Peritoneal Endometriosis Impairs Ovarian Reserve and Increases Atresia in a Rat Model
Abstract
1. Introduction
2. Materials and Methods
2.1. Animal Model
2.2. Ovarian Morphology
2.3. Apoptosis Detection System
2.4. Western Blot
2.5. Co-Culture
2.6. Quantitative Real-Time Polymerase Chain Reaction (PCR) Analysis
2.7. Data Analysis
3. Results
3.1. Endometriosis Alters Folliculogenesis In Vivo
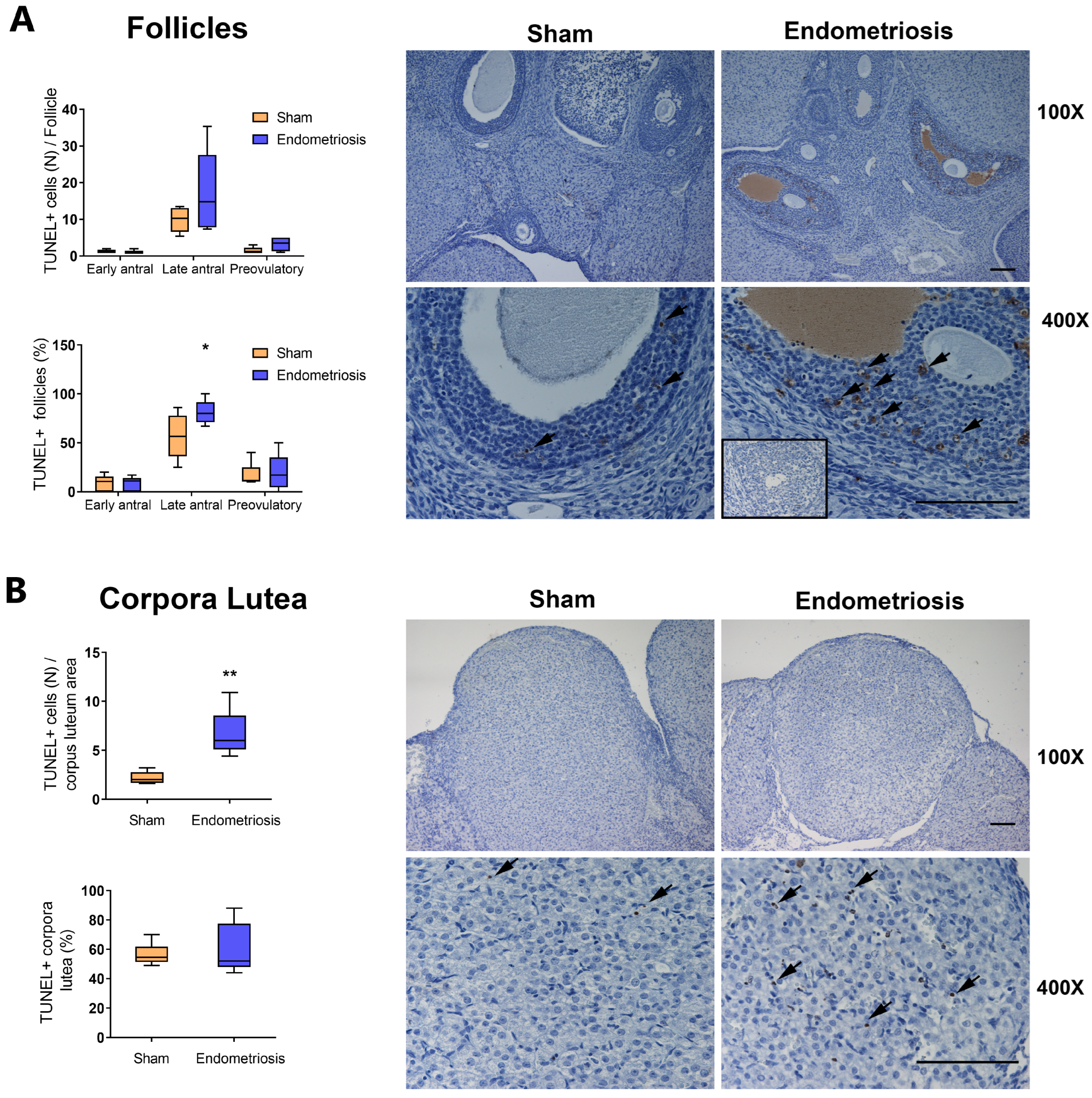
3.2. Endometriosis Increases Ovarian Apoptosis In Vivo
3.3. Endometriosis Alters the Expression of Proteins Related to Apoptosis in the Ovary In Vivo
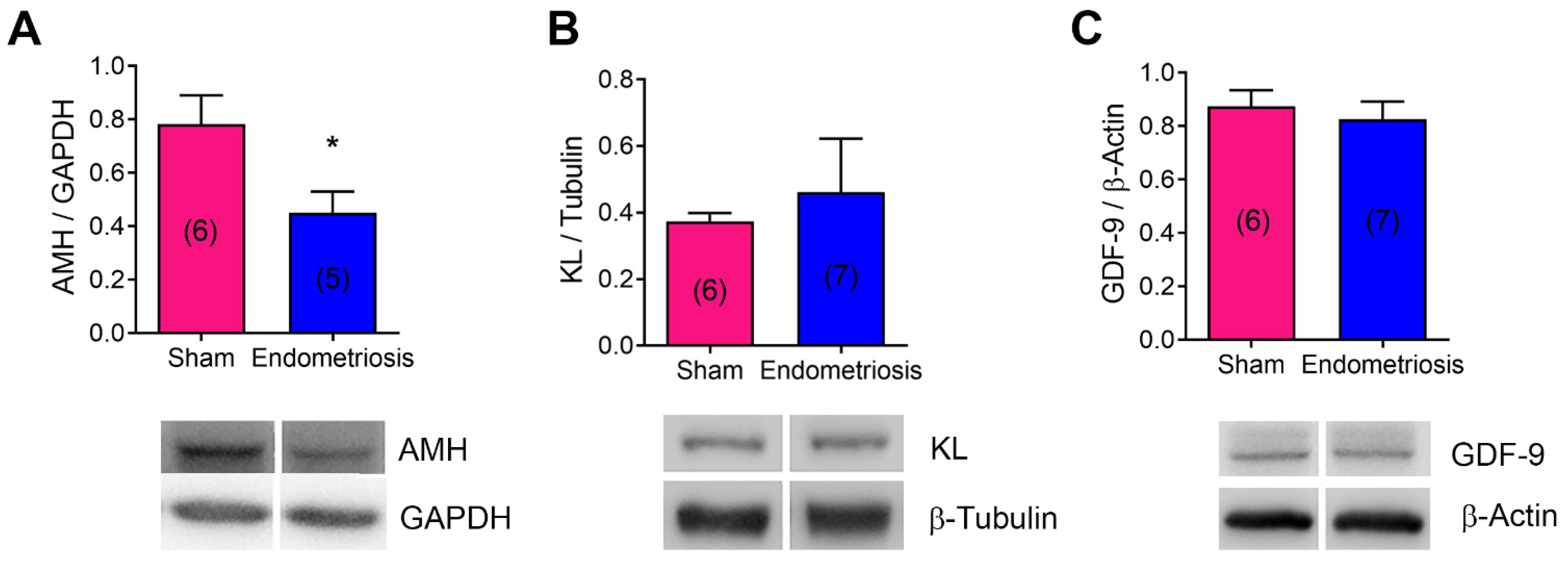
3.4. Endometriosis Alters the Expression of mRNA and Proteins Related to Folliculogenesis In Vivo and In Vitro
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zondervan, K.T.; Becker, C.M.; Koga, K.; Missmer, S.A.; Taylor, R.N.; Viganò, P. Endometriosis. Nat. Rev. Dis. Primers 2018, 4, 1–9. [Google Scholar] [CrossRef]
- Requadt, E.; Nahlik, A.J.; Jacobsen, A.; Ross, W.T. Patient Experiences of Endometriosis Diagnosis: A Mixed Methods Approach. BJOG Int. J. Obstet. Gynaecol. 2024, 131, 941–951. [Google Scholar] [CrossRef]
- Vercellini, P.; Viganò, P.; Bandini, V.; Buggio, L.; Berlanda, N.; Somigliana, E. Association of Endometriosis and Adenomyosis with Pregnancy and Infertility. Fertil. Steril. 2023, 119, 727–740. [Google Scholar] [CrossRef]
- Chapron, C.; Marcellin, L.; Borghese, B.; Santulli, P. Rethinking Mechanisms, Diagnosis and Management of Endometriosis. Nat. Rev. Endocrinol. 2019, 15, 666–682. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Liu, K. Cellular and Molecular Regulation of the Activation of Mammalian Primordial Follicles: Somatic Cells Initiate Follicle Activation in Adulthood. Hum. Reprod. Update 2015, 21, 779–786. [Google Scholar] [CrossRef] [PubMed]
- Thomas, F.H.; Vanderhyden, B.C. Oocyte-Granulosa Cell Interactions during Mouse Follicular Development: Regulation of Kit Ligand Expression and Its Role in Oocyte Growth. Reprod. Biol. Endocrinol. 2006, 4, 19. [Google Scholar] [CrossRef]
- Monniaux, D. Driving Folliculogenesis by the Oocyte-Somatic Cell Dialog: Lessons from Genetic Models. Theriogenology 2016, 86, 41–53. [Google Scholar] [CrossRef]
- Matsuzaki, S.; Pankhurst, M.W. Hyperactivation of Dormant Primordial Follicles in Ovarian Endometrioma Patients. Reproduction 2020, 160, R145–R153. [Google Scholar] [CrossRef]
- Findlay, J.K.; Hutt, K.J.; Hickey, M.; Anderson, R.A. What Is the “Ovarian Reserve”? Fertil. Steril. 2015, 103, 628–630. [Google Scholar] [CrossRef] [PubMed]
- Dewailly, D.; Andersen, C.Y.; Balen, A.; Broekmans, F.; Dilaver, N.; Fanchin, R.; Griesinger, G.; Kelsey, T.W.; La Marca, A.; Lambalk, C.; et al. The Physiology and Clinical Utility of Anti-Mullerian Hormone in Women. Hum. Reprod. Update 2014, 20, 370–385. [Google Scholar] [CrossRef]
- Jiang, D.; Nie, X. Effect of Endometrioma and Its Surgical Excision on Fertility (Review). Exp. Ther. Med. 2020, 20, 114. [Google Scholar] [CrossRef]
- Casalechi, M.; Di Stefano, G.; Fornelli, G.; Somigliana, E.; Viganò, P. Impact of Endometriosis on the Ovarian Follicles. Best. Pr. Res. Clin. Obs. Gynaecol. 2024, 92, 102430. [Google Scholar] [CrossRef]
- Rangi, S.; Hur, C.; Richards, E.; Falcone, T. Fertility Preservation in Women with Endometriosis. J. Clin. Med. 2023, 12, 4331. [Google Scholar] [CrossRef]
- Pedachenko, N.; Anagnostis, P.; Shemelko, T.; Tukhtarian, R.; Alabbas, L. Serum Anti-Mullerian Hormone, Prolactin and Estradiol Concentrations in Infertile Women with Endometriosis. Gynecol. Endocrinol. 2021, 37, 162–165. [Google Scholar] [CrossRef]
- Ata, B.; Uncu, G. Impact of Endometriomas and Their Removal on Ovarian Reserve. Curr. Opin. Obs. Gynecol. 2015, 27, 235–241. [Google Scholar] [CrossRef]
- Mc Cormack, B.A.; Olivares, C.N.; Madanes, D.; Ricci, A.G.; Bilotas, M.A.; Barañao, R.I. Effect of Urolithins A and B on Ectopic Endometrial Growth in a Murine Model of Endometriosis. Food Funct. 2021, 12, 9894–9903. [Google Scholar] [CrossRef]
- Woodruff, T.K.; Lyon, R.J.; Hansen, S.E.; Rice, G.C.; Mather, J.P. Inhibin and Activin Locally Regulate Rat Ovarian Folliculogenesis. Endocrinology 1990, 127, 3196–3205. [Google Scholar] [CrossRef] [PubMed]
- Scotti, L.; Irusta, G.; Abramovich, D.; Tesone, M.; Parborell, F. Administration of a Gonadotropin-Releasing Hormone Agonist Affects Corpus Luteum Vascular Stability and Development and Induces Luteal Apoptosis in a Rat Model of Ovarian Hyperstimulation Syndrome. Mol. Cell. Endocrinol. 2011, 335, 116–125. [Google Scholar] [CrossRef]
- Bradford, M.M. A Rapid and Sensitive Method for the Quantitation of Microgram Quantities of Protein Utilizing the Principle of Protein-Dye Binding. Anal. Biochem. 1976, 72, 248–254. [Google Scholar]
- Zeitvogel, A.; Baumann, R.; Starzinski-Powitz, A. Identification of an Invasive, N-Cadherin-Expressing Epithelial Cell Type in Endometriosis Using a New Cell Culture Model. Am. J. Pathol. 2001, 159, 1839–1852. [Google Scholar] [CrossRef]
- Pfaffl, M.W. A New Mathematical Model for Relative Quantification in Real-Time RT–PCR. Nucleic Acids Res. 2001, 29, E45. [Google Scholar] [CrossRef]
- Hsueh, A.J.W.; Billig, H.; Tsafriri, A. Ovarian Follicle Atresia: A Hormonally Controlled Apoptotic Process. Endocr. Rev. 1994, 15, 707–724. [Google Scholar] [CrossRef]
- Tang, Y.; Chen, S.L.; Chen, X.; He, Y.X.; Ye, D.S.; Guo, W.; Zheng, H.Y.; Yang, X.H. Ovarian Damage after Laparoscopic Endometrioma Excision Might Be Related to the Size of Cyst. Fertil. Steril. 2013, 100, 464–469. [Google Scholar] [CrossRef] [PubMed]
- Torng, P.-L. Clinical Implication for Endometriosis Associated with Ovarian Cancer. Gynecol. Minim. Invasive Ther. 2017, 6, 152–156. [Google Scholar] [CrossRef]
- Di Nisio, V.; Rossi, G.; Di Luigi, G.; Palumbo, P.; D’Alfonso, A.; Iorio, R.; Cecconi, S. Increased Levels of Proapoptotic Markers in Normal Ovarian Cortex Surrounding Small Endometriotic Cysts. Reprod. Biol. 2019, 19, 225–229. [Google Scholar] [CrossRef]
- Kitajima, M.; Dolmans, M.-M.; Donnez, O.; Masuzaki, H.; Soares, M.; Donnez, J. Enhanced Follicular Recruitment and Atresia in Cortex Derived from Ovaries with Endometriomas. Fertil. Steril. 2014, 101, 1031–1037. [Google Scholar] [CrossRef]
- Cacciottola, L.; Donnez, J.; Dolmans, M.-M. Can Endometriosis-Related Oxidative Stress Pave the Way for New Treatment Targets? Int. J. Mol. Sci. 2021, 22, 7138. [Google Scholar] [CrossRef] [PubMed]
- Nasiri, N.; Moini, A.; Eftekhari-Yazdi, P.; Karimian, L.; Salman-Yazdi, R.; Arabipoor, A. Oxidative Stress Statues in Serum and Follicular Fluid of Women with Endometriosis. Cell J. 2017, 18, 582–587. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Chen, Y.; Liu, Y.; Xing, Y.; Miao, C.; Zhao, Y.; Chang, X.; Zhang, Q. The Role of Oxidative Stress and Natural Antioxidants in Ovarian Aging. Front. Pharmacol. 2021, 11, 617843. [Google Scholar] [CrossRef]
- Yan, F.; Zhao, Q.; Li, Y.; Zheng, Z.; Kong, X.; Shu, C.; Liu, Y.; Shi, Y. The Role of Oxidative Stress in Ovarian Aging: A Review. J. Ovarian Res. 2022, 15, 100. [Google Scholar] [CrossRef]
- Rasmussen, M.L.; Gama, V. A Connection in Life and Death: The BCL-2 Family Coordinates Mitochondrial Network Dynamics and Stem Cell Fate. Int. Rev. Cell Mol. Biol. 2020, 353, 255–284. [Google Scholar] [CrossRef]
- Iwase, A.; Hasegawa, Y.; Tsukui, Y.; Kobayashi, M.; Hiraishi, H.; Nakazato, T.; Kitahara, Y. Anti-Müllerian Hormone beyond an Ovarian Reserve Marker: The Relationship with the Physiology and Pathology in the Life-Long Follicle Development. Front. Endocrinol. 2023, 14, 1273966. [Google Scholar] [CrossRef]
- Durlinger, A.; Visser, J.; Themmen, A. Regulation of Ovarian Function: The Role of Anti-Mullerian Hormone. Reproduction 2002, 124, 601–609. [Google Scholar] [CrossRef] [PubMed]
- Kitajima, M.; Matsumoto, K.; Murakami, N.; Kajimura, I.; Harada, A.; Kitajima, Y.; Masuzaki, H.; Miura, K. AMH Concentrations in Peritoneal Fluids of Women With and Without Endometriosis. Front. Surg. 2020, 7, 600202. [Google Scholar] [CrossRef]
- Pais, A.S.; Flagothier, C.; Tebache, L.; Almeida Santos, T.; Nisolle, M. Impact of Surgical Management of Endometrioma on AMH Levels and Pregnancy Rates: A Review of Recent Literature. J. Clin. Med. 2021, 10, 414. [Google Scholar] [CrossRef]
- Younis, J.S.; Shapso, N.; Ben-Sira, Y.; Nelson, S.M.; Izhaki, I. Endometrioma Surgery-a Systematic Review and Meta-Analysis of the Effect on Antral Follicle Count and Anti-Müllerian Hormone. Am. J. Obs. Gynecol. 2021, 226, 33–51.e7. [Google Scholar] [CrossRef]
- Saleh, A.C.; Sabry, R.; Mastromonaco, G.F.; Favetta, L.A. BPA and BPS Affect the Expression of Anti-Mullerian Hormone (AMH) and Its Receptor during Bovine Oocyte Maturation and Early Embryo Development. Reprod. Biol. Endocrinol. 2021, 19, 119. [Google Scholar] [CrossRef]
- Takeuchi, A.; Koga, K.; Satake, E.; Makabe, T.; Taguchi, A.; Miyashita, M.; Takamura, M.; Yoshino, O.; Wada-hiraike, O.; Fujii, T.; et al. Endometriosis Triggers Excessive Activation of Primordial Follicles via PI3K-PTEN-Akt-Foxo3 Pathway. J. Clin. Endocrinol. Metab. 2019, 104, 5547–5554. [Google Scholar] [CrossRef]
- Jin, X.; Han, C.; Yu, F.; Wei, P.; Hu, Z.; Liu, Y. Anti-apoptotic Action of Stem Cell Factor on Oocytes in Primordial Follicles and Its Signal Transduction. Mol. Reprod. Dev. 2005, 70, 82–90. [Google Scholar] [CrossRef]
- Panwar, D.; Rawal, L.; Ali, S. The Potential Role of the KFG and KITLG Proteins in Preventing Granulosa Cell Apoptosis in Bubalus Bubalis. J. Genet. Eng. Biotechnol. 2023, 21. [Google Scholar] [CrossRef]
- Luan, Y.; So, W.; Dong, R.; Abazarikia, A.; Kim, S.Y. KIT in Oocytes: A Key Factor for Oocyte Survival and Reproductive Lifespan. EBioMedicine 2024, 106, 105263. [Google Scholar] [CrossRef]
- Park, M.J.; Ahn, J.-W.; Kim, K.H.; Bang, J.; Kim, S.C.; Jeong, J.Y.; Choi, Y.E.; Kim, C.-W.; Joo, B.S. Prediction of Ovarian Aging Using Ovarian Expression of BMP15, GDF9, and C-KIT. Exp. Biol. Med. 2020, 245, 711–719. [Google Scholar] [CrossRef] [PubMed]
- Ochoa Bernal, M.A.; Fazleabas, A.T. The Known, the Unknown and the Future of the Pathophysiology of Endometriosis. Int. J. Mol. Sci. 2024, 25, 5815. [Google Scholar] [CrossRef]
- Muraoka, A.; Suzuki, M.; Hamaguchi, T.; Watanabe, S.; Iijima, K.; Murofushi, Y.; Shinjo, K.; Osuka, S.; Hariyama, Y.; Ito, M.; et al. Fusobacterium Infection Facilitates the Development of Endometriosis through the Phenotypic Transition of Endometrial Fibroblasts. Sci. Transl. Med. 2023, 15, eadd1531. [Google Scholar] [CrossRef] [PubMed]
- Pai, A.H.Y.; Wang, Y.W.; Lu, P.C.; Wu, H.M.; Xu, J.L.; Huang, H.Y. Gut Microbiome–Estrobolome Profile in Reproductive-Age Women with Endometriosis. Int. J. Mol. Sci. 2023, 24, 16301. [Google Scholar] [CrossRef] [PubMed]
- Alghetaa, H.; Mohammed, A. Estrobolome Dysregulation Is Associated with Altered Immunometabolism in a Mouse Model of Endometriosis. Front. Endocrinol. 2023, 14, 1261781. [Google Scholar] [CrossRef]
- Wei, W.; Komatsu, K.; Osuka, S.; Murase, T.; Bayasula, B.; Nakanishi, N.; Nakamura, T.; Goto, M.; Iwase, A.; Masubuchi, S.; et al. Tamoxifen Activates Dormant Primordial Follicles in Mouse Ovaries. Reprod. Sci. 2022, 29, 3404–3412. [Google Scholar] [CrossRef]
- Praveen Chakravarthi, V.; Ghosh, S.; Roby, K.F.; Wolfe, M.W.; Karim Rumi, M.A. A Gatekeeping Role of ESR2 to Maintain the Primordial Follicle Reserve. Endocrinology 2020, 161, bqaa037. [Google Scholar] [CrossRef]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ricci, A.; Bengochea, T.; Olivares, C.; del Valle, S.; Simone, J.; Gemzell-Danielsson, K.; Barañao, R.I.; Meresman, G.; Bilotas, M. Peritoneal Endometriosis Impairs Ovarian Reserve and Increases Atresia in a Rat Model. Biomedicines 2025, 13, 348. https://doi.org/10.3390/biomedicines13020348
Ricci A, Bengochea T, Olivares C, del Valle S, Simone J, Gemzell-Danielsson K, Barañao RI, Meresman G, Bilotas M. Peritoneal Endometriosis Impairs Ovarian Reserve and Increases Atresia in a Rat Model. Biomedicines. 2025; 13(2):348. https://doi.org/10.3390/biomedicines13020348
Chicago/Turabian StyleRicci, Analía, Tatiana Bengochea, Carla Olivares, Sofía del Valle, Julieta Simone, Kristina Gemzell-Danielsson, Rosa Inés Barañao, Gabriela Meresman, and Mariela Bilotas. 2025. "Peritoneal Endometriosis Impairs Ovarian Reserve and Increases Atresia in a Rat Model" Biomedicines 13, no. 2: 348. https://doi.org/10.3390/biomedicines13020348
APA StyleRicci, A., Bengochea, T., Olivares, C., del Valle, S., Simone, J., Gemzell-Danielsson, K., Barañao, R. I., Meresman, G., & Bilotas, M. (2025). Peritoneal Endometriosis Impairs Ovarian Reserve and Increases Atresia in a Rat Model. Biomedicines, 13(2), 348. https://doi.org/10.3390/biomedicines13020348




