The Role of Immature Granulocytes in Fibromyalgia: An Indicator of Subclinical Inflammation?
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Clinical Measurements
3. Statistics
4. Results
5. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Maffei, M.E. Fibromyalgia: Recent Advances in Diagnosis, Classification, Pharmacotherapy and Alternative Remedies. Int. J. Mol. Sci. 2020, 21, 7877. [Google Scholar] [CrossRef] [PubMed]
- Bellato, E.; Marini, E.; Castoldi, F.; Barbasetti, N.; Mattei, L.; Bonasia, D.E.; Blonna, D. Fibromyalgia syndrome: Etiology, pathogenesis, diagnosis, and treatment. Pain Res. Treat. 2012, 2012, 426130. [Google Scholar] [CrossRef]
- Meester, I.; Rivera-Silva, G.F.; González-Salazar, F. Immune System Sex Differences May Bridge the Gap Between Sex and Gender in Fibromyalgia. Front. Neurosci. 2019, 13, 1414. [Google Scholar] [CrossRef]
- Ruschak, I.; Montesó-Curto, P.; Rosselló, L.; Aguilar Martín, C.; Sánchez-Montesó, L.; Toussaint, L. Fibromyalgia Syndrome Pain in Men and Women: A Scoping Review. Healthcare 2023, 11, 223. [Google Scholar] [CrossRef]
- Schertzinger, M.; Wesson-Sides, K.; Parkitny, L.; Younger, J. Daily Fluctuations of Progesterone and Testosterone Are Associated with Fibromyalgia Pain Severity. J. Pain 2018, 19, 410–417. [Google Scholar] [CrossRef]
- Chinn, S.; Caldwell, W.; Gritsenko, K. Fibromyalgia Pathogenesis and Treatment Options Update. Curr. Pain Headache Rep. 2016, 20, 25. [Google Scholar] [CrossRef]
- Siracusa, R.; Paola, R.D.; Cuzzocrea, S.; Impellizzeri, D. Fibromyalgia: Pathogenesis, Mechanisms, Diagnosis and Treatment Options Update. Int. J. Mol. Sci. 2021, 22, 3891. [Google Scholar] [CrossRef] [PubMed]
- Coskun Benlidayi, I. Role of inflammation in the pathogenesis and treatment of fibromyalgia. Rheumatol. Int. 2019, 39, 781–791. [Google Scholar] [CrossRef]
- Bazzichi, L.; Rossi, A.; Massimetti, G.; Giannaccini, G.; Giuliano, T.; De Feo, F.; Ciapparelli, A.; Dell’Osso, L.; Bombardieri, S. Cytokine patterns in fibromyalgia and their correlation with clinical manifestations. Clin. Exp. Rheumatol. 2007, 25, 225–230. [Google Scholar]
- Cetın, N.; Kocaturk, E.; Tufan, A.K.; Kıraz, Z.K.; Alatas, O. Immature granulocytes as biomarkers of inflammation in children with predialysis chronic kidney disease. Pediatr. Nephrol. 2023, 38, 219–225. [Google Scholar] [CrossRef] [PubMed]
- Biyik, Z.; Yavuz, Y.C.; Altintepe, L.; Cizmecioglu, A.; Yakşı, E.; Korez, M.K.; Yılmaz, S. Immature Granulocyte: A Novel Inflammatory Biomarker in Familial Mediterranean Fever. Int. J. Rheum. Dis. 2025, 28, e70149. [Google Scholar] [CrossRef]
- Ayres, L.S.; Sgnaolin, V.; Munhoz, T.P. Immature granulocytes index as early marker of sepsis. Int. J. Lab. Hematol. 2019, 41, 392–396. [Google Scholar] [CrossRef]
- Georgakopoulou, V.E.; Makrodimitri, S.; Triantafyllou, M.; Samara, S.; Voutsinas, P.M.; Anastasopoulou, A.; Papageorgiou, C.V.; Spandidos, D.A.; Gkoufa, A.; Papalexis, P.; et al. Immature granulocytes: Innovative biomarker for SARS-CoV-2 infection. Mol. Med. Rep. 2022, 26, 217. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, F.; Clauw, D.J.; Fitzcharles, M.-A.; Goldenberg, D.L.; Häuser, W.; Katz, R.L.; Mease, P.J.; Russell, A.S.; Russell, I.J.; Walitt, B. 2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteria. Semin. Arthritis Rheum. 2016, 46, 319–329. [Google Scholar] [CrossRef]
- Sarmer, S.; Ergin, S.; Yavuzer, G. The validity and reliability of the Turkish version of the Fibromyalgia Impact Questionnaire. Rheumatol. Int. 2000, 20, 9–12. [Google Scholar] [CrossRef] [PubMed]
- Sarzi-Puttini, P.; Giorgi, V.; Marotto, D.; Atzeni, F. Fibromyalgia: An update on clinical characteristics, aetiopathogenesis and treatment. Nat. Rev. Rheumatol. 2020, 16, 645–660. [Google Scholar] [CrossRef] [PubMed]
- García-Domínguez, M. Fibromyalgia and Inflammation: Unrevealing the Connection. Cells 2025, 14, 271. [Google Scholar] [CrossRef] [PubMed]
- Littlejohn, G.; Guymer, E. Neurogenic inflammation in fibromyalgia. Semin. Immunopathol. 2018, 40, 291–300. [Google Scholar] [CrossRef]
- Arnold, L.M.; Gebke, K.B.; Choy, E.H. Fibromyalgia: Management strategies for primary care providers. Int. J. Clin. Pract. 2016, 70, 99–112. [Google Scholar] [CrossRef]
- Carvalho, L.S.; Correa, H.; Silva, G.C.; Campos, F.S.; Baião, F.R.; Ribeiro, L.S.; Faria, A.M.; d’Avila Reis, D. May genetic factors in fibromyalgia help to identify patients with differentially altered frequencies of immune cells? Clin. Exp. Immunol. 2008, 154, 346–352. [Google Scholar] [CrossRef]
- D’Agnelli, S.; Arendt-Nielsen, L.; Gerra, M.C.; Zatorri, K.; Boggiani, L.; Baciarello, M.; Bignami, E. Fibromyalgia: Genetics and epigenetics insights may provide the basis for the development of diagnostic biomarkers. Mol. Pain 2019, 15, 1–12. [Google Scholar] [CrossRef]
- Erdrich, S.; Hawrelak, J.A.; Myers, S.P.; Harnett, J.E. Determining the association between fibromyalgia, the gut microbiome and its biomarkers: A systematic review. BMC Musculoskelet. Disord. 2020, 21, 181. [Google Scholar] [CrossRef]
- Iannuccelli, C.; Favretti, M.; Dolcini, G.; Di Carlo, M.; Pellegrino, G.; Bazzichi, L.; Atzeni, F.; Lucini, D.; Varassi, G.; Leoni, M.L.G.; et al. Fibromyalgia: One year in review 2025. Clin. Exp. Rheumatol. 2025, 43, 957–969. [Google Scholar] [CrossRef] [PubMed]
- Badaeva, A.; Danilov, A.; Kosareva, A.; Lepshina, M.; Novikov, V.; Vorobyeva, Y.; Danilov, A. Neuronutritional Approach to Fibromyalgia Management: A Narrative Review. Pain Ther. 2024, 13, 1047–1061. [Google Scholar] [CrossRef]
- Nadal-Nicolás, Y.; Miralles-Amorós, L.; Martínez-Olcina, M.; Sánchez-Ortega, M.; Mora, J.; Martínez-Rodríguez, A. Vegetarian and Vegan Diet in Fibromyalgia: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 4955. [Google Scholar] [CrossRef]
- Aktürk, S.; Büyükavcı, R. Evaluation of blood neutrophil-lymphocyte ratio and platelet distribution width as inflammatory markers in patients with fibromyalgia. Clin. Rheumatol. 2017, 36, 1885–1889. [Google Scholar] [CrossRef]
- Khamisy-Farah, R.; Fund, E.; Raibman-Spector, S.; Adawi, M. Inflammatory Markers in the Diagnosis of Fibromyalgia. Isr. Med. Assoc. J. 2021, 23, 801–804. [Google Scholar]
- Sariyildiz, A.; Benlidayi, I.C.; Ornek, C.; Basaran, S. Value of Diverse Hematological Markers in Fibromyalgia: A Real-World Study. J. Clin. Pract. Res. 2024, 46, 370–376. [Google Scholar] [CrossRef]
- Deniz, M.; Sahin Yildirim, Z.; Erdin, Z.; Alisik, M.; Erdin, R.; Yildirim, M. Role of immature granulocytes in monitoring sepsis treatment. BMC Anesthesiol. 2025, 25, 198. [Google Scholar] [CrossRef]
- Jeon, K.; Lee, N.; Jeong, S.; Park, M.J.; Song, W. Immature granulocyte percentage for prediction of sepsis in severe burn patients: A machine leaning-based approach. BMC Infect. Dis. 2021, 21, 1258. [Google Scholar] [CrossRef] [PubMed]
- Korkmaz, M.F.; Karacan, A.; Mehmedali, A.; Bozdemir, Ş.E.; Arslan, D.; Oto, A.; Tutanç, M. Immature granulocytes as an early clinical predictor in children with respiratory syncytial virus bronchiolitis. Pediatr. Int. 2024, 66, e15840. [Google Scholar] [CrossRef]
- Aydin, G.; Akdogan, R.A.; Rakici, H.; Akdogan, E. Predictive value of immature granulocyte percentage and neutrophil lymphocyte ratio in terms of prognosis in the course of acute pancreatitis. Bratisl. Lek. Listy 2024, 125, 477–483. [Google Scholar] [CrossRef] [PubMed]
- Xu, T.T.; Chen, S.B. The value of immature granulocyte percentage united with D-Dimer in the evaluation of severe pancreatitis and its prognosis. Clinics 2024, 79, 100446. [Google Scholar] [CrossRef]
- Seringec Akkececi, N.; Ciftcioglu, M.; Okyar, B.; Yildirim Cetin, G. Relationship of immature granulocytes with disease activity in rheumatoid arthritis. Int. J. Rheum. Dis. 2024, 27, e15216. [Google Scholar] [CrossRef] [PubMed]
- Okyar, B.; Yüce, S.; Bilen, İ.H.; Torun, B.; Öztürk, İ.; Çetin, G.Y. Changes in immature granulocyte levels and their association with disease activation following biologic therapy in patients with ankylosing spondylitis. Reumatol. Clin. 2024, 20, 533–538. [Google Scholar] [CrossRef]
- Haliloğlu, S.; Carlioglu, A.; Sahiner, E.; Karaaslan, Y.; Kosar, A. Mean platelet volume in patients with fibromyalgia. Z. Rheumatol. 2014, 73, 742–745. [Google Scholar] [CrossRef]
- Molina, F.; Del Moral, M.L.; La Rubia, M.; Blanco, S.; Carmona, R.; Rus, A. Are Patients With Fibromyalgia in a Prothrombotic State? Biol. Res. Nurs. 2019, 21, 224–230. [Google Scholar] [CrossRef] [PubMed]
- Karlıbel, İ.A.; Demirci, H.; Kasapoğlu, M.; Türe, D.A.; Altan, L. The relationship between vitamin 25 (OH) D level and hematological parameters in newly diagnosed women with fibromyalgia syndrome. J. Surg. Med. 2021, 5, 61–65. [Google Scholar]
- Jiang, C.; Wu, Y.; Huang, J.; Wang, Y.; Cong, H. Clinical value of complete blood count ratio in benign and malignant thyroid diseases. Cancer Epidemiol. 2024, 92, 102636. [Google Scholar] [CrossRef]
- Wysokiński, A.; Szczepocka, E. Platelet parameters (PLT, MPV, P-LCR) in patients with schizophrenia, unipolar depression and bipolar disorder. Psychiatry Res. 2016, 237, 238–245. [Google Scholar] [CrossRef]
- Bousounis, P.; Bergo, V.; Trompouki, E. Inflammation, Aging and Hematopoiesis: A Complex Relationship. Cells 2021, 10, 1386. [Google Scholar] [CrossRef] [PubMed]
| FM | Healthy Control | p * | p ** | |
|---|---|---|---|---|
| Mean ± SD; Median (Min-Max) | Mean ± SD; Median (Min-Max) | |||
| Age | 44.6 ± 9.4 | 40.37 ± 10.33 | 0.009 | |
| FIQ | 70.06 ± 13.74 | |||
| FSDC | 20 ± 3.83 | |||
| ESR (mm/h) | 9 (2–33) | 10 (2–24) | 0.562 | 0.364 |
| CRP (mg/L) | 2.37 (0.2–16) | 1.8 (0.2–16.26) | 0.537 | 0.803 |
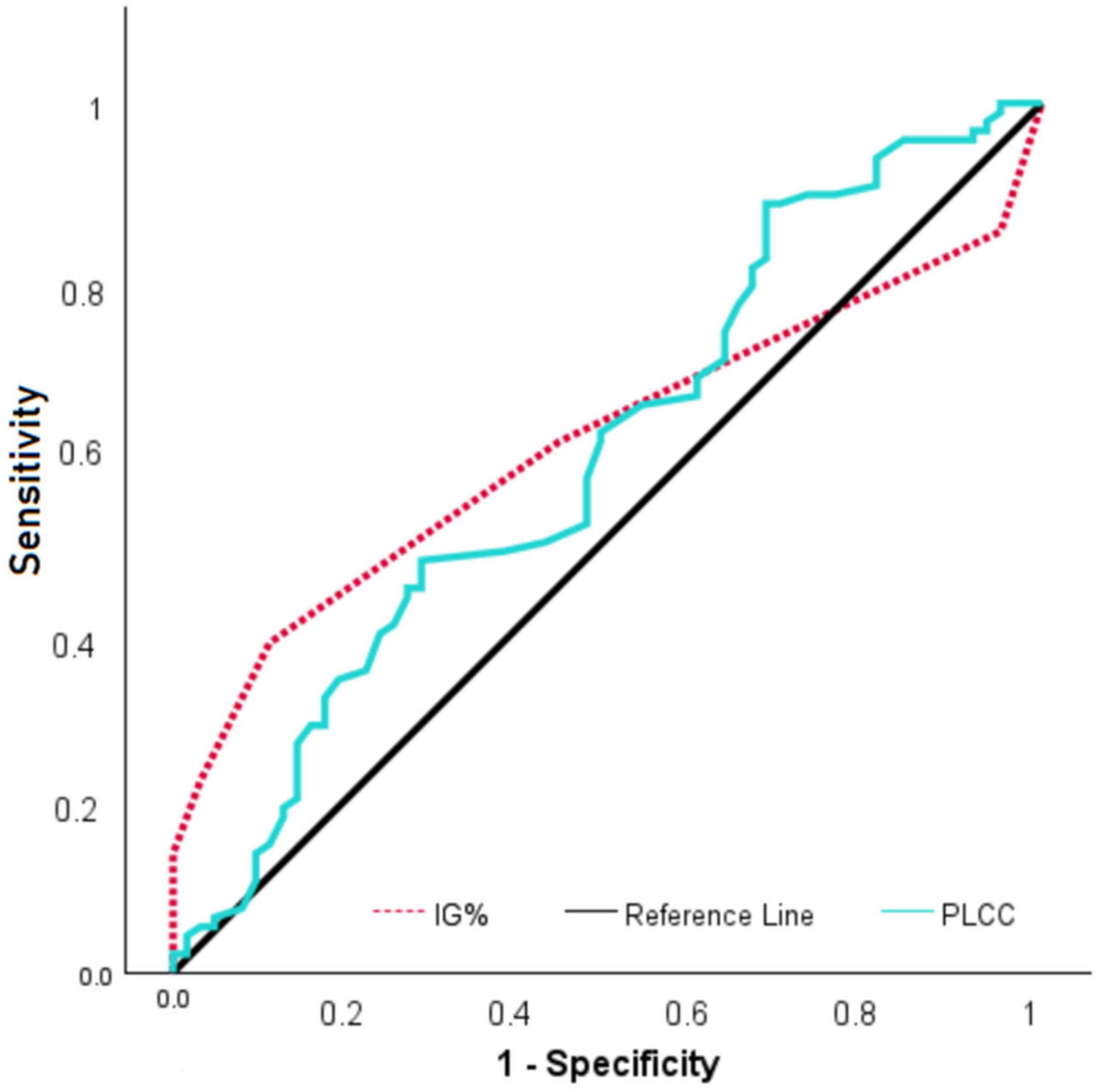
| IG% | 0.2 (0–1.1) | 0.1 (0–0.4) | 0.015 | <0.001 |
| IG# (×103/μL) | 0.01 (0–0.09) | 0.01 (0–0.03) | 0.241 | 0.006 |
| Albumin (g/L) | 44.7 ± 2.5 | 45.3 ± 2.4 | 0.169 | 0.348 |
| WBC (×103/μL) | 6.67 ± 1.46 | 7.17 ± 1.71 | 0.05 | 0.097 |
| NEU (×103/μL) | 3.91 ± 1.09 | 4.39 ± 1.32 | 0.012 | 0.029 |
| BA (×103/μL) | 0.03 (0.01–0.15) | 0.03 (0.01–0.08) | 0.695 | 0.988 |
| EO (×103/μL) | 0.14 (0–0.53) | 0.11 (0.01–0.53) | 0.355 | 0.519 |
| LYM (×103/μL) | 2.15 ± 0.63 | 2.15 ± 0.58 | 1.000 | 0.877 |
| MON (×103/μL) | 0.39 (0.23–3.43) | 0.44 (0.18–0.74) | 0.176 | 0.997 |
| RBC (×103/μL) | 4.51 (3.55–6.13) | 4.38 (3.76–5.2) | 0.125 | 0.274 |
| HGB (g/dL) | 13.26 ± 1.13 | 13.03 ± 0.96 | 0.185 | 0.341 |
| HCT (%) | 39.44 ± 3.14 | 38.83 ± 2.65 | 0.202 | 0.418 |
| MCV (fL) | 87.92 ± 4.33 | 88.21 ± 4.92 | 0.692 | 0.519 |
| MCH (pg) | 29.54 ± 1.69 | 29.59 ± 1.9 | 0.861 | 0.755 |
| MCHC (g/dL) | 33.59 ± 0.79 | 33.54 ± 0.79 | 0.702 | 0.533 |
| PLT (×103/μL) | 278.37 ± 66.23 | 277.03 ± 71.95 | 0.905 | 0.94 |
| MPV (fL) | 10.45 ± 1.29 | 10.89 ± 1.22 | 0.035 | 0.105 |
| PDW (%) | 16 (10.4–16.9) | 16 (15.5–16.8) | 0.989 | 0.431 |
| PCT (%) | 0.29 ± 0.06 | 0.3 ± 0.07 | 0.244 | 0.269 |
| NLR | 1.83 (0.71–4.35) | 2 (0.95–4.86) | 0.039 | 0.054 |
| BMI (kg/m2) | 26.95 (20.57–40.26) | 25.59 (19.72–48) | 0.276 | 0.688 |
| PLR | 136.44 ± 40.43 | 134.72 ± 41.98 | 0.797 | 0.931 |
| PLCC (×103/μL) | 77.13 ± 19.14 | 85.84 ± 24.96 | 0.014 | 0.032 |
| PLCR (%) | 29.04 ± 9.14 | 31.86 ± 8.43 | 0.038 | 0.077 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Topaloğlu, M.S.; Arpa, M.; Şen, B.; Bilgin Topaloğlu, H.; Cüre, O. The Role of Immature Granulocytes in Fibromyalgia: An Indicator of Subclinical Inflammation? Biomedicines 2025, 13, 2511. https://doi.org/10.3390/biomedicines13102511
Topaloğlu MS, Arpa M, Şen B, Bilgin Topaloğlu H, Cüre O. The Role of Immature Granulocytes in Fibromyalgia: An Indicator of Subclinical Inflammation? Biomedicines. 2025; 13(10):2511. https://doi.org/10.3390/biomedicines13102511
Chicago/Turabian StyleTopaloğlu, Mehmet Serhat, Medeni Arpa, Bayram Şen, Hacer Bilgin Topaloğlu, and Osman Cüre. 2025. "The Role of Immature Granulocytes in Fibromyalgia: An Indicator of Subclinical Inflammation?" Biomedicines 13, no. 10: 2511. https://doi.org/10.3390/biomedicines13102511
APA StyleTopaloğlu, M. S., Arpa, M., Şen, B., Bilgin Topaloğlu, H., & Cüre, O. (2025). The Role of Immature Granulocytes in Fibromyalgia: An Indicator of Subclinical Inflammation? Biomedicines, 13(10), 2511. https://doi.org/10.3390/biomedicines13102511






