The Generation of ROS by Exposure to Trihalomethanes Promotes the IκBα/NF-κB/p65 Complex Dissociation in Human Lung Fibroblast
Abstract
1. Introduction
2. Materials and Methods
2.1. Culture of Human Lung MRC-5 Fibroblasts and Treatments
2.2. Evaluation of Biomarkers
2.3. Activity of the Antioxidant Defenses (SOD, CAT and GPx)
2.4. Assay of Phosphorylated NF-κB/p65 Levels
2.5. Molecular Docking Studies
2.6. Statistical Analysis
3. Results
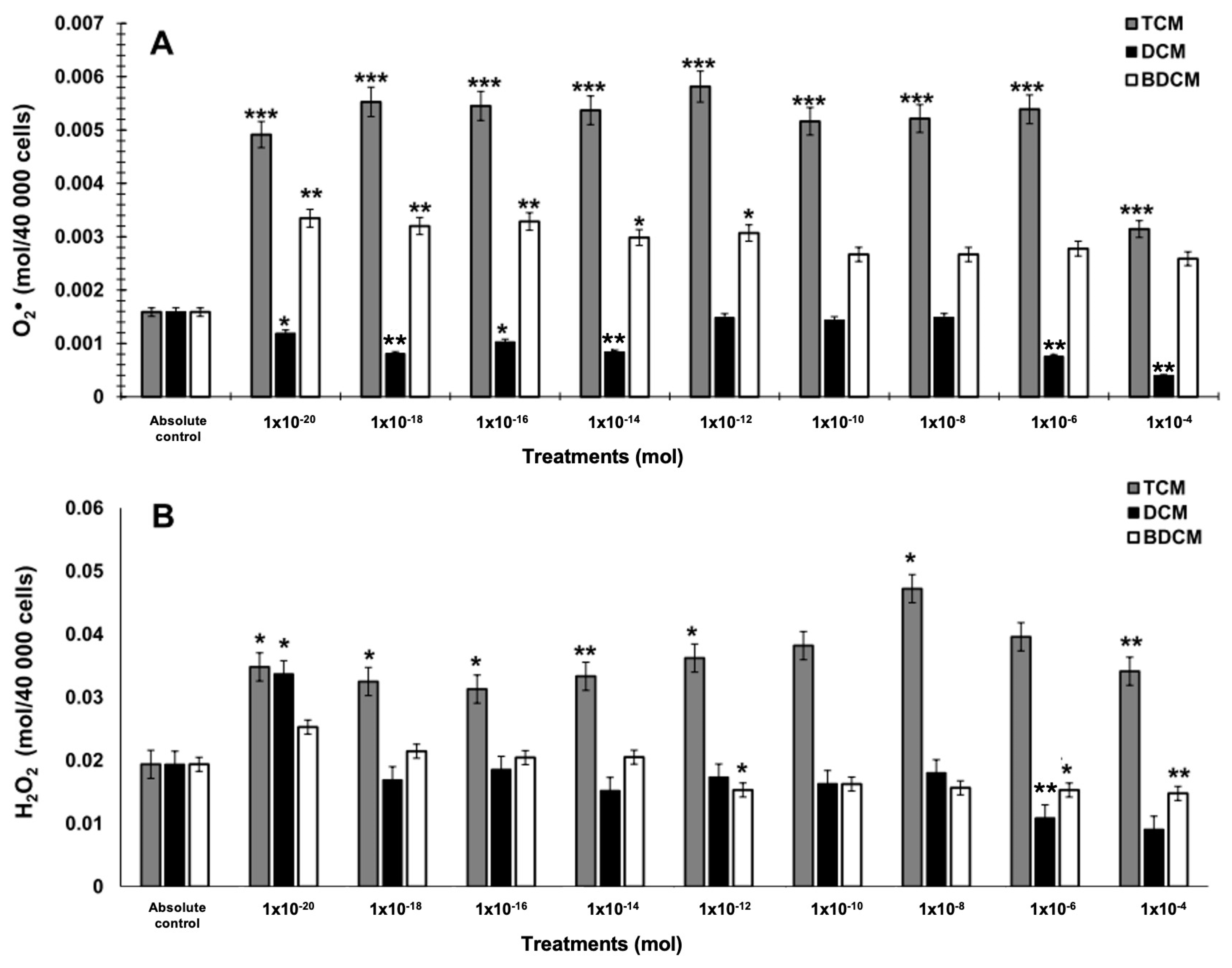
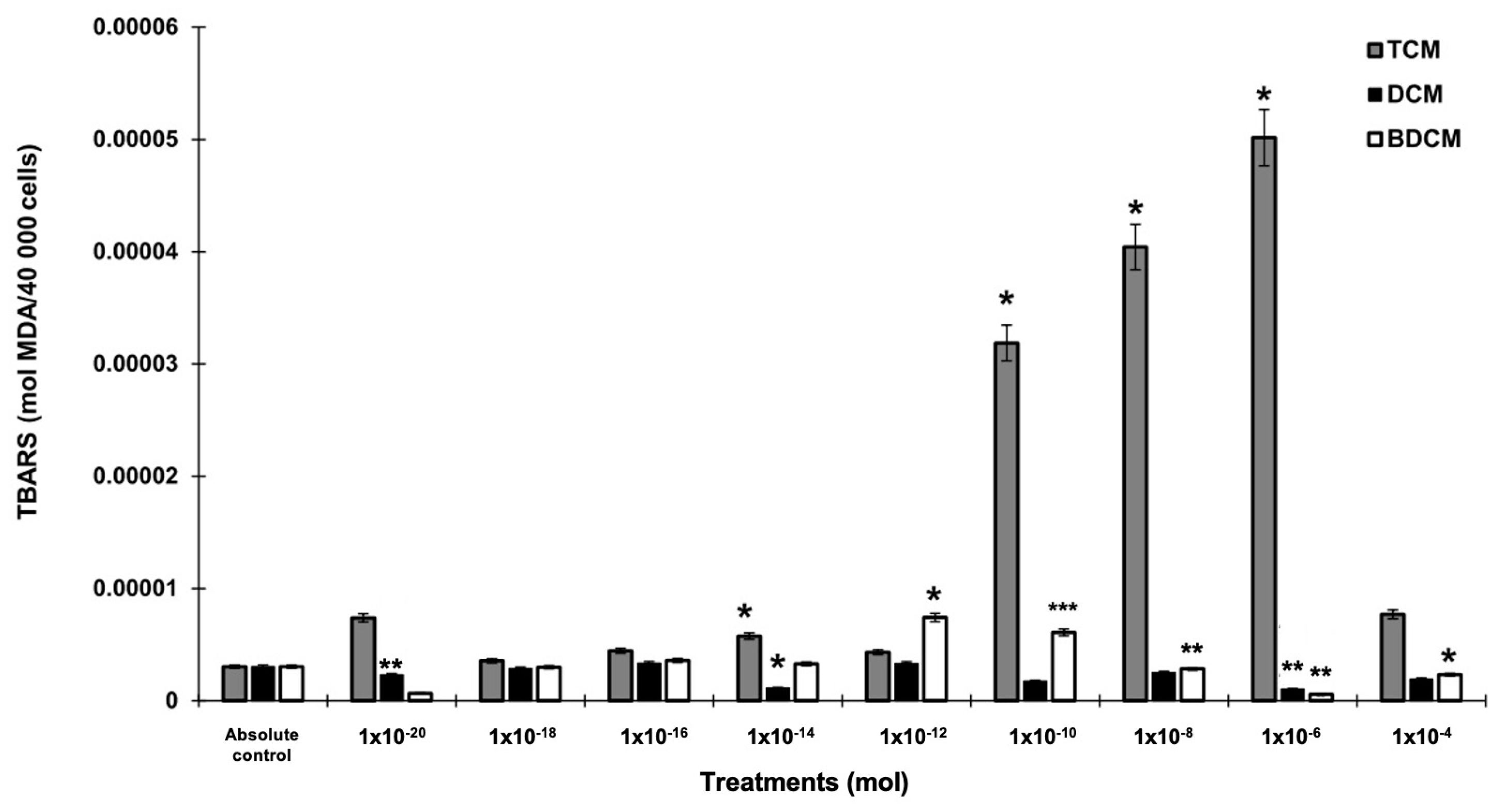
3.1. The Generation of Hydrogen Peroxide (H2O2), Superoxide Anion (O2•), and Lipid Peroxidation by Exposure to Halomethanes (CH2Cl2, CHCl3, BrCHCl2) in Human Lung Fibroblasts (MRC-5)
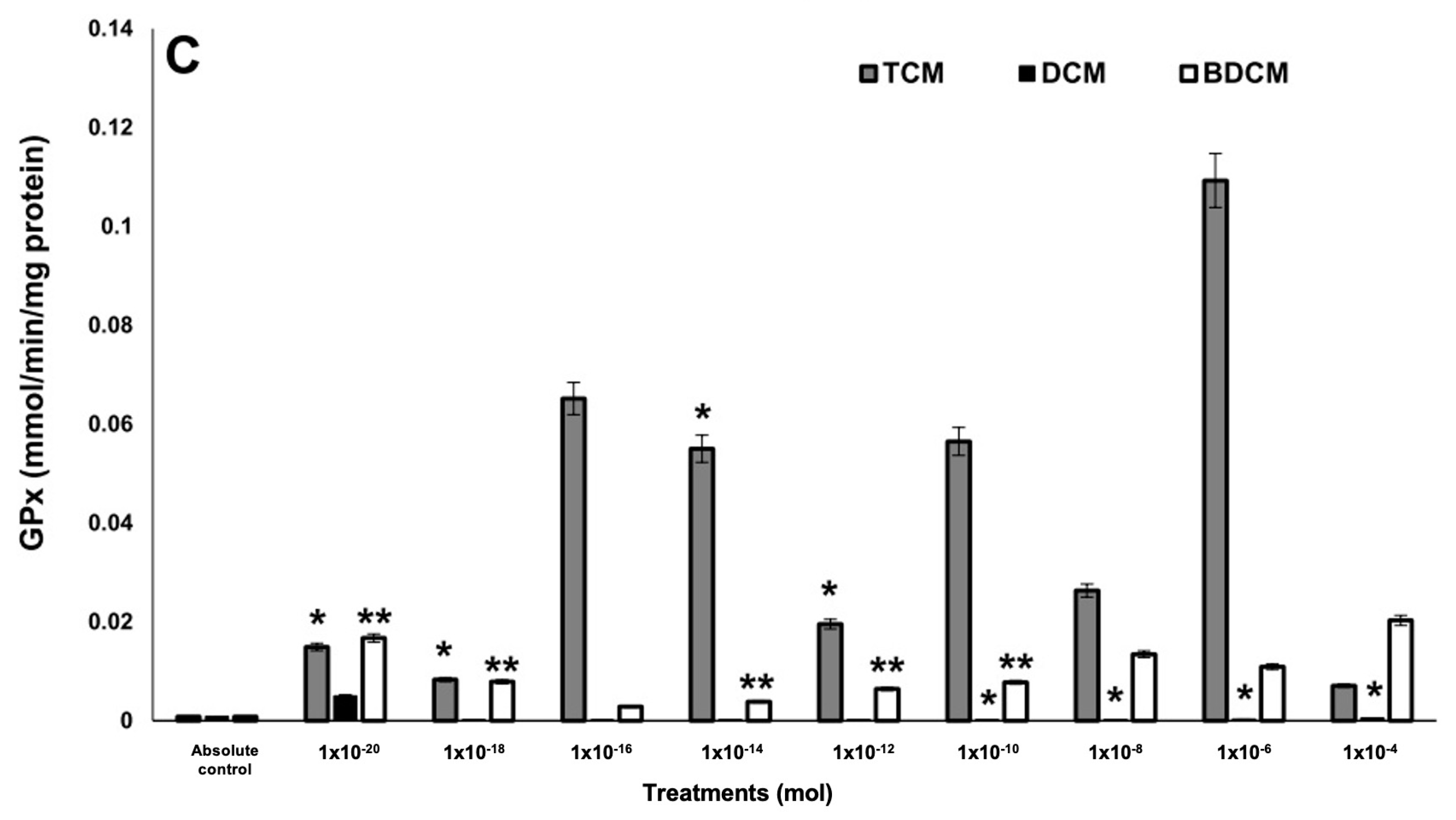
3.2. The Activity of the Antioxidant Enzymes
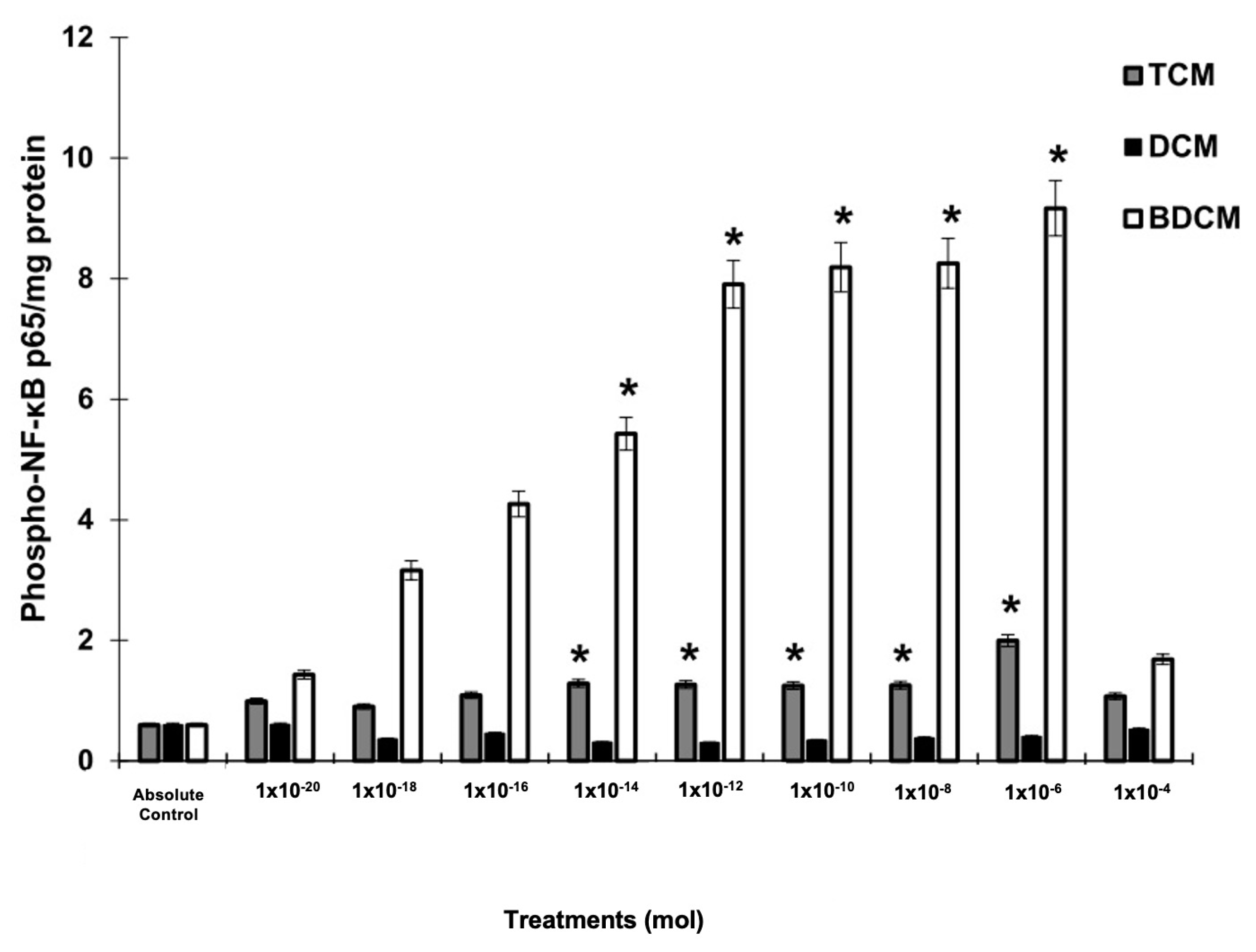
3.3. Evaluation of Phosphorylated NF-κB/p65 Levels
3.4. Relation Between Biomarkers
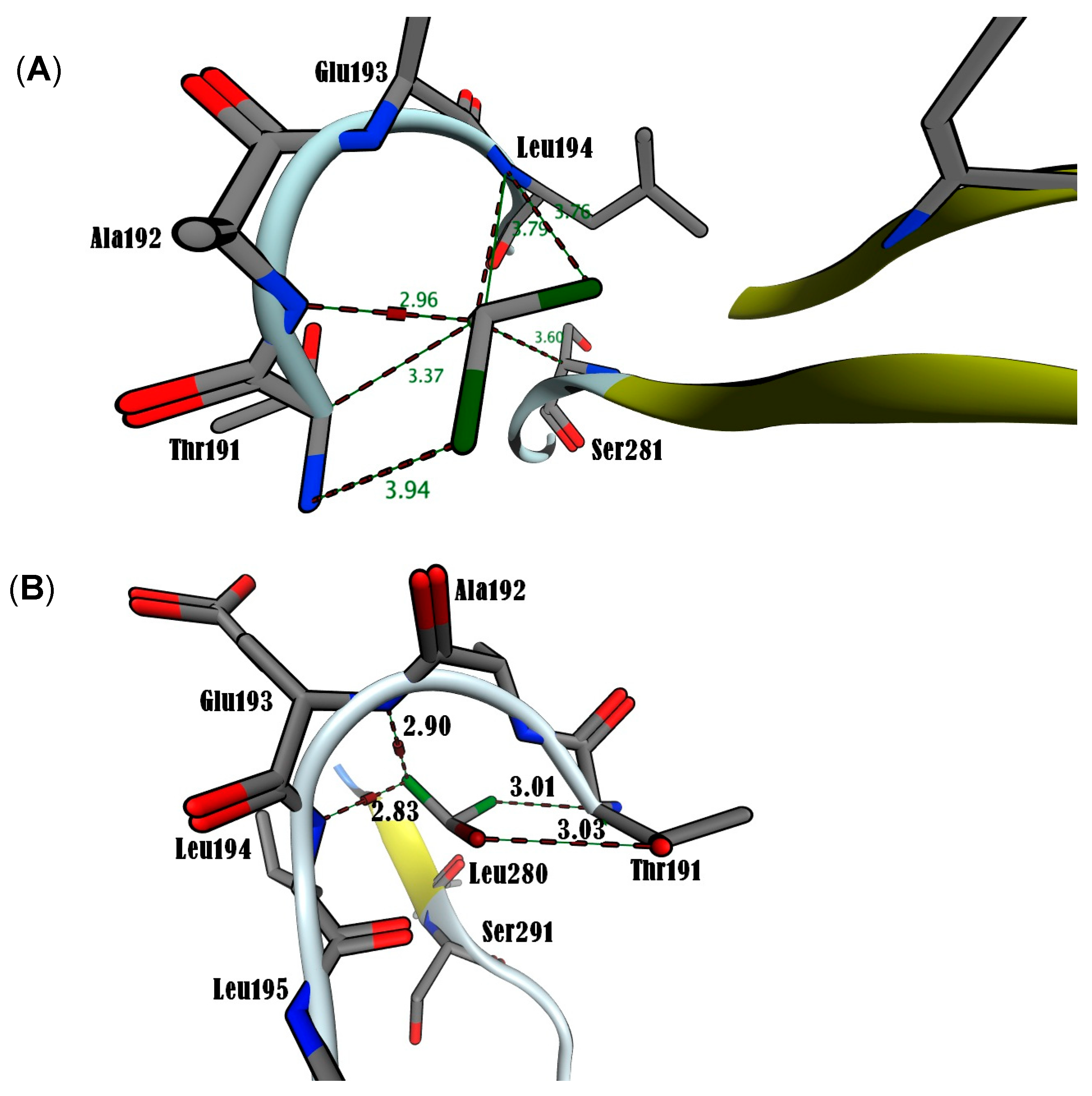
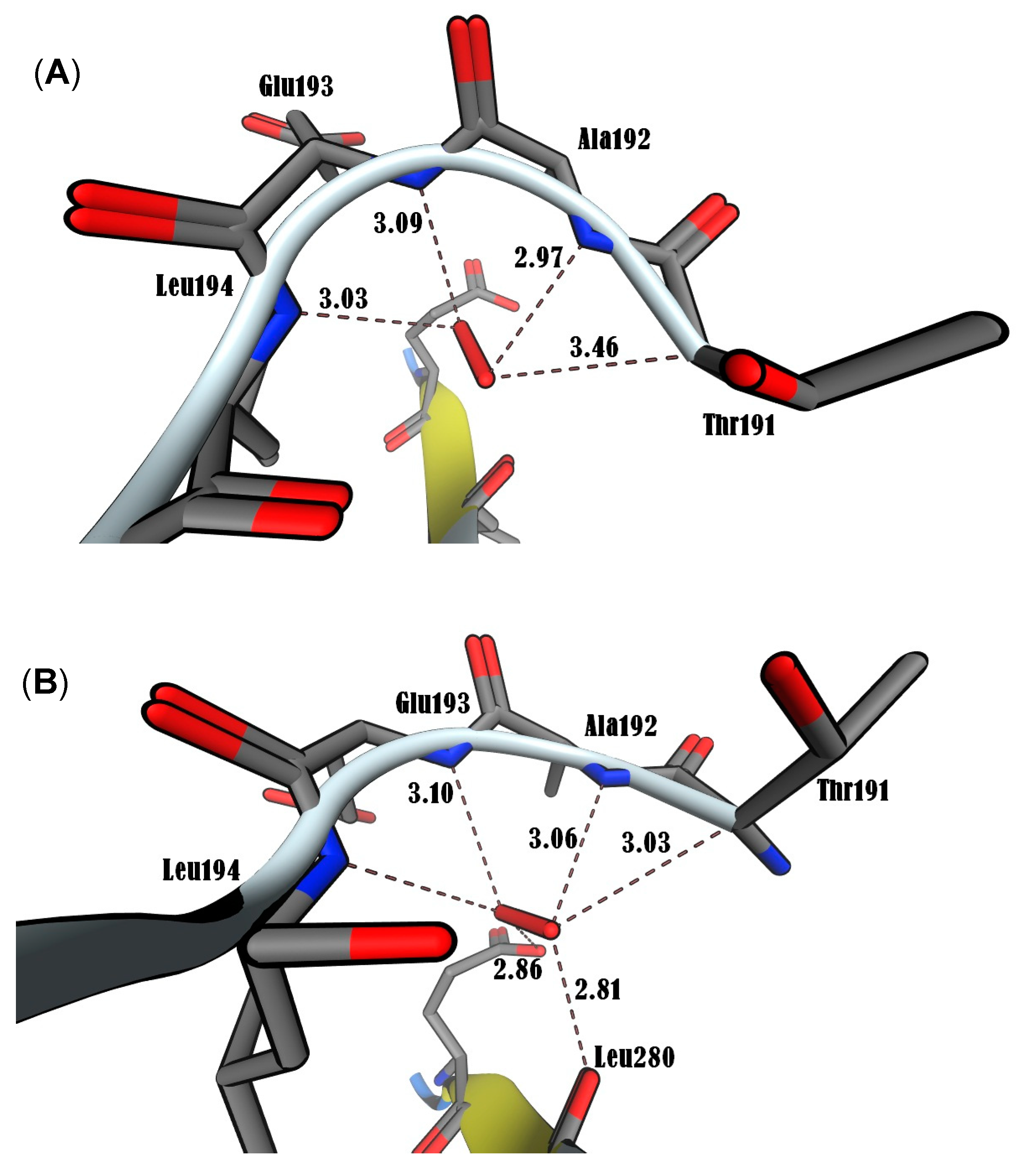
3.5. Molecular Docking Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Snezhkina, A.V.; Kudryavtseva, A.V.; Kardymon, O.L.; Savvateeva, M.V.; Melnikova, N.V.; Krasnov, G.S.; Dmitriev, A.A. ROS Generation and Antioxidant Defense Systems in Normal and Malignant Cells. Oxid. Med. Cell. Longev. 2019, 2019, 6175804. [Google Scholar] [CrossRef] [PubMed]
- Schieber, M.; Chandel, N.S. ROS function in redox signaling and oxidative stress. Curr. Biol. 2014, 24, R453–R462. [Google Scholar] [CrossRef] [PubMed]
- Fulda, S.; Gorman, A.M.; Hori, O.; Samali, A. Cellular Stress Responses: Cell Survival and Cell Death. Int. J. Cell Biol. 2010, 2010, 214074. [Google Scholar] [CrossRef] [PubMed]
- Reuter, S.; Gupta, S.C.; Chaturvedi, M.M.; Aggarwal, B.B. Oxidative stress, inflammation, and cancer: How are they linked? Free Radic. Biol. Med. 2010, 49, 1603–1616. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Li, H.; Yang, S. Role of oxygen free radicals in the proliferation of myofibroblasts induced by AngII. Acta Pharm. Sin. B 2013, 3, 32–37. [Google Scholar] [CrossRef][Green Version]
- Kinnula, V.L.; Fattman, C.L.; Tan, R.J.; Oury, T.D. Oxidative Stress in Pulmonary Fibrosis. Am. J. Respir. Crit. Care Med. 2005, 172, 417–422. [Google Scholar] [CrossRef]
- Fukushima, K.; Satoh, T.; Kida, H.; Kumanogoh, A. Revisiting Cell Death Responses in Fibrotic Lung Disease: Crosstalk between Structured and Non-Structured Cells. Diagnostic 2020, 10, 504. [Google Scholar] [CrossRef]
- Nájera-Martínez, M.; García-Latorre, E.A.; Reyes-Maldonado, E.; Domínguez-López, M.L.; Vega-López, A. Halomethane-induced cytotoxicity and cell proliferation in human lung MRC-5 fibroblasts and NL20-TA epithelial cells. Inh. Toxicol. 2012, 24, 762–773. [Google Scholar] [CrossRef]
- Htwe, S.S.; Harrington, H.; Knox, A.; Rose, F.; Aylott, J.; Haycock, J.W.; Ghaemmaghami, A.M. Investigating NF-κB signaling in lung fibroblasts in 2D and 3D culture systems. Respir. Res. 2015, 16, 144. [Google Scholar] [CrossRef]
- Thompson, J.E.; Phillips, R.J.; Erdjument-Bromage, H.; Tempst, P.; Ghosh, S.I. kappa B-beta regulates the persistent response in a biphasic activation of NF-kappa B. Cell 1995, 80, 573–582. [Google Scholar] [CrossRef]
- Hayden, M.S.; Ghosh, S. Shared principles in NF-kappaB signaling. Cell 2008, 132, 344–362. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, S.; Dass, F.P.J. Non-canonical pathway network modelling and ubiquitination site prediction through homology modelling of NF-κB. Gene 2016, 581, 48–56. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Zhang, L.; Joo, D.; Sun, S.C. NF-κB signaling in inflammation. Signal Transduct. Target. Ther. 2017, 2, 17023. [Google Scholar] [CrossRef] [PubMed]
- Huxford, T.; Mishler, D.; Phelps, C.B.; Huang, D.B.; Sengchanthalangsy, L.L.; Reeves, R.; Hughes, C.A.; Elizabeth AKomives, E.A.; Ghosh, G. Solvent Exposed Non-contacting Amino Acids Play a Critical Role in NF-kB/IkBa Complex Formation. J. Mol. Biol. 2002, 324, 587–597. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.J.; Parent, L.; Maniatis, T. Site-specific phosphorylation of IκB by a novel ubiquitination-dependent protein kinase activity. Cell 1996, 84, 853–862. [Google Scholar] [CrossRef]
- Whiteside, S.T.; Epinat, J.C.; Rice, N.R.; Israel, A. I kappa B epsilon, a novel member of the I kappa B family, controls RelA and cRel NF-kappa B activity. EMBO J. 1997, 16, 1413–1426. [Google Scholar] [CrossRef]
- Christian, F.; Smith, E.; Carmody, R. The Regulation of NF-κB Subunits by Phosphorylation. Cells 2016, 5, 12. [Google Scholar] [CrossRef]
- Agency for Toxic Substances and Disease Registry. Toxicological Profile for Methylene Chloride; U.S. Department of Health and Human Services, Public Health Service: Washington, DC, USA, 2000. Available online: https://www.atsdr.cdc.gov/ToxProfiles/tp14.pdf (accessed on 15 October 2024).
- Gad, S.C. Trihalomethanes. Encyclopedia of Toxicology, 3rd ed.; Elsevier: Amsterdam, The Netherlands, 2014; pp. 849–885. [Google Scholar] [CrossRef]
- Dekant, W.; Jean, P.; Arts, J. Evaluation of the carcinogenicity of dichloromethane in rats, mice, hamsters and humans. Regul. Toxicol. Pharmacol. 2021, 120, 104858. [Google Scholar] [CrossRef]
- Agency for Toxic Substances and Disease Registry. Toxicological profile for Bromodichloromethane; U.S. Department of Health and Human Services, Public Health Service: Washington, DC, USA; Elsevier: Amsterdam, The Netherlands, 2020. Available online: https://www.atsdr.cdc.gov/ToxProfiles/tp129.pdf (accessed on 15 October 2024).
- Sun, X.F.; Zhang, H. NFKB and NFKBI polymorphisms in relation to susceptibility of tumour and other diseases. Histol. Histopathol. 2007, 22, 1387–1398. [Google Scholar] [CrossRef]
- Uraga-Tovar, D.I.; Domíguez-López, M.L.; Madera-Sandoval, R.L.; Nájera-Martínez, M.; García-Latorre, E.; Vega-López, A. Generation of oxyradicals O2• and H2O2), mitochondrial activity and induction of apoptosis of PBMC of Cyprinus carpio carpio treated in vivo with halomethanes and with recombinant HSP60 kDa and with LPS of Klebsiella pneumoniae. Immunopharmacol. Immunotoxicol. 2014, 36, 329–340. [Google Scholar] [CrossRef]
- Dzul-Caamal, R.; Salazar-Coria, L.; Olivares-Rubio, H.F.; Rocha-Gómez, M.A.; Girón-Pérez, M.I.; Vega-López, A. Oxidative stress response in the skin mucus layer of Goodea gracilis (Hubbs and Turner, 1939) exposed to crude oil: A non-invasive approach. Comp. Biochem. Physiol. Part A Mol. Integr. Physiol. 2016, 200, 9–20. [Google Scholar] [CrossRef] [PubMed]
- Buege, J.A.; Aust, S.D. Microsomal lipid peroxidation. Methods Enzymol. 1978, 52, 302–310. [Google Scholar] [CrossRef] [PubMed]
- Misra, H.P.; Fridovich, I. The role of superoxide dismutase anion in the autooxidation of epinephrine and a simple assay for superoxide dismutase. J. Biol. Chem. 1972, 247, 3170–3175. [Google Scholar] [CrossRef] [PubMed]
- Radi, R.; Turrens, J.F.; Chang, L.Y.; Bush, K.M.; Crapo, J.D.; Freeman, B.A. Detection of catalase in rat heart mitochondria. J. Biol. Chem. 1991, 266, 22028–22034. [Google Scholar] [CrossRef] [PubMed]
- Lei, X.G.; Evenson, J.K.; Thompson, K.M.; Sunde, R.A. Glutathione peroxidase and phospholipid hydroperoxide glutathione peroxidase are differentially regulated in rats by dietary selenium. J. Nutr. 1995, 125, 1438–1446. [Google Scholar] [CrossRef] [PubMed]
- Mackerell, A.D., Jr.; Feig, M.; Brooks, C.L. 3rd. Extending the treatment of backbone energetics in protein force fields: Limitations of gas-phase quantum mechanics in reproducing protein conformational distributions in molecular dynamics simulations. J. Comput. Chem. 2004, 25, 1400–1415. [Google Scholar] [CrossRef]
- Phillips, J.C.; Hardy, D.J.; Maia, J.D.C.; Stone, J.E.; Ribeiro, J.V.; Bernardi, R.C.; Buch, R.; Fiorin, G.; Hénin, J.; Jiang, W.; et al. Scalable molecular dynamics on CPU and GPU architectures with NAMD. J. Chem. Phys. 2020, 153, 044130. [Google Scholar] [CrossRef]
- MacKerell, A.D., Jr.; Bashford, D.; Bellott, M.L.; Dunbrack, R.L., Jr.; Evanseck, J.D.; Field, M.J.; Fischer, S.; Gao, J.; Guo, H.; Ha, S.; et al. All-atom empirical potential for molecular modeling and dynamics studies of proteins. J. Phys. Chem. B 1998, 102, 3586–3616. [Google Scholar] [CrossRef]
- Jorgensen, W.L.; Chandrasekhar, J.; Madura, J.D. Comparison of simple potential functions for simulating liquid water. J. Chem. Phys. 1983, 79, 926–935. [Google Scholar] [CrossRef]
- Grubmüller, H.; Heller, H.; Windemuth, A.; Schulten, K. Generalized Verlet Algorithm for Efficient Molecular Dynamics Simulations with Long-range Interactions. Mol. Simul. 1991, 6, 121–142. [Google Scholar] [CrossRef]
- Schlick, T.; Skeel, R.D.; Brunger, A.T.; Kalé, L.V.; Board, J.A.; Hermans, J.; Schulten, K. Algorithmic challenges in computational molecular biophysics. J. Comput. Phys. 1999, 151, 9–48. [Google Scholar] [CrossRef]
- Brunger, A.T. X-PLOR Version 3.1, A System for X-ray Crystallography and NMR; Yale University: New Haven, CT, USA, 1992; 405p, ISBN 9780300054026. [Google Scholar]
- Hsu, C.C.; Lien, J.C.; Chang, C.W.; Chang, C.H.; Kuo, S.C.; Huang, T.F. Yuwen02f1 suppresses LPS-induced endotoxemia and adjuvant-induced arthritis primarily through blockade of ROS formation, NFkB and MAPK activation. Biochem. Pharmacol. 2013, 85, 385–395. [Google Scholar] [CrossRef] [PubMed]
- Tkaczyk, J.; Vízek, M. Oxidative Stress in the Lung Tissue—Sources of Reactive Oxygen Species and Antioxidant Defence. Prague Med. Rep. 2007, 108, 105–114. [Google Scholar] [PubMed]
- Rimal, B.; Greenberg, A.K.; Rom, W.N. Basic pathogenetic mechanisms in silicosis: Current understanding. Curr. Opin. Pulm. Med. 2005, 11, 169–173. [Google Scholar] [CrossRef] [PubMed]
- Mittal, M.; Siddiqui, M.R.; Tran, K.; Reddy, S.P.; Malik, A.B. Reactive oxygen species in inflammation and tissue injury. Antioxid. Redox Signal. 2014, 20, 1126–1167. [Google Scholar] [CrossRef]
- Becklake, M.R. Occupational exposures: Evidence for a causal association with chronic obstructive pulmonary disease. Am. Rev. Respir. Dis. 1989, 140, S85–S91. [Google Scholar] [CrossRef]
- Omland, O.; Würtz, E.T.; Aasen, T.B.; Blanc, P.; Brisman, J.; Miller, M.R.; Pederson, O.F.; Schlünssen, V.; Sigsgaard, T.; Ulrik, C.S.; et al. Occupational chronic obstructive pulmonary disease: A systematic literature review. Scand. J. Work Environ. Health 2011, 40, 19–35. [Google Scholar] [CrossRef]
- Mikolka, P.; Kosutova, P.; Kolomaznik, M.; Nemcova, N.; Hanusrichterova, J.; Curstedt, T.; Johansson, J.; Calkovska, A. The Synthetic Surfactant CHF5633 Restores Lung Function and Lung Architecture in Severe Acute Respiratory Distress Syndrome in Adult Rabbits. Lung 2024, 202, 299–315. [Google Scholar] [CrossRef]
- Di, Y.P.; Kuhn, J.M.; Mangoni, M.L. Lung antimicrobial proteins and peptides: From host defense to therapeutic strategies. Physiol. Rev. 2024, 104, 1643–1677. [Google Scholar] [CrossRef]
- JLi, J.; Song, H.; Luo, T.; Cao, Y.; Zhang, L.; Zhao, Q.; Li, Z.; Hu, X.; Gu, J.; Tian, S. Exposure to O3 and NO2 on the interfacial chemistry of the pulmonary surfactant and the mechanism of lung oxidative damage. Chemosphere 2024, 362, 142669. [Google Scholar] [CrossRef]
- Xiang, Y.; Xu, H. Occurrence, formation, and proteins perturbation of disinfection byproducts in indoor air resulting from chlorine disinfection. Chemosphere 2023, 343, 140182. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.; Zhang, K.; Xiao, T.; Yang, J.; Sun, Y.; Yang, C.; Dai, H.; Yang, W. Exposure to disinfection by-products and risk of cancer: A systematic review and dose-response meta-analysis. Ecotoxicol. Environ. Saf. 2024, 270, 115925. [Google Scholar] [CrossRef] [PubMed]
- US Environmental Protection Agency. Safe drinking water act (SDWA). 2023. Available online: https://www.epa.gov/sdwa (accessed on 15 October 2024).
- Gabriel, M.F.; Felgueiras, F.; Mourão, Z.; Fernandes, E.O. Assessment of the air quality in 20 public indoor swimming pools located in the Northern Region of Portugal. Environ. Int. 2019, 133, 105274. [Google Scholar] [CrossRef] [PubMed]
- Melnick, R.L.; Kohn, M.C.; Dunnick, J.K. Regenerative hyperplasia is not required for liver tumor induction in female B6C3F1 mice exposed to trihalomethanes. Toxicol. Appl. Pharmacol. 1998, 148, 137–147. [Google Scholar] [CrossRef] [PubMed]
- Vega-López, A.; Carrillo-Morales, C.I.; Olivares-Rubio, H.F. Evidence of bioactivation of halomethanes and its relation to oxidative stress response in Chirostoma riojai, an endangered fish from a polluted lake in Mexico. Arch. Environ. Cont. Toxicol. 2012, 62, 479–493. [Google Scholar] [CrossRef] [PubMed]
- Dzul-Caamal, R.; Olivares-Rubio, H.F.; López-Tapia, P.; Vega-López, A. Pro-oxidant and antioxidant response elicited by CH2Cl2, CHCl3 and BrCHCl2 in Goodea gracilis using non-invasive methods. Comp. Bioch. Physiol. A Mol. Integr. Physiol. 2013, 165, 515–527. [Google Scholar] [CrossRef]
- Dekant, W.; Vamvakas, S. Glutathione-dependent bioactivation of xenobiotics. Xenobiotica 1993, 23, 873–887. [Google Scholar] [CrossRef]
- Zhang, H.; Zhang, J.; Zhu, Y. In vitro investigations for the QSAR mechanism of lymphocytes apoptosis induced by substituted aromatic toxicants. Fish Shellfish Immunol. 2008, 25, 710–717. [Google Scholar] [CrossRef]
- Crapo, J.D.; Tierney, D.F. Superoxide dismutase and pulmonary oxygen toxicity. Am. J. Physiol. 1974, 226, 1401–1407. [Google Scholar] [CrossRef]
- Birben, E.; Sahiner, E.M.; Sackesen, C.; Erzurum, S.; Kalayci, O. Oxidative Stress and Antioxidant Defense. World Allergy Org. J. 2012, 5, 9–19. [Google Scholar] [CrossRef]
- Hermes-Lima, M. Oxygen in biology and biochemistry: Role free radicals. In Functional Metabolism: Regulation and Adaptation; Storey, K.B., Ed.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2004; pp. 319–368. [Google Scholar] [CrossRef]
- Finkel, T.; Holbrook, N.J. Oxidants, oxidative stress and the biology of ageing. Nature 2000, 408, 239–247. [Google Scholar] [CrossRef] [PubMed]
- Klaunig, J.E.; Kamendulis, L.M. The role of oxidative stress in carcinogenesis. Ann. Rev. Pharmacol. Toxicol. 2004, 44, 239–267. [Google Scholar] [CrossRef] [PubMed]
- Gao, F.; Kinnula, L.V.; Marjukka Myllärniemi, M.; Oury, D.T. Extracellular Superoxide Dismutase in Pulmonary Fibrosis. Antioxid. Redox Signal. 2008, 10, 343–354. [Google Scholar] [CrossRef] [PubMed]
- Brand, M.D. Mitochondrial generation of superoxide and hydrogen peroxide as the source of mitochondrial redox signaling. Free Radic. Biol. Med. 2016, 100, 14–31. [Google Scholar] [CrossRef] [PubMed]
- McCord, J.M.; Fridovich, I. Superoxide dismutase. An enzymic function for erythrocuprein (hemocuprein). J. Biol. Chem. 1969, 244, 6049–6055. [Google Scholar] [CrossRef]
- Sauer, H.; Rahimi, G.; Hescheler, J.; Wartenberg, M. Role of reactive oxygen species and phosphatidylinositol 3-kinase in cardiomyocyte differentiation of embryonic stem cells. FEBS Lett. 2000, 476, 218–223. [Google Scholar] [CrossRef]
- Foreman, J.; Demidchik, V.; Bothwell, J.H.; Mylona, P.; Miedema, H.; Torres, M.A.; Linstead, P.; Costa, S.; Brownlee, C.; Jones, J.D. Reactive oxygen species produced by NADPH oxidase regulate plant cell growth. Nature 2003, 422, 442–446. [Google Scholar] [CrossRef]
- Geiszt, M.; Leto, T.L. The Nox family of NAD(P)H oxidases: Host defense and beyond. J. Biol. Chem. 2004, 279, 51715–51718. [Google Scholar] [CrossRef]
- Cai, H. Hydrogen peroxide regulation of endothelial function: Origins, mechanisms, and consequences. Cardiovasc. Res. 2005, 68, 26–36. [Google Scholar] [CrossRef]
- Li, J.; Stouffs, M.; Serrander, L.; Banfi, B.; Bettiol, E.; Charnay, Y.; Steger, K.; Krause, K.H.; Jaconi, M.E. The NADPH oxidase NOX4 drives cardiac differentiation: Role in regulating cardiac transcription factors and MAP kinase activation. Mol. Biol. Cell. 2006, 17, 3978–3988. [Google Scholar] [CrossRef]
- Cantin, A.M.; North, S.L.; Hubbard, R.C.; Crystal, R.G. Normal alveolar epithelial lining fluid contains high levels of glutathione. J. Appl. Physiol. 1987, 63, 152–157. [Google Scholar] [CrossRef] [PubMed]
- Ayala, A.; Muñoz, M.F.; Argüelles, S. Lipid Peroxidation: Production, Metabolism, and Signaling Mechanisms of Malondialdehyde and 4-Hydroxy-2-Nonenal. Oxidative Medicine and Cellular Longevity. Oxid. Med. Cell. Longev. 2014, 2014, 360438. [Google Scholar] [CrossRef] [PubMed]
- Kornbrust, D.J.; Mavis, R.D. Relative susceptibility of microsomes from lung, heart, liver, kidney, brain and testes to lipid peroxidation: Correlation with vitamin E content. Lipids 1980, 15, 315–322. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, W.V.; Lu, J. Regulation of early lung morphogenesis: Questions, facts and controversies. Development 2006, 133, 1611–1624. [Google Scholar] [CrossRef]
- Cardoso, W.V.; Whitsett, J.A. Resident cellular components of the lung: Developmental aspects. Proc. Am. Thorac. Soc. 2008, 5, 767–771. [Google Scholar] [CrossRef]
- Morrisey, E.E.; Hogan, B.L. Preparing for the first breath: Genetic and cellular mechanisms in lung development. Dev. Cell. 2010, 18, 8–23. [Google Scholar] [CrossRef]
- O’shea, J.M.; Perkins, N.D. Regulation of the RelA (p65) transactivation domain. Biochem. Soc. Trans. 2008, 36, 603–608. [Google Scholar] [CrossRef]
- Cramer, P.; Müller, C.W. A firm hand on NFkappaB: Structures of the IkappaBalpha-NFkappaB complex. Structure 1999, 7, R1–R6. [Google Scholar] [CrossRef][Green Version]
- Li, X.; Stark, G.R. NFkappaB-dependent signaling pathways. Exp. Hematol. 2002, 30, 285–296. [Google Scholar] [CrossRef]
- Zhou, Z.; Wang, M.; Zhao, J.; Wang, L.; Gao, Y.; Zhang, H.; Liu, R.; Song, L. increased transcriptional response and translocation of a Rel/NF-κB homologue in scallop Chlamys farreri during the immune stimulation. Fish Shellfish Immunol. 2013, 34, 1209–1215. [Google Scholar] [CrossRef]
- Du, R.H.; Tan, J.; Yan, N.; Wang, L.; Qiao, C.; Ding, J.H.; Lu, M.; Hu, G. Kir6.2 knockout aggravates lipopolysaccharide-induced mouse liver injury via enhancing NLRP3 inflammasome activation. J. Gastroenterol. 2014, 49, 727–736. [Google Scholar] [CrossRef] [PubMed]
- He, J.Y.; Li, P.H.; Huang, X.; Sun, Y.H.; He, X.P.; Huang, W.; Yu, Z.H.; Sun, H.Y. Molecular cloning, expression and functional analysis of NF-kB1 p105 from sea cucumber Holothuria leucospilota. Dev. Comp. Immunol. 2021, 114, 103801. [Google Scholar] [CrossRef] [PubMed]
- Huang, D.-B.; Huxford, T.; Chen, Y.-Q.; Ghosh, G. The role of DNA in the mechanism of NFkB dimer formation: Crystal structures of the dimerization domains of the p50 and p65 subunits. Structure 1997, 5, 1427–1436. [Google Scholar] [CrossRef] [PubMed]
- Vermeulen, L.; De Wilde, G.; Notebaert, S.; Vanden Berghe, W.; Haegeman, G. Regulation of the transcriptional activity of the nuclear factor-κB p65 subunit. Bioch. Pharmacol. 2002, 64, 963–970. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, M.D.; Harrison, S.C. Structure of an IkBa/NF-kB Complex. Cell 1998, 95, 749–758. [Google Scholar] [CrossRef]
- Wu, C.; Ghosh, S. Differential phosphorylation of the signal-responsive domain of I kappa B alpha and I kappa B beta by I kappa B kinases. J. Biol. Chem. 2003, 278, 31980–31987. [Google Scholar] [CrossRef]
- Kanarek, N.; Ben-Neriah, Y. Regulation of NF-κB by ubiquitination and degradation of the IκBs. Immunol. Rev. 2012, 246, 77–94. [Google Scholar] [CrossRef]
- Anrather, J.; Racchumi, G.; Iadecola, C. cis-Acting Element-specific Transcriptional Activity of Differentially Phosphorylated Nuclear Factor-κB. J. Biol. Chem. 2004, 280, 244–252. [Google Scholar] [CrossRef]
- Cramer, P.; Larson, C.J.; Verdine, G.L.; Müller, C.W. Structure of the human NF-kappaB p52 homodimer-DNA complex at 2.1 A resolution. EMBO J. 1997, 16, 7078–7090. [Google Scholar] [CrossRef]
- Milanovic, M.; Kracht, M.; Schmitz, M.L. The cytokine-induced conformational switch of nuclear factor κB p65 is mediated by p65 phosphorylation. Bioch. J. 2014, 457, 401–413. [Google Scholar] [CrossRef]
- Schwartz, J.L.; Antoniades, D.Z.; Zhao, S. Molecular and biochemical reprogramming of oncogenesis through the activity of prooxidants and antioxidants. Ann. N. Y. Acad. Sci. 1993, 686, 262–278. [Google Scholar] [CrossRef] [PubMed]
- Dominici, S.; Visvikis, A.; Pieri, L.; Paolicchi, A.; Valentini, M.A.; Comporti, M.; Pompella, A. Redox modulation of NF-kappaB nuclear translocation and DNA binding in metastatic melanoma. The role of endogenous and gamma-glutamyl transferase-dependent oxidative stress. Tumori 2003, 89, 426–433. [Google Scholar] [CrossRef] [PubMed]
- Yao, H.; Yang, S.R.; Kode, A.; Rajendrasozhan, S.; Caito, S.; Adenuga, D.; Henry, R.; Edirisinghe, I.; Rahman, I. Redox regulation of lung inflammation: Role of NADPH oxidase and NF-kappaB signalling. Biochem. Soc. Trans. 2007, 5 Pt 35, 1151–1155. [Google Scholar] [CrossRef] [PubMed]
- Zhong, Z.M.; Bai, L.; Chen, J.T. Advanced oxidation protein products inhibit proliferation and differentiation of rat osteoblast-like cells via NF-kappaB pathway. Cell. Physiol. Biochem. 2009, 24, 105–114. [Google Scholar] [CrossRef] [PubMed]
- Ali, F.; Sultana, S. Repeated short-term stress synergizes the ROS signalling through up regulation of NFkB and iNOS expression induced due to combined exposure of trichloroethylene and UVB rays. Mol. Cell. Biochem. 2012, 360, 133–145. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Liu, Y.J.; Lv, G.; Zhang, D.L.; Zhang, L.; Li, D. Propofol protects against hydrogen peroxide-induced apoptosis in cardiac H9c2 cells is associated with the NF-κB activation and PUMA expression. Eur. Rev. Med. Pharmacol. Sci. 2014, 18, 1517–1524. [Google Scholar] [PubMed]
- Fenga, C.; Gangemi, S.; Giambò, F.; Tsitsimpikou, C.; Golokhvast, K.; Tsatsakis, A.; Costa, C. Low-dose occupational exposure to benzene and signal transduction pathways involved in the regulation of cellular response to oxidative stress. Life Sci. 2016, 147, 67–70. [Google Scholar] [CrossRef]
- Hu, W.; Shi, L.; Li, M.Y.; Zhou, P.H.; Qiu, B.; Yin, K.; Zhang, H.H.; Gao, Y.; Kang, R.; Qin, S.L.; et al. Adrenomedullin protects Leydig cells against lipopolysaccharide-induced oxidative stress and inflammatory reaction via MAPK/NF-κB signalling pathways. Sci. Rep. 2017, 7, 16479. [Google Scholar] [CrossRef]
- Liu, L.; Zuo, Z.; Lu, S.; Liu, A.; Liu, X. Naringin attenuates diabetic retinopathy by inhibiting inflammation, oxidative stress and NF-κB activation in vivo and in vitro. Iran. J. Basic Med. Sci. 2017, 20, 813–821. [Google Scholar] [CrossRef]
- He, J.; Zhou, D.; Yan, B. Eriocitrin alleviates oxidative stress and inflammatory response in cerebral ischemia reperfusion rats by regulating phosphorylation levels of Nrf2/NQO-1/HO-1/NF-κB p65 proteins. Ann. Transl. Med. 2020, 8, 757. [Google Scholar] [CrossRef]
- Li, Q.; Sun, Y.; Liu, B.; Li, J.; Hao, X.; Ge, W.; Zhang, X.; Bao, S.; Gong, J.; Jiang, Z.; et al. ACT001 modulates the NF-κB/MnSOD/ROS axis by targeting IKKβ to inhibit glioblastoma cell growth. J. Mol. Med. 2020, 98, 263–277. [Google Scholar] [CrossRef] [PubMed]
- Kamata, H.; Manabe, T.; Oka, S.; Kamata, K.; Hirata, H. Hydrogen peroxide activates IkappaB kinases through phosphorylation of serine residues in the activation loops. FEBS Lett. 2002, 519, 231–237. [Google Scholar] [CrossRef] [PubMed]
- Oliveira-Marques, V.; Marinho, H.S.; Cyrne, L.; Antunes, F. Role of hydrogen peroxide in NF-B activation: From inducer to modulator. Antioxid. Redox Signal. 2009, 11, 2223–2243. [Google Scholar] [CrossRef] [PubMed]
- Dumont, J.; Euwart, D.; Mei, B.; Estes, S.; Kshirsagar, R. Human cell lines for biopharmaceutical manufacturing: History, status, and future perspectives. Crit. Rev. Biotechnol. 2015, 36, 1110–1122. [Google Scholar] [CrossRef]
- Zuchowska, A.; Kwiatkowski, P.; Jastrzebska, E.; Chudy, M.; Dybko, A.; Brzozka, Z. Adhesion of MRC-5 and A549 cells on poly(dimethylsiloxane) surface modified by proteins. Electrophoresis 2015, 37, 536–544. [Google Scholar] [CrossRef]
- Lekovic, M.H.; Drekovic, N.E.; Granica, N.D.; Mahmutovic, E.H.; Djordjevic, N.Z. Extremely low-frequency electromagnetic field induces a change in proliferative capacity and redox homeostasis of human lung fibroblast cell line MRC-5. Environ. Sci. Pollut. Res. 2020, 27, 39466–39473. [Google Scholar] [CrossRef]
- Liu, X.; Liu, H.; Zhai, Y.; Li, Y.; Zhu, X.; Zhang, W. Laminarin protects against hydrogen peroxide-induced oxidative damage in MRC-5 cells possibly via regulating NRF2. PeerJ 2017, 5, e3642. [Google Scholar] [CrossRef]
- Wu, F.; Fan, J.; He, Y.; Xiong, A.; Yu, J.; Li, Y.; Zhang, Y.; Zhao, W.; Zhou, F.; Li, W.; et al. Single-cell profiling of tumor heterogeneity and the microenvironment in advanced non-small cell lung cancer. Nat. Commun. 2021, 12, 2540. [Google Scholar] [CrossRef]



| R, p | R, p | R, p | R, p | R, p | R, p | |
|---|---|---|---|---|---|---|
| CH2Cl2 | ||||||
| H2O2 | TBARS | SOD | CAT | GPx | NF-κB | |
| O2• | 0.590, <0.001 | 0.728, <0.001 | 0.596, <0.001 | −0.533, <0.01 | ||
| H2O2 | 0.736, <0.001 | 0.541, <0.01 | ||||
| TBARS | 0.408, <0.05 | −0.471, <0.01 | ||||
| SOD | 0.584, <0.001 | |||||
| CHCl3 | ||||||
| H2O2 | TBARS | SOD | CAT | GPx | NF-κB | |
| O2• | 0.884, <0.001 | 0.504, <0.01 | −0.611, <0.001 | |||
| H2O2 | 0.465, <0.05 | 0.592, <0.001 | −0.672, <0.001 | |||
| TBARS | 0.771, <0.001 | 0.514, <0.01 | ||||
| BrCHCl2 | ||||||
| H2O2 | TBARS | SOD | CAT | GPx | NF-κB | |
| O2• | 0.915, <0.001 | 0.418, <0.05 | 0.539, <0.01 | 0.682, <0.001 | 0.407, <0.05 | |
| H2O2 | 0.404, <0.05 | 0.396, <0.05 | 0.653, <0.001 | 0.451, <0.05 | ||
| SOD | 0.536, <0.01 | |||||
| CAT | −0.406, <0.05 | |||||
| Compound | SCF (a.u.) | ΔH (kcal/mol) | ΔE(eV) | ΔG (kcal/mol) |
|---|---|---|---|---|
| CHCl3 | −46.4 | −23.6 | 11.6 | −3.5 |
| BrCHCl2 | −23.9 | −17.9 | 12.5 | −3.3 |
| O2• | −24.4 | −35.3 | 0.5 | −3.6 |
| H2O2 | −45 | −15.5 | 0.3 | −3.6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nájera-Martínez, M.; Lara-Vega, I.; Avilez-Alvarado, J.; Pagadala, N.S.; Dzul-Caamal, R.; Domínguez-López, M.L.; Tuszynski, J.; Vega-López, A. The Generation of ROS by Exposure to Trihalomethanes Promotes the IκBα/NF-κB/p65 Complex Dissociation in Human Lung Fibroblast. Biomedicines 2024, 12, 2399. https://doi.org/10.3390/biomedicines12102399
Nájera-Martínez M, Lara-Vega I, Avilez-Alvarado J, Pagadala NS, Dzul-Caamal R, Domínguez-López ML, Tuszynski J, Vega-López A. The Generation of ROS by Exposure to Trihalomethanes Promotes the IκBα/NF-κB/p65 Complex Dissociation in Human Lung Fibroblast. Biomedicines. 2024; 12(10):2399. https://doi.org/10.3390/biomedicines12102399
Chicago/Turabian StyleNájera-Martínez, Minerva, Israel Lara-Vega, Jhonatan Avilez-Alvarado, Nataraj S. Pagadala, Ricardo Dzul-Caamal, María Lilia Domínguez-López, Jack Tuszynski, and Armando Vega-López. 2024. "The Generation of ROS by Exposure to Trihalomethanes Promotes the IκBα/NF-κB/p65 Complex Dissociation in Human Lung Fibroblast" Biomedicines 12, no. 10: 2399. https://doi.org/10.3390/biomedicines12102399
APA StyleNájera-Martínez, M., Lara-Vega, I., Avilez-Alvarado, J., Pagadala, N. S., Dzul-Caamal, R., Domínguez-López, M. L., Tuszynski, J., & Vega-López, A. (2024). The Generation of ROS by Exposure to Trihalomethanes Promotes the IκBα/NF-κB/p65 Complex Dissociation in Human Lung Fibroblast. Biomedicines, 12(10), 2399. https://doi.org/10.3390/biomedicines12102399









