherd, J.D.; Murphy, M.P.; Golde, T.E.; Kayed, R.; Metherate, R.; Mattson, M.P.; Akbari, Y.; LaFerla, F.M. Triple-transgenic model of Alzheimer’s disease with plaques and tangles: Intracellular Abeta and synaptic dysfunction. Neuron 2003, 39, 409–421. [Google Scholar] [CrossRef] [PubMed]
- Hilgenberg, L.G.; Smith, M.A. Preparation of dissociated mouse cortical neuron cultures. J. Vis. Exp. 2007, 10, 562. [Google Scholar] [CrossRef]
- Stine, W.B.; Jungbauer, L.; Yu, C.; LaDu, M.J. Preparing synthetic Aβ in different aggregation states. Methods Mol. Biol. 2011, 670, 13–32. [Google Scholar] [CrossRef]
- Radić, T.M.; Svetličić, V.; Zutić, V.; Boulgaropoulos, B. Seawater at the nanoscale: Marine gel imaged by atomic force microscopy. J. Mol. Recognit. 2011, 24, 397–405. [Google Scholar] [CrossRef] [PubMed]
- Pletikapić, G.; Radić, T.M.; Zimmermann, A.H.; Svetličić, V.; Pfannkuchen, M.; Marić, D.; Godrijan, J.; Zutić, V. AFM imaging of extracellular polymer release by marine diatom Cylindrotheca closterium (Ehrenberg) Reiman & J.C. Lewin. J. Mol. Recognit. 2011, 24, 436–445. [Google Scholar] [CrossRef] [PubMed]
- Farkas, S.; Szabó, A.; Török, B.; Sólyomvári, C.; Fazekas, C.L.; Bánrévi, K.; Correia, P.; Chaves, T.; Zelena, D. Ovariectomy-induced hormone deprivation aggravates Aβ1-42 deposition in the basolateral amygdala and cholinergic fiber loss in the cortex but not cognitive behavioral symptoms in a triple transgenic mouse model of Alzheimer’s disease. Front. Endocrinol. 2022, 13, 985424. [Google Scholar] [CrossRef]
- Paxinos, G.; Franklin, K.B.J. The Mouse Brain in Stereotaxic Coordinates, 2nd ed.; Academic Press: Cambridge, MA, USA, 2001; Volume 1. [Google Scholar]
- Hardy, J.A.; Higgins, G.A. Alzheimer’s disease: The amyloid cascade hypothesis. Science 1992, 256, 184–185. [Google Scholar] [CrossRef]
- Karran, E.; De Strooper, B. The amyloid hypothesis in Alzheimer disease: New insights from new therapeutics. Nat. Rev. Drug Discov. 2022, 21, 306–318. [Google Scholar] [CrossRef] [PubMed]
- Sandebring, A.; Welander, H.; Winblad, B.; Graff, C.; Tjernberg, L.O. The pathogenic aβ43 is enriched in familial and sporadic Alzheimer disease. PLoS ONE 2013, 8, e55847. [Google Scholar] [CrossRef]
- Zhang, Y.; Chen, H.; Li, R.; Sterling, K.; Song, W. Amyloid β-based therapy for Alzheimer’s disease: Challenges, successes and future. Signal Transduct. Target. Ther. 2023, 8, 248. [Google Scholar] [CrossRef] [PubMed]
- Kienlen-Campard, P.; Miolet, S.; Tasiaux, B.; Octave, J.N. Intracellular amyloid-beta 1-42, but not extracellular soluble amyloid-beta peptides, induces neuronal apoptosis. J. Biol. Chem. 2002, 277, 15666–15670. [Google Scholar] [CrossRef] [PubMed]
- Bhatia, S.; Rawal, R.; Sharma, P.; Singh, T.; Singh, M.; Singh, V. Mitochondrial Dysfunction in Alzheimer’s Disease: Opportunities for Drug Development. Curr. Neuropharmacol. 2022, 20, 675–692. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Zhao, F.; Ma, X.; Perry, G.; Zhu, X. Mitochondria dysfunction in the pathogenesis of Alzheimer’s disease: Recent advances. Mol. Neurodegener. 2020, 15, 30. [Google Scholar] [CrossRef]
- Goel, P.; Chakrabarti, S.; Goel, K.; Bhutani, K.; Chopra, T.; Bali, S. Neuronal cell death mechanisms in Alzheimer’s disease: An insight. Front. Mol. Neurosci. 2022, 15, 937133. [Google Scholar] [CrossRef]
- Fricker, M.; Tolkovsky, A.M.; Borutaite, V.; Coleman, M.; Brown, G.C. Neuronal Cell Death. Physiol. Rev. 2018, 98, 813–880. [Google Scholar] [CrossRef] [PubMed]
- Selznick, L.A.; Zheng, T.S.; Flavell, R.A.; Rakic, P.; Roth, K.A. Amyloid beta-induced neuronal death is bax-dependent but caspase-independent. J. Neuropathol. Exp. Neurol. 2000, 59, 271–279. [Google Scholar] [CrossRef]
- Paradis, E.; Douillard, H.; Koutroumanis, M.; Goodyer, C.; LeBlanc, A. Amyloid beta peptide of Alzheimer’s disease downregulates Bcl-2 and upregulates bax expression in human neurons. J. Neurosci. 1996, 16, 7533–7539. [Google Scholar] [CrossRef]
- Lemasters, J.J.; Qian, T.; Bradham, C.A.; Brenner, D.A.; Cascio, W.E.; Trost, L.C.; Nishimura, Y.; Nieminen, A.L.; Herman, B. Mitochondrial dysfunction in the pathogenesis of necrotic and apoptotic cell death. J. Bioenerg. Biomembr. 1999, 31, 305–319. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Dorstyn, L.; Lim, Y. The role of caspases as executioners of apoptosis. Biochem. Soc. Trans. 2022, 50, 33–45. [Google Scholar] [CrossRef] [PubMed]
- Orrenius, S.; Gogvadze, V.; Zhivotovsky, B. Mitochondrial oxidative stress: Implications for cell death. Annu. Rev. Pharmacol. Toxicol. 2007, 47, 143–183. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Che, X.; Zheng, Q.; Wu, A.; Pan, K.; Shao, A.; Wu, Q.; Zhang, J.; Hong, Y. Caspases: A molecular switch node in the crosstalk between autophagy and apoptosis. Int. J. Biol. Sci. 2014, 10, 1072–1083. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, I.L.; Ferreiro, E.; Schmidt, J.; Cardoso, J.M.; Pereira, C.M.; Carvalho, A.L.; Oliveira, C.R.; Rego, A.C. Aβ and NMDAR activation cause mitochondrial dysfunction involving ER calcium release. Neurobiol. Aging 2015, 36, 680–692. [Google Scholar] [CrossRef] [PubMed]
- Rui, Y.; Zheng, J.Q. Amyloid β oligomers elicit mitochondrial transport defects and fragmentation in a time-dependent and pathway-specific manner. Mol. Brain 2016, 9, 79. [Google Scholar] [CrossRef] [PubMed]
- Arrázola, M.S.; Ramos-Fernández, E.; Cisternas, P.; Ordenes, D.; Inestrosa, N.C. Wnt Signaling Prevents the Aβ Oligomer-Induced Mitochondrial Permeability Transition Pore Opening Preserving Mitochondrial Structure in Hippocampal Neurons. PLoS ONE 2017, 12, e0168840. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.; Park, J.; Chang, K.T.; Lee, D.S. Peroxiredoxin 5 prevents amyloid-beta oligomer-induced neuronal cell death by inhibiting ERK-Drp1-mediated mitochondrial fragmentation. Free Radic. Biol. Med. 2016, 90, 184–194. [Google Scholar] [CrossRef] [PubMed]
- Krishtal, J.; Bragina, O.; Metsla, K.; Palumaa, P.; Tõugu, V. In situ fibrillizing amyloid-beta 1-42 induces neurite degeneration and apoptosis of differentiated SH-SY5Y cells. PLoS ONE 2017, 12, e0186636. [Google Scholar] [CrossRef]
- Camilleri, A.; Zarb, C.; Caruana, M.; Ostermeier, U.; Ghio, S.; Högen, T.; Schmidt, F.; Giese, A.; Vassallo, N. Mitochondrial membrane permeabilisation by amyloid aggregates and protection by polyphenols. Biochim. Biophys. Acta 2013, 1828, 2532–2543. [Google Scholar] [CrossRef]
- Kato-Negishi, M.; Kawahara, M. Neurosteroids block the increase in intracellular calcium level induced by Alzheimer’s β-amyloid protein in long-term cultured rat hippocampal neurons. Neuropsychiatr. Dis. Treat. 2008, 4, 209–218. [Google Scholar] [CrossRef]
- Li, L.L.; Wang, D.; Ge, C.Y.; Yu, L.; Zhao, J.L.; Ma, H.T. Dehydroepiandrosterone reduced lipid droplet accumulation via inhibiting cell proliferation and improving mitochondrial function in primary chicken hepatocytes. Physiol. Res. 2018, 67, 443–456. [Google Scholar] [CrossRef] [PubMed]
- Ding, X.; Wang, D.; Li, L.; Ma, H. Dehydroepiandrosterone ameliorates H2O2-induced Leydig cells oxidation damage and apoptosis through inhibition of ROS production and activation of PI3K/Akt pathways. Int. J. Biochem. Cell Biol. 2016, 70, 126–139. [Google Scholar] [CrossRef] [PubMed]
- Tsui, K.H.; Wang, P.H.; Lin, L.T.; Li, C.J. DHEA protects mitochondria against dual modes of apoptosis and necroptosis in human granulosa HO23 cells. Reproduction 2017, 154, 101–110. [Google Scholar] [CrossRef]
- Goguadze, N.; Zhuravliova, E.; Morin, D.; Mikeladze, D.; Maurice, T. Sigma-1 Receptor Agonists Induce Oxidative Stress in Mitochondria and Enhance Complex I Activity in Physiological Condition but Protect Against Pathological Oxidative Stress. Neurotox. Res. 2019, 35, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Pan, J.; Yao, Q.; Wang, Y.; Chang, S.; Li, C.; Wu, Y.; Shen, J.; Yang, R. The role of PI3K signaling pathway in Alzheimer’s disease. Front. Aging Neurosci. 2024, 16, 1459025. [Google Scholar] [CrossRef] [PubMed]
- Jacob, M.H.; Janner Dda, R.; Belló-Klein, A.; Llesuy, S.F.; Ribeiro, M.F. Dehydroepiandrosterone modulates antioxidant enzymes and Akt signaling in healthy Wistar rat hearts. J. Steroid Biochem. Mol. Biol. 2008, 112, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Charalampopoulos, I.; Alexaki, V.I.; Tsatsanis, C.; Minas, V.; Dermitzaki, E.; Lasaridis, I.; Vardouli, L.; Stournaras, C.; Margioris, A.N.; Castanas, E.; et al. Neurosteroids as endogenous inhibitors of neuronal cell apoptosis in aging. Ann. N. Y Acad. Sci. 2006, 1088, 139–152. [Google Scholar] [CrossRef]
- O’Keeffe, S.T.; Kazeem, H.; Philpott, R.M.; Playfer, J.R.; Gosney, M.; Lye, M. Gait disturbance in Alzheimer’s disease: A clinical study. Age Ageing 1996, 25, 313–316. [Google Scholar] [CrossRef] [PubMed]
- Collyer, T.A.; Murray, A.M.; Woods, R.L.; Storey, E.; Chong, T.T.; Ryan, J.; Orchard, S.G.; Brodtmann, A.; Srikanth, V.K.; Shah, R.C.; et al. Association of Dual Decline in Cognition and Gait Speed with Risk of Dementia in Older Adults. JAMA Netw. Open 2022, 5, e2214647. [Google Scholar] [CrossRef] [PubMed]
- Nyul-Toth, A.; DelFavero, J.; Mukli, P.; Tarantini, A.; Ungvari, A.; Yabluchanskiy, A.; Csiszar, A.; Ungvari, Z.; Tarantini, S. Early manifestation of gait alterations in the Tg2576 mouse model of Alzheimer’s disease. Geroscience 2021, 43, 1947–1957. [Google Scholar] [CrossRef] [PubMed]
- Bhandari, S.; Hu, H.; Chen, B.; Basilio, S.; Sartipi, P.; Sontag, H.; Shen, W.; Tao, R.; Prentice, H.; Wu, J.-Y. Assessing Behavioral and Psychological Symptoms of Dementia in a 3xTg-AD Mouse Model of Alzheimer’s Disease. Open Access J. Neurol. Neurosurg. 2024, 18, 555996. [Google Scholar] [CrossRef]
- Stover, K.R.; Campbell, M.A.; Van Winssen, C.M.; Brown, R.E. Analysis of motor function in 6-month-old male and female 3xTg-AD mice. Behav. Brain Res. 2015, 281, 16–23. [Google Scholar] [CrossRef] [PubMed]
- Oore, J.J.; Fraser, L.M.; Brown, R.E. Age-related changes in motor ability nad motor learning in triple transgenic (3×TG-AD) and control (B6129SF1/J) mice on the accelerating rotarod. Proc. Nov. Scotian Inst. Sci. 2013, 74, 281–296. [Google Scholar] [CrossRef]
- Caruso, D.; Barron, A.M.; Brown, M.A.; Abbiati, F.; Carrero, P.; Pike, C.J.; Garcia-Segura, L.M.; Melcangi, R.C. Age-related changes in neuroactive steroid levels in 3xTg-AD mice. Neurobiol. Aging 2013, 34, 1080–1089. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chen, S.; Wang, J.M.; Irwin, R.W.; Yao, J.; Liu, L.; Brinton, R.D. Allopregnanolone promotes regeneration and reduces β-amyloid burden in a preclinical model of Alzheimer’s disease. PLoS ONE 2011, 6, e24293. [Google Scholar] [CrossRef] [PubMed]
- Farr, S.A.; Banks, W.A.; Uezu, K.; Gaskin, F.S.; Morley, J.E. DHEAS improves learning and memory in aged SAMP8 mice but not in diabetic mice. Life Sci. 2004, 75, 2775–2785. [Google Scholar] [CrossRef] [PubMed]
- Xu, B.; Yang, R.; Chang, F.; Chen, L.; Xie, G.; Sokabe, M.; Chen, L. Neurosteroid PREGS protects neurite growth and survival of newborn neurons in the hippocampal dentate gyrus of APPswe/PS1dE9 mice. Curr. Alzheimer Res. 2012, 9, 361–372. [Google Scholar] [CrossRef] [PubMed]
- Nenezic, N.; Kostic, S.; Strac, D.S.; Grunauer, M.; Nenezic, D.; Radosavljevic, M.; Jancic, J.; Samardzic, J. Dehydroepiandrosterone (DHEA): Pharmacological Effects and Potential Therapeutic Application. Mini Rev. Med. Chem. 2023, 23, 941–952. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vuic, B.; Milos, T.; Kvak, E.; Konjevod, M.; Tudor, L.; Farkas, S.; Nedic Erjavec, G.; Nikolac Perkovic, M.; Zelena, D.; Svob Strac, D. Neuroprotective Effects of Dehydroepiandrosterone Sulphate Against Aβ Toxicity and Accumulation in Cellular and Animal Model of Alzheimer’s Disease. Biomedicines 2025, 13, 432. https://doi.org/10.3390/biomedicines13020432
Vuic B, Milos T, Kvak E, Konjevod M, Tudor L, Farkas S, Nedic Erjavec G, Nikolac Perkovic M, Zelena D, Svob Strac D. Neuroprotective Effects of Dehydroepiandrosterone Sulphate Against Aβ Toxicity and Accumulation in Cellular and Animal Model of Alzheimer’s Disease. Biomedicines. 2025; 13(2):432. https://doi.org/10.3390/biomedicines13020432
Chicago/Turabian StyleVuic, Barbara, Tina Milos, Erika Kvak, Marcela Konjevod, Lucija Tudor, Szidónia Farkas, Gordana Nedic Erjavec, Matea Nikolac Perkovic, Dora Zelena, and Dubravka Svob Strac. 2025. "Neuroprotective Effects of Dehydroepiandrosterone Sulphate Against Aβ Toxicity and Accumulation in Cellular and Animal Model of Alzheimer’s Disease" Biomedicines 13, no. 2: 432. https://doi.org/10.3390/biomedicines13020432
APA StyleVuic, B., Milos, T., Kvak, E., Konjevod, M., Tudor, L., Farkas, S., Nedic Erjavec, G., Nikolac Perkovic, M., Zelena, D., & Svob Strac, D. (2025). Neuroprotective Effects of Dehydroepiandrosterone Sulphate Against Aβ Toxicity and Accumulation in Cellular and Animal Model of Alzheimer’s Disease. Biomedicines, 13(2), 432. https://doi.org/10.3390/biomedicines13020432






