Obesity as a Risk Factor for Hyperglycemia, Electrolyte Disturbances, and Acute Kidney Injury in the Emergency Department
Abstract
1. Introduction
2. Materials and Methods
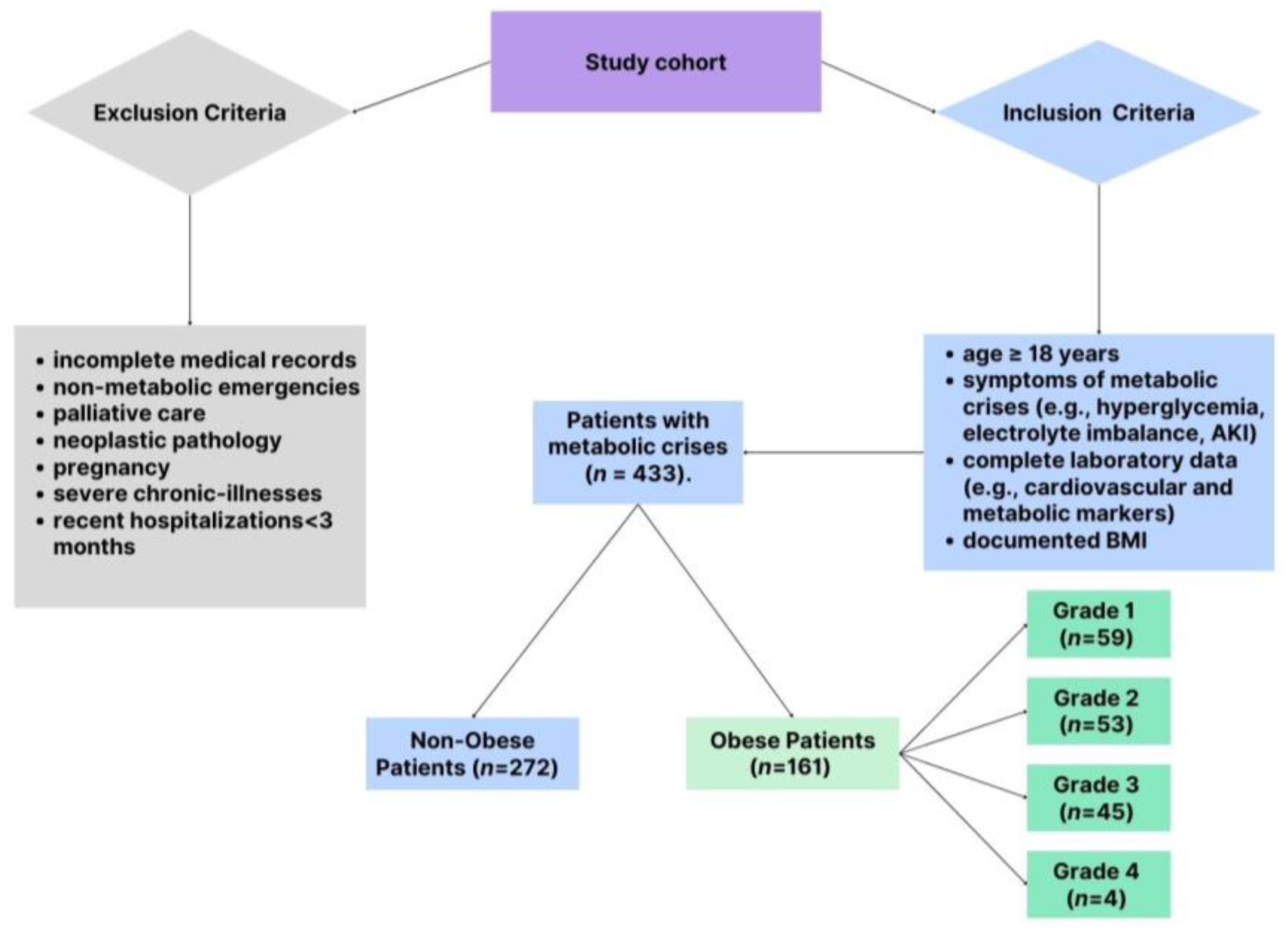
2.1. Study Design
2.2. Study Population
2.3. Data Collection
2.4. Parameters Assessed
2.5. Impact of COVID-19 Pandemic on Patient Selection
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 2 November 2024).
- Flegal, K.M.; Kit, B.K.; Orpana, H.; Graubard, B.I. Association of All-Cause Mortality With Overweight and Obesity Using Standard Body Mass Index Categories: A Systematic Review and Meta-analysis. JAMA 2013, 309, 71–82. [Google Scholar] [CrossRef] [PubMed]
- Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z. The metabolic syndrome. Lancet 2005, 365, 1415–1428. [Google Scholar] [CrossRef]
- Hotamisligil, G.S. Inflammation and metabolic disorders. Nature 2006, 444, 860–867. [Google Scholar] [CrossRef] [PubMed]
- Mechanick, J.I.; Youdim, A.; Jones, D.B.; Garvey, W.T.; Hurley, D.L.; McMahon, M.M.; Heinberg, L.J.; Kushner, R.; Adams, T.D.; Shikora, S.; et al. Clinical Practice Guidelines for the Perioperative Nutritional, Metabolic, and Nonsurgical Support of the Bariatric Surgery Patient—2013 Update: Cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic and Bariatric Surgery. Endocr. Pract. 2013, 19, 337–372. [Google Scholar] [CrossRef]
- Hales, C.M.; Carroll, M.D.; Fryar, C.D.; Ogden, C.L. Prevalence of Obesity Among Adults and Youth: United States, 2015–2016. NCHS Data Brief 2017, 288, 1–8. [Google Scholar]
- Després, J.P.; Lemieux, I. Abdominal obesity and metabolic syndrome. Nature 2006, 444, 881–887. [Google Scholar] [CrossRef] [PubMed]
- Kahn, S.E.; Hull, R.L.; Utzschneider, K.M. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature 2006, 444, 840–846. [Google Scholar] [CrossRef]
- Pi-Sunyer, X. The medical risks of obesity. Postgrad Med. 2009, 121, 21–33. [Google Scholar] [CrossRef] [PubMed]
- Romania—Global Obesity Observatory. Available online: https://data.worldobesity.org/country/romania-178/ (accessed on 2 November 2024).
- World Health Organization. Who European Regional Obesity Report 2022. Available online: https://iris.who.int/bitstream/handle/10665/353747/9789289057738-eng.pdf (accessed on 2 November 2024).
- Tan, W.S.Y.; Young, A.M.; Di Bella, A.L.; Comans, T.; Banks, M. Exploring the Impact of Obesity on Health Care Resources and Coding in the Acute Hospital Setting: A Feasibility Study. Healthcare 2020, 8, 459. [Google Scholar] [CrossRef] [PubMed]
- Lam, B.C.C.; Lim, A.Y.L.; Chan, S.L.; Yum, M.P.S.; Koh, N.S.Y.; Finkelstein, E.A. The impact of obesity: A narrative review. Singap. Med. J. 2023, 64, 163–171. [Google Scholar] [CrossRef]
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic. Report of a WHO Consultation; World Health Organ Technical Report Series 894; World Health Organization: Geneva, Switzerland, 2000; pp. 1–253. [Google Scholar]
- Dickerson, R.N.; Andromalos, L.; Brown, J.C.; Correia, M.I.T.D.; Pritts, W.; Ridley, E.J.; Robinson, K.N.; Rosenthal, M.D.; van Zanten, A.R.H. Obesity and critical care nutrition: Current practice gaps and directions for future research. Crit. Care 2022, 26, 283. [Google Scholar] [CrossRef]
- Khwaja, A. KDIGO Clinical Practice Guidelines for Acute Kidney Injury. Nephron Clin. Pract. 2012, 120, c179–c184. [Google Scholar] [CrossRef] [PubMed]
- Kovesdy, C.P.; Furth, S.L.; Zoccali, C.; World Kidney Day Steering Committee. Obesity and Kidney Disease: Hidden Consequences of the Epidemic. Can. J. Kidney Health Dis. 2017, 30, 1–10. [Google Scholar] [CrossRef]
- Choi, J.I.; Cho, Y.H.; Lee, S.Y.; Jeong, D.W.; Lee, J.G.; Yi, Y.H.; Tak, Y.J.; Lee, S.H.; Hwang, H.R.; Park, E.J. The Association between Obesity Phenotypes and Early Renal Function Decline in Adults without Hypertension, Dyslipidemia, and Diabetes. Korean J. Fam. Med. 2019, 40, 176–181. [Google Scholar] [CrossRef]
- Di Giacinto, I.; Guarnera, M.; Esposito, C.; Montomoli, C.; Feltracco, P.; Costa, M.G. Emergency in Obese Patients: A Reply to SOBA UK. J. Anesth. Analg. Crit. Care 2022, 2, 12. [Google Scholar] [CrossRef]
- Clemente-Suárez, V.J.; Redondo-Flórez, L.; Beltrán-Velasco, A.I.; Martín-Rodríguez, A.; Martínez-Guardado, I.; Navarro-Jiménez, E.; Laborde-Cárdenas, C.C.; Tornero-Aguilera, J.F. The Role of Adipokines in Health and Disease. Biomedicines 2023, 11, 1290. [Google Scholar] [CrossRef] [PubMed]
- Roberts, C.K.; Hevener, A.L.; Barnard, R.J. Metabolic Syndrome and Insulin Resistance: Underlying Causes and Modification by Exercise Training. Compr. Physiol. 2013, 3, 1–58. [Google Scholar] [CrossRef] [PubMed]
- Kirichenko, T.V.; Markina, Y.V.; Bogatyreva, A.I.; Tolstik, T.V.; Varaeva, Y.R.; Starodubova, A.V. The Role of Adipokines in Inflammatory Mechanisms of Obesity. Int. J. Mol. Sci. 2022, 23, 14982. [Google Scholar] [CrossRef] [PubMed]
- Hall, J.E.; do Carmo, J.M.; da Silva, A.A.; Wang, Z.; Hall, M.E. Obesity, Kidney Dysfunction and Hypertension: Mechanistic Links. Nat. Rev. Nephrol. 2019, 15, 367–385. [Google Scholar] [CrossRef]
- Lee, J.; Hwang, Y.; Kim, K.N.; Ahn, C.; Sung, H.K.; Ko, K.P.; Oh, K.H.; Ahn, C.; Park, Y.J.; Kim, S.; et al. Associations of Urinary Sodium Levels with Overweight and Central Obesity in a Population with a Sodium Intake. BMC Nutr. 2018, 4, 47. [Google Scholar] [CrossRef] [PubMed]
- Horita, S.; Seki, G.; Yamada, H.; Suzuki, M.; Koike, K.; Fujita, T. Insulin Resistance, Obesity, Hypertension, and Renal Sodium Transport. Int. J. Hypertens. 2011, 2011, 391762. [Google Scholar] [CrossRef]
- Ortega, F.B.; Lavie, C.J.; Blair, S.N. Obesity and Cardiovascular Disease. Circ. Res. 2016, 118, 1752–1770. [Google Scholar] [CrossRef]
- Hall, J.E.; do Carmo, J.M.; da Silva, A.A.; Wang, Z.; Hall, M.E. Obesity-Induced Hypertension: Interaction of Neurohumoral and Renal Mechanisms. Circ. Res. 2015, 116, 991–1006. [Google Scholar] [CrossRef] [PubMed]
- Forcina, G.; Luciano, M.; Frattolillo, V.; Mori, S.; Monaco, N.; Guarino, S.; Marzuillo, P.; Miraglia del Giudice, E.; Di Sessa, A. Kidney Damage in Pediatric Obesity: Insights from an Emerging Perspective. J. Clin. Med. 2024, 13, 7025. [Google Scholar] [CrossRef]
- Tonneijck, L.; Muskiet, M.H.; Smits, M.M.; van Bommel, E.J.; Heerspink, H.J.; van Raalte, D.H.; Joles, J.A. Glomerular Hyperfiltration in Diabetes: Mechanisms, Clinical Significance, and Treatment. J. Am. Soc. Nephrol. 2017, 28, 1023–1039. [Google Scholar] [CrossRef]
- Basolo, A.; Salvetti, G.; Giannese, D.; Genzano, S.B.; Ceccarini, G.; Giannini, R.; Sotgia, G.; Fierabracci, P.; Piaggi, P.; Santini, F. Obesity, Hyperfiltration, and Early Kidney Damage: A New Formula for the Estimation of Creatinine Clearance. J. Clin. Endocrinol. Metab. 2023, 108, 3280–3286. [Google Scholar] [CrossRef]
- D’Agati, V.D.; Chagnac, A.; de Vries, A.P.; Levi, M.; Porrini, E.; Herman-Edelstein, M.; Praga, M. Obesity-Related Glomerulopathy: Clinical and Pathologic Characteristics and Pathogenesis. Nat. Rev. Nephrol. 2016, 12, 453–471. [Google Scholar] [CrossRef] [PubMed]
- Whaley-Connell, A.; Nistala, R.; Chaudhary, K. The Importance of Early Identification of Chronic Kidney Disease. Mo. Med. 2011, 108, 25–28. [Google Scholar]
- Ozbek, L.; Abdel-Rahman, S.M.; Unlu, S.; Guldan, M.; Copur, S.; Burlacu, A.; Covic, A.; Kanbay, M. Exploring Adiposity and Chronic Kidney Disease: Clinical Implications, Management Strategies, Prognostic Considerations. Medicina 2024, 60, 1668. [Google Scholar] [CrossRef] [PubMed]
- Artham, S.M.; Lavie, C.J.; De Schutter, A.; Ventura, H.O.; Milani, R.V. Obesity, Age, and Cardiac Risk. Curr. Cardiovasc. Risk Rep. 2011, 5, 128–137. [Google Scholar] [CrossRef]
- Norris, T.; Cole, T.J.; Bann, D.; Hamer, M.; Hardy, R.; Li, L.; Ong, K.K.; Ploubidis, G.B.; Viner, R.; Johnson, W. Duration of Obesity Exposure between Ages 10 and 40 Years and Its Relationship with Cardiometabolic Disease Risk Factors: A Cohort Study. PLoS Med. 2020, 17, e1003387. [Google Scholar] [CrossRef]
- den Engelsen, C.; Koekkoek, P.S.; Gorter, K.J.; van den Donk, M.; Salomé, P.L.; Rutten, G.E. High-sensitivity C-reactive protein to detect metabolic syndrome in a centrally obese population: A cross-sectional analysis. Cardiovasc. Diabetol. 2012, 11, 25. [Google Scholar] [CrossRef]
- Rolver, M.G.; Emanuelsson, F.; Nordestgaard, B.G.; Benn, M. Contributions of elevated CRP, hyperglycaemia, and type 2 diabetes to cardiovascular risk in the general population: Observational and Mendelian randomization studies. Cardiovasc. Diabetol. 2024, 23, 165. [Google Scholar] [CrossRef]
- Blokhin, I.O.; Lentz, S.R. Mechanisms of thrombosis in obesity. Curr. Opin. Hematol. 2013, 20, 437–444. [Google Scholar] [CrossRef]
- Gentile, F.; Aimo, A.; Januzzi, J.L.J.; Richards, A.M.; Lam, C.S.P.; Latini, R.; Anand, I.S.; Ueland, T.; Brunner-La Rocca, H.P.; Bayes-Genis, A.; et al. Prognostic value of NT-proBNP and best cut-offs for risk prediction in obese patients with chronic systolic heart failure. Eur. Heart J. 2020, 41 (Suppl. 2), ehaa946.1002. [Google Scholar] [CrossRef]
- de Lemos, J.A.; Drazner, M.H.; Omland, T.; Ayers, C.R.; Khera, A.; Rohatgi, A.; Hashim, I.; Berry, J.D.; Das, S.R.; Morrow, D.A.; et al. Association of Troponin T Detected With a Highly Sensitive Assay and Cardiac Structure and Mortality Risk in the General Population. JAMA 2010, 304, 2503–2512. [Google Scholar] [CrossRef]
- Odqvist, M.; Bandstein, N.; Tygesen, H.; Eggers, K.M.; Andersson, P.O.; Holzmann, M.J. Outcomes in patients with chest pain in emergency departments using high-sensitivity versus conventional troponins. Scand. Cardiovasc. J. 2023, 57, 2190546. [Google Scholar] [CrossRef]
- Lorgis, L.; Cottin, Y.; Danchin, N.; Mock, L.; Sicard, P.; Buffet, P.; L’Huillier, I.; Richard, C.; Beer, J.C.; Touzery, C.; et al. Impact of obesity on the prognostic value of the N-terminal pro-B-type natriuretic peptide (NT-proBNP) in patients with acute myocardial infarction. Heart 2011, 97, 551–556. [Google Scholar] [CrossRef] [PubMed]
- Rossi, A.P.; Muollo, V.; Dalla Valle, Z.; Urbani, S.; Pellegrini, M.; El Ghoch, M.; Mazzali, G. The Role of Obesity, Body Composition, and Nutrition in COVID-19 Pandemia: A Narrative Review. Nutrients 2022, 14, 3493. [Google Scholar] [CrossRef]
- Hansen, E.S.; Rinde, F.B.; Edvardsen, M.S.; Hindberg, K.; Latysheva, N.; Aukrust, P.; Ueland, T.; Michelsen, A.E.; Hansen, J.B.; Brækkan, S.K.; et al. Elevated plasma D-dimer levels are associated with risk of future incident venous thromboembolism. Thromb. Res. 2021, 208, 121–126. [Google Scholar] [CrossRef]
- Kwaifa, I.K.; Bahari, H.; Yong, Y.K.; Noor, S.M. Endothelial Dysfunction in Obesity-Induced Inflammation: Molecular Mechanisms and Clinical Implications. Biomolecules 2020, 10, 291. [Google Scholar] [CrossRef] [PubMed]
- Hawley, P.C.; Hawley, M.P. Difficulties in diagnosing pulmonary embolism in the obese patient: A literature review. Vasc. Med. 2011, 16, 444–451. [Google Scholar] [CrossRef] [PubMed]
- Kornblith, L.Z.; Howard, B.; Kunitake, R.; Redick, B.; Nelson, M.; Cohen, M.J.; Callcut, R.A. Obesity and clotting: Body mass index independently contributes to hypercoagulability after injury. J. Trauma Acute Care Surg. 2015, 78, 30–38. [Google Scholar] [CrossRef] [PubMed]
- La Rosa, F.; Montecucco, F.; Liberale, L.; Sessarego, M.; Carbone, F. Venous thrombosis and obesity: From clinical needs to therapeutic challenges. Intern. Emerg. Med. 2024. [Google Scholar] [CrossRef] [PubMed]
- Gutiérrez-Cuevas, J.; Sandoval-Rodriguez, A.; Meza-Rios, A.; Monroy-Ramírez, H.C.; Galicia-Moreno, M.; García-Bañuelos, J.; Santos, A.; Armendariz-Borunda, J. Molecular Mechanisms of Obesity-Linked Cardiac Dysfunction: An Up-Date on Current Knowledge. Cells 2021, 10, 629. [Google Scholar] [CrossRef] [PubMed]
- Yaribeygi, H.; Maleki, M.; Butler, A.E.; Jamialahmadi, T.; Sahebkar, A. Molecular mechanisms linking stress and insulin resistance. EXCLI J. 2022, 21, 317–334. [Google Scholar] [CrossRef] [PubMed]
- Chu, B.; Marwaha, K.; Sanvictores, T.; Awosika, A.O.; Ayers, D. Physiology, Stress Reaction. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- Kauppi, J.; Airaksinen, K.E.J.; Lehto, J.; Pouru, J.P.; Saha, J.; Purola, P.; Jaakkola, S.; Lehtonen, J.; Vasankari, T.; Juonala, M.; et al. Performance of D-dimer, cardiac troponin T, C-reactive protein, and NT-proBNP in prediction of long-term mortality in patients with suspected pulmonary embolism. Eur. Heart J. Open 2024, 4, oeae079. [Google Scholar] [CrossRef]
- Ma, Y.; Zheng, J.; Zhou, W.; Luo, Z.; Jiang, W. Predictive value of perioperative NT-proBNP levels for acute kidney injury in patients with compromised renal function undergoing cardiac surgery: A case control study. BMC Anesthesiol. 2024, 24, 298. [Google Scholar] [CrossRef] [PubMed]
- Malachias, M.V.B.; Wijkman, M.O.; Bertoluci, M.C. NT-proBNP as a predictor of death and cardiovascular events in patients with type 2 diabetes. Diabetol. Metab. Syndr. 2022, 14, 64. [Google Scholar] [CrossRef] [PubMed]
- Mohiuddin, S.G.; Ward, M.E.; Hollingworth, W.; Watson, J.C.; Whiting, P.F.; Thom, H.H.Z. Cost-effectiveness of routine monitoring of long-term conditions in primary care: Informing decision modelling with a systematic review in hypertension, type 2 diabetes and chronic kidney disease. PharmacoEconomics Open 2024, 8, 359–371. [Google Scholar] [CrossRef]
- GoodSmith, M.S.; Skandari, M.R.; Huang, E.S.; Naylor, R.N. The impact of biomarker screening and cascade genetic testing on the cost-effectiveness of MODY genetic testing. Diabetes Care 2019, 42, 2247–2255. [Google Scholar] [CrossRef]
- Johnson, S.R.; Carter, H.E.; Leo, P.; Hollingworth, S.A.; Davis, E.A.; Jones, T.W.; Conwell, L.S.; Harris, M.; Brown, M.A.; Graves, N.; et al. Cost-effectiveness analysis of routine screening using massively parallel sequencing for maturity-onset diabetes of the young in a pediatric diabetes cohort: Reduced health system costs and improved patient quality of life. Diabetes Care 2019, 42, 69–76. [Google Scholar] [CrossRef]
- Clark, J.M.; Garvey, W.T.; Niswender, K.D.; Schmidt, A.M.; Ahima, R.S.; Aleman, J.O.; Battarbee, A.N.; Beckman, J.; Bennett, W.L.; Brown, N.J.; et al. Obesity and Overweight: Probing Causes, Consequences, and Novel Therapeutic Approaches Through the American Heart Association’s Strategically Focused Research Network. J. Am. Heart Assoc. 2023, 12, e027693. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | Obese Patients (n = 161) Mean ± SD/% | Non-Obese Patients (n = 272) Mean ± SD/% | p-Value |
|---|---|---|---|
| Age (years) | 72.2± 9.4 | 68.1± 10.1 | 0.03 |
| BMI (kg/m2) | 36.3± 4.7 | 24.5± 3.2 | 0.001 |
| Gender (% male) | 45% | 52% | 0.07 |
| Cardiovascular comorbidities: | |||
| Hypertension (%) | 90.7% | 73.5% | 0.002 |
| Cardiac Insufficiency (%) | 89.4% | 92.3% | 0.04 |
| Atrial fibrillation (%) | 56% | 48% | 0.08 |
| Obesity grades: | |||
| Grade 1 (%) | 36.6% | - | - |
| Grade 2 (%) | 33.3% | - | - |
| Grade 3 (%) | 28.0% | - | - |
| Grade 4 (%) | 2.5% | - | - |
| Markers | Grade 1 (n = 59) Mean ± SD | Grade 2 (n = 53) Mean ± SD | Grade 3 (n = 45) Mean ± SD | Grade 4 (n = 4) Mean ± SD |
|---|---|---|---|---|
| Cardiovascular markers | ||||
| NT-proBNP (pg/mL) | 5682.27 ± 7640.97 | 5831.47 ± 5779.03 | 6440.63 ± 5063.91 | 8036.33 ± 1151.46 |
| Troponin I (ng/mL) | 125.19 ± 336.01 | 42.91 ± 44.00 | 114.37 ± 435.23 | 18.70 ± 20.50 |
| C-reactive protein (mg/L) | 53.52 ± 88.12 | 47.80 ± 78.13 | 47.04 ± 50.18 | 48.22 ± 39.21 |
| CK-MB (ng/mL) | 22.52 ± 17.53 | 26.45 ± 38.69 | 23.97 ± 37.78 | 48.22 ± 39.21 |
| D-dimer (µg/mL) | 2.39 ± 3.04 | 2.99 ± 4.38 | 3.18 ± 3.74 | 2.35 ± 1.36 |
| Metabolic markers | ||||
| Blood Glucose (mg/dL) | 142.5 ± 12.4 | 154.2 ± 14.6 | 165.7 ± 17.3 | 178.4 ± 17.7 |
| Potassium (mmol/L) | 4.3 ± 0.2 | 4.5 ± 0.3 | 4.6 ± 0.4 | 4.8 ± 0.5 |
| Sodium (mmol/L) | 139.5 ± 3.5 | 140.1 ± 3.2 | 141.0 ± 3.1 | 142.3 ± 3.0 |
| Urea (mmol/L) | 44.3 ± 5.2 | 46.8 ± 6.0 | 49.2 ± 6.5 | 52.6 ± 7.2 |
| Creatinine (mg/dL) | 1.3 ± 0.1 | 1.4 ± 0.2 | 1.5 ± 0.3 | 1.7 ± 0.4 |
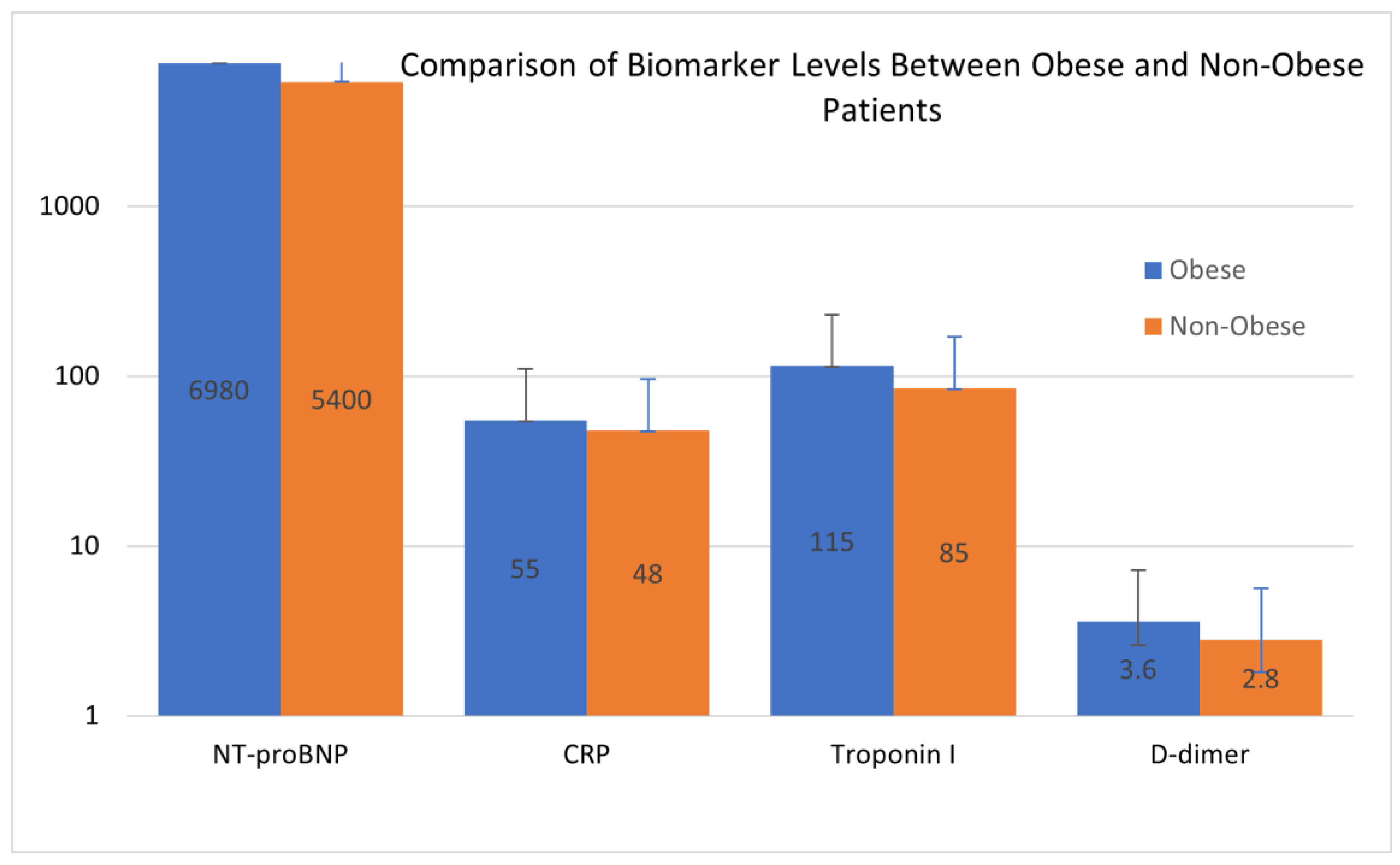
| Cardiovascular Markers | Hypertension (Mean ± SD) | Cardiac Insufficiency (Mean ± SD) | Atrial Fibrillation (Mean ± SD) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Obese Patients | Non-Obese Patients | p-Value | Obese Patients | Non-Obese Patients | p-Value | Obese Patients | Non-Obese Patients | p-Value | |
| NT-proBNP (pg/mL) | 7200 ± 2500 | 4600 ± 2100 | <0.001 | 7700 ± 3100 | 4300 ± 1900 | <0.001 | 7400 ± 2600 | 4500 ± 2100 | <0.001 |
| Troponin I (ng/mL) | 115 ± 320 | 85 ± 290 | 0.01 | 130 ± 340 | 90 ± 280 | 0.02 | 125 ± 330 | 95 ± 300 | 0.01 |
| CRP (mg/L) | 58 ± 15 | 48 ± 12 | 0.02 | 62 ± 18 | 44 ± 10 | 0.01 | 65 ± 14 | 50 ± 11 | 0.02 |
| CK-MB (ng/mL) | 26 ± 12 | 23 ± 10 | 0.04 | 29 ± 14 | 20 ± 9 | 0.03 | 28 ± 13 | 24 ± 10 | 0.03 |
| D-dimer (ng/mL) | 3.6 ± 1.4 | 2.8 ± 1.2 | 0.03 | 4.1 ± 1.5 | 2.4 ± 1.1 | 0.02 | 4.2 ± 1.6 | 3.0 ± 1.3 | 0.04 |
| Variable | Odds Ratio (95% CI) | p-Value |
|---|---|---|
| Obesity Grade 1 | 1.20 (0.90–1.60) | 0.15 |
| Obesity Grade 2 | 1.45 (1.10–1.92) | 0.02 |
| Obesity Grade 3 | 1.78 (1.30–2.44) | <0.001 |
| Obesity Grade 4 | 2.25 (1.50–3.40) | <0.001 |
| NT-proBNP (pg/mL) | 1.12 (1.05–1.18) | <0.001 |
| Troponin I (ng/mL) | 1.08 (1.02–1.15) | 0.01 |
| CRP (mg/L) | 1.05 (1.01–1.09) | 0.04 |
| CK-MB (mg/mL) | 1.10 (1.03–1.17) | 0.01 |
| D-dimer (ng/mL) | 1.15 (1.08–1.22) | <0.001 |
| Age (years) | 1.20 (1.10–1.31) | <0.001 |
| Gender (male) | 0.85 (0.65–1.10) | 0.21 |
| Hypertension | 1.50 (1.20–1.88) | <0.001 |
| Cardiac Insufficiency | 2.10 (1.60–2.80) | <0.001 |
| Atrial Fibrillation | 1.85 (1.40–2.44) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Crintea, I.N.; Cindrea, A.C.; Mederle, O.A.; Fulga, T.F.; Marza, A.M.; Petrica, A.; Trebuian, C.I.; Timar, R. Obesity as a Risk Factor for Hyperglycemia, Electrolyte Disturbances, and Acute Kidney Injury in the Emergency Department. Biomedicines 2025, 13, 349. https://doi.org/10.3390/biomedicines13020349
Crintea IN, Cindrea AC, Mederle OA, Fulga TF, Marza AM, Petrica A, Trebuian CI, Timar R. Obesity as a Risk Factor for Hyperglycemia, Electrolyte Disturbances, and Acute Kidney Injury in the Emergency Department. Biomedicines. 2025; 13(2):349. https://doi.org/10.3390/biomedicines13020349
Chicago/Turabian StyleCrintea, Iulia Najette, Alexandru Cristian Cindrea, Ovidiu Alexandru Mederle, Teodor Florin Fulga, Adina Maria Marza, Alina Petrica, Cosmin Iosif Trebuian, and Romulus Timar. 2025. "Obesity as a Risk Factor for Hyperglycemia, Electrolyte Disturbances, and Acute Kidney Injury in the Emergency Department" Biomedicines 13, no. 2: 349. https://doi.org/10.3390/biomedicines13020349
APA StyleCrintea, I. N., Cindrea, A. C., Mederle, O. A., Fulga, T. F., Marza, A. M., Petrica, A., Trebuian, C. I., & Timar, R. (2025). Obesity as a Risk Factor for Hyperglycemia, Electrolyte Disturbances, and Acute Kidney Injury in the Emergency Department. Biomedicines, 13(2), 349. https://doi.org/10.3390/biomedicines13020349








