Molecular Hydrogen Protects against Various Tissue Injuries from Side Effects of Anticancer Drugs by Reducing Oxidative Stress and Inflammation
Abstract
1. Introduction
2. Methodology
3. Pharmacological Effects and Side Effects of Anticancer Drugs
3.1. CIS and OXA
3.2. DXR
3.3. BLM
3.4. GEF
4. Development of Therapies and Therapeutic Substances for the Side Effects of Anticancer Drugs
4.1. Nephrotoxicity of CIS
4.2. Cardiotoxicity of DXR
5. Reduction in Side Effects of Anticancer Drugs by H2
5.1. Effects on CIS- and OXA-Induced Toxicity
5.1.1. Nephrotoxicity
5.1.2. Ototoxicity
5.1.3. Ovarian Injury
5.1.4. Peripheral Neuropathy
5.2. Effects on DXR-Induced Cardiotoxicity and Hepatotoxicity
5.3. Effects on BLM-Induced Lung Injury
5.4. Effects on GEF-Induced Lung Injury
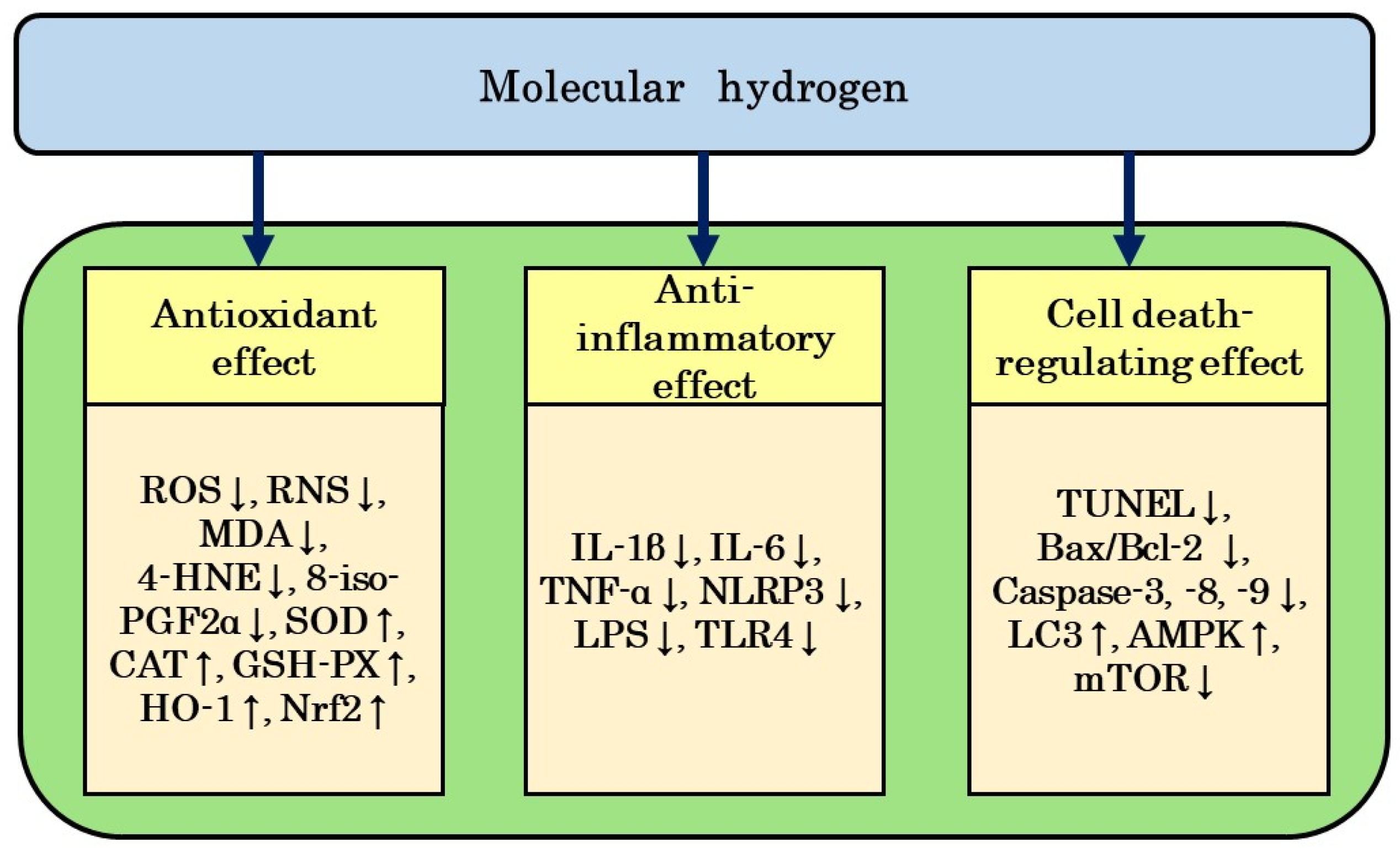
6. Mechanisms by Which H2 Reduces Side Effects of Anticancer Drugs
6.1. Antioxidant Effects
6.2. Anti-Inflammatory Effects
6.3. Regulation of Cell Death
7. Anticancer and Radioprotective Effects of H2
7.1. Anticancer Effects
7.2. Radioprotective Effects
8. Prospects for the Clinical Application of H2
9. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Global Cancer Burden Growing, Amidst Mounting Need for Services. Available online: https://www.who.int/news/item/01-02-2024-global-cancer-burden-growing--amidst-mounting-need-for-services (accessed on 28 February 2024).
- Papaioannou, D.; Rafia, R.; Stevenson, M.D.; Stevens, J.W.; Evans, P. Trabectedin for the treatment of relapsed ovarian cancer. Health Technol. Assess 2011, 15 (Suppl. S1), 69–75. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.T.; Tan, Y.J.; Oon, C.E. Molecular targeted therapy: With specificity. Eur. J. Pharmacol. 2018, 834, 188–196. [Google Scholar] [CrossRef] [PubMed]
- Shim, M.; Bang, W.J.; Oh, C.Y.; Lee, Y.S.; Cho, J.S. Effectiveness of three different luteinizing hormone-releasing hormone agonists in the chemical castration of patients with prostate cancer: Goserelin versus triptorelin versus leuprolide. Investig. Clin. Urol. 2019, 60, 244–250. [Google Scholar] [CrossRef] [PubMed]
- Kharb, R.; Haider, K.; Neha, K.; Yar, M.S. Aromatase inhibitors: Role in postmenopausal breast cancer. Arch. Pharm. 2020, 353, e2000081. [Google Scholar] [CrossRef] [PubMed]
- Xu, C.; Chen, Y.-P.; Du, X.-J.; Liu, J.-Q.; Huang, C.-L.; Chen, L.; Zhou, G.-Q.; Li, W.-F.; Mao, Y.-P.; Hsu, C.; et al. Comparative safety of immune checkpoint inhibitors in cancer: Systematic review and network meta-analysis. BMJ 2018, 363, k4226. [Google Scholar] [CrossRef] [PubMed]
- Shah, V.; Panchal, V.; Shah, A.; Vyas, B.; Agrawal, S.; Bharadwaj, S. Immune checkpoint inhibitors in metastatic melanoma therapy (Review). Med. Int. 2024, 4, 13. [Google Scholar] [CrossRef] [PubMed]
- Kumar, M.; Dubey, R.; Kumar Shukla, P.; Dayal, D.; Kumar Chaubey, K.; Tsai, L.W.; Kumar, S. Identification of small molecule inhibitors of RAD52 for breast cancer therapy: In silico approach. J. Biomol. Struct. Dyn. 2024, 42, 4605–4618. [Google Scholar] [CrossRef]
- Waseem, M.; Wang, B.-D. Combination of miR-99b-5p and enzalutamide or abiraterone synergizes the suppression of EMT-mediated metastasis in prostate cancer. Cancers 2024, 16, 1933. [Google Scholar] [CrossRef]
- Karn, V.; Ahmed, S.; Tsai, L.W.; Dubey, R.; Ojha, S.; Singh, H.N.; Kumar, M.; Gupta, P.K.; Sadhu, S.; Jha, N.K.; et al. Extracellular vesicle-based therapy for COVID-19: Promises, challenges and future prospects. Biomedicines 2021, 9, 1373. [Google Scholar] [CrossRef]
- Vasan, N.; Baselga, J.; Hyman, D.M. A view on drug resistance in cancer. Nature 2019, 575, 299–309. [Google Scholar] [CrossRef]
- Imbaby, S.; Ewais, M.; Essawy, S.; Farag, N. Cardioprotective effects of curcumin and nebivolol against doxorubicin-induced cardiac toxicity in rats. Hum. Exp. Toxicol. 2014, 33, 800–813. [Google Scholar] [CrossRef] [PubMed]
- Manavi, M.A.; Fathian Nasab, M.H.; Mohammad Jafari, R.; Dehpour, A.R. Mechanisms underlying dose-limiting toxicities of conventional chemotherapeutic agents. J. Chemother. 2024, 5, 1–31. [Google Scholar] [CrossRef] [PubMed]
- Rossi, A.; Di Maio, M.; Chiodini, P.; Rudd, R.M.; Okamoto, H.; Skarlos, D.V.; Früh, M.; Qian, W.; Tamura, T.; Samantas, E.; et al. Carboplatin- or cisplatin-based chemotherapy in first-line treatment of small-cell lung cancer: The COCIS meta-analysis of individual patient data. J. Clin. Oncol. 2012, 30, 1692–1698. [Google Scholar] [CrossRef] [PubMed]
- Hirano, S.; Wakazono, K.; Agata, N.; Iguchi, H.; Tone, H. Comparison of cardiotoxicity of pirarubicin, epirubicin and doxorubicin in the rat. Drugs Exptl. Res. 1994, 20, 153–160. [Google Scholar]
- Hirano, S.; Agata, N.; Iguchi, H.; Tone, H. Effects of pirarubicin in comparison with epirubicin and doxorubicin on the contractile function in rat isolated cardiac muscles. Gen. Pharmacol. 1995, 26, 1339–1347. [Google Scholar] [CrossRef] [PubMed]
- Li, X.-R.; Cheng, X.-H.; Zhang, G.-N.; Wang, H.-H.; Huang, J.-M. Cardiac safety analysis of first-line chemotherapy drug pegylated liposomal doxorubicin in ovarian cancer. J. Ovarian. Res. 2022, 15, 96–103. [Google Scholar] [CrossRef] [PubMed]
- Fang, C.-Y.; Lou, D.-Y.; Zhou, L.-Q.; Wang, J.-C.; Yang, B.; He, Q.-J.; Wang, J.-J.; Weng, Q.-J. Natural products: Potential treatments for cisplatin-induced nephrotoxicity. Acta. Pharmacol. Sin. 2021, 42, 1951–1969. [Google Scholar] [CrossRef] [PubMed]
- Al-Hussaniy, H.A.; Alburghaif, A.H.; Alkhafaje, Z.; Al-Zobaidy, M.A.J.; Alkuraishy, H.M.; Mostafa-Hedeab, G.; Azam, F.; Al-Samydai, A.M.; Al-Tameemi, Z.S.; Naji, M.A. Chemotherapy-induced cardiotoxicity: A new perspective on the role of digoxin, ATG7 activators, resveratrol, and herbal drugs. J. Med. Life 2023, 16, 491–500. [Google Scholar] [CrossRef] [PubMed]
- Ohsawa, I.; Ishikawa, M.; Takahashi, K.; Watanabe, M.; Nishimaki, K.; Yamagata, K.; Katsura, K.-I.; Katayama, Y.; Asoh, S.; Ohta, S. Hydrogen acts as a therapeutic antioxidant by selectively reducing cytotoxic oxygen radicals. Nat. Med. 2007, 13, 688–694. [Google Scholar] [CrossRef]
- Artamonov, M.Y.; Martusevich, A.K.; Pyatakovich, F.A.; Minenko, I.A.; Dlin, S.V.; LeBaron, T.W. Molecular hydrogen: From molecular effects to stem cells management and tissue regeneration. Antioxidants 2023, 12, 636. [Google Scholar] [CrossRef]
- Jin, Z.; Zhao, P.; Gong, W.; Ding, W.; He, Q. Fe-porphyrin: A redox-related biosensor of hydrogen molecule. Nano Res. 2023, 16, 2020–2025. [Google Scholar] [CrossRef]
- Nogueira, J.E.; Passaglia, P.; Mota, C.M.D.; Santos, B.M.; Batalhão, M.E.; Carnio, E.C.; Branco, L.G.S. Molecular hydrogen reduces acute exercise-induced inflammatory and oxidative stress status. Free Radic. Biol. Med. 2018, 129, 186–193. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Wang, L.; Zhang, Y.; Zhao, Y.; Chen, G. Hydrogen gas inhibits lung cancer progression through targeting SMC3. Biomed. Pharmacother. 2018, 104, 788–797. [Google Scholar] [CrossRef]
- Hirano, S.-I.; Ichikawa, Y.; Sato, B.; Yamamoto, H.; Takefuji, Y.; Satoh, F. Molecular hydrogen as a potential clinically applicable radioprotective agent. Int. J. Mol. Sci. 2021, 22, 4566. [Google Scholar] [CrossRef]
- Kawamura, T.; Wakabayashi, N.; Shigemura, N.; Huang, C.-S.; Masutani, K.; Tanaka, Y.; Noda, K.; Peng, X.; Takahashi, T.; Billiar, T.R.; et al. Hydrogen gas reduces hyperoxic lung injury via the Nrf2 pathway in vivo. Am. J. Physiol. Lung. Cell. Mol. Physiol. 2013, 304, L646–L656. [Google Scholar] [CrossRef]
- Hirano, S.-I.; Yamamoto, H.; Ichikawa, Y.; Sato, B.; Takefuji, Y.; Satoh, F. Molecular hydrogen as a novel antitumor agent: Possible mechanisms underlying gene expression. Int. J. Mol. Sci. 2021, 22, 8724. [Google Scholar] [CrossRef]
- Runtuwene, J.; Amitani, H.; Amitani, M.; Asakawa, A.; Cheng, K.-C.; Inui, A. Hydrogen-water enhances 5-fluorouracil-induced inhibition of colon cancer. PeerJ 2015, 3, e859. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Liu, P.Y.; Bao, W.; Chen, S.J.; Wu, F.S.; Zhu, P.Y. Hydrogen inhibits endometrial cancer growth via a ROS/NLRP3/caspase-1/GSDMD-mediated pyroptotic pathway. BMC Cancer 2020, 20, 28. [Google Scholar] [CrossRef]
- Chen, J.-B.; Kong, X.-F.; Lv, Y.-Y.; Qin, S.-C.; Sun, X.-J.; Mu, F.; Lu, T.-Y.; Xu, K.-C. “Real world survey” of hydrogen-controlled cancer: A follow-up report of 82 advanced cancer patients. Med. Gas Res. 2019, 9, 115–121. [Google Scholar]
- Nakashima-Kamimura, N.; Mori, T.; Ohsawa, I.; Asoh, S.; Ohta, S. Molecular hydrogen alleviates nephrotoxicity induced by an anti-cancer drug cisplatin without compromising anti-tumor activity in mice. Cancer Chemother. Pharmacol. 2009, 64, 753–761. [Google Scholar] [CrossRef]
- Kitamura, A.; Kobayashi, S.; Matsushita, T.; Fujinawa, H.; Murase, K. Experimental verification of protective effect of hydrogen-rich water against cisplatin-induced nephrotoxicity in rats using dynamic contrast-enhanced CT. Br. J. Radiol. 2010, 83, 509–514. [Google Scholar] [CrossRef] [PubMed]
- Matsushita, T.; Kusakabe, Y.; Kitamura, A.; Okada, S.; Murase, K. Investigation of protective effect of hydrogen-rich water against cisplatin-induced nephrotoxicity in rats using blood oxygenation level-dependent magnetic resonance imaging. Jpn. J. Radiol. 2011, 29, 503–512. [Google Scholar] [CrossRef] [PubMed]
- Qu, J.; Li, X.; Wang, J.; Mi, W.; Xie, K.; Qiu, J. Inhalation of hydrogen gas attenuates cisplatin-induced ototoxicity via reducing oxidative stress. Int. J. Pediatr. Otorhinolaryngol. 2012, 76, 111–115. [Google Scholar] [CrossRef] [PubMed]
- Kikkawa, Y.S.; Nakagawa, T.; Taniguchi, M.; Ito, J. Hydrogen protects auditory hair cells from cisplatin-induced free radicals. Neurosci. Lett. 2014, 579, 125–129. [Google Scholar] [CrossRef]
- Fransson, A.E.; Kisiel, M.; Pirttilä, K.; Pettersson, C.; Videhult Pierre, P.; Laurell, G.F.E. Hydrogen inhalation protects against ototoxicity induced by intravenous cisplatin in the guinea pig. Front. Cell. Neurosci. 2017, 11, 280. [Google Scholar] [CrossRef] [PubMed]
- Meng, X.; Chen, H.; Wang, G.; Yu, Y.; Xie, K. Hydrogen-rich saline attenuates chemotherapy-induced ovarian injury via regulation of oxidative stress. Exp. Ther. Med. 2015, 10, 2277–2282. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Martel, I.; Pol, O. A Novel Therapy for Cisplatin-Induced Allodynia and Dysfunctional and Emotional Impairments in Male and Female Mice. Antioxidants 2023, 12, 2063. [Google Scholar] [CrossRef]
- Lian, N.; Shen, M.; Zhang, K.; Pan, J.; Jiang, Y.; Yu, Y.; Yu, Y. Drinking hydrogen-rich water alleviates chemotherapy-induced neuropathic pain through the regulation of gut microbiota. J. Pain Res. 2021, 14, 681–691. [Google Scholar] [CrossRef]
- Gao, Y.; Yang, H.; Fan, Y.; Li, L.; Fang, J.; Yang, W. Hydrogen-rich saline attenuates cardiac and hepatic injury in doxorubicin rat model by inhibiting inflammation and apoptosis. Mediat. Inflamm. 2016, 2016, 1320365. [Google Scholar] [CrossRef] [PubMed]
- Ma, T.; Yang, L.; Zhang, B.; Lv, X.; Gong, F.; Yang, W. Hydrogen inhalation enhances autophagy via the AMPK/mTOR pathway, thereby attenuating doxorubicin-induced cardiac injury. Int. Immunopharmacol. 2023, 119, 110071. [Google Scholar] [CrossRef]
- Gao, L.; Jiang, D.; Geng, J.; Dong, R.; Dai, H. Hydrogen inhalation attenuated bleomycin-induced pulmonary fibrosis by inhibiting transforming growth factor-β1 and relevant oxidative stress and epithelial-to-mesenchymal transition. Exp. Physiol. 2019, 104, 1942–1951. [Google Scholar] [CrossRef] [PubMed]
- Aokage, T.; Seya, M.; Hirayama, T.; Nojima, T.; Iketani, M.; Ishikawa, M.; Terasaki, Y.; Taniguchi, A.; Miyahara, N.; Nakao, A.; et al. The effects of inhaling hydrogen gas on macrophage polarization, fibrosis, and lung function in mice with bleomycin-induced lung injury. BMC Pulm. Med. 2021, 21, 339. [Google Scholar] [CrossRef] [PubMed]
- Terasaki, Y.; Suzuki, T.; Tonaki, K.; Terasaki, M.; Kuwahara, N.; Ohsiro, J.; Iketani, M.; Takahashi, M.; Hamanoue, M.; Kajimoto, Y.; et al. Molecular hydrogen attenuates gefitinib-induced exacerbation of naphthalene-evoked acute lung injury through a reduction in oxidative stress and inflammation. Lab. Investig. 2019, 99, 793–806. [Google Scholar] [CrossRef] [PubMed]
- Akagi, J.; Baba, H. Hydrogen gas activates coenzyme Q10 to restore exhausted CD8+ T cells, especially PD-1+Tim3+terminal CD8+ T cells, leading to better nivolumab outcomes in patients with lung cancer. Oncol. Lett. 2020, 20, 258. [Google Scholar] [CrossRef]
- Chen, J.-B.; Kong, X.-F.; Mu, F.; Lu, T.-Y.; Lu, Y.-Y.; Xu, K.-C. Hydrogen therapy can be used to control tumor progression and alleviate the adverse events of medications in patients with advanced non-small cell lung cancer. Med. Gas Res. 2020, 10, 75–80. [Google Scholar] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. J. Clin. Epidemiol. 2021, 372, n71. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Moher, D. Updating guidance for reporting systematic reviews: Development of the PRISMA 2020 statement. J. Clin. Epidemiol. 2021, 134, 103–112. [Google Scholar] [CrossRef]
- Yonezawa, A.; Inui, K. Organic cation transporter OCT/SLC22A and H+/organic cation antiporter MATE/SLC47A are key molecules for nephrotoxicity of platinum agents. Biochem. Pharmacol. 2011, 81, 563–568. [Google Scholar] [CrossRef]
- Lebwohl, D.; Canetta, R. Clinical development of platinum complexes in cancer therapy: An historical perspective and an update. Eur. J. Cancer 1998, 34, 1522–1534. [Google Scholar] [CrossRef]
- Wolfgang, G.H.I.; Dominick, M.A.; Walsh, K.; Hoeschele, J.D.; Pegg, D.G. Comparative nephrotoxicity of a novel platinum compound, cisplatin, and carboplatin in male Wistar rats. Toxicol. Sci. 1994, 22, 73–79. [Google Scholar] [CrossRef]
- Bagheri, M.; Zandieh, M.A.; Daryab, M.; Samaei, S.S.; Gholami, S.; Rahmanian, P.; Dezfulian, S.; Eary, M.; Rezaee, A.; Rajabi, R.; et al. Nanostructures for site-specific delivery of oxaliplatin cancer therapy: Versatile nanoplatforms in synergistic cancer therapy. Transl. Oncol. 2024, 39, 101838. [Google Scholar] [CrossRef]
- Smith, L.; Cornelius, V.R.; Plummer, C.J.; Levitt, G.; Verrill, M.; Canney, P.; Jones, A. Cardiotoxicity of anthracycline agents for the treatment of cancer: Systematic review and meta-analysis of randomised controlled trials. BMC Cancer 2010, 10, 337. [Google Scholar] [CrossRef]
- Tewey, K.M.; Rowe, T.C.; Yang, L.; Halligan, B.D.; Liu, L.F. Adriamycin-induced DNA damage mediated by mammalian DNA topoisomerase II. Science 1984, 226, 466–468. [Google Scholar] [CrossRef]
- Cardinale, D.; Colombo, A.; Bacchiani, G.; Tedeschi, I.; Meroni, C.A.; Veglia, F.; Civelli, M.; Lamantia, G.; Colombo, N.; Curigliano, G.; et al. Early detection of anthracycline cardiotoxicity and improvement with heart failure therapy. Circulation 2015, 131, 1981–1988. [Google Scholar] [CrossRef]
- Keizer, H.G.; Pinedo, H.M.; Schuurhuis, G.J.; Joenje, H. Doxorubicin (adriamycin): A critical review of free radical-dependent mechanisms of cytotoxicity. Pharmacol. Ther. 1990, 47, 219–231. [Google Scholar] [CrossRef] [PubMed]
- Link, G.; Tirosh, R.; Pinson, A.; Hershko, C. Role of iron in the potentiation of anthracycline cardiotoxicity: Identification of heart cell mitochondria as a major site of iron-anthracycline interaction. J. Lab. Clin. Med. 1996, 127, 272–278. [Google Scholar] [CrossRef]
- Capranico, G.; Tinelli, S.; Austin, C.A.; Fisher, M.L.; Zunino, F. Different patterns of gene expression of topoisomerase II isoforms in differentiated tissues during murine development. Biochim. Biophys. Acta (BBA) Gene Struct. Expr. 1992, 1132, 43–48. [Google Scholar] [CrossRef]
- Chahvar, S.T.; Al-Shawaf, T.; Tranquilli, A.L. Pharmacologic ovarian preservation in young women undergoing chemotherapy. Curr. Med. Chem. 2014, 21, 223–229. [Google Scholar] [CrossRef] [PubMed]
- Rashid, R.; Langfinger, D.; Wagner, R.; Schuchmann, H.P.; von Sonntag, C. Bleomycin versus OH-radical-induced malonaldehydic-product formation in DNA. Int. J. Radiat. Biol. 1999, 75, 101–109. [Google Scholar] [CrossRef] [PubMed]
- Della Latta, V.; Cecchettini, A.; Del Ry, S.; Morales, M.A. Bleomycin in the setting of lung fibrosis induction: From biological mechanisms to counteractions. Pharmacol. Res. 2015, 97, 122–130. [Google Scholar] [CrossRef]
- Kuwano, K.; Kunitake, R.; Maeyama, T.; Hagimoto, N.; Kawasaki, M.; Matsuba, T.; Yoshimi, M.; Inoshima, I.; Yoshida, K.; Hara, N. Attenuation of bleomycin-induced pneumopathy in mice by a caspase inhibitor. Am. J. Physiol. Lung Cell Mol. Physiol. 2001, 280, L316–L325. [Google Scholar] [CrossRef] [PubMed]
- Hoyt, D.G.; Lazo, J.S. Alterations in pulmonary mRNA encoding procollagens, fibronectin and transforming growth factor-beta precede bleomycin-induced pulmonary fibrosis in mice. J. Pharmacol. Exp. Ther. 1988, 246, 765–771. [Google Scholar] [PubMed]
- Cooper, J.A., Jr. Pulmonary fibrosis: Pathways are slowly coming into light. Am. J. Respir. Cell Mol. Biol. 2000, 22, 520–523. [Google Scholar] [CrossRef] [PubMed]
- Oh, H.-N.; Lee, M.-H.; Kim, E.; Kwak, A.-W.; Yoon, G.; Cho, S.-S.; Liu, K.; Chae, J.-I.; Shim, J.-H. Licochalcone D induces ROS-dependent apoptosis in gefitinib-sensitive or resistant lung cancer cells by targeting EGFR and MET. Biomolecules 2020, 10, 297. [Google Scholar] [CrossRef]
- Li, L.; Huang, W.; Li, K.; Zhang, K.; Lin, C.; Han, R.; Lu, C.; Wang, Y.; Chen, H.; Sun, F.; et al. Metformin attenuates gefitinib-induced exacerbation of pulmonary fibrosis by inhibition of TGF-β signaling pathway. Oncotarget 2015, 6, 43605–43619. [Google Scholar] [CrossRef]
- Noguchi, T.; Sekiguchi, Y.; Kudoh, Y.; Naganuma, R.; Kagi, T.; Nishidate, A.; Maeda, K.; Ishii, C.; Toyama, T.; Hirata, Y.; et al. Gefitinib initiates sterile inflammation by promoting IL-1β and HMGB1 release via two distinct mechanisms. Cell Death Dis. 2021, 12, 49. [Google Scholar] [CrossRef]
- Hutchison, F.N.; Perez, E.A.; Gandara, D.R.; Lawrence, H.J.; Kaysen, G.A. Renal salt wasting in patients treated with cisplatin. Ann. Intern. Med. 1988, 108, 21–25. [Google Scholar] [CrossRef] [PubMed]
- Crona, D.J.; Faso, A.; Nishijima, T.F.; McGraw, K.A.; Galsky, M.D.; Milowsky, M.I. A Systematic review of strategies to prevent cisplatin-induced nephrotoxicity. Oncologist 2017, 22, 609–619. [Google Scholar] [CrossRef]
- Naziroglu, M.; Karaoğlu, A.; Aksoy, A.O. Selenium and high dose vitamin E administration protects cisplatin-induced oxidative damage to renal, liver and lens tissues in rats. Toxicology 2004, 195, 221–230. [Google Scholar] [CrossRef]
- Giri, A.; Khynriam, D.; Prasad, S.B. Vitamin C mediated protection on cisplatin induced mutagenicity in mice. Mutat. Res./Fundam. Mol. Mech. Mutagen. 1998, 421, 139–148. [Google Scholar] [CrossRef]
- Baldew, G.S.; van den Hamer, C.J.; Los, G.; Vermeulen, N.P.; de Goeij, J.J.; McVie, J.G. Selenium-induced protection against cis-diamminedichloroplatinum(II) nephrotoxicity in mice and rats. Cancer Res. 1989, 49, 3020–3023. [Google Scholar] [PubMed]
- Atessahin, A.; Yilmaz, S.; Karahan, I.; Ceribasi, A.O.; Karaoglu, A. Effects of lycopene against cisplatin-induced nephrotoxicity and oxidative stress in rats. Toxicology 2005, 212, 116–123. [Google Scholar] [CrossRef] [PubMed]
- Sener, G.; Satiroglu, H.; Kabasakal, L.; Arbak, S.; Oner, S.; Ercan, F.; Keyer-Uysa, M. The protective effect of melatonin on cisplatin nephrotoxicity. Fundam. Clin. Pharmacol. 2000, 14, 553–560. [Google Scholar] [CrossRef] [PubMed]
- Nisar, S.; Feinfeld, D.A. N-acetylcysteine as salvage therapy in cisplatin nephrotoxicity. Ren. Fail. 2002, 24, 529–533. [Google Scholar] [CrossRef] [PubMed]
- Dickey, D.T.; Muldoon, L.L.; Doolittle, N.D.; Peterson, D.R.; Kraemer, D.F.; Neuwelt, E.A. Effect of N-acetylcysteine route of administration on chemoprotection against cisplatin-induced toxicity in rat models. Cancer Chemother. Pharmacol. 2008, 62, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Katsuda, H.; Yamashita, M.; Katsura, H.; Yu, J.; Waki, Y.; Nagata, N.; Sai, Y.; Miyamoto, K. Protecting cisplatin-induced nephrotoxicity with cimetidine does not affect antitumor activity. Biol. Pharm. Bull. 2010, 33, 1867–1871. [Google Scholar] [CrossRef] [PubMed]
- Carvalho Rodrigues, M.A.; Gobe, G.; Santos, N.A.G.; Santos, A.C. Carvedilol protects against apoptotic cell death induced by cisplatin in renal tubular epithelial cells. J. Toxicol. Environ. Health Part A 2012, 75, 981–990. [Google Scholar] [CrossRef] [PubMed]
- Humanes, B.; Lazaro, A.; Camano, S.; Moreno-Gordaliza, E.; Lazaro, J.A.; Blanco-Codesido, M.; Lara, J.M.; Ortiz, A.; Gomez-Gomez, M.M.; Martín-Vasallo, P.; et al. Cilastatin protects against cisplatin-induced nephrotoxicity without compromising its anticancer efficiency in rats. Kidney Int. 2012, 82, 652–663. [Google Scholar] [CrossRef] [PubMed]
- Ozkaya, O.; Yavuz, O.; Can, B.; Dilek, M.; Savli, E.; Acikgoz, Y.; Bedir, A.; Akpolat, T. Effect of rosiglitazone on cisplatin-induced nephrotoxicity. Ren. Fail. 2010, 32, 368–371. [Google Scholar] [CrossRef]
- Capizzi, R.L. Amifostine reduces the incidence of cumulative nephrotoxicity from cisplatin: Laboratory and clinical aspects. Semin. Oncol. 1999, 26, 72–81. [Google Scholar]
- Tan, R.Z.; Wang, C.; Deng, C.; Zhong, X.; Yan, Y.; Luo, Y.; Lan, H.Y.; He, T.; Wang, L. Quercetin protects against cisplatin-induced acute kidney injury by inhibiting Mincle/Syk/NF-κB signaling maintained macrophage inflammation. Phytother. Res. 2020, 34, 139–152. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Dang, C.; Kang, H.; Dai, Z.; Lin, S.; Guan, H.; Liu, X.; Wang, X.; Hui, W. Saikosaponin-D reduces cisplatin-induced nephrotoxicity by repressing ROS-mediated activation of MAPK and NF-κB signalling pathways. Int. Immunopharmacol. 2015, 28, 399–408. [Google Scholar] [CrossRef] [PubMed]
- Domitrović, R.; Cvijanović, O.; Pernjak-Pugel, E.; Skoda, M.; Mikelić, L.; Crnčević-Orlić, Z. Berberine exerts nephroprotective effect against cisplatin-induced kidney damage through inhibition of oxidative/nitrosative stress, inflammation, autophagy and apoptosis. Food Chem. Toxicol. 2013, 62, 397–406. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.; Peng, H.; Dong, L.; Chen, L.; Ma, X.; Peng, Y.; Dai, S.; Liu, Q. Activation of the NRF2-ARE signalling pathway by the Lentinula edodes polysaccharose LNT alleviates ROS-mediated cisplatin nephrotoxicity. Int. Immunopharmacol. 2016, 36, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Bunel, V.; Antoine, M.-H.; Nortier, J.; Duez, P.; Stévigny, C. Protective effects of schizandrin and schizandrin B towards cisplatin nephrotoxicity in vitro. J. Appl. Toxicol. 2013, 34, 1311–1319. [Google Scholar] [CrossRef] [PubMed]
- de Baat, E.C.; Mulder, R.L.; Armenian, S.; Feijen, E.A.; Grotenhuis, H.; Hudson, M.M.; Mavinkurve-Groothuis, A.M.; Kremer, L.C.; van Dalen, E.C. Dexrazoxane for preventing or reducing cardiotoxicity in adults and children with cancer receiving anthracyclines. Cochrane Database Syst. Rev. 2022, 9, CD014638. [Google Scholar] [CrossRef] [PubMed]
- Macedo, A.V.S.; Hajjar, L.A.; Lyon, A.R.; Nascimento, B.R.; Putzu, A.; Rossi, L.; Costa, R.B.; Landoni, G.; Nogueira-Rodrigues, A.; Ribeiro, A.L.P. Efficacy of Dexrazoxane in Preventing Anthracycline Cardiotoxicity in Breast Cancer. JACC CardioOncol. 2019, 1, 68–79. [Google Scholar] [CrossRef] [PubMed]
- Mathavan, S.; Kue, C.S.; Kumar, S. Identification of potential candidate genes for lip and oral cavity cancer using network analysis. Genom. Inform. 2021, 19, e4. [Google Scholar] [CrossRef] [PubMed]
- Langer, S.W. Dexrazoxane for the treatment of chemotherapy-related side effects. Cancer Manag. Res. 2014, 6, 357–363. [Google Scholar] [CrossRef]
- Wang, Y.; Ma, Q.; Zhang, S.; Liu, H.; Zhao, B.; Du, B.; Wang, W.; Lin, P.; Zhang, Z.; Zhong, Y.; et al. Digoxin enhances the anticancer effect on non-small cell lung cancer while reducing the cardiotoxicity of adriamycin. Front. Pharmacol. 2020, 11, 186. [Google Scholar] [CrossRef]
- Wang, Y.; Lu, X.; Wang, X.; Qiu, Q.; Zhu, P.; Ma, L.; Ma, X.; Herrmann, J.; Lin, X.; Wang, W.; et al. atg7-Based Autophagy Activation Reverses Doxorubicin-Induced Cardiotoxicity. Circ. Res. 2021, 129, e166–e182. [Google Scholar] [CrossRef] [PubMed]
- Monahan, D.S.; Flaherty, E.; Hameed, A.; Duffy, G.P. Resveratrol significantly improves cell survival in comparison to dexrazoxane and carvedilol in a h9c2 model of doxorubicin induced cardiotoxicity. Biomed. Pharmacother. 2021, 140, 111702. [Google Scholar] [CrossRef] [PubMed]
- Al-kuraishy, H.M.; Al-Gareeb, A.I.; Al-hussaniy, H.A. Doxorubicin-Induced Cardiotoxicity: Molecular Mechanism and Protection by Conventional Drugs and Natural Products. Int. J. Clin. Oncol. Cancer Res. 2017, 2, 31–44. [Google Scholar]
- Tadokoro, T.; Ikeda, M.; Ide, T.; Deguchi, H.; Ikeda, S.; Okabe, K.; Ishikita, A.; Matsushima, S.; Koumura, T.; Yamada, K.-I.; et al. Mitochondria-dependent ferroptosis plays a pivotal role in doxorubicin cardiotoxicity. JCI Insight. 2020, 5, e132747. [Google Scholar] [CrossRef] [PubMed]
- Abe, K.; Ikeda, M.; Ide, T.; Tadokoro, T.; Miyamoto, H.D.; Furusawa, S.; Tsutsui, Y.; Miyake, R.; Ishimaru, K.; Watanabe, M.; et al. Doxorubicin causes ferroptosis and cardiotoxicity by intercalating into mitochondrial DNA and disrupting Alas1-dependent heme synthesis. Sci. Signal. 2022, 15, eabn8017. [Google Scholar] [CrossRef] [PubMed]
- Hirano, S.; Ichikawa, Y.; Sato, B.; Yamamoto, H.; Takefuji, Y.; Satoh, F. Potential therapeutic applications of hydrogen in chronic inflammatory diseases: Possible inhibiting role on mitochondrial stress. Int. J. Mol. Sci. 2021, 22, 2549. [Google Scholar] [CrossRef] [PubMed]
- Shao, L.; Luo, Y.; Zhou, D. Hematopoietic stem cell injury induced by ionizing radiation. Antioxid. Redox Signal. 2014, 20, 1447–1462. [Google Scholar] [CrossRef] [PubMed]
- Ward, J.F. DNA damage produced by ionizing radiation in mammalian cells: Identities, mechanisms of formation, and reparability. Prog. Nucleic Acid Res. Mol. Biol. 1988, 35, 95–125. [Google Scholar]
- Caer, S.L. Water radiolysis: Influence of oxide surfaces on H2 production under ionizing radiation. Water 2011, 3, 235–253. [Google Scholar] [CrossRef]
- Nickoloff, J.A.; Sharma, N.; Taylor, L. Clustered DNA double-strand breaks: Biological effects and relevance to cancer radiotherapy. Gene 2020, 11, 99. [Google Scholar] [CrossRef]
- Kang, K.-M.; Kang, Y.-N.; Choi, I.-B.; Gu, Y.; Kawamura, T.; Toyoda, Y.; Nakao, A. Effects of drinking hydrogen-rich water on the quality of life of patients treated with radiotherapy for liver tumors. Med. Gas Res. 2011, 1, 11. [Google Scholar] [CrossRef] [PubMed]
- Hirano, S.; Aoki, Y.; Li, X.K.; Ichimaru, N.; Takahara, S.; Takefuji, Y. Protective effects of hydrogen gas inhalation on radiationinduced bone marrow damage in cancer patients: A retrospective observational study. Med. Gas Res. 2021, 11, 104–109. [Google Scholar] [PubMed]
- Song, W.; Zhang, M.; Huang, X.; Chen, B.; Ding, Y.; Zhang, Y.; Yu, D.G.; Kim, I. Smart l-borneol-loaded hierarchical hollow polymer nanospheres with antipollution and antibacterial capabilities. Material. Today Chemist. 2022, 26, 101252. [Google Scholar] [CrossRef]
- Liao, Q.; Kim, E.J.; Tang, Y.; Xu, H.; Yu, D.-G.; Song, W.; Kim, B.J. Rational design of hyper-crosslinked polymers for biomedical applications. J. Polym. Sci. 2024, 62, 1517–1535. [Google Scholar] [CrossRef]



| Anticancer Drugs | Toxicities/Injuries | Changes in Biomarkers | Ref. No. |
|---|---|---|---|
| CIS | Nephrotoxicity | BUN ↓, Creatinine ↓, TUNEL ↓ | [31] |
| Creatinine ↓ | [32] | ||
| BUN ↓, Creatinine ↓ | [33] | ||
| CIS | Ototoxicity | MDA ↓, 8-iso-PGF2α ↓ | [34] |
| •OH ↓ | [35] | ||
| Synaptophysin ↑, Copper transporter 1 ↑ | [36] | ||
| CIS | Ovarian injury | SOD ↑, CAT ↑, MDA ↓, Nrf2 ↑ | [37] |
| CIS | Peripheral neuropathy | NLRP3 ↓, 4-HNE ↓, HO-1 ↑, SOD ↑ | [38] |
| OXA | Peripheral neuropathy | TNF-α ↓, IL-6 ↓, •OH ↓, ONOO− ↓, LPS ↓, TLR4 ↓ | [39] |
| DXR | Cardiotoxicity and hepatotoxicity | BNP ↓, AST ↓, ALT ↓, ROS ↓, MDA ↓, TNF-α ↓, IL-1β ↓, IL-6 ↓, TUNEL ↓, Bax/Bcl-2 ↓, Caspase-3 ↓, Caspase-8 ↓ | [40] |
| DXR | Cardiotoxicity | LC3 ↑, TUNEL ↓, Bax/Bcl-2 ↓, Caspase-3 ↓, Caspase-9 ↓, AMPK ↑, mTOR ↓ | [41] |
| BLM | Lung injury | ROS ↓, MDA ↓ TGF-β1 ↓,TNF-α ↓, GSH-PX ↑, E-cadherin ↑, Vimentin ↓, α-SMA ↓, Collagen I ↓ | [42] |
| IL-4 ↓, IL-6 ↓, IL-13 ↓ TGF-β1 ↓ | [43] | ||
| GEF | Lung injury | (GSH ↓, MDA ↓, 4-HNE ↓) * | [44] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hirano, S.-i.; Takefuji, Y. Molecular Hydrogen Protects against Various Tissue Injuries from Side Effects of Anticancer Drugs by Reducing Oxidative Stress and Inflammation. Biomedicines 2024, 12, 1591. https://doi.org/10.3390/biomedicines12071591
Hirano S-i, Takefuji Y. Molecular Hydrogen Protects against Various Tissue Injuries from Side Effects of Anticancer Drugs by Reducing Oxidative Stress and Inflammation. Biomedicines. 2024; 12(7):1591. https://doi.org/10.3390/biomedicines12071591
Chicago/Turabian StyleHirano, Shin-ichi, and Yoshiyasu Takefuji. 2024. "Molecular Hydrogen Protects against Various Tissue Injuries from Side Effects of Anticancer Drugs by Reducing Oxidative Stress and Inflammation" Biomedicines 12, no. 7: 1591. https://doi.org/10.3390/biomedicines12071591
APA StyleHirano, S.-i., & Takefuji, Y. (2024). Molecular Hydrogen Protects against Various Tissue Injuries from Side Effects of Anticancer Drugs by Reducing Oxidative Stress and Inflammation. Biomedicines, 12(7), 1591. https://doi.org/10.3390/biomedicines12071591







