Is Ultrasonography an Effective Method for Diagnosing Degenerative Changes in the Temporomandibular Joint?
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
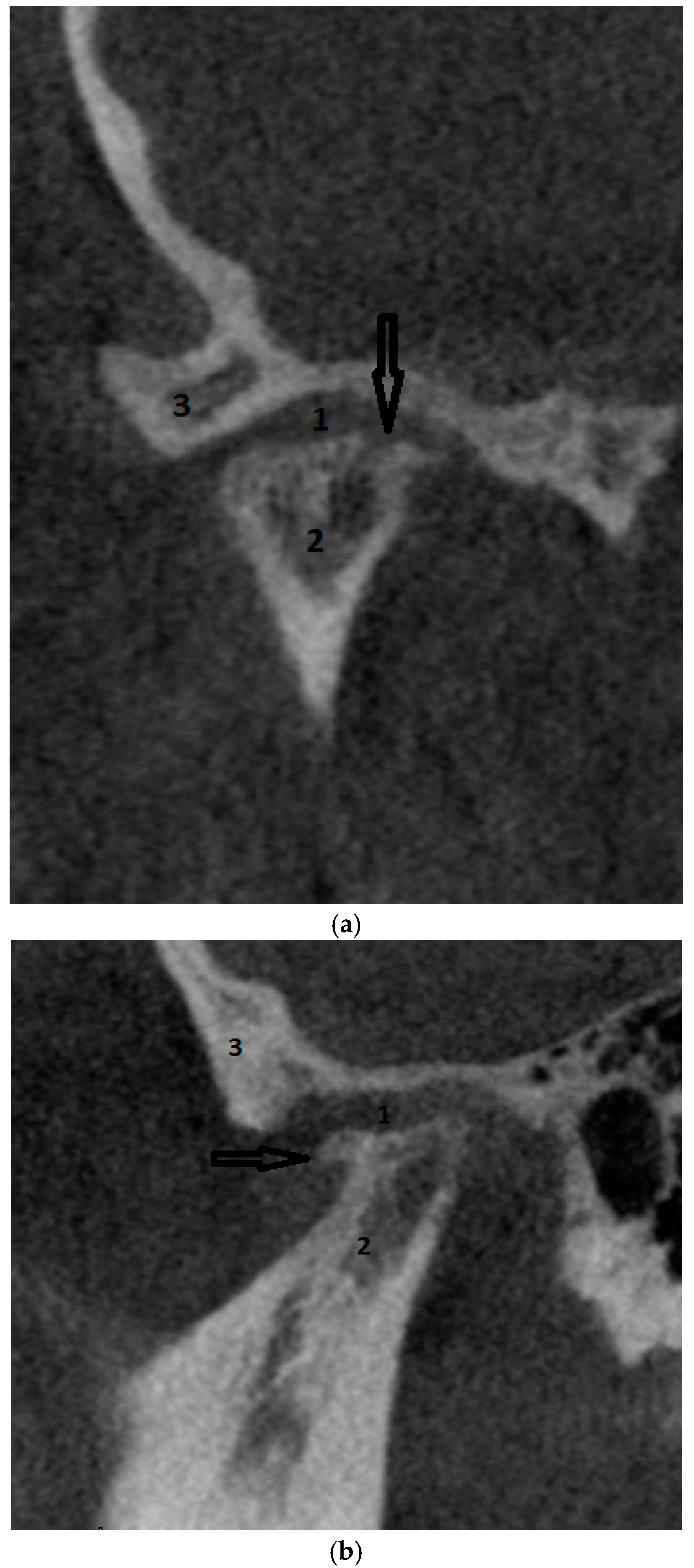
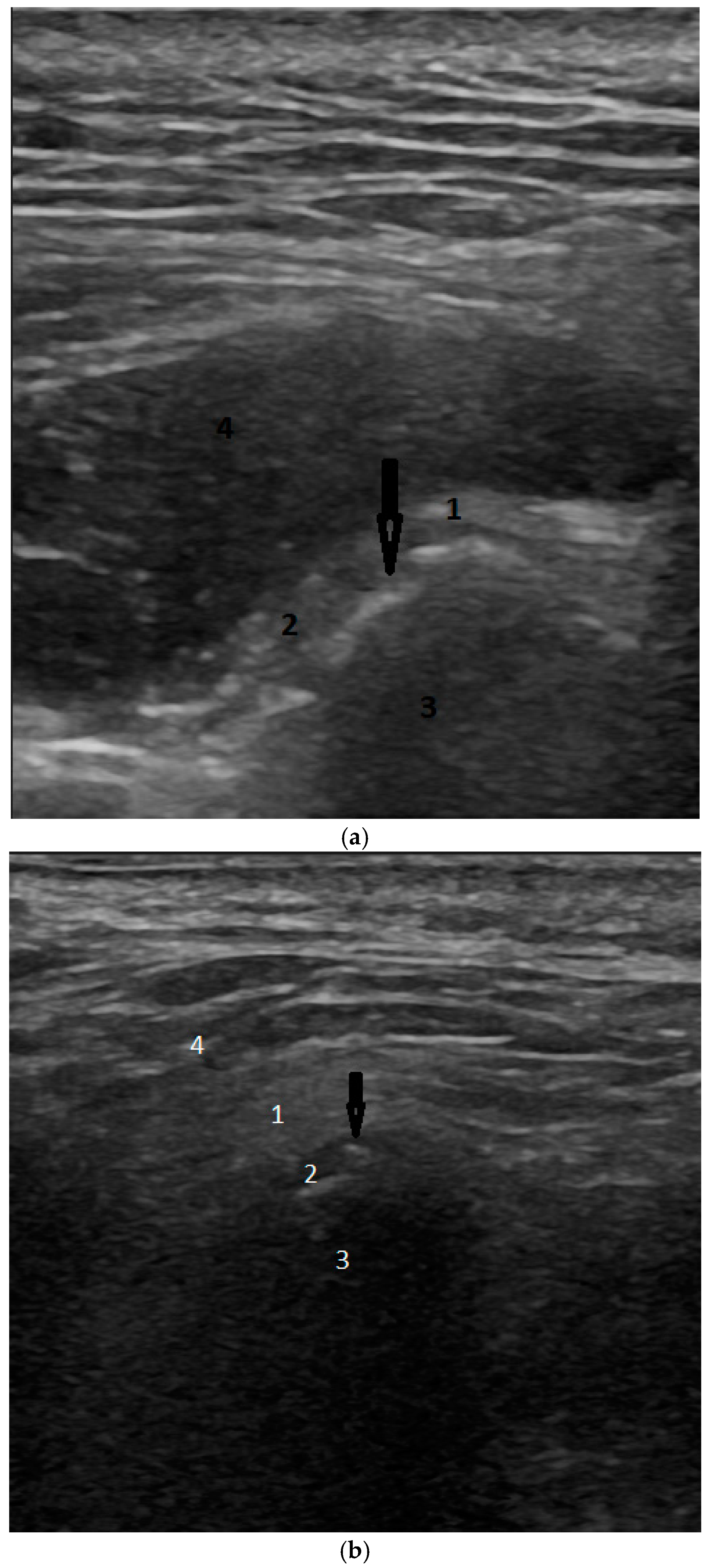
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kapos, F.P.; Exposto, F.G.; Oyarzo, J.F.; Durham, J. Temporomandibular disorders: A review of current concepts in aetiology, diagnosis and management. Oral Surg. 2020, 13, 321–334. [Google Scholar] [CrossRef] [PubMed]
- Alomar, X.; Medrano, J.; Cabratosa, J.; Clavero, J.A.; Lorente, M.; Serra, I.; Monill, J.M.; Salvador, A. Anatomy of the temporomandibular joint. Semin. Ultrasound CT MRI 2007, 28, 170–183. [Google Scholar] [CrossRef]
- Bechtold, T.E.; Kurio, N.; Nah, H.-D.; Saunders, C.; Billings, P.C.; Koyama, E. The Roles of Indian Hedgehog Signaling in TMJ Formation. Int. J. Mol. Sci. 2019, 20, 6300. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Gupta, D.S.; Pal, U.S.; Jurel, S.K. Etiological factors of temporomandibular joint disorders. Natl. J. Maxillofac. Surg. 2011, 2, 116–119. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Acharya, G.; Singh, H.; Poudyal, S.; Redhu, A.; Shivhare, P. Assessment of Condylar Shape through Digital Panoramic Radiograph among Nepalese Population: A Proposal for Classification. BioMed Res. Int. 2022, 2022, 6820824. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, M.; Schiffman, E.L. Temporomandibular Joint Disorders and Orofacial Pain. Dent. Clin. N. Am. 2016, 60, 105–124. [Google Scholar] [CrossRef]
- Wroclawski, C.; Mediratta, J.K.; Fillmore, W.J. Recent Advances in Temporomandibular Joint Surgery. Medicina 2023, 59, 1409. [Google Scholar] [CrossRef] [PubMed]
- Gauer, R.L.; Semidey, M.J. Diagnosis and treatment of temporomandibular disorders. Am. Fam. Physician 2015, 91, 378–386. [Google Scholar]
- Zieliński, G.; Pająk-Zielińska, B.; Ginszt, M. A Meta-Analysis of the Global Prevalence of Temporomandibular Disorders. J. Clin. Med. 2024, 13, 1365. [Google Scholar] [CrossRef] [PubMed]
- Wojciechowska, B.; Szarmach, A.; Michcik, A.; Wach, T.; Drogoszewska, B. Association between Clinical Manifestations in Temporomandibular Joint Disorders and Corresponding Radiographic Findings. J. Clin. Med. 2024, 13, 4886. [Google Scholar] [CrossRef]
- Murphy, M.K.; MacBarb, R.F.; Wong, M.E.; Athanasiou, K.A. Temporomandibular disorders: A review of etiology, clinical management, and tissue engineering strategies. Int. J. Oral Maxillofac. Implant. 2013, 28, 393–414. [Google Scholar] [CrossRef]
- Mélou, C.; Pellen-Mussi, P.; Jeanne, S.; Novella, A.; Tricot-Doleux, S.; Chauvel-Lebret, D. Osteoarthritis of the Temporomandibular Joint: A Narrative Overview. Medicina 2023, 59, 8. [Google Scholar] [CrossRef] [PubMed]
- Chung, M.K.; Wang, S.; Alshanqiti, I.; Hu, J.; Ro, J.Y. The degeneration-pain relationship in the temporomandibular joint: Current understandings and rodent models. Front. Pain Res. 2023, 4, 1038808. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, V.; Sharma, G.; Dutra, E.H.; Chen, P.J.; Yadav, S. Degenerative disorders of temporomandibular joint—Current practices and treatment modalities. Semin. Orthod. 2024, 30, 271–276. [Google Scholar] [CrossRef]
- Tanaka, E.; Detamore, M.S.; Mercuri, L.G. Degenerative disorders of the temporomandibular joint: Etiology, diagnosis, and treatment. J. Dent. Res. 2008, 87, 296–307. [Google Scholar] [CrossRef] [PubMed]
- Feng, S.Y.; Lei, J.; Li, Y.X.; Shi, W.G.; Wang, R.R.; Yap, A.U.; Wang, Y.X.; Fu, K.Y. Increased joint loading induces subchondral bone loss of the temporomandibular joint via the RANTES-CCRs-Akt2 axis. JCI Insight 2022, 7, 158874. [Google Scholar] [CrossRef]
- Yap, A.U.; Lei, J.; Zhang, X.H.; Fu, K.Y. TMJ degenerative joint disease: Relationships between CBCT findings, clinical symptoms, and signs. Acta Odontol. Scand. 2023, 81, 562–568. [Google Scholar] [CrossRef]
- Kothari, S.F.; Bead-Hansen, L.; Hansen, L.B.; Bang, N.; Sørensen, L.H.; Eskildsen, H.W.; Svensson, P. Pain profiling of patients with temporomandibular joint arthralgia and osteoarthritis diagnosed with different imaging techniques. J. Headache Pain 2016, 17, 61. [Google Scholar] [CrossRef]
- Bag, A.K.; Gaddikeri, S.; Singhal, A.; Hardin, S.; Tran, B.D.; Medina, J.A.; Curé, J.K. Imaging of the temporomandibular joint: An update. World J. Radiol. 2014, 6, 567–582. [Google Scholar] [CrossRef]
- Larheim, T.A.; Hol, C.; Ottersen, M.K.; Mork-Knutsen, B.B.; Arvidsson, L.Z. The Role of Imaging in the Diagnosis of Temporomandibular Joint Pathology. Oral Maxillofac. Surg. Clin. N. Am. 2018, 30, 239–249. [Google Scholar] [CrossRef]
- Dhabale, G.S.; Bhowate, R.R. Cone-Beam Computed Tomography for Temporomandibular Joint Imaging. Cureus 2022, 14, 31515. [Google Scholar] [CrossRef]
- Palconet, G.; Ludlow, J.B.; Tyndall, D.A.; Lim, P.F. Correlating cone beam CT results with temporomandibular joint pain of osteoarthritic origin. Dentomaxillofac. Radiol. 2012, 41, 126–130. [Google Scholar] [CrossRef]
- De Nordenflycht, D.; Tesch, R.S. Advantages of ultrasound guidance for TMJ arthrocentesis and intra-articular injection: A narrative review. Dent. Med. Probl. 2022, 59, 647–656. [Google Scholar] [CrossRef]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendationsof the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group. J. Oral Facial Pain Headache 2014, 28, 6–27. [Google Scholar] [CrossRef]
- Zaman, M.U.; Alam, M.K.; Alqhtani, N.R.; Alqahtani, M.; Alsaadi, M.J.; Ronsivalle, V.; Cicciù, M.; Minervini, G. Effectiveness of ultrasonography in the diagnosis of temporomandibular joint disorders: A systematic review and meta-analysis. J. Oral Rehabil. 2024. ahead of printing. [Google Scholar] [CrossRef]
- Manfredini, D.; Guarda-Nardini, L. Ultrasonography of the temporomandibular joint: A literature review. Int. J. Oral Maxillofac. Surg. 2009, 38, 1229–1236. [Google Scholar] [CrossRef]
- Halligan, S.; Altman, D.G.; Mallett, S. Disadvantages of using the area under the receiver operating characteristic curve to assess imaging tests: A discussion and proposal for an alternative approach. Eur. Radiol. 2015, 25, 932–939. [Google Scholar] [CrossRef]
- Chęciński, M.; Chęcińska, K.; Bliźniak, F.; Lubecka, K.; Turosz, N.; Rąpalska, I.; Michcik, A.; Chlubek, D.; Sikora, M. Temporomandibular Joint (TMJ) Replacement Affects Quality of Life: A Systematic Review and Synthesis of Clinical Trials. Appl. Sci. 2024, 14, 2912. [Google Scholar] [CrossRef]
- Lubecka, K.; Chęcińska, K.; Bliźniak, F.; Chęciński, M.; Turosz, N.; Michcik, A.; Chlubek, D.; Sikora, M. Intra-Articular Local Anesthetics in Temporomandibular Disorders: A Systematic Review and Meta-Analysis. J. Clin. Med. 2024, 13, 106. [Google Scholar] [CrossRef] [PubMed]
- Klatkiewicz, T.; Gawriołek, K.; Pobudek Radzikowska, M.; Czajka-Jakubowska, A. Ultrasonography in the Diagnosis of Temporomandibular Disorders: A Meta-Analysis. Med. Sci. Monit. 2018, 24, 812–817. [Google Scholar] [CrossRef]
- Hussain, A.M.; Packota, G.; Major, P.W.; Flores-Mir, C. Role of different imaging modalities in assessment of temporomandibular joint erosions and osteophytes: A systematic review. Dentomaxillofac. Radiol. 2008, 37, 63–71. [Google Scholar] [CrossRef]
- Almashraqi, A.A.; Sayed, B.A.; Mokli, L.K.; Jaafari, S.A.; Halboub, E.; Parveen, S.; Al-Ak’hali, M.S.; Alhammadi, M.S. Recommendations for standard criteria for the positional and morphological evaluation of temporomandibular joint osseous structures using cone-beam CT: A systematic review. Eur. Radiol. 2024, 34, 3126–3140. [Google Scholar] [CrossRef] [PubMed]
- Al-Saleh, M.A.; Alsufyani, N.A.; Saltaji, H.; Jaremko, J.L.; Major, P.W. MRI and CBCT image registration of temporomandibular joint: A systematic review. J. Otolaryngol. Head Neck Surg. 2016, 45, 30. [Google Scholar] [CrossRef] [PubMed]
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Patients over 18 years of age | Patients under 18 years of age |
| Patients who presented to the Maxillofacial Surgery Department due to TMD | Patients with polyarthritis (such as rheumatoid arthritis, gout arthritis and psoriatic arthritis) |
| Patients who agreed to participate in the study | Subjects who were not willing to participate in the study |
| Patients with history of TMD treatment | |
| Patients with trauma | |
| Patients with a history of orthodontic treatment, plastic surgery, or other craniofacial surgery |
| Characteristic | n | Examination Technique | p b | |
|---|---|---|---|---|
| CBCT, n1 = 40 a | US, n2 = 40 a | |||
| Right mandibular head | ||||
| normal outline | 40 | 22 (55.00%) | 31 (77.50%) | 0.039 |
| abnormal outline | 40 | 18 (45.00%) | 9 (22.50%) | 0.039 |
| erosions present | 40 | 7 (17.50%) | 3 (7.50%) | 0.289 |
| osteophytes present | 40 | 11 (27.50%) | 3 (7.50%) | 0.027 |
| Left mandibular head | ||||
| normal outline | 40 | 27 (67.50%) | 23 (57.50%) | 0.502 |
| abnormal outline | 40 | 13 (32.50%) | 10 (25.00%) | 0.628 |
| erosions present | 40 | 6 (15.00%) | 1 (2.50%) | 0.131 |
| osteophytes present | 40 | 5 (12.50%) | 8 (20.00%) | 0.505 |
| Bone structure | ||||
| normal (right) | 40 | 36 (90.00%) | 30 (75.00%) | 0.149 |
| normal (left) | 40 | 35 (87.50%) | 30 (75.00%) | 0.182 |
| Conclusions | ||||
| degenerative change (right joint) | 40 | 19 (47.50%) | 18 (45.00%) | 1.000 |
| degenerative change (left joint) | 40 | 14 (35.00%) | 22 (55.00%) | 0.043 |
| Characteristic | AC1 | SE | CI 95% | p |
|---|---|---|---|---|
| Right mandibular head | ||||
| normal outline | 0.32 | 0.16 | −0.002, 0.645 | 0.052 |
| abnormal outline | 0.32 | 0.16 | −0.002, 0.645 | 0.052 |
| erosions present | 0.74 | 0.10 | 0.549, 0.939 | <0.001 |
| osteophytes present | 0.65 | 0.12 | 0.411, 0.886 | <0.001 |
| Left mandibular head | ||||
| normal outline | 0.06 | 0.17 | −0.289, 0.406 | 0.734 |
| abnormal outline | 0.28 | 0.17 | −0.059, 0.619 | 0.103 |
| erosions present | 0.79 | 0.08 | 0.622, 0.961 | <0.001 |
| osteophytes present | 0.69 | 0.11 | 0.470, 0.911 | <0.001 |
| Bone structure | ||||
| normal (right) | 0.58 | 0.13 | 0.317, 0.840 | <0.001 |
| normal (left) | 0.68 | 0.11 | 0.448, 0.905 | <0.001 |
| Conclusions | ||||
| degenerative change (right joint) | 0.35 | 0.15 | 0.053, 0.654 | 0.022 |
| degenerative change (left joint) | 0.41 | 0.15 | 0.112, 0.700 | 0.008 |
| Characteristic | AP | AT | Sens | Spec | PPV | NPV | PLR | NLR | T+O− | T−O+ | T+T+ | T−T− | CCP |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Right mandibular head | |||||||||||||
| normal outline | 0.78 (0.62, 0.89) | 0.55 (0.38, 0.71) | 0.86 (0.65, 0.97) | 0.33 (0.13, 0.59) | 0.61 (0.42, 0.78) | 0.67 (0.30, 0.93) | 1.30 (0.90, 0.87) | 0.41 (0.12, 1.41) | 0.67 (0.41, 0.87) | 0.14 (0.03, 0.35) | 0.39 (0.22, 0.58) | 0.33 (0.07, 0.70) | 0.62 (0.46, 0.77) |
| abnormal outline | 0.22 (0.11, 0.38) | 0.45 (0.29, 0.62) | 0.33 (0.13, 0.59) | 0.86 (0.65, 0.97) | 0.67 (0.30, 0.93) | 0.61 (0.42, 0.78) | 2.44 (0.71, 8.43) | 0.77 (0.54, 1.11) | 0.14 (0.03, 0.35) | 0.67 (0.41, 0.87) | 0.33 (0.07, 0.70) | 0.39 (0.22, 0.58) | 0.62 (0.46, 0.77) |
| erosions present | 0.07 (0.02, 0.20) | 0.17 (0.07, 0.33) | 0.14 (0.00, 0.58) | 0.94 (0.80, 0.99) | 0.33 (0.01, 0.91) | 0.84 (0.68, 0.94) | 2.36 (0.25, 22.54) | 0.91 (0.67, 1.25) | 0.06 (0.01, 0.20) | 0.86 (0.42, 1.00) | 0.67 (0.09, 0.99) | 0.16 (0.09, 0.99) | 0.80 (0.64, 0.91) |
| osteophytes present | 0.07 (0.02, 0.20) | 0.28 (0.15, 0.44) | 0.18 (0.02, 0.52) | 0.97 (0.82, 1.00) | 0.67 (0.09, 0.99) | 0.76 (0.59, 0.88) | 5.27 (0.53, 52.48) | 0.85 (0.64, 1.13) | 0.03 (0.00, 0.18) | 0.82 (0.48, 0.98) | 0.33 (0.01, 0.91) | 0.24 (0.12, 0.41) | 0.75 (0.59, 0.87) |
| Left mandibular head | |||||||||||||
| normal outline | 0.57 (0.41, 0.73) | 0.68 (0.51, 0.81) | 0.56 (0.35, 0.75) | 0.38 (0.14, 0.68) | 0.65 (0.43, 0.84) | 0.29 (0.10, 0.56) | 0.90 (0.52, 1.56) | 1.16 (0.52, 2.59) | 0.62 (0.32, 0.86) | 0.44 (0.25, 0.65) | 0.35 (0.16, 0.57) | 0.71 (0.44, 0.90) | 0.50 (0.34, 0.66) |
| abnormal outline | 0.25 (0.13, 0.41) | 0.32 (0.19, 0.49) | 0.23 (0.05, 0.54) | 0.74 (0.54, 0.89) | 0.30 (0.07, 0.65) | 0.67 (0.47, 0.83) | 0.89 (0.27, 0.90) | 1.04 (0.72, 1,51) | 0.26 (0.11, 0.46) | 0.77 (0.46, 0.95) | 0.70 (0.35, 0.93) | 0.33 (0.17, 0.53) | 0.57 (0.41, 0.73) |
| erosions present | 0.02 (0.00, 0.13) | 0.15 (0.06, 0.30) | 0.00 (0.00, 0.46) | 0.97 (0.85, 1.00) | 0.00 (0.00, 0.97) | 0.85 (0.69, 0.94) | 0.00 (0.00, n/a) | 1.03 (0.97, 1.09) | 0.03 (0.00,0.15) | 1.00 (0.54,1.00) | 1.00 (0.02, 1.00) | 0.15 (0.06, 0.31) | 0.82 (0.67, 0.93) |
| osteophytes present | 0.20 (0.09, 0.36) | 0.12 (0.04, 0.27) | 0.40 (0.05, 0.85) | 0.83 (0.66, 0.93) | 0.25 (0.03, 0.65) | 0.91 (0.75, 0.98) | 2.33 (0.64, 8.54) | 0.72 (0.35, 1.50) | 0.17 (0.07, 0.34) | 0.60 (0.15, 0.95) | 0.75 (0.35, 0.97) | 0.09 (0.02, 0.25) | 0.78 (0.62, 0.89) |
| Bone structure | |||||||||||||
| normal (right) | 0.75 (0.59, 0.87) | 0.90 (0.76, 0.97) | 0.75 (0.58, 0.88) | 0.25 (0.01, 0.81) | 0.90 (0.73, 0.98) | 0.10 (0.00, 0.45) | 1.00 (0.55, 1.82) | 1.00 (0.17, 5.98) | 0.75 (0.19, 0.99) | 0.25 (0.12, 0.42) | 0.10 (0.02, 0.27) | 0.90 (0.55, 1.00) | 0.70 (0.53, 0.83) |
| normal (left) | 0.75 (0.59, 0.87) | 0.88 (0.73, 0.96) | 0.80 (0.63, 0.92) | 0.60 (0.15, 0.95) | 0.93 (0.78, 0.99) | 0.30 (0.07, 0.65) | 2.00 (0.67, 5.93) | 0.33 (0.13, 0.88) | 0.40 (0.05, 0.85) | 0.20 (0.08, 0.37) | 0.07 (0.01, 0.22) | 0.70 (0.35, 0.93) | 0.78 (0.62, 0.89) |
| Conclusions | |||||||||||||
| degenerative change (right joint) | 0.45 (0.29, 0.62) | 0.47 (0.32, 0.64) | 0.63 (0.38, 0.84) | 0.71 (0.48, 0.89) | 0.67 (0.41, 0.87) | 0.68 (0.45, 0.86) | 2.21 (1.04, 4.72) | 0.52 (0.27, 0.99) | 0.29 (0.11, 0.52) | 0.37 (0.16, 0.62) | 0.33 (0.13, 0.59) | 0.32 (0.14, 0.55) | 0.68 (0.51, 0.81) |
| degenerative change (left joint) | 0.55 (0.38, 0.71) | 0.35 (0.21, 0.52) | 0.86 (0.57, 0.98) | 0.62 (0.41, 0.80) | 0.55 (0.32, 0.76) | 0.89 (0.65, 0.99) | 2.23 (0.06, 0.87) | 0.23 (0.06, 0.87) | 0.38 (0.20, 0.59) | 0.14 (0.02, 0.43) | 0.45 (0.24, 0.68) | 0.11 (0.01, 0.35) | 0.70 (0.53,0.83) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wojciechowska, B.; Szarmach, A.; Michcik, A.; Sikora, M.; Drogoszewska, B. Is Ultrasonography an Effective Method for Diagnosing Degenerative Changes in the Temporomandibular Joint? Biomedicines 2024, 12, 2915. https://doi.org/10.3390/biomedicines12122915
Wojciechowska B, Szarmach A, Michcik A, Sikora M, Drogoszewska B. Is Ultrasonography an Effective Method for Diagnosing Degenerative Changes in the Temporomandibular Joint? Biomedicines. 2024; 12(12):2915. https://doi.org/10.3390/biomedicines12122915
Chicago/Turabian StyleWojciechowska, Barbara, Arkadiusz Szarmach, Adam Michcik, Maciej Sikora, and Barbara Drogoszewska. 2024. "Is Ultrasonography an Effective Method for Diagnosing Degenerative Changes in the Temporomandibular Joint?" Biomedicines 12, no. 12: 2915. https://doi.org/10.3390/biomedicines12122915
APA StyleWojciechowska, B., Szarmach, A., Michcik, A., Sikora, M., & Drogoszewska, B. (2024). Is Ultrasonography an Effective Method for Diagnosing Degenerative Changes in the Temporomandibular Joint? Biomedicines, 12(12), 2915. https://doi.org/10.3390/biomedicines12122915








