A Novel Technology for Needle-Free Injections of Liquids, Particles and Viable Cells into the Submucosa of the Urethra by a Pressure-Controlled Waterjet Technology
Abstract
1. Introduction
2. Materials and Methods
2.1. Investigation of the Calibre of Tubings as a Function of the Pressure Levels Required to Grant Sufficient Cell Viability After Waterjet Injections
2.2. Preparation of Urethral Tissue Samples and Waterjet Injection
2.3. Preparation of Cryosections and Histologic Evaluation
2.4. Preparation of Porcine Stromal Cells and Myoblasts for Waterjet Injections
2.5. Data Processing
3. Results
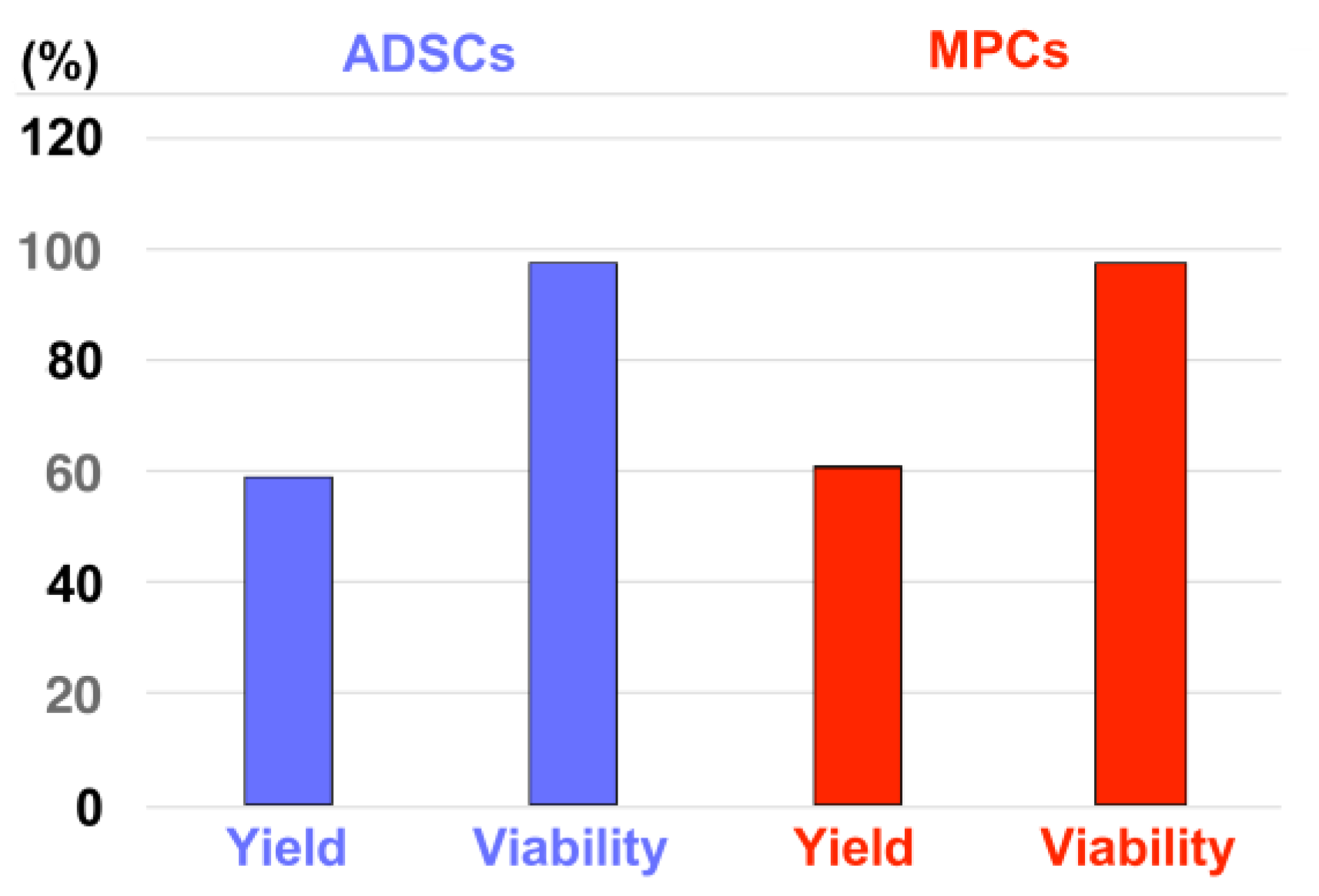
3.1. Determining the Calibre of the Waterjet Injection Devices for Cell Injections
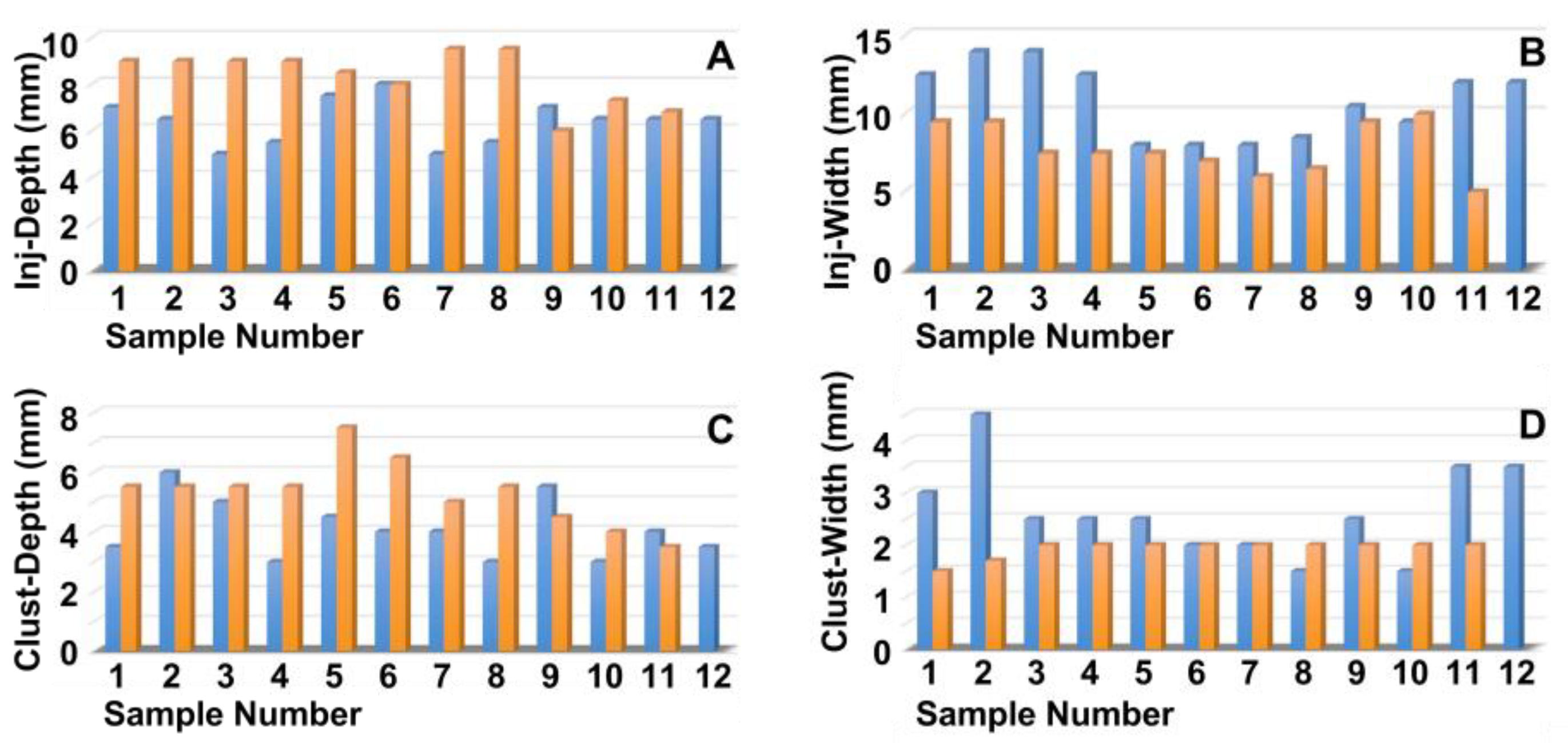
3.2. Determining the Pressure Levels Required to Transport the Particles in the Urethral Tissue
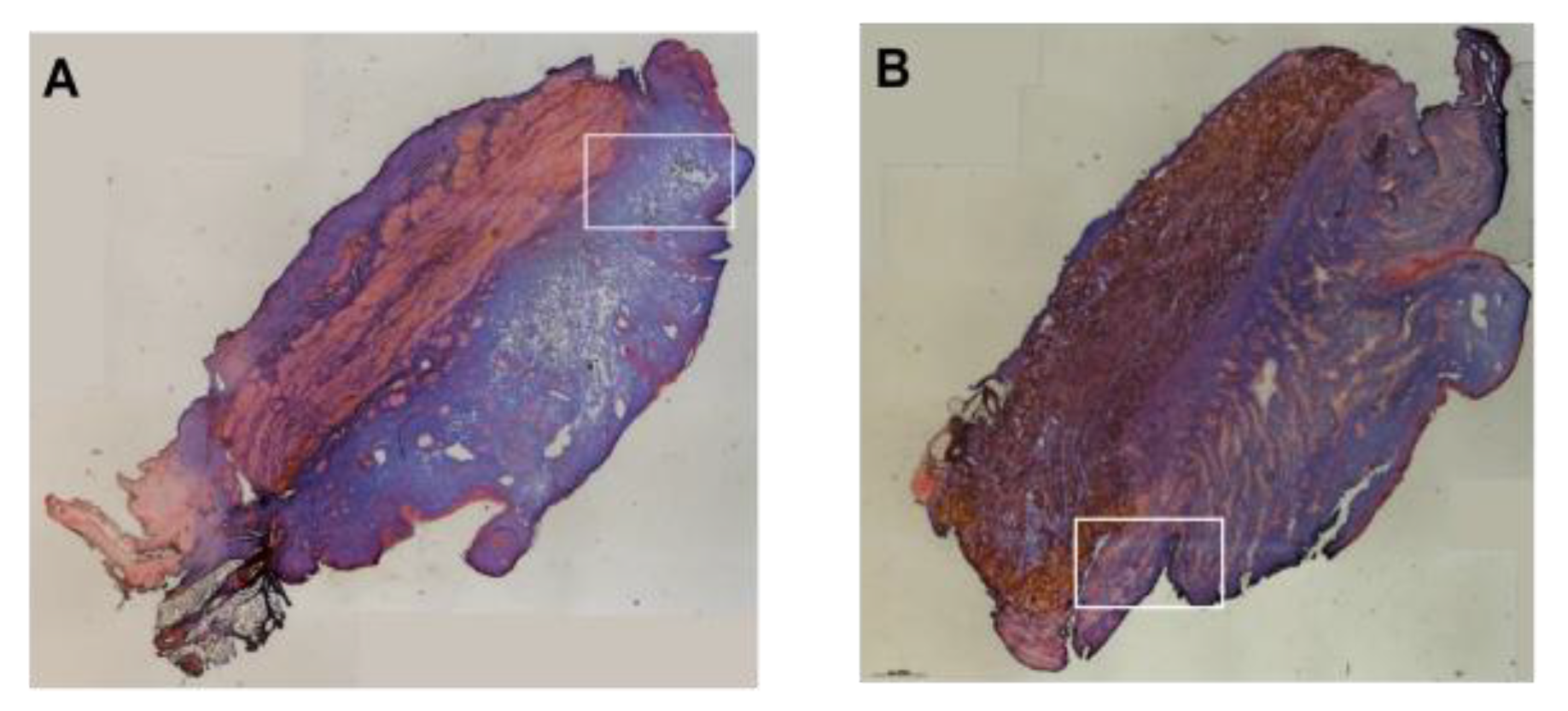
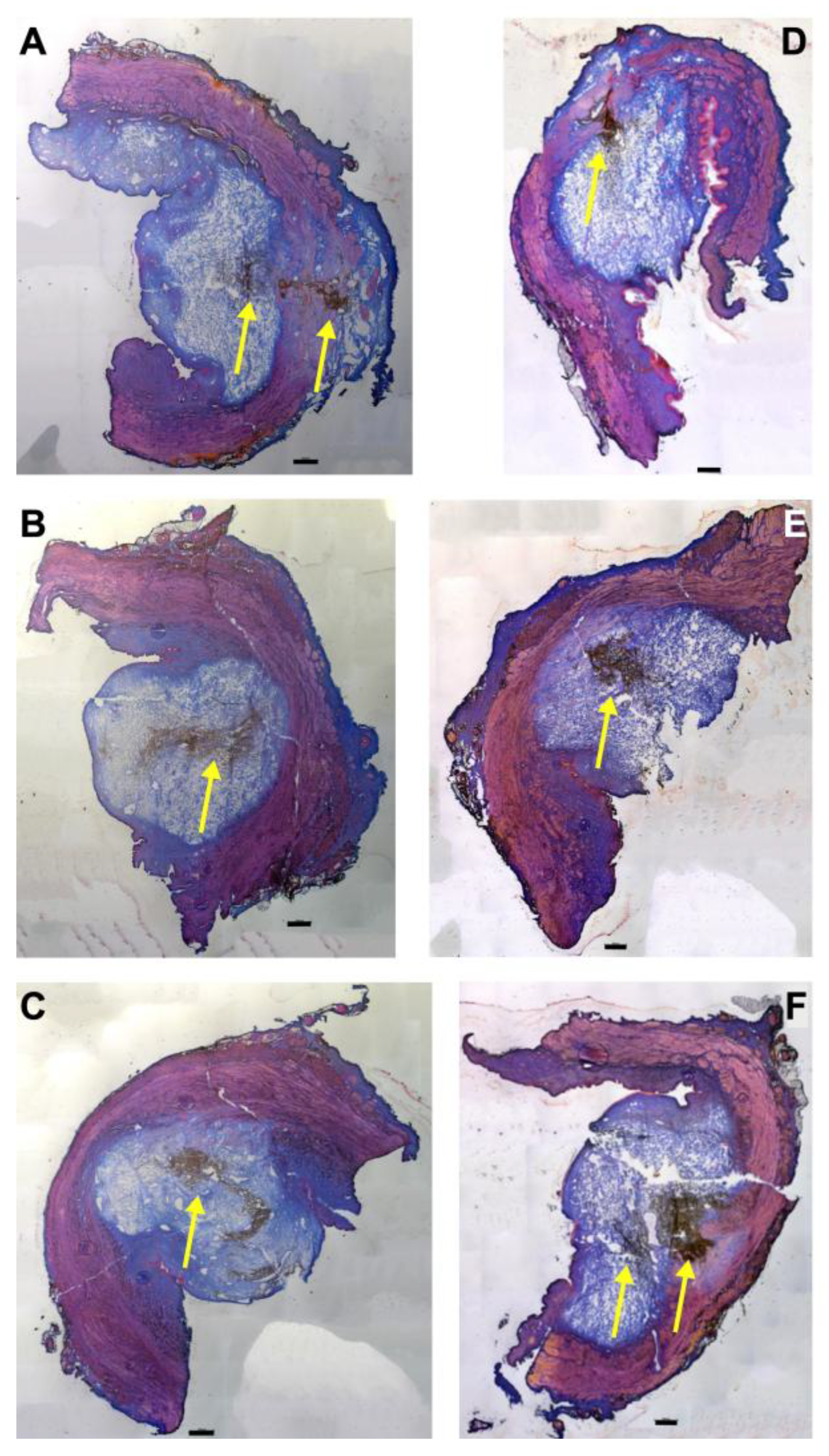
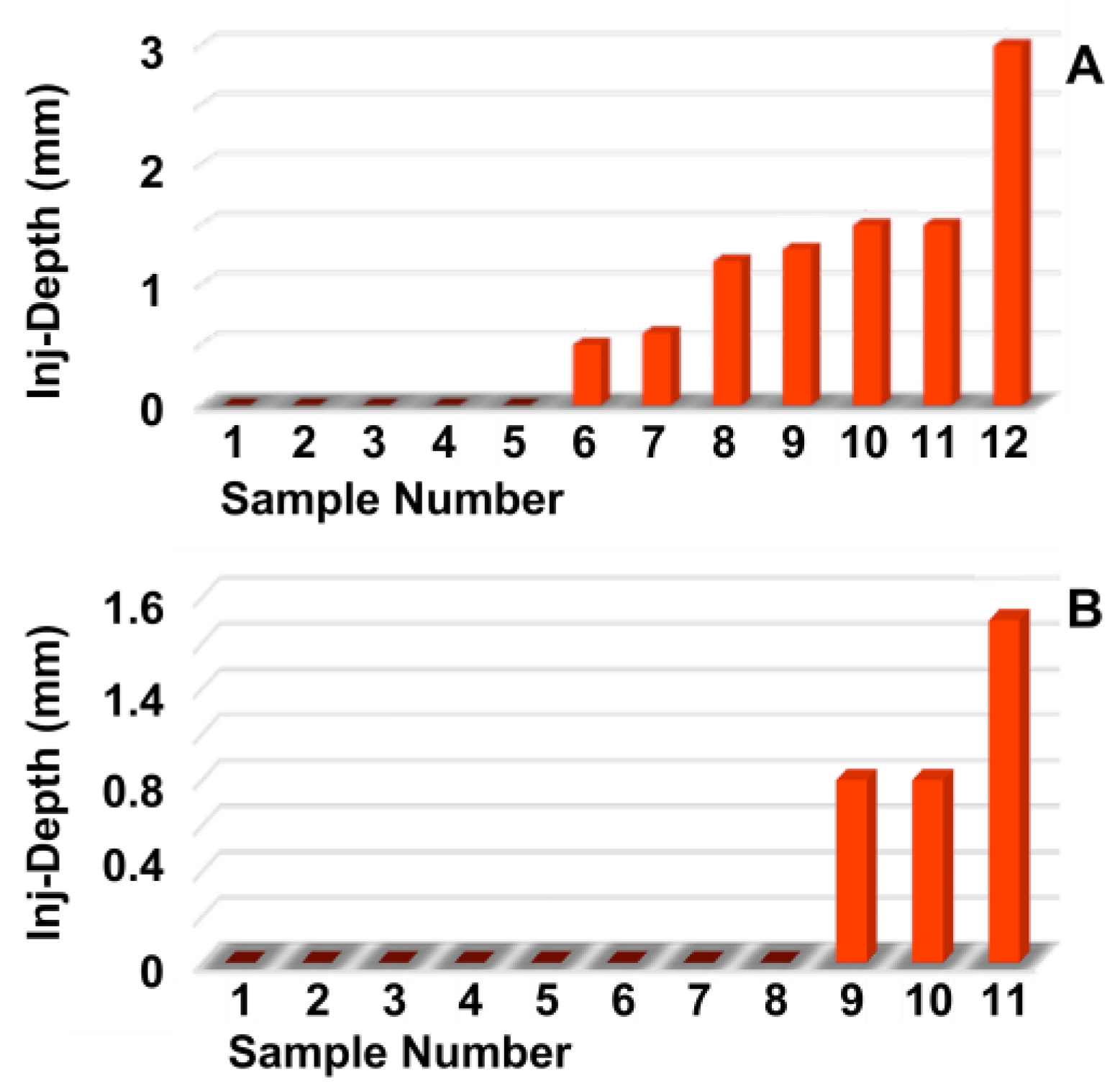
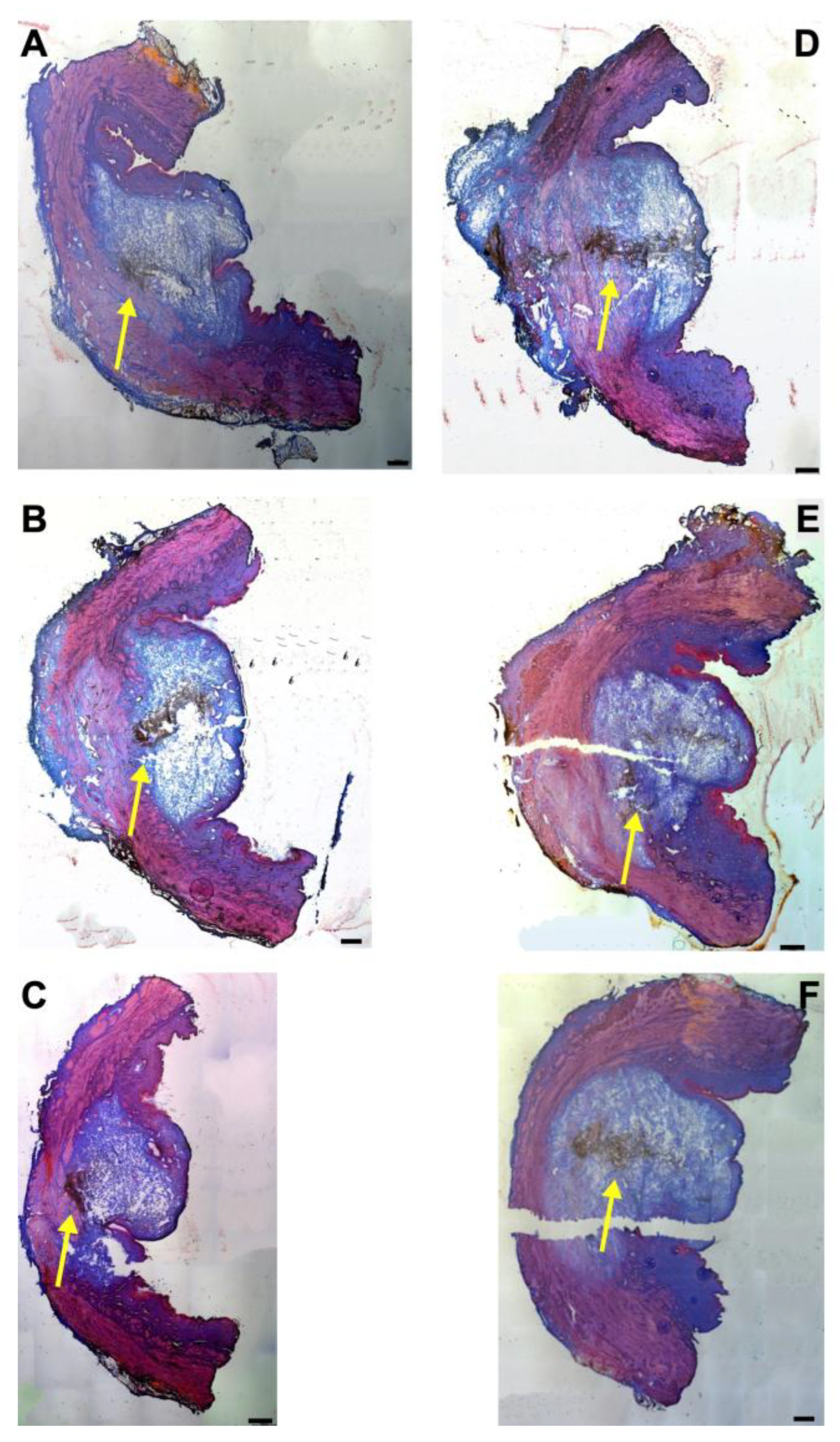
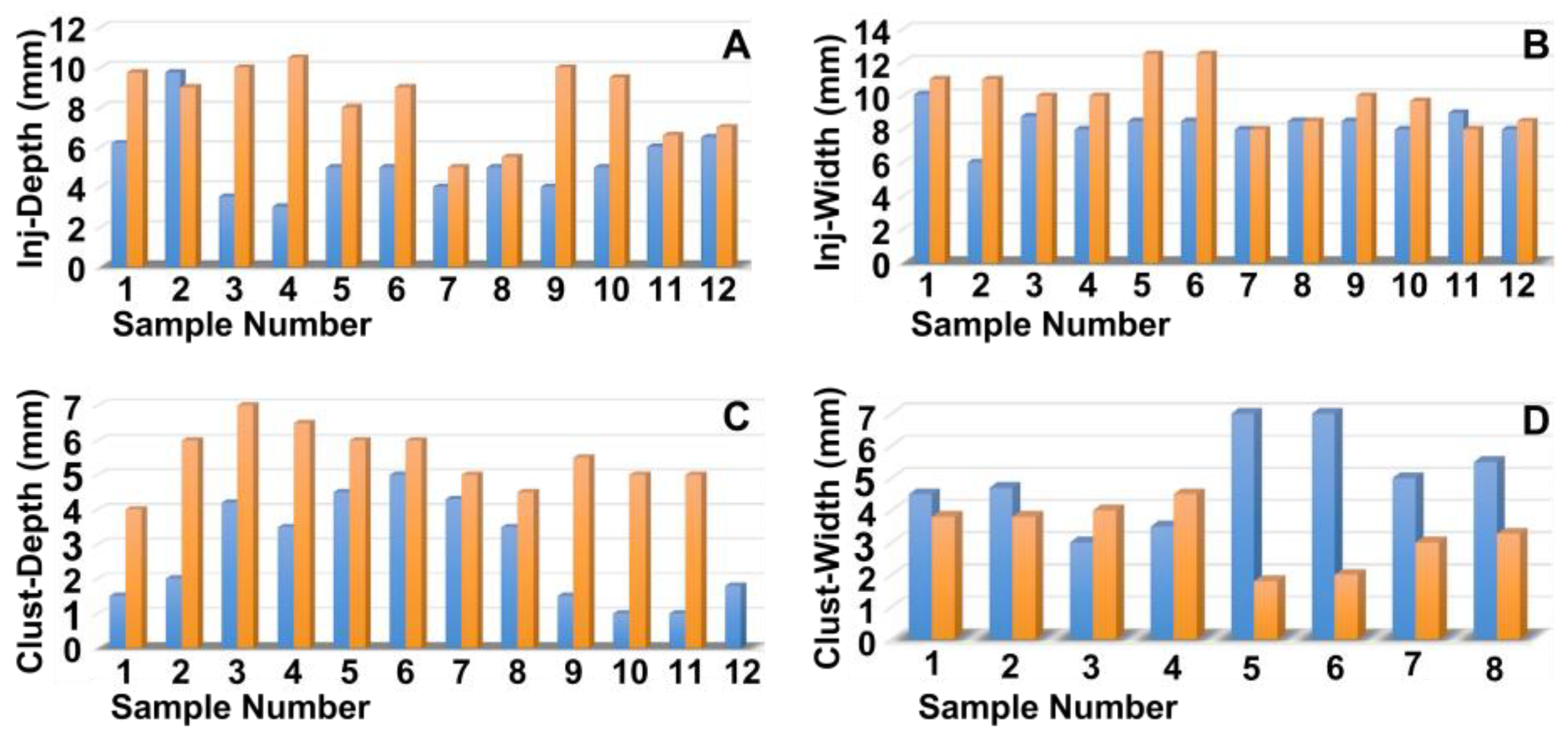
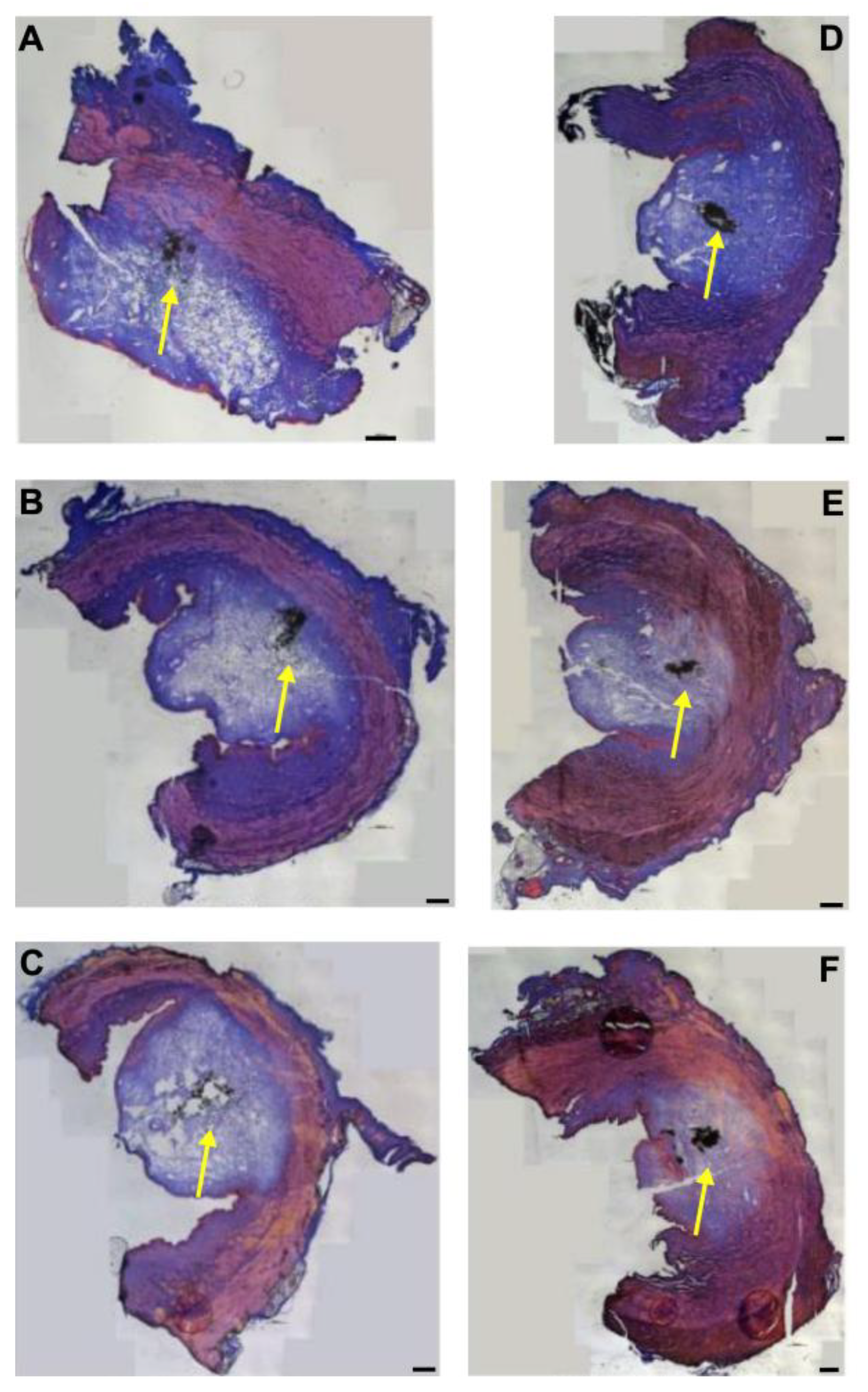
3.3. Injections of Nanoparticles in the Porcine Urethra by Waterjet with Moderate Pressure E60
3.4. Injections of Nanoparticles in the Porcine Urethra by Waterjet with Elevated Pressure E80
3.5. Injections of Microparticles in the Porcine Urethra by Waterjet with Moderate Pressure E60
3.6. Injections of Microparticles in the Porcine Urethra by Waterjet with Elevated Pressure
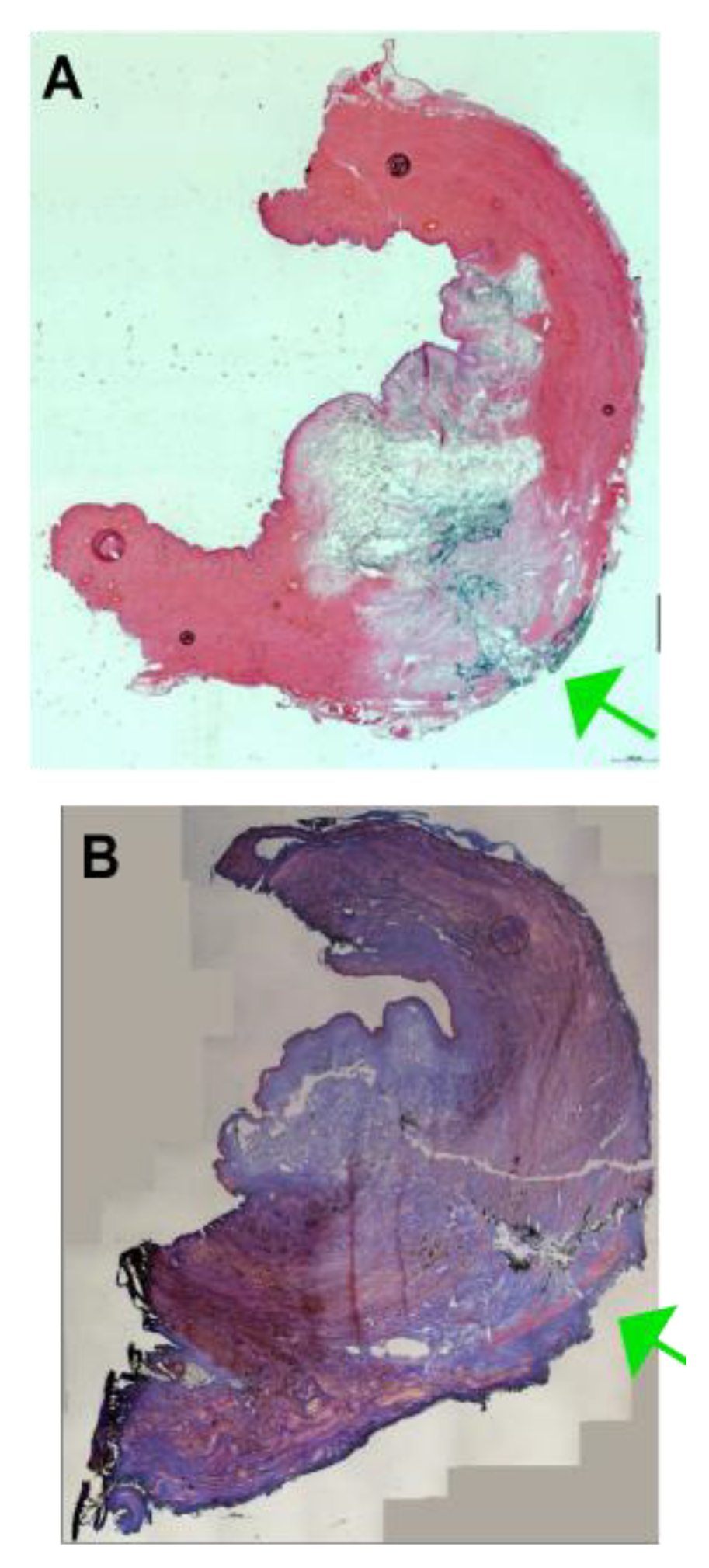
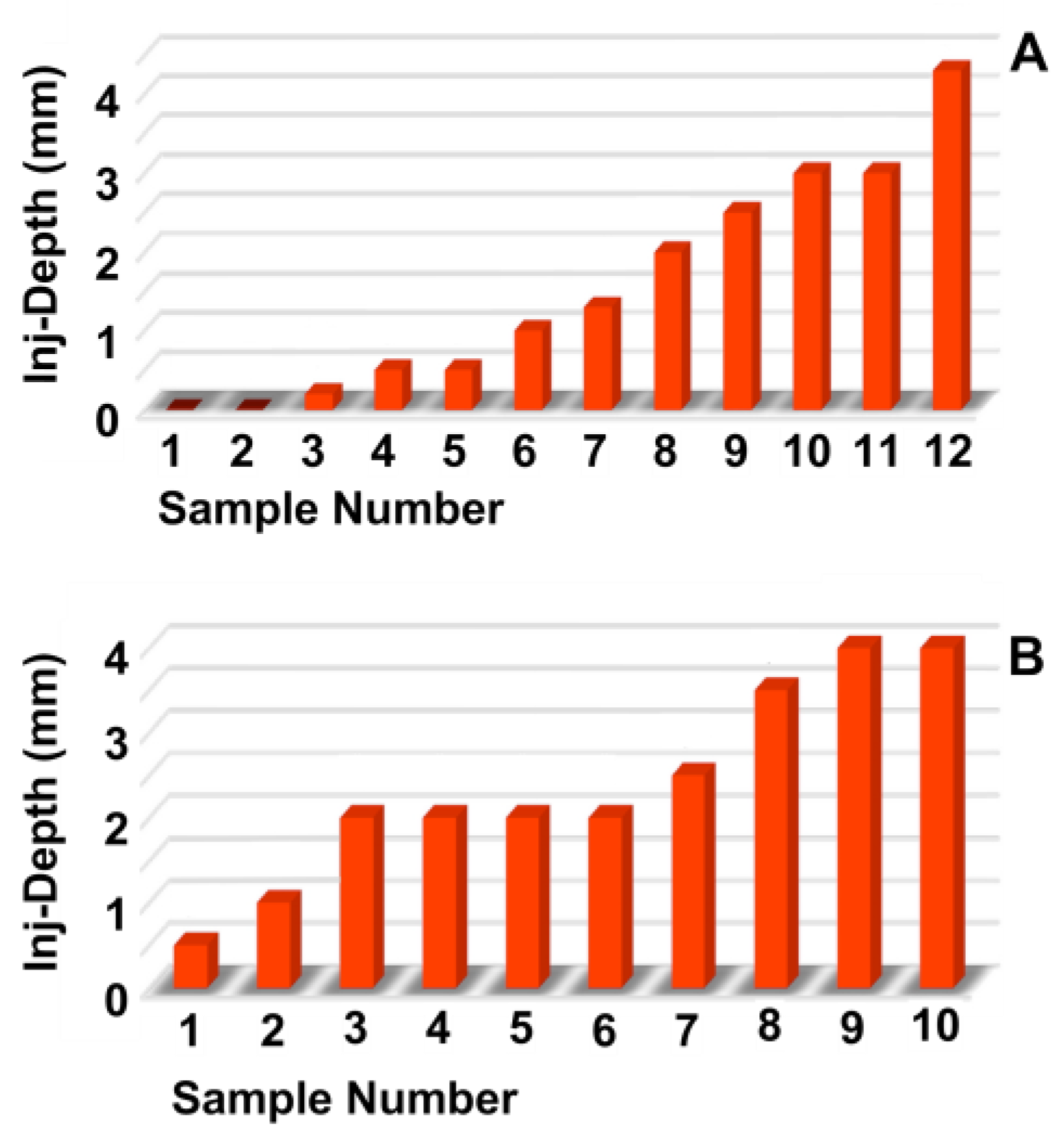
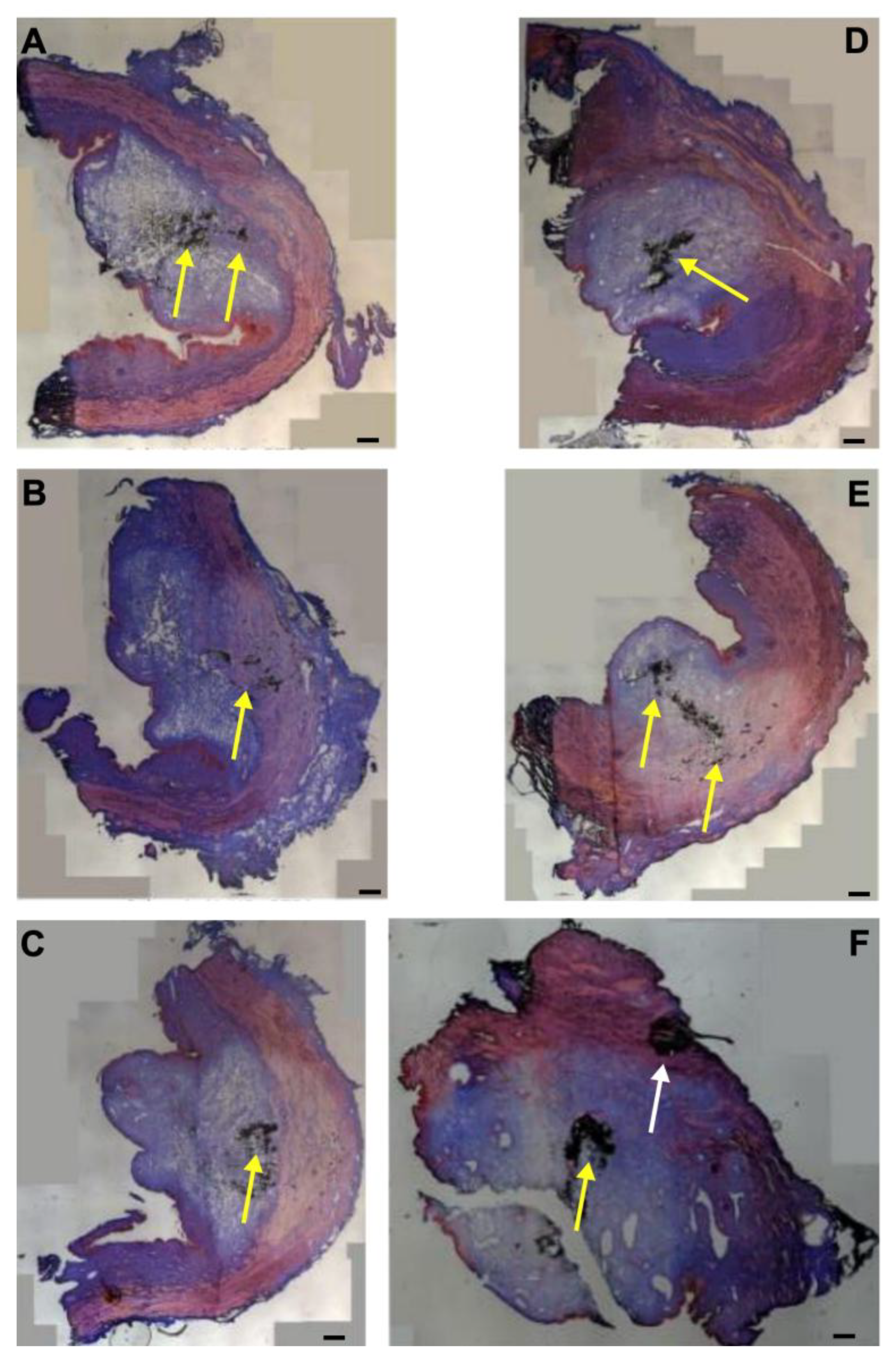
3.7. Injections of Isotonic Liquids in the Porcine Urethra by Waterjet
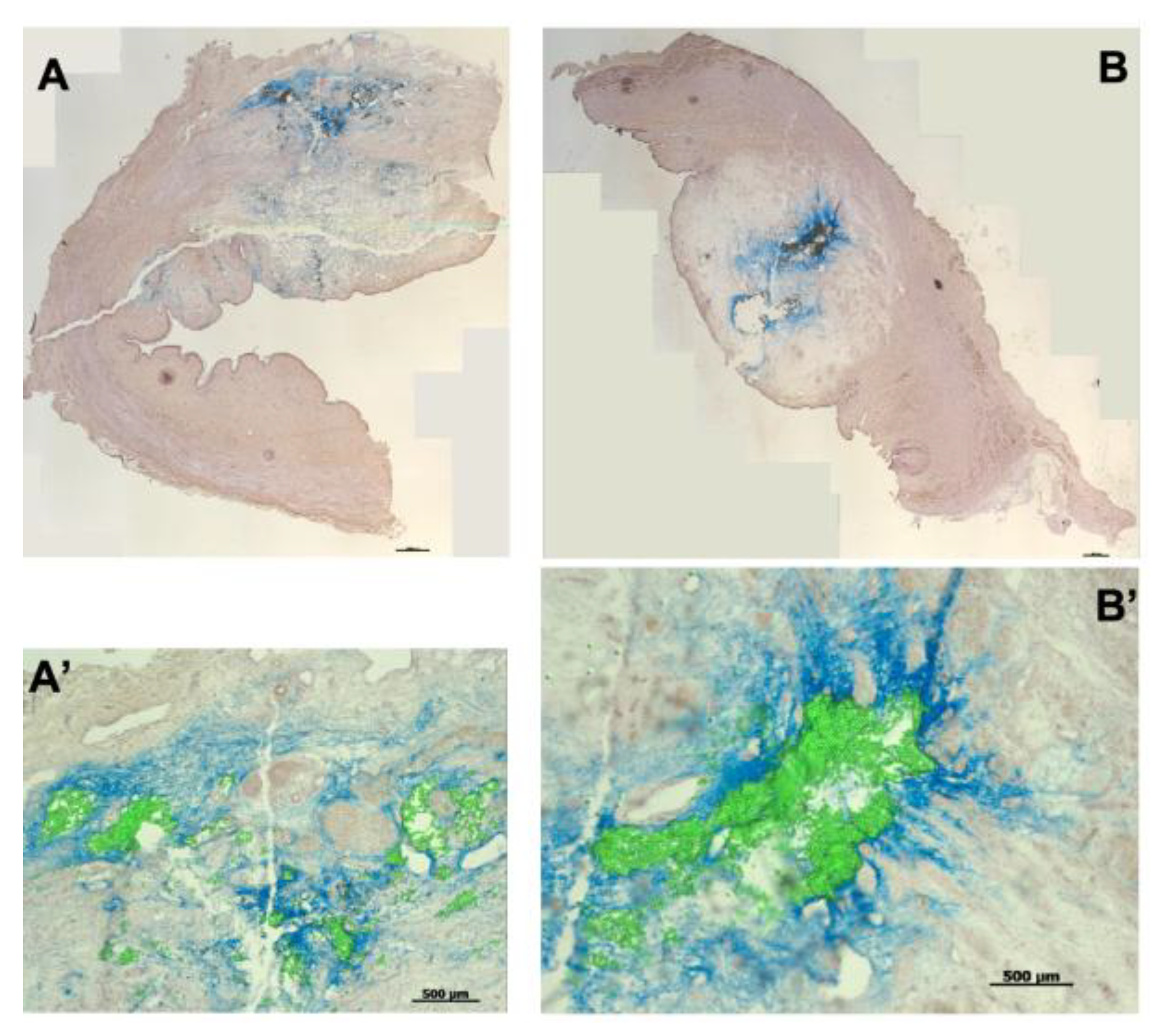
3.8. Injection of Porcine Stromal Cells and Myoblasts by Waterjet
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Figures and Legends


References
- Sussman, R.D.; Syan, R.; Brucker, B.M. Guideline of guidelines: Urinary incontinence in women. BJU Int. 2020, 125, 638–655. [Google Scholar] [CrossRef]
- Gacci, M.; Sakalis, V.I.; Karavitakis, M.; Cornu, J.N.; Gratzke, C.; Herrmann, T.R.W.; Kyriazis, I.; Malde, S.; Mamoulakis, C.; Rieken, M.; et al. European Association of Urology Guidelines on Male Urinary Incontinence. Eur. Urol. 2022, 82, 387–398. [Google Scholar] [CrossRef]
- Harland, N.; Walz, S.; Eberli, D.; Schmid, F.A.; Aicher, W.K.; Stenzl, A.; Amend, B. Stress Urinary Incontinence: An Unsolved Clinical Challenge. Biomedicines 2023, 11, 2486. [Google Scholar] [CrossRef] [PubMed]
- Broome, B.A. The impact of urinary incontinence on self-efficacy and quality of life. Health Qual. Life Outcomes 2003, 1, 35. [Google Scholar] [CrossRef]
- Milsom, I.; Gyhagen, M. The prevalence of urinary incontinence. Climacteric 2019, 22, 217–222. [Google Scholar] [CrossRef]
- Zimmern, P.; Litman, H.J.; Nager, C.W.; Lemack, G.E.; Richter, H.E.; Sirls, L.; Kraus, S.R.; Sutkin, G.; Mueller, E.R. Effect of Aging on Storage and Voiding Function in Women with Stress Predominant Urinary Incontinence. J. Urol. 2014, 192, 464–468. [Google Scholar] [CrossRef]
- Huebner, M.; Antolic, A.; Tunn, R. The impact of pregnancy and vaginal delivery on urinary incontinence. Int. J. Gynecol. Obstet. 2010, 110, 249–251. [Google Scholar] [CrossRef] [PubMed]
- Tähtinen, R.M.; Cartwright, R.; Tsui, J.F.; Aaltonen, R.L.; Aoki, Y.; Cárdenas, J.L.; El Dib, R.; Joronen, K.M.; Al Juaid, S.; Kalantan, S.; et al. Long-term Impact of Mode of Delivery on Stress Urinary Incontinence and Urgency Urinary Incontinence: A Systematic Review and Meta-analysis. Eur. Urol. 2016, 70, 148–158. [Google Scholar] [CrossRef] [PubMed]
- Osborn, D.J.; Strain, M.; Gomelsky, A.; Rothschild, J.; Dmochowski, R. Obesity and Female Stress Urinary Incontinence. Urology 2013, 82, 759–763. [Google Scholar] [CrossRef]
- Falah-Hassani, K.; Reeves, J.; Shiri, R.; Hickling, D.; McLean, L. The pathophysiology of stress urinary incontinence: A systematic review and meta-analysis. Int. Urogynecol. J. 2021, 32, 501–552, Erratum in Int. Urogynecol. J. 2021, 32, 1607. [Google Scholar] [CrossRef]
- Lokeshwar, S.D.; Harper, B.T.; Webb, E.; Jordan, A.; Dykes, T.A.; Neal, D.; Terris, M.K.; Klaassen, Z. Epidemiology and treatment modalities for the management of benign prostatic hyperplasia. Transl. Androl. Urol. 2019, 8, 529–539. [Google Scholar] [CrossRef]
- Hester, A.G.; Kretschmer, A.; Badlani, G. Male Incontinence: The Etiology or Basis of Treatment. Eur. Urol. Focus 2017, 3, 377–384. [Google Scholar] [CrossRef] [PubMed]
- Culp, M.B.; Soerjomataram, I.; Efstathiou, J.A.; Bray, F.; Jemal, A. Recent Global Patterns in Prostate Cancer Incidence and Mortality Rates. Eur. Urol. 2020, 77, 38–52. [Google Scholar] [CrossRef]
- Doan, D.K.; Schmidt, K.T.; Chau, C.H.; Figg, W.D. Germline Genetics of Prostate Cancer: Prevalence of Risk Variants and Clinical Implications for Disease Management. Cancers 2021, 13, 2154. [Google Scholar] [CrossRef]
- Lowrance, W.; Dreicer, R.; Jarrard, D.F.; Scarpato, K.R.; Kim, S.K.; Kirkby, E.; Buckley, D.I.; Griffin, J.C.; Cookson, M.S. Updates to Advanced Prostate Cancer: AUA/SUO Guideline (2023). J. Urol. 2023, 209, 1082–1090. [Google Scholar] [CrossRef]
- Ma, J.J.; Gharaee-Kermani, M.; Kunju, L.; Hollingsworth, J.M.; Adler, J.; Arruda, E.M.; Macoska, J.A. Prostatic Fibrosis is Associated with Lower Urinary Tract Symptoms. J. Urol. 2012, 188, 1375–1381. [Google Scholar] [CrossRef]
- Hillary, C.J.; Roman, S.; MacNeil, S.; Aicher, W.K.; Stenzl, A.; Chapple, C.R. Author Correction: Regenerative medicine and injection therapies in stress urinary incontinence. Nat. Rev. Urol. 2020, 17, 650. [Google Scholar] [CrossRef] [PubMed]
- Schmid, F.A.; Williams, J.K.; Kessler, T.M.; Stenzl, A.; Aicher, W.K.; Andersson, K.E.; Eberli, D. Treatment of Stress Urinary Incontinence with Muscle Stem Cells and Stem Cell Components: Chances, Challenges and Future Prospects. Int. J. Mol. Sci. 2021, 22, 3981. [Google Scholar] [CrossRef]
- Vinarov, A.; Atala, A.; Yoo, J.; Slusarenco, R.; Zhumataev, M.; Zhito, A.; Butnaru, D. Cell therapy for stress urinary incontinence: Present-day frontiers. J. Tissue Eng. Regen. Med. 2018, 12, e1108–e1121. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Pickles, T.; Berthelet, E.; Agranovich, A.; Kwan, W.; Tyldesley, S.; McKenzie, M.; Keyes, M.; Morris, J.; Pai, H.; et al. Urinary incontinence in prostate cancer patients treated with external beam radiotherapy. Radiother. Oncol. 2005, 74, 197–201. [Google Scholar] [CrossRef]
- Cozzarini, C.; Rancati, T.; Palorini, F.; Avuzzi, B.; Garibaldi, E.; Balestrini, D.; Cante, D.; Munoz, F.; Franco, P.; Girelli, G.; et al. Patient-reported urinary incontinence after radiotherapy for prostate cancer: Quantifying the dose–effect. Radiother. Oncol. 2017, 125, 101–106. [Google Scholar] [CrossRef]
- Dobberfuhl, A.D. Evaluation and treatment of female stress urinary incontinence after pelvic radiotherapy. Neurourol. Urodyn. 2019, 38, S59–S69. [Google Scholar] [CrossRef]
- Han, L.Y.; Wang, L.; Wang, Q.; Li, H.L.; Zang, H. Association between pelvic organ prolapse and stress urinary incontinence with collagen. Exp. Ther. Med. 2014, 7, 1337–1341. [Google Scholar] [CrossRef]
- Li, M.Z.; Qiu, K.X.; Guo, H.R.; Fan, M.S.; Yan, L. Conservative treatments for women with stress urinary incontinence: A systematic review and network meta-analysis. Front. Med. 2024, 11, 1517962. [Google Scholar] [CrossRef]
- Petca, A.; Fota, A.; Petca, R.C.; Rotar, I.C. Modern Conservative Management Strategies for Female Stress Urinary Incontinence: A Systematic Review. J. Clin. Med. 2025, 14, 3268. [Google Scholar] [CrossRef] [PubMed]
- Moris, L.; Heesakkers, J.; Nitti, V.; O’Connell, H.E.; Peyronnet, B.; Serati, M.; Omar, M.I.; Harding, C. Prevalence, Diagnosis, and Management of Stress Urinary Incontinence in Women: A Collaborative Review. Eur. Urol. 2025, 87, 292–301. [Google Scholar] [CrossRef] [PubMed]
- Hoe, V.; Haller, B.; Yao, H.; O’Connell, H. Urethral Bulking Agents for the Treatment of Stress Urinary Incontinence in Women: A Systematic Review. Neurourol. Urodyn. 2021, 40, S109–S110. [Google Scholar] [CrossRef]
- Goessens, E.M.V.; Cammu, H. A 10-to 20-year follow-up after tension-free vaginal tape for stress urinary incontinence. Int. Urogynecol. J. 2023, 34, 2107–2114. [Google Scholar] [CrossRef]
- Capobianco, G.; Saderi, L.; Dessole, F.; Petrillo, M.; Dessole, M.; Piana, A.; Cherchi, P.L.; Dessole, S.; Sotgiu, G. Efficacy and effectiveness of bulking agents in the treatment of stress and mixed urinary incontinence: A systematic review and meta-analysis. Maturitas 2020, 133, 13–31. [Google Scholar] [CrossRef] [PubMed]
- Wu, K.; Huang, E.; Kobashi, K.C. Evolution of stress urinary incontinence (SUI) outcomes assessment: A narrative review. Gynecol. Pelvic Med. 2024, 7, 24. [Google Scholar] [CrossRef]
- Braga, A.; Caccia, G.; Papadia, A.; Treglia, G.; Castronovo, F.; Salvatore, S.; Torella, M.; Ghezzi, F.; Serati, M. Urethral bulking agents for the treatment of recurrent stress urinary incontinence: A systematic review and meta-analysis. Maturitas 2022, 163, 28–37. [Google Scholar] [CrossRef]
- Yiou, R.; Yoo, J.J.; Atala, A. Restoration of functional motor units in a rat model of sphincter injury by muscle precursor cell autografts1. Transplantation 2003, 76, 1053–1060. [Google Scholar] [CrossRef] [PubMed]
- Eberli, D.; Andersson, K.E.; Yoo, J.J.; Atala, A. A canine model of irreversible urethral sphincter insufficiency. BJU Int. 2009, 103, 248–253. [Google Scholar] [CrossRef]
- Hijaz, A.; Daneshgari, F.; Sievert, K.D.; Damaser, M.S. Animal models of female stress urinary incontinence. J. Urol. 2008, 179, 2103–2110. [Google Scholar] [CrossRef] [PubMed]
- Burdzinska, A.; Dybowski, B.; Zarychta-Wisniewska, W.; Kulesza, A.; Butrym, M.; Zagozdzon, R.; Graczyk-Jarzynka, A.; Radziszewski, P.; Gajewski, Z.; Paczek, L. Intraurethral co-transplantation of bone marrow mesenchymal stem cells and muscle-derived cells improves the urethra closure. Stem Cell Res. Ther. 2018, 9, 239. [Google Scholar] [CrossRef]
- Burdzinska, A.; Dybowski, B.; Zarychta-Wisniewska, W.; Kulesza, A.; Hawryluk, J.; Graczyk-Jarzynka, A.; Kaupa, P.; Gajewski, Z.; Paczek, L. Limited accuracy of transurethral and periurethral intrasphincteric injections of cellular suspension. Neurourol. Urodyn. 2018, 37, 1612–1622. [Google Scholar] [CrossRef]
- Williams, J.K.; Badlani, G.; Dean, A.; Lankford, S.; Poppante, K.; Criswell, T.; Andersson, K.E. Local versus intravenous injections of skeletal muscle precursor cells in nonhuman primates with acute or chronic intrinsic urinary sphincter deficiency. Stem Cell Res. Ther. 2016, 7, 147. [Google Scholar] [CrossRef]
- González Enguita, C.; Garranzo García-Ibarrola, M.; Tufet I Jaumont, J.J.; Garde García, H.; González López, R.; Quintana Franco, L.M.; Torres Zambrano, G.M.; García-Arranz, M. Cell Therapy in the Treatment of Female Stress Urinary Incontinence: Current Status and Future Proposals. Life 2024, 14, 861. [Google Scholar] [CrossRef]
- Amend, B.; Kelp, A.; Vaegler, M.; Klunder, M.; Frajs, V.; Klein, G.; Sievert, K.D.; Sawodny, O.; Stenzl, A.; Aicher, W.K. Precise injection of human mesenchymal stromal cells in the urethral sphincter complex of Gottingen minipigs without unspecific bulking effects. Neurourol. Urodyn. 2017, 36, 1723–1733. [Google Scholar] [CrossRef]
- Chermansky, C.J.; Tarin, T.; Kwon, D.D.; Jankowski, R.J.; Cannon, T.W.; de Groat, W.C.; Huard, J.; Chancellor, M.B. Intraurethral muscle-derived cell injections increase leak point pressure in a rat model of intrinsic sphincter deficiency. Urology 2004, 63, 780–785. [Google Scholar] [CrossRef] [PubMed]
- Herrera-Imbroda, B.; Lara, M.F.; Izeta, A.; Sievert, K.D.; Hart, M.L. Stress urinary incontinence animal models as a tool to study cell-based regenerative therapies targeting the urethral sphincter. Adv. Drug Deliv. Rev. 2015, 82–83, 106–116. [Google Scholar] [CrossRef]
- Ganzer, R.; Köhler, D.; Neuhaus, J.; Dorschner, W.; Stolzenburg, J.-U. Is the Rhesus Monkey (Macaca mulatta) Comparable to Humans? Histomorphology of the Sphincteric Musculature of the Lower Urinary Tract Including 3D-reconstruction. Anat. Histol. Embryol. 2004, 33, 355–361. [Google Scholar] [CrossRef] [PubMed]
- Amend, B.; Harland, N.; Knoll, J.; Stenzl, A.; Aicher, W.K. Large Animal Models for Investigating Cell Therapies of Stress Urinary Incontinence. Int. J. Mol. Sci. 2021, 22, 6092. [Google Scholar] [CrossRef] [PubMed]
- Wallner, C.; Dabhoiwala, N.F.; DeRuiter, M.C.; Lamers, W.H. The anatomical components of urinary continence. Eur. Urol. 2009, 55, 932–943. [Google Scholar] [CrossRef] [PubMed]
- Jung, J.; Ahn, H.K.; Huh, Y. Clinical and functional anatomy of the urethral sphincter. Int. Neurourol. J. 2012, 16, 102–106. [Google Scholar] [CrossRef]
- Zini, L.; Lecoeur, C.; Swieb, S.; Combrisson, H.; Delmas, V.; Gherardi, R.; Abbou, C.; Chopin, D.; Yiou, R. The striated urethral sphincter of the pig shows morphological and functional characteristics essential for the evaluation of treatments for sphincter insufficiency. J. Urol. 2006, 176, 2729–2735. [Google Scholar] [CrossRef]
- Chen, Y.J.; Liu, H.Y.; Chang, Y.T.; Cheng, Y.H.; Mersmann, H.J.; Kuo, W.H.; Ding, S.T. Isolation and Differentiation of Adipose-Derived Stem Cells from Porcine Subcutaneous Adipose Tissues. JOVE 2016, 109, 53886. [Google Scholar] [CrossRef]
- Ding, S.J.; Wang, F.; Liu, Y.; Liz, S.; Zhou, G.H.; Hu, P. Characterization and isolation of highly purified porcine satellite cells. Cell Death Discov. 2017, 3, 17003. [Google Scholar] [CrossRef]
- Knoll, J.; Amend, B.; Abruzzese, T.; Harland, N.; Stenzl, A.; Aicher, W.K. Production of Proliferation- and Differentiation-Competent Porcine Myoblasts for Preclinical Studies in a Porcine Large Animal Model of Muscular Insufficiency. Life 2024, 14, 212. [Google Scholar] [CrossRef]
- Kelp, A.; Albrecht, A.; Amend, B.; Klunder, M.; Rapp, P.; Sawodny, O.; Stenzl, A.; Aicher, W.K. Establishing and monitoring of urethral sphincter deficiency in a large animal model. World J. Urol. 2017, 35, 1977–1986. [Google Scholar] [CrossRef]
- Jager, L.; Linzenbold, W.; Fech, A.; Enderle, M.; Abruzzese, T.; Stenzl, A.; Aicher, W.K. A novel waterjet technology for transurethral cystoscopic injection of viable cells in the urethral sphincter complex. Neurourol. Urodyn. 2020, 39, 594–602. [Google Scholar] [CrossRef]
- Yahagi, N.; Neuhaus, H.; Schumacher, B.; Neugebauer, A.; Kaehler, G.F.; Schenk, M.; Fischer, K.; Fujishiro, M.; Enderle, M.D. Comparison of standard endoscopic submucosal dissection (ESD) versus an optimized ESD technique for the colon: An animal study. Endoscopy 2009, 41, 340–345. [Google Scholar] [CrossRef]
- Agency, E.M. Advanced Therapy Medicinal Products: Overview. Available online: https://www.ema.europa.eu/en/human-regulatory-overview/advanced-therapy-medicinal-products-overview (accessed on 14 October 2025).
- Linzenbold, W.; Jager, L.; Stoll, H.; Abruzzese, T.; Harland, N.; Beziere, N.; Fech, A.; Enderle, M.; Amend, B.; Stenzl, A.; et al. Rapid and precise delivery of cells in the urethral sphincter complex by a novel needle-free waterjet technology. BJU Int. 2021, 127, 463–472. [Google Scholar] [CrossRef] [PubMed]
- Schulz, J.A.; Nager, C.W.; Stanton, S.L.; Baessler, K. Bulking agents for stress urinary incontinence: Short-term results and complications in a randomized comparison of periurethral and transurethral injections. Int. Urogynecol. J. 2004, 15, 261–265. [Google Scholar] [CrossRef] [PubMed]
- Geng, R.; Knoll, J.; Harland, N.; Amend, B.; Enderle, M.D.; Linzenbold, W.; Abruzzese, T.; Kalbe, C.; Kemter, E.; Wolf, E.; et al. Replacing Needle Injection by a Novel Waterjet Technology Grants Improved Muscle Cell Delivery in Target Tissues. Cell Transplant. 2022, 31, 9636897221080943. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Harland, N.; Fech, A.; Linzenbold, W.; Amend, B.; Stenzl, A.; Rajendran, M.D.V.; Enderle, M.D.; Aicher, W.K. A Novel Technology for Needle-Free Injections of Liquids, Particles and Viable Cells into the Submucosa of the Urethra by a Pressure-Controlled Waterjet Technology. Biomedicines 2025, 13, 2986. https://doi.org/10.3390/biomedicines13122986
Harland N, Fech A, Linzenbold W, Amend B, Stenzl A, Rajendran MDV, Enderle MD, Aicher WK. A Novel Technology for Needle-Free Injections of Liquids, Particles and Viable Cells into the Submucosa of the Urethra by a Pressure-Controlled Waterjet Technology. Biomedicines. 2025; 13(12):2986. https://doi.org/10.3390/biomedicines13122986
Chicago/Turabian StyleHarland, Niklas, Andreas Fech, Walter Linzenbold, Bastian Amend, Arnulf Stenzl, M. D. Venkatachalam Rajendran, Markus D. Enderle, and Wilhelm K. Aicher. 2025. "A Novel Technology for Needle-Free Injections of Liquids, Particles and Viable Cells into the Submucosa of the Urethra by a Pressure-Controlled Waterjet Technology" Biomedicines 13, no. 12: 2986. https://doi.org/10.3390/biomedicines13122986
APA StyleHarland, N., Fech, A., Linzenbold, W., Amend, B., Stenzl, A., Rajendran, M. D. V., Enderle, M. D., & Aicher, W. K. (2025). A Novel Technology for Needle-Free Injections of Liquids, Particles and Viable Cells into the Submucosa of the Urethra by a Pressure-Controlled Waterjet Technology. Biomedicines, 13(12), 2986. https://doi.org/10.3390/biomedicines13122986






