Tacrolimus Treatment for TAFRO Syndrome
Abstract
1. Introduction
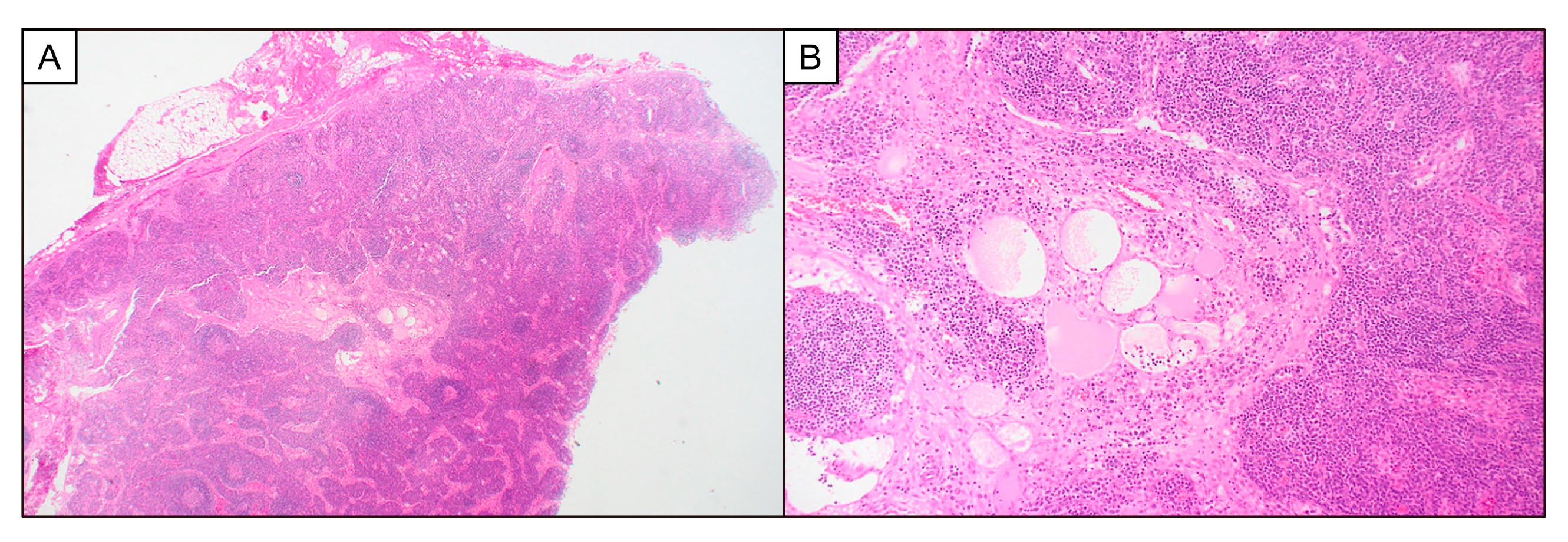
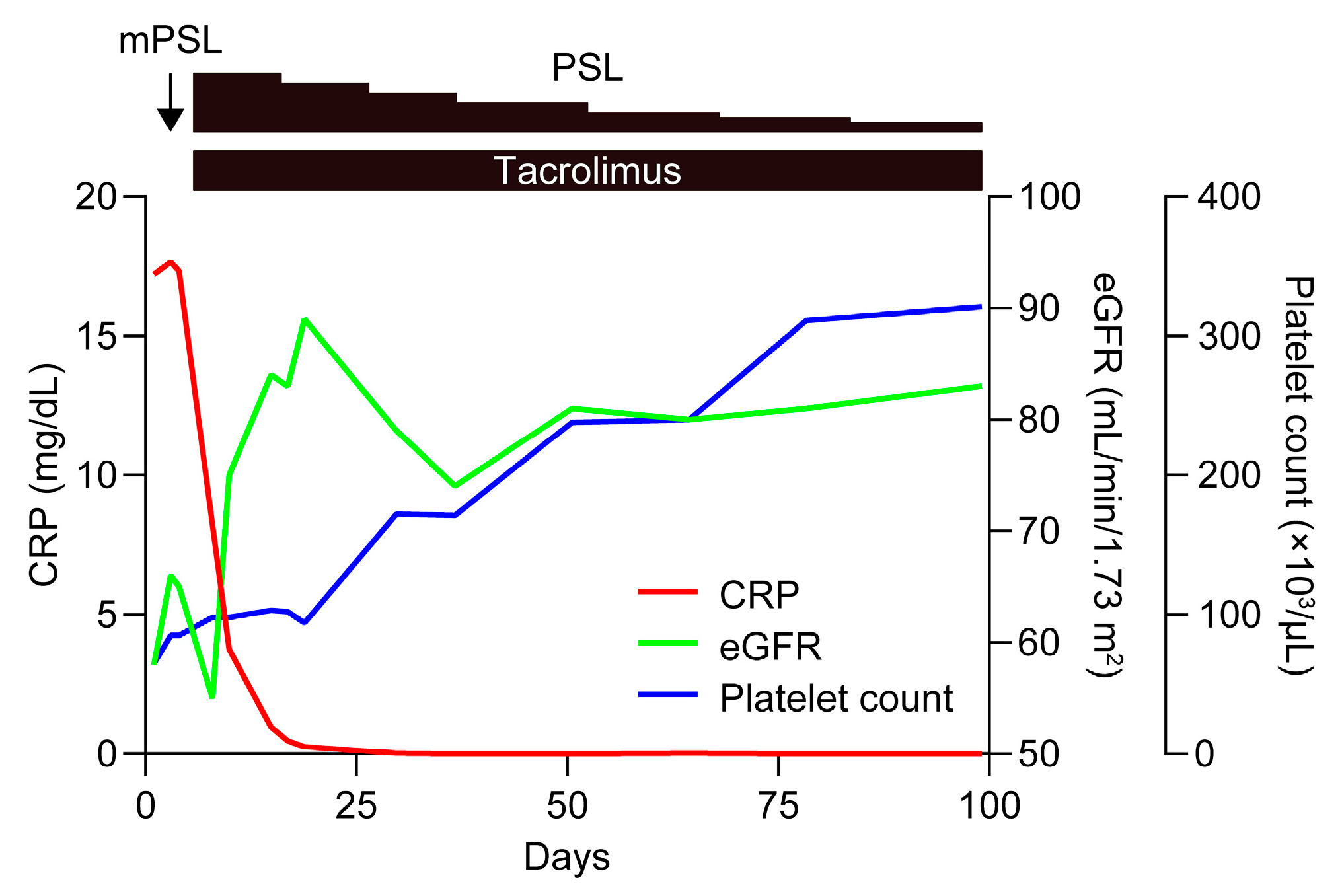
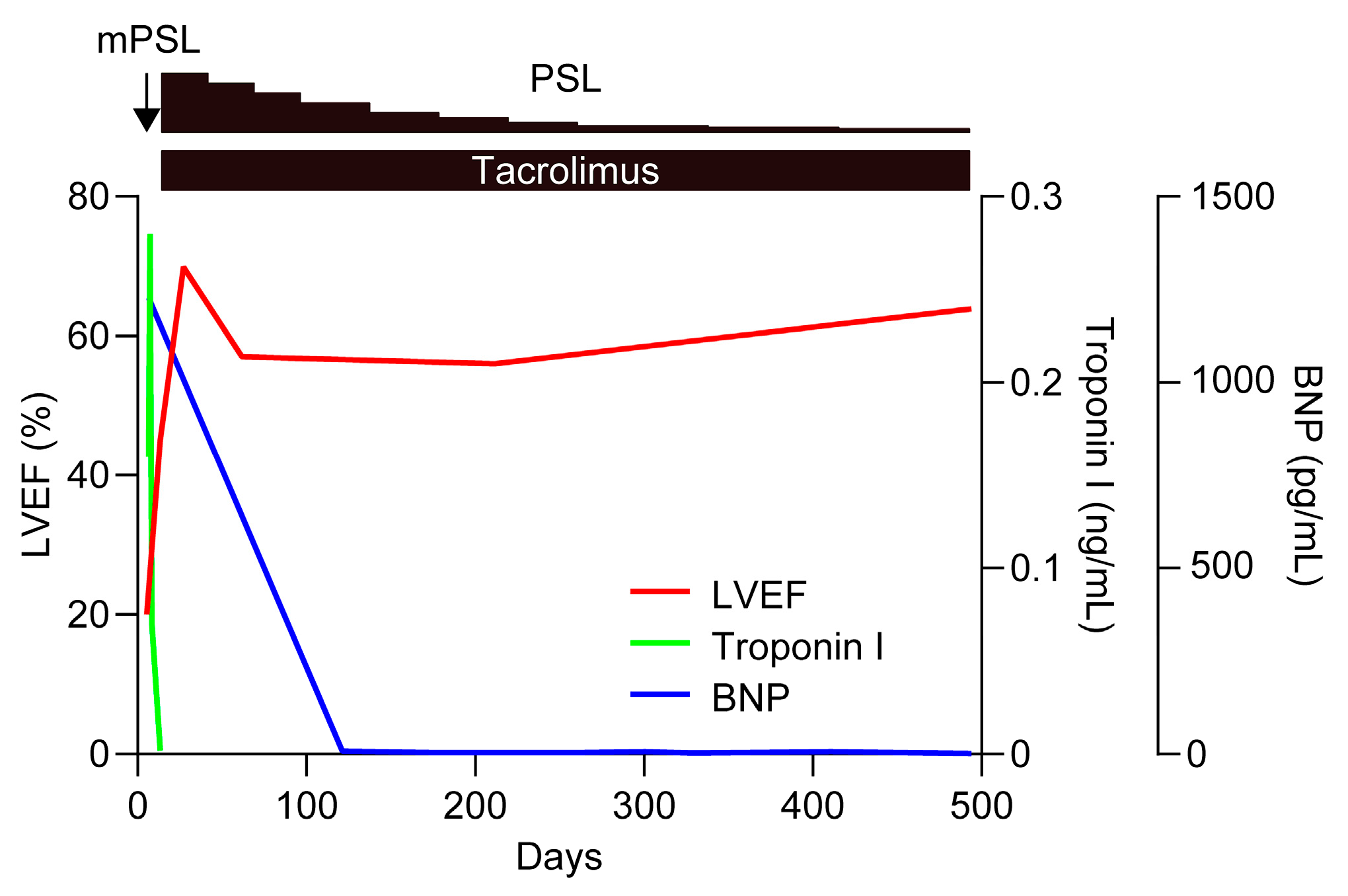
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Carbone, A.; Borok, M.; Damania, B.; Gloghini, A.; Polizzotto, M.N.; Jayanthan, R.K.; Fajgenbaum, D.C.; Bower, M. Castleman disease. Nat. Rev. Dis. Primers 2021, 7, 84. [Google Scholar] [CrossRef]
- Dispenzieri, A.; Fajgenbaum, D.C. Overview of Castleman disease. Blood 2020, 135, 1353–1364. [Google Scholar] [CrossRef] [PubMed]
- Takai, K.; Nikkuni, K.; Shibuya, H.; Hashidate, H. Thrombocytopenia with mild bone marrow fibrosis accompanied by fever, pleural effusion, ascites and hepatosplenomegaly. Rinsho Ketsueki 2010, 51, 320–325. [Google Scholar] [PubMed]
- Kawabata, H.; Takai, K.; Kojima, M.; Nakamura, N.; Aoki, S.; Nakamura, S.; Kinoshita, T.; Masaki, Y. Castleman-Kojima disease (TAFRO syndrome): A novel systemic inflammatory disease characterized by a constellation of symptoms, namely, thrombocytopenia, ascites (anasarca), microcytic anemia, myelofibrosis, renal dysfunction, and organomegaly: A status report and summary of Fukushima (6 June 2012) and Nagoya meetings (22 September 2012). J. Clin. Exp. Hematop. 2013, 53, 57–61. [Google Scholar] [PubMed]
- Masaki, Y.; Kawabata, H.; Fujimoto, S.; Kawano, M.; Iwaki, N.; Kotani, T.; Nakashima, A.; Kurose, N.; Takai, K.; Suzuki, R.; et al. Epidemiological analysis of multicentric and unicentric Castleman disease and TAFRO syndrome in Japan. J. Clin. Exp. Hematop. 2019, 59, 175–178. [Google Scholar] [CrossRef] [PubMed]
- Kurose, N.; Futatsuya, C.; Mizutani, K.-i.; Kumagai, M.; Shioya, A.; Guo, X.; Aikawa, A.; Nakada, S.; Fujimoto, S.; Kawabata, H.; et al. The clinicopathological comparison among nodal cases of idiopathic multicentric Castleman disease with and without TAFRO syndrome. Hum. Pathol. 2018, 77, 130–138. [Google Scholar] [CrossRef] [PubMed]
- Fujimoto, S.; Sakai, T.; Kawabata, H.; Kurose, N.; Yamada, S.; Takai, K.; Aoki, S.; Kuroda, J.; Ide, M.; Setoguchi, K.; et al. Is TAFRO syndrome a subtype of idiopathic multicentric Castleman disease? Am. J. Hematol. 2019, 94, 975–983. [Google Scholar] [CrossRef] [PubMed]
- Iwaki, N.; Fajgenbaum, D.C.; Nabel, C.S.; Gion, Y.; Kondo, E.; Kawano, M.; Masunari, T.; Yoshida, I.; Moro, H.; Nikkuni, K.; et al. Clinicopathologic analysis of TAFRO syndrome demonstrates a distinct subtype of HHV-8-negative multicentric Castleman disease. Am. J. Hematol. 2016, 91, 220–226. [Google Scholar] [CrossRef]
- Fajgenbaum, D.C.; van Rhee, F.; Nabel, C.S. HHV-8-negative, idiopathic multicentric Castleman disease: Novel insights into biology, pathogenesis, and therapy. Blood 2014, 123, 2924–2933. [Google Scholar] [CrossRef]
- Tanaka, T.; Narazaki, M.; Kishimoto, T. IL-6 in inflammation, immunity, and disease. Cold Spring Harb. Perspect. Biol. 2014, 6, a016295. [Google Scholar] [CrossRef]
- Casper, C.; Chaturvedi, S.; Munshi, N.; Wong, R.; Qi, M.; Schaffer, M.; Bandekar, R.; Hall, B.; van de Velde, H.; Vermeulen, J.; et al. Analysis of inflammatory and anemia-related biomarkers in a randomized, double-blind, placebo-controlled study of siltuximab (anti-il6 monoclonal antibody) in patients with multicentric Castleman disease. Clin. Cancer Res. 2015, 21, 4294–4304. [Google Scholar] [CrossRef] [PubMed]
- van Rhee, F.; Voorhees, P.; Dispenzieri, A.; Fosså, A.; Srkalovic, G.; Ide, M.; Munshi, N.; Schey, S.; Streetly, M.; Pierson, S.K.; et al. International, evidence-based consensus treatment guidelines for idiopathic multicentric Castleman disease. Blood 2018, 132, 2115–2124. [Google Scholar] [CrossRef] [PubMed]
- Fujimoto, S.; Kawabata, H.; Sakai, T.; Yanagisawa, H.; Nishikori, M.; Nara, K.; Ohara, S.; Tsukamoto, N.; Kurose, N.; Yamada, S.; et al. Optimal treatments for TAFRO syndrome: A retrospective surveillance study in Japan. Int. J. Hematol. 2021, 113, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Konishi, Y.; Takahashi, S.; Nishi, K.; Sakamaki, T.; Mitani, S.; Kaneko, H.; Mizutani, C.; Ukyo, N.; Hirata, H.; Tsudo, M. Successful treatment of TAFRO syndrome, a variant of multicentric Castleman’s disease, with cyclosporine A: Possible pathogenetic contribution of interleukin-2. Tohoku J. Exp. Med. 2015, 236, 289–295. [Google Scholar] [CrossRef] [PubMed]
- Yamaga, Y.; Tokuyama, K.; Kato, T.; Yamada, R.; Murayama, M.; Ikeda, T.; Yamakita, N.; Kunieda, T. Successful treatment with cyclosporin A in tocilizumab-resistant TAFRO syndrome. Intern. Med. 2016, 55, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Inoue, M.; Ankou, M.; Hua, J.; Iwaki, Y.; Hagihara, M.; Ota, Y. Complete resolution of TAFRO syndrome (thrombocytopenia, anasarca, fever, reticulin fibrosis and organomegaly) after immunosuppressive therapies using corticosteroids and cyclosporin A: A case report. J. Clin. Exp. Hematop. 2013, 53, 95–99. [Google Scholar] [CrossRef]
- Takasawa, N.; Sekiguchi, Y.; Takahashi, T.; Muryoi, A.; Satoh, J.; Sasaki, T. A case of TAFRO syndrome, a variant of multicentric Castleman’s disease, successfully treated with corticosteroid and cyclosporine A. Mod. Rheumatol. 2019, 29, 198–202. [Google Scholar] [CrossRef] [PubMed]
- Mukherjee, S.; Mukherjee, U. A comprehensive review of immunosuppression used for liver transplantation. J. Transplant. 2009, 2009, 701464. [Google Scholar] [CrossRef] [PubMed]
- Kitahara, K.; Kawai, S. Cyclosporine and tacrolimus for the treatment of rheumatoid arthritis. Curr. Opin. Rheumatol. 2007, 19, 238–245. [Google Scholar] [CrossRef]
- Shirai, T.; Onishi, A.; Waki, D.; Saegusa, J.; Morinobu, A. Successful treatment with tacrolimus in TAFRO syndrome: Two case reports and literature review. Medicine 2018, 97, e11045. [Google Scholar] [CrossRef]
- Masaki, Y.; Kawabata, H.; Takai, K.; Tsukamoto, N.; Fujimoto, S.; Ishigaki, Y.; Kurose, N.; Miura, K.; Nakamura, S.; Aoki, S.; et al. 2019 Updated diagnostic criteria and disease severity classification for TAFRO syndrome. Int. J. Hematol. 2020, 111, 155–158. [Google Scholar] [CrossRef] [PubMed]
- Nishimura, Y.; Fajgenbaum, D.C.; Pierson, S.K.; Iwaki, N.; Nishikori, A.; Kawano, M.; Nakamura, N.; Izutsu, K.; Takeuchi, K.; Nishimura, M.F.; et al. Validated international definition of the thrombocytopenia, anasarca, fever, reticulin fibrosis, renal insufficiency, and organomegaly clinical subtype (TAFRO) of idiopathic multicentric Castleman disease. Am. J. Hematol. 2021, 96, 1241–1252. [Google Scholar] [CrossRef]
- Henter, J.-I.; Horne, A.; Aricó, M.; Egeler, R.M.; Filipovich, A.H.; Imashuku, S.; Ladisch, S.; McClain, K.; Webb, D.; Winiarski, J.; et al. HLH-2004: Diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr. Blood Cancer 2007, 48, 124–131. [Google Scholar] [CrossRef] [PubMed]
- Fardet, L.; Galicier, L.; Lambotte, O.; Marzac, C.; Aumont, C.; Chahwan, D.; Coppo, P.; Hejblum, G. Development and validation of the HScore, a score for the diagnosis of reactive hemophagocytic syndrome. Arthritis Rheumatol. 2014, 66, 2613–2620. [Google Scholar] [CrossRef] [PubMed]
- Masaki, Y.; Kawabata, H.; Takai, K.; Kojima, M.; Tsukamoto, N.; Ishigaki, Y.; Kurose, N.; Ide, M.; Murakami, J.; Nara, K.; et al. Proposed diagnostic criteria, disease severity classification and treatment strategy for TAFRO syndrome, 2015 version. Int. J. Hematol. 2016, 103, 686–692. [Google Scholar] [CrossRef] [PubMed]
- Yanagiya, R.; Suzuki, T.; Nakamura, S.; Fujita, K.; Oyama, M.; Okuyama, A.; Sugasawa, K.; Nakayama, T.; Suzuki, Y.; Ishizawa, K.; et al. TAFRO syndrome presenting with retroperitoneal panniculitis-like computed tomography findings at disease onset. Intern. Med. 2020, 59, 997–1000. [Google Scholar] [CrossRef]
- Oka, S.; Ono, K.; Nohgawa, M. Subclinical hypothyroidism in TAFRO syndrome. Intern. Med. 2019, 58, 2615–2620. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, G.; Homma, N.; Kasai, A.; Kasami, T.; Makino, K.; Aoki, Y.; Wakaki, K.; Nakagawa, N. Magnetic resonance imaging of bone marrow for TAFRO syndrome. Mod. Rheumatol. 2019, 29, 551–557. [Google Scholar] [CrossRef]
- Fujiki, T.; Hirasawa, S.; Watanabe, S.; Iwamoto, S.; Ando, R. Successful treatment by tocilizumab without steroid in a very severe case of TAFRO syndrome. CEN Case Rep. 2017, 6, 105–110. [Google Scholar] [CrossRef]
- Yamagami, K.; Hanioka, Y.; Yao, S.; Nakamura, R.; Nakamura, T.; Ishii, N.; Goto, H. A case of TAFRO syndrome maintained in remission for 5 years after discontinuation of tocilizumab. Mod. Rheumatol. Case Rep. 2022, 7, 205–210. [Google Scholar] [CrossRef]
- Zhou, Q.; Zhang, Y.; Zhou, G.; Zhu, J. Kidney biopsy findings in two patients with TAFRO syndrome: Case presentations and review of the literature. BMC Nephrol. 2020, 21, 499. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, K.; Sano, T.; Honma, Y.; Ida, M.; Tominaga, H.; Sawada, A.; Abe, T.; Takahashi, H.; Shimada, Y.; Masaki, T.; et al. An autopsy case of TAFRO syndrome with membranoproliferative glomerulonephritis-like lesions. CEN Case Rep. 2019, 8, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Ducoux, G.; Guerber, A.; Durel, C.A.; Asli, B.; Fadlallah, J.; Hot, A. Thrombocytopenia, anasarca, fever, reticulin fibrosis/renal failure, and organomegaly (TAFRO) syndrome with bilateral adrenal hemorrhage in two Caucasian patients. Am. J. Case. Rep. 2020, 21, e919536. [Google Scholar] [CrossRef] [PubMed]
- Ono, S.; Yoshimoto, K.; Nishimura, N.; Yoneima, R.; Kawashima, H.; Kobayashi, T.; Tai, Y.; Miyamoto, M.; Tsushima, E.; Yada, N.; et al. Complete resolution of a case of TAFRO syndrome accompanied by mediastinal panniculitis, adrenal lesion, and liver damage with hyperbilirubinemia. Intern. Med. 2021, 60, 1303–1309. [Google Scholar] [CrossRef] [PubMed]
- Nagayama, Y.; Yamano, M.; Yagame, M.; Nariyama, T.; Takahashi, M.; Kawamoto, M.; Matsui, K. TAFRO syndrome as a cause of glomerular microangiopathy: A case report and literature review. BMC Nephrol. 2019, 20, 375. [Google Scholar] [CrossRef] [PubMed]
- Allegra, A.; Rotondo, F.; Russo, S.; Calabrò, L.; Maisano, V.; Bacci, F.; Musolino, C. Castleman–Kojima disease (TAFRO syndrome) in a Caucasian patient: A rare case report and review of the literature. Blood Cells Mol. Dis. 2015, 55, 206–207. [Google Scholar] [CrossRef]
- Yamamoto, S.; Wells, K.; Morita, K.; Tanigaki, K.; Muro, K.; Matsumoto, M.; Nakai, H.; Arai, Y.; Akizuki, S.; Takahashi, K.; et al. Severe TAFRO syndrome mimicking hepatorenal syndrome successfully treated with a multidisciplinary approach: A case report and literature review. Intern. Med. 2023, 62, 2715–2724. [Google Scholar] [CrossRef]
- Abe, N.; Kono, M.; Kono, M.; Ohnishi, N.; Sato, T.; Tarumi, M.; Yoshimura, M.; Sato, T.; Karino, K.; Shimizu, Y.; et al. Glycogen synthase kinase 3β/CCR6-positive bone marrow cells correlate with disease activity in multicentric Castleman disease-TAFRO. Br. J. Haematol. 2022, 196, 1194–1204. [Google Scholar] [CrossRef]
- Ohta, R.; Sano, C. Thrombocytopenia, Anasarca, Myelofibrosis, Renal dysfunction, and Organomegaly (TAFRO) Syndrome Initially Diagnosed as Fibromyalgia: A Case Report. Cureus 2023, 15, e42514. [Google Scholar] [CrossRef]
- Hayashi, M.; Wada, J.; Fujita, M.; Asano, T.; Matsuoka, N.; Fujita, Y.; Temmoku, J.; Matsumoto, H.; Yashio-Furuya, M.; Sato, S.; et al. TAFRO syndrome complicated by porto-sinusoidal vascular liver disease with portal hypertension: A case report. Clin. J. Gastroenterol. 2021, 14, 1711–1717. [Google Scholar] [CrossRef]
- Minomo, S.; Fujiwara, Y.; Sakashita, S.; Takamura, A.; Nagata, K. A severe case of thrombocytopenia, anasarca, fever, renal insufficiency or reticulin fibrosis, and organomegaly syndrome with myocardial and skeletal muscle calcification despite hypocalcemia: A case report. J. Med. Case Rep. 2021, 15, 3. [Google Scholar] [CrossRef] [PubMed]
- Matsuhisa, T.; Takahashi, N.; Nakaguro, M.; Sato, M.; Inoue, E.; Teshigawara, S.; Ozawa, Y.; Kondo, T.; Nakamura, S.; Sato, J.; et al. Fatal case of TAFRO syndrome associated with over-immunosuppression: A case report and review of the literature. Nagoya J. Med. Sci. 2019, 81, 519–528. [Google Scholar] [PubMed]
- Fujiwara, Y.; Ito, K.; Takamura, A.; Nagata, K. The first case of thrombocytopenia, anasarca, fever, renal impairment or reticulin fibrosis, and organomegaly (TAFRO) syndrome with unilateral adrenal necrosis: A case report. J. Med. Case Reports 2018, 12, 295. [Google Scholar] [CrossRef] [PubMed]
- Kageyama, C.; Igawa, T.; Gion, Y.; Iwaki, N.; Tabata, T.; Tanaka, T.; Kondo, E.; Sakai, H.; Tsuneyama, K.; Nomoto, K.; et al. Hepatic Campylobacter jejuni infection in patients with Castleman-Kojima disease (idiopathic multicentric Castleman disease with thrombocytopenia, anasarca, fever, reticulin fibrosis, and organomegaly (TAFRO) syndrome). Pathol. Int. 2019, 69, 572–579. [Google Scholar] [CrossRef] [PubMed]
- Coutier, F.; Meaux Ruault, N.; Crepin, T.; Bouiller, K.; Gil, H.; Humbert, S.; Bedgedjian, I.; Magy-Bertrand, N. A comparison of TAFRO syndrome between Japanese and non-Japanese cases: A case report and literature review. Ann. Hematol. 2018, 97, 401–407. [Google Scholar] [CrossRef] [PubMed]
- Kawabata, H.; Kotani, S.-i.; Matsumura, Y.; Kondo, T.; Katsurada, T.; Haga, H.; Kadowaki, N.; Takaori-Kondo, A. Successful treatment of a patient with multicentric castleman’s disease who presented with thrombocytopenia, ascites, renal failure and myelofibrosis using tocilizumab, an anti-interleukin-6 receptor antibody. Intern. Med. 2013, 52, 1503–1507. [Google Scholar] [CrossRef] [PubMed]
- Hibi, A.; Mizuguchi, K.; Yoneyama, A.; Kasugai, T.; Kamiya, K.; Kamiya, K.; Ito, C.; Kominato, S.; Miura, T.; Koyama, K. Severe refractory TAFRO syndrome requiring continuous renal replacement therapy complicated with Trichosporon asahii infection in the lungs and myocardial infarction: An autopsy case report and literature review. Ren. Replace. Ther. 2018, 4, 16. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, Y.; Maeda, Y.; Shibahara, T.; Nameki, S.; Nakabayashi, A.; Komuta, K.; Mizuno, Y.; Yagita, M.; Manabe, Y.; Morita, T.; et al. Recovery from prolonged thrombocytopenia in patients with TAFRO syndrome: Case series and literature review. Mod. Rheumatol. Case Rep. 2020, 4, 302–309. [Google Scholar] [CrossRef]
- Wakiya, R.; Kameda, T.; Takeuchi, Y.; Ozaki, H.; Nakashima, S.; Shimada, H.; Kadowaki, N.; Dobashi, H. Sequential change in serum VEGF levels in a case of tocilizumab-resistant TAFRO syndrome treated effectively with rituximab. Mod. Rheumatol. Case Rep. 2021, 5, 145–151. [Google Scholar] [CrossRef]
- Tsurumi, H.; Fujigaki, Y.; Yamamoto, T.; Iino, R.; Taniguchi, K.; Nagura, M.; Arai, S.; Tamura, Y.; Ota, T.; Shibata, S.; et al. Remission of refractory ascites and discontinuation of hemodialysis after additional rituximab to long-term glucocorticoid therapy in a patient with TAFRO syndrome. Intern. Med. 2018, 57, 1433–1438. [Google Scholar] [CrossRef]
- Pierson, S.K.; Stonestrom, A.J.; Shilling, D.; Ruth, J.; Nabel, C.S.; Singh, A.; Ren, Y.; Stone, K.; Li, H.; van Rhee, F.; et al. Plasma proteomics identifies a ‘chemokine storm’ in idiopathic multicentric Castleman disease. Am. J. Hematol. 2018, 93, 902–912. [Google Scholar] [CrossRef] [PubMed]
- Iwaki, N.; Gion, Y.; Kondo, E.; Kawano, M.; Masunari, T.; Moro, H.; Nikkuni, K.; Takai, K.; Hagihara, M.; Hashimoto, Y.; et al. Elevated serum interferon γ-induced protein 10 kDa is associated with TAFRO syndrome. Sci. Rep. 2017, 7, 42316. [Google Scholar] [CrossRef] [PubMed]
- Dufour, J.H.; Dziejman, M.; Liu, M.T.; Leung, J.H.; Lane, T.E.; Luster, A.D. IFN-γ-inducible protein 10 (IP-10; CXCL10)-deficient mice reveal a role for IP-10 in effector T cell generation and trafficking. J. Immunol. 2002, 168, 3195–3204. [Google Scholar] [CrossRef] [PubMed]
- Fajgenbaum, D.C.; Langan, R.-A.; Japp, A.S.; Partridge, H.L.; Pierson, S.K.; Singh, A.; Arenas, D.J.; Ruth, J.R.; Nabel, C.S.; Stone, K.; et al. Identifying and targeting pathogenic PI3K/AKT/mTOR signaling in IL-6 blockade–refractory idiopathic multicentric Castleman disease. J. Clin. Investig. 2019, 129, 4451–4463. [Google Scholar] [CrossRef] [PubMed]
- Goteti, S.; Johnson, A.; Williams, T.; Richardson, K.; Hogan, M. An infant with TAFRO syndrome: Case report and review of the literature. Authorea 2022. [Google Scholar] [CrossRef]
- Nagai, M.; Uchida, T.; Yamada, M.; Komatsu, S.; Ota, K.; Mukae, M.; Iwamoto, H.; Hirano, H.; Karube, M.; Kaname, S.; et al. TAFRO syndrome in a kidney transplant recipient that was diagnosed on autopsy: A case report. Front. Med. 2021, 8, 747678. [Google Scholar] [CrossRef] [PubMed]
- Hiramatsu, S.; Ohmura, K.; Tsuji, H.; Kawabata, H.; Kitano, T.; Sogabe, A.; Hashimoto, M.; Murakami, K.; Imura, Y.; Yukawa, N.; et al. Successful treatment by rituximab in a patient with TAFRO syndrome with cardiomyopathy. Nihon Rinsho Meneki Gakkai Kaishi 2016, 39, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Yasuda, S.; Tanaka, K.; Ichikawa, A.; Watanabe, K.; Uchida, E.; Yamamoto, M.; Yamamoto, K.; Mizuchi, D.; Miura, O.; Fukuda, T. Aggressive TAFRO syndrome with reversible cardiomyopathy successfully treated with combination chemotherapy. Int. J. Hematol. 2016, 104, 512–518. [Google Scholar] [CrossRef] [PubMed]
- Moy, L.N.; Patel, M.; Eschbach, J.; Knouse, P.; Gálvez, Á. A case of TAFRO syndrome with DIC and neurologic and cardiac involvement. Clin. Case Rep. 2023, 11, e07340. [Google Scholar] [CrossRef]
- Goel, M.; Flaherty, L.; Lavine, S.; Redman, B.G. Reversible Cardiomyopathy After High-Dose Interleukin-2 Therapy. J. Immunother. 1992, 11, 225–229. [Google Scholar] [CrossRef]
| Treatments (Suspected Drugs) | Adverse Events | |||
|---|---|---|---|---|
| Monotherapy | ||||
| Glucocorticoid | Bacterial infection [26,27,28,29] | CMV infection [3,28,29,30,31] | Fungal infection [29] | Tuberculosis [32] |
| Tocilizumab | Bacterial infection [29] | Toxic epidermal necrolysis [33] | ||
| Cyclosporine A | Hepatotoxicity [20,30,34,35,36] | Renal toxicity [37] | Thrombotic microangiopathy [38] | |
| Combination therapy with glucocorticoid | ||||
| Tocilizumab | Bacterial infection [20,39,40,41,42,43] | CMV infection [37,43,44,45,46] | Fungal infection [40,42] | |
| Cyclosporine A | Bacterial infection [47] | CMV infection [32,47,48] | Fungal infection [14,17,47] | |
| Rituximab | Bacterial infection [49,50] | CMV infection [50] |
| Patient | 1 (Present Case) | 2 [20] | 3 [20] | 4 [55] | 5 [56] | 6 [38] | 7 [38] |
|---|---|---|---|---|---|---|---|
| Clinical characteristics | |||||||
| Disease new-onset or relapse | New onset | New onset | New onset | New onset | Relapse | New onset | Relapse |
| Sex | Female | Female | Male | Female | Male | Female | Male |
| Age at disease onset or relapse | 33 | 68 | 17 | 11 months | 57 | 47 | 64 |
| Disease severity classification [21] | 3 | 3 | 3 | 2 | 2 | 4 | 2 |
| Treatment history | |||||||
| Previous treatment | N.A. | N.A. | N.A. | N.A. | PSL, TAC, MMF | N.A. | PSL |
| Treatment for initial onset or relapse | |||||||
| mPSL/PSL | + | + | + | + | + | + | + |
| Experienced agents | TAC | TCZ, CsA, TAC | TAC | TCZ, TAC | TAC, MMF | TCZ, TAC, MMF, CsA | TAC, CsA |
| Effective agents | TAC | TAC | TAC | TCZ, TAC | − | CsA | CsA |
| Adverse events | − | TCZ: bacterial infection CsA: hepatotoxicity | − | − | − | − | − |
| Relapse-free survival | >4 years | >6 years | >5 years | >1.5 years | − | N.A. | N.A. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shirai, T.; Ichikawa, S.; Saegusa, J. Tacrolimus Treatment for TAFRO Syndrome. Biomedicines 2024, 12, 1070. https://doi.org/10.3390/biomedicines12051070
Shirai T, Ichikawa S, Saegusa J. Tacrolimus Treatment for TAFRO Syndrome. Biomedicines. 2024; 12(5):1070. https://doi.org/10.3390/biomedicines12051070
Chicago/Turabian StyleShirai, Taiichiro, Shinya Ichikawa, and Jun Saegusa. 2024. "Tacrolimus Treatment for TAFRO Syndrome" Biomedicines 12, no. 5: 1070. https://doi.org/10.3390/biomedicines12051070
APA StyleShirai, T., Ichikawa, S., & Saegusa, J. (2024). Tacrolimus Treatment for TAFRO Syndrome. Biomedicines, 12(5), 1070. https://doi.org/10.3390/biomedicines12051070






