Abstract
(1) Background: Malaria remains a significant global public health issue. Since parasites quickly became resistant to most of the available antimalarial drugs, treatment effectiveness must be constantly monitored. In Brazil, up to 10% of cases of vivax malaria resistant to chloroquine (CQ) have been registered. Unlike P. falciparum, there are no definitive molecular markers for the chemoresistance of P. vivax to CQ. This work aimed to investigate whether polymorphisms in the pvcrt-o and pvmdr1 genes could be used as markers for assessing its resistance to CQ. (2) Methods: A total of 130 samples from P. vivax malaria cases with no clinical and/or parasitological evidence of CQ resistance were studied through polymerase chain reaction for gene amplification followed by target DNA sequencing. (3) Results: In the pvcrt-o exons, the K10 insert was present in 14% of the isolates. Regarding pvmdr1, T958M and F1076L haplotypes showed frequencies of 95% and 3%, respectively, while the SNP Y976F was not detected. (4) Conclusions: Since K10-pvcrt-o and F1076L/T958M-pvmdr1 polymorphisms were detected in samples from patients who responded well to CQ treatment, it can be concluded that mutations in these genes do not seem to have a potential for association with the phenotype of CQ resistance.
1. Introduction
Malaria is a major important public health problem worldwide. According to the World Malaria Report from the World Health Organization (WHO), there were 247 million new cases and 619 thousand malaria-related deaths in 2021 [1]. Plasmodium vivax is the most widely distributed species causing most malaria cases in Asia and South America [2,3]. Since 2007, Brazil has observed a stable incidence rate of malaria cases, with P. vivax accounting for about 80% of cases. This trend continued in 2022. The country recorded around 129,000 malaria cases, of which around 83% were attributable to P. vivax and 16%, to P. falciparum [4]. In the last 60 years, the combination of chloroquine (CQ) and primaquine (PQ) has been used in Latin America to radically cure P. vivax, i.e., eradicate the blood forms and hepatic hypnozoites [5]. However, emerging resistance to antimalarial drugs may threaten malaria control programs [1].
The first report of P. vivax resistance to chloroquine (CQR) in Papua New Guinea dates from 1989 [6], 30 years after resistance reports for P. falciparum [7,8]. In Brazil, the first cases of P. vivax resistant to CQ were described in Manaus, Amazonas, in 1999 [9]. This timeline reflects the emergence of chloroquine resistance in P. vivax occurring later than in P. falciparum. Since then, studies have reported a 10% prevalence of CQR [10] and a recurrence or reemergence of P. vivax in 5.2% of cases in the same region [11], threatening current international efforts to control and eliminate malaria [1]. Given the emerging risk of drug resistance, drug efficacy monitoring studies using molecular markers represent an important tool for refining CQR surveillance and validating potential molecular markers associated with the P. vivax resistance phenotype through mutated single nucleotide polymorphisms (SNPs) in related genes [12].
Currently, the mechanisms of resistance of P. vivax to antimalarial drugs are still unclear due to the lack of continuous in vitro culture systems and the possible involvement of multigenic loci [13]. The P. vivax multidrug resistance 1 gene (pvmdr1) and the chloroquine resistance transporter gene (pvcrt-o) are orthologous to two genes described in P. falciparum, the multidrug resistance 1 gene (pfmdr1) and the chloroquine resistance transporter gene (pfcrt), which have been identified as potential markers for CQR in P. vivax [14].
The pvcrt-o gene, described about 20 years ago [15], emerged as a candidate marker of drug resistance and in contrast to pfcrt, only a few SNPs (~10) have been described in pvcrt-o, and most of them were related but occurring at low frequencies [16]. Although the sequence polymorphism in the pvcrt-o locus is relatively limited, a lysine (AAG) insertion in the first exon (amino acid 10), originally discovered in Southeast Asian strains, has been found to be associated with a significant reduction in chloroquine (CQ)’s half-maximal inhibitory concentration (IC50) [13,17,18]. Thenceforth, studies have demonstrated the presence of the K10 insertion in parasites from Southeast Asia and South America [16,19,20].
In the context of pvmdr1, this gene was identified in 2005 and, due to its strong sequence similarity to pfmdr1, became one of the most important candidate genes investigated in drug susceptibility studies of P. vivax [16]. Since then, several SNPs have been identified as potential molecular markers for CQ resistance in P. vivax, including T958M, Y976F and F1076L, which are non-synonymous amino acid mutations associated with resistance to CQ [13,14,20,21]. Judging by their protein sequence, the 3 pvmdr1 mutations are located in 9 to 11 domains of the hydrophobic transmembrane [22]. The presence of these polymorphisms at codons Y976F and F1076L was registered in malaria-endemic areas where CQ was being used as the first-line antimalarial drug [17,23,24,25]. However, the possibility has been raised that the presence of these two mutations together would be required for the re-emergence of P. vivax resistance to CQ [26]. While the Y976F and F1076L polymorphisms are widely distributed in Latin America [27], in Brazil, the increased expression of pvcrt-o and pvmdr1 has been associated with P. vivax resistance to CQ [20].
Considering that knowledge of CQ-chemoresistant P. vivax circulating parasites in Brazilian endemic areas is crucial for predicting the spread of resistant phenotypes and the need for the introduction of alternative therapies, the aim of this study was to investigate the polymorphisms in the pvcrt-o and pvmdr1 genes to identify their potential predictive role of the CQR phenotype in P. vivax samples from Brazilian endemic areas.
2. Materials and Methods
2.1. Location of the Study and Samples Collected
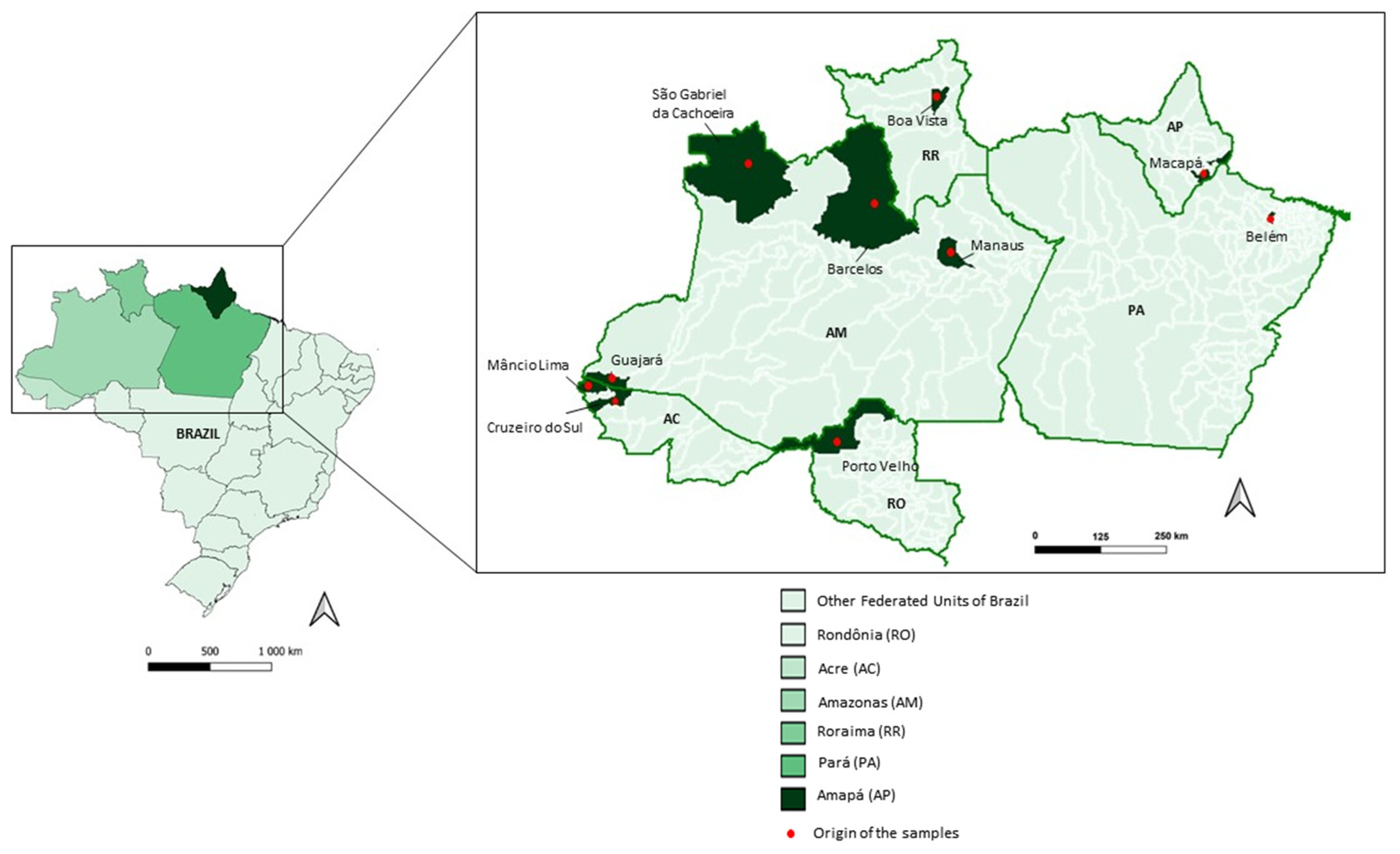
Samples were collected from January 2018 to August 2022, from P. vivax-infected patients in six Amazonian states (Acre, Amazonas, Amapá, Pará, Rondônia and Roraima). Patients were treated and followed clinically and with laboratory testing to verify if they were cured after chemotherapy treatment at the Outpatient Clinic for Acute Febrile Syndromes/Instituto Nacional de Infectologia (INI), which is part of the Reference Center for Malaria Research, Diagnosis and Training—CPD-Mal/Fundação Oswaldo Cruz (FIOCRUZ)/Rio de Janeiro of Extra-Amazonian (22°54′ S 43°12′ W). The treatment adopted for the patients was recommended by the National Program of Malaria Control (PNCM), which comprised the administration of a combination of CQ for 3 days (10 milligrams (mg)/kilogram (kg) on day 1 and 7.5 mg/kg on days 2 and 3) and PQ for 7 days (0.5 mg/kg/day). If patients returned, they were evaluated on days 0, 1, 2, 3, 7, 14, 28 and 42 and in case of symptoms, at any time during the follow-up period.
Besides at CPD-Mal, blood samples were also collected in Manaus (3.1190° S, 60.0217° W), the capital of the Amazon state, at the Fundação de Medicina Tropical Doutor Heitor Vieira Dourado (FMT-HVD) and in field conditions in the municipality of Guajará (bordering the Amazonas and Acre states; 02°58’18″ S and 57°40′38′ W), in two municipalities of the Acre state, Cruzeiro do Sul (07°37’50″ S and 72°40’13″ W) and Mâncio Lima (07°36′49″ S and 72°53′47″ W), as well as in the Boa vista municipality (02°49′12″ S and 60°40′23″ W), Roraima state (Table 1 and Figure 1).

Table 1.
Localities of P. vivax parasite blood collection by Brazilian states.
Figure 1.
Brazilian map highlighting the Acre (AC), Amazonas (AM), Amapá (AP), Pará (PA), Rondônia (RO) and Roraima (RR) states and the municipalities of parasite infection.
2.2. Malaria Diagnosis
The malaria diagnoses were made by light microscopy (Giemsa-stained thick blood droplets) in situ. To ensure the presence of a mono-P. vivax infection, together with microscopic diagnosis, all samples were subjected to molecular diagnosis by polymerase chain reaction (PCR). Firstly, conventional and real-time PCRs were performed using Plasmodium primers [28]. Then, the positive samples were submitted to species-specific single or nested PCRs to detect P. vivax [29], P. falciparum [30] and/or P. malariae [31]. The samples were stored at the Malaria Research Laboratory (LPM) at Instituto Oswaldo Cruz (IOC), headquarters of the Reference Center for Malaria Treatment and Diagnosis (CPD-Mal/Fiocruz). Only patients with P. vivax mono-infections were included in the study.
2.3. DNA Extraction, Amplification and Sequencing
The DNA from 1 mL blood samples was extracted using the QIAamp™ DNA Blood Midi Kit (QIAGEN, Hilden, Germany), according to the manufacturer’s instructions. For this study, approximately 1186 base pair (bp) fragments of the pvcrt-o gene of P. vivax were amplified according to the protocol described by Cheong et al. (2020) [14] and a fragment of 800 bp was amplified for the analysis of the SNPs T958M, Y976F and F1076L in the pvmdr1 gene according to the protocol described by Brega et al. (2005) [32]. PCR products were analyzed by electrophoresis on 2% agarose gel, visualized under a UV transilluminator (DigiDoc-It; UVP, Unpland, CA, USA) and purified using Wizard™ SV Gel and the PCR Clean-Up System (Promega, Madison, WI, USA), following the manufacturer’s procedure. The purified DNA sequencing was carried out through Big Dye™ Terminator Cycle Sequencing Ready Reaction version 3.1 (Applied Biosystems, Carlsbad, CA, USA), with 3.2 μM of forward and reverse PCR primers. DNA sequences to investigate the SNPs in pvcrt-o and pvmdr1 genes were determined using the ABI Prism DNA Analyzer™ 3730 (Applied Biosystems, Carlsbad, CA, USA), at the Fiocruz Genomic Platform PDTIS/Fiocruz RPT01A. Nucleotide sequences were aligned using a ClustalW multiple sequence aligner in BioEdit version 7.7.1 software (North Carolina State University, Raleigh, USA), and the electropherograms were analyzed using NovoSNP® version 3.0.1 software (University of Antwerp, Antwerpen, Belgium), using the quality cutoff set to 10, in order to avoid the lack of real variation, and using the Salvador 1 strain as a reference sequence (GenBank Accession No. AF314649.1 for pvcrt-o and GenBank Accession No. AY571984.1 for pvmdr1). DNA sequences were deposited in GenBank (the NIH’s genetic sequence database; www.ncbi/nlm/nih.gov/GenBank accessed on 21 August 2023) with the accession numbers OR461289–OR461401.
3. Results
3.1. Prevalence of Polymorphisms in the pvcrt-o Gene
A total of 104 (80%) of the 130 samples were successfully sequenced for the pvcrt-o gene. The insertion of lysine (AAG codon) at position 10, named the K10 insertion and considered a candidate molecular marker of CQR, was detected in 15 (14%) samples: seven from Acre (n = 50; 14%), five from Amazonas (n = 30; 16%), one from Pará (n = 1; 100%) and two from Roraima (n = 19; 11%). Meanwhile, it was not detected in the Rondônia (n = 2) and Amapá (n = 2) (Table 2) samples. In the vast majority of pvcrt-o sequenced samples (n = 89; 86%), no mutations were detected and, therefore, these DNA sequences were identical to the Sal-1 strain used as the wild-type reference of CQ-sensitive parasites.

Table 2.
Distribution of the K10 insertion (AAG codon) in the pvcrt-o gene in 104 samples of P. vivax from the Legal Amazon.
All patients who attended the Malaria Reference Center located in Rio de Janeiro (CPD-Mal) had uncomplicated malaria and were followed up clinically and through laboratory testing; clinical and parasitological cures were confirmed within the expected time frame (Supplementary Materials Table S1). Using the Malaria Epidemiological Surveillance Information System (SIVEP-Malaria data) and Malaria Control Nacional Program (PMCN) definitions, there was no recrudescence in the six patients from the endemic area who had parasites with the K10 insertion until 60 days after initiating treatment of the primary vivax infection. The three patients I, J and L, were considered cases of reinfections and not recrudescence by CQ-resistant parasites due to P. vivax notifications >60 days after initiating treatment of the primary vivax infection (Supplementary Materials Table S1).
3.2. Prevalence of Polymorphisms in the pvmdr1 Gene
The pvmdr1 gene was satisfactorily amplified and sequenced in 113 (86%) of the 130 samples investigated. Three-point mutations (T958M, Y976F and F1076L) considered as potentially associated with the P. vivax resistance phenotype were examined. The SNP T958M was the most prevalent (93%) and was found in parasites from all states. The SNP F1076L was present in only three samples from Amazonas (n = 25; 12%), while the Y976F mutation was absent in all samples examined (Table 3).

Table 3.
Frequency of alleles in the pvmdr1 gene in 113 samples of P. vivax, according to the malaria diagnosis localities.
Haplotype analysis of the pvmdr1 gene showed that almost all samples (n = 104; 92%) had the MYF single mutant profile at codon T958M, predominating in the states of Acre (58/62; 93%), Amazonas (22/25; 88%) and Roraima (19/21; 90%). In the other states studied, the proportion was less than 2%. The MYL double mutant profile (T958M + F1076L) was detected exclusively in 12% (3/25) of the samples from Amazonas, while the wild-type TYF was detected in the minority of samples: four from Acre (n = 62; 5%) and two from Roraima (n = 21; 10%) (Table 4). In this way, the polymorphism in codon F1076L was always associated with polymorphism in codon T958M.

Table 4.
Distribution of haplotypes in the pvmdr1 gene in 113 samples of P. vivax from the Legal Amazon.
The three P. vivax patients harboring double mutant MYL parasites in pvmdr1, whose samples were followed up clinically at the CPD-Mal laboratory, were cured within the expected time (Table 5).

Table 5.
Patients followed up at CPD-Mal, carrying P. vivax parasites containing the MYL double pvmdr1 mutant haplotype infected in the Amazonas state and the dates of diagnosis and of cure (parasitological and molecular negative assays).
3.3. Comparative Alignment between Here Presented pvcrt-o and pvmdr1 Sequences of CQ-Sensitive Parasites with Those Reported by Melo et al. (2014) [20]
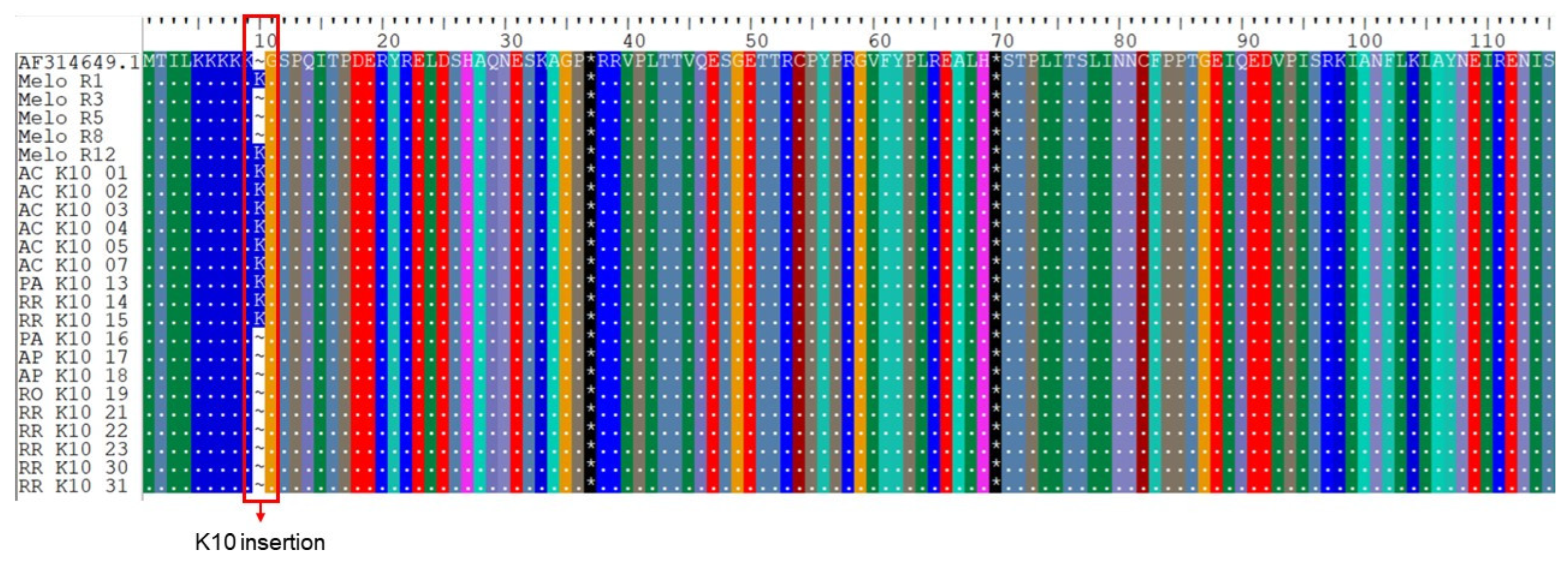
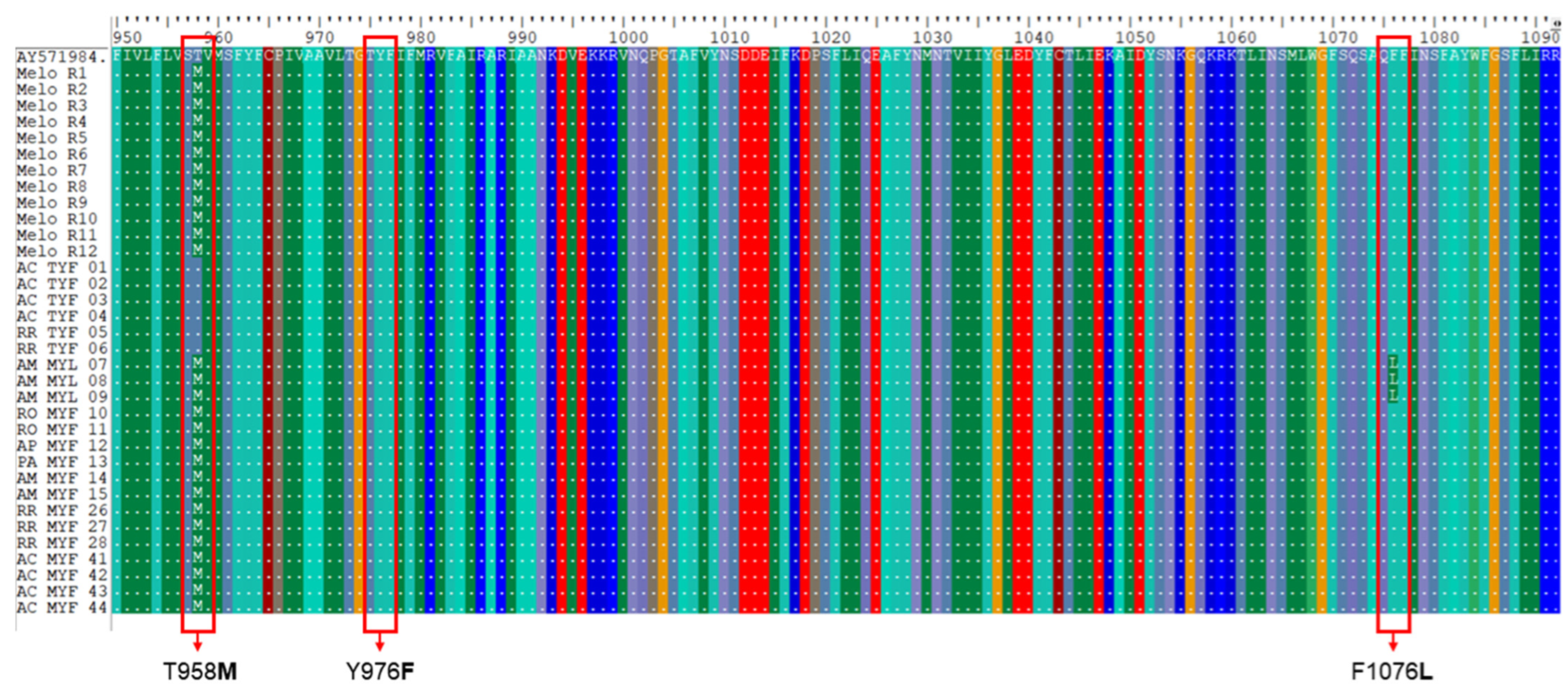
When we analyzed our CQ-sensitive sequences with those that were CQ-resistant of Melo et al. [20], we found that 14% of the sensitive pvcrt-o gene sequences had the K10 insertion against only two resistant isolates presenting the K10 insertion (Figure 2). In relation to the pvmdr1 gene, 92% of CQ-sensitive isolates presented the single mutant MYF haplotype whereas 100% of CQ-resistant or -sensitive sequences [20] contained the MYF haplotype (Figure 3).
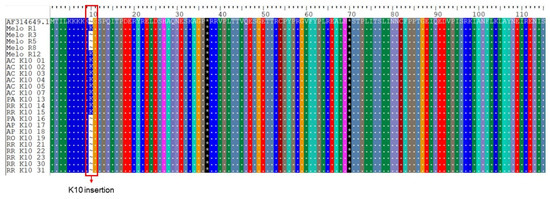
Figure 2.
Alignment of representative CQ-resistant and -sensitive pvcrt-o sequences, with the K10 insertion highlighted in red. Melo R1 to R12 correspond to CQ-resistant sequences of Melo et al. [20]. The sequences named K10 01 to 31 correspond to the isolates sequenced in this study. AC: Acre; AM: Amazonas; AP: Amapá; PA: Pará; RO: Rondônia; RR: Roraima.
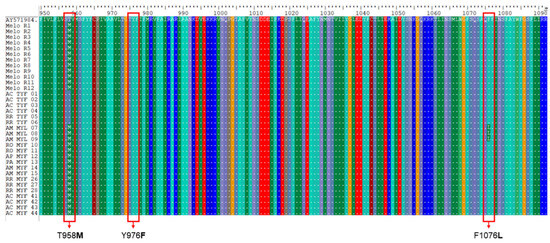
Figure 3.
Alignment of representative CQ-resistant and -sensitive pvmdr1 sequences, with the SNPs investigated highlighted in red (T958M, Y976F and F1076L). Melo R1 to R12 correspond to CQ-resistant sequences of Melo et al. [20]. The sequences named TYF correspond to the isolates with the wild-type haplotype sequenced in this study. Sequences named MYL and MYF correspond to the isolates with one and two non-synonymous mutations detected in this study, respectively. AC: Acre; AM: Amazonas; AP: Amapá; PA: Pará; RO: Rondônia; RR: Roraima.
4. Discussion
P. vivax is the most geographically widespread pathogen of human malaria and is responsible for most cases outside the African continent [1]. Vivax malaria is considered a public health problem in many parts of the world, particularly with regard to the morbidity of children and pregnant women [33], the rare but real possibility of fatal infections [16] and the presence of CQ-resistant P. vivax parasites [5]. Due to the biological characteristics of P. vivax that prevent a continuous in vitro culture system, molecular monitoring has become the tool of choice for the surveillance of resistance to antimalarials due to its practical and economic advantages over in vivo fieldwork and in vitro assays, recommended by the WHO [1,13]. Previous work has shown a significant association between the allele pfcrt and pfmdr1 variants and P. falciparum drug resistance [25]. However, putative mutations in these genes, considered as candidate markers of antimalarial drug resistance, are not clear with respect to P. vivax [34,35]. In fact, regardless of the chemoresistance phenotype, the genetic polymorphism of P. vivax is notable [36] and this parasite is known to be more diverse than P. falciparum [37]. As, so far, little is known about the genotype of P. vivax parasites circulating in Brazilian endemic areas, thus, it is quite pertinent to investigate the polymorphisms of pvmdr1 and pvcrt-o.
The main gene related to P. vivax CQ resistance is pvcrt-o. Indeed, the presence of the “AAG” lysine insert in exon I of pvcrt-o (referred as the “K10 insert”) has been associated with a significant reduction in the IC50 of CQ [18]. In our analysis, it was possible to identify the K10 insertion in 15 samples (14%) distributed among the states of Acre (7), Amazonas (5), Pará (1) and Roraima (2). This SNP was also reported in studies from French Guiana (57%) [38], China (32%) [39] and, to a lesser extent, India (5.6%) [40], Pakistan (16%) [41] and Thailand (18%) [42]. Due to the scarcity of previous studies, we do not have knowledge about the expansion or retraction of this mutation in Brazil. One possibility would be that this mutation has been introduced to Brazil through the events of illegal mining in French Guiana, where this insertion is frequent, although not directly associated with CQR [38]. In fact, when we analyzed the results of samples from patients who carried P. vivax with the K10 insertion, a good response to the CQ treatment occurred within the 28-day expected period, with no observed case of recrudescence. Thus, excluding the small possibility of primaquine acting against minority populations of CQR parasite clones, our data reinforce that the K10 insertion is not a predictor of the P. vivax resistance phenotype to treatment with CQ, as previously suggested [13,43,44].
Regarding the pvmdr1 gene, several studies describe that the substitution in the Y976F codon, which changes the amino acid tyrosine to phenylalanine, would be associated with a reduced susceptibility to CQ [39,45,46,47,48]. This SNP has even been identified in endemic areas of China, Cambodia and Ethiopia [19,24,47], where treatment failure has been reported in patients with vivax malaria treated with CQ. Although this SNP was not detected in the present study nor in 2018 in the triple border region involving Colombia, Peru and Brazil/Amazonas [49], previous studies by our group reported the Y976F polymorphism at a high frequency (85.7%) in 2009 [26] and at a low frequency (15%) from 2010 to 2014 [50] in the endemic areas of the Legal Amazon. These facts seem to indicate two possibilities of events: either the SNP Y976F was present in only a few locations in the endemic region of the Legal Amazon or this mutation was not becoming fixed in the Brazilian endemic region. On the other hand, since we did neither detect the Y976F polymorphism in any of the samples here examined, nor any therapeutic failure to CQ in this casuistic, we cannot draw a conclusion about the role of this polymorphism as a marker of P. vivax CQR.
In addition to Y976F, we also investigated SNPs at the T958M and F1076L codons in the pvmdr1 gene, both of which have also been proposed to be potentially associated with CQ resistance [20,34]. The SNP at codon T958M was present in almost all analyzed samples (92%), including those of the 34 patients whose parasite genes could be sequenced and responded to CQ treatment within the expected period. This high frequency has been verified by previous studies carried out by our group in Brazilian endemic areas [26,50], as well as by other authors analyzing samples from Africa [51], South America [50] and Southeast Asia [19], indicating the fixation of T958M in parasitic populations of P. vivax circulating in Brazil and in the world. This fact indicates a low potential of this polymorphism as a CQR marker.
It has been mentioned that the T958M and F1076L polymorphisms alone may not be associated with CQR, unless if acting together, they could modify the protein’s conformation and enable drug evasion [32,51]. When analyzing these double mutants, we verified that the F1076L polymorphism was always present with T958M, originating the MYL double mutant haplotype. This dependency relationship between these alleles was already noted by our group in isolated parasites from Acre, Amazonas, Rondônia and in autochthonous cases from the Atlantic Forest of Rio de Janeiro [50], as well as by other authors in Southeast Asia [52,53,54], where there are cases of P. vivax resistant to CQ treatment. However, once again, the good therapeutic response in patients carrying MYL parasites in the present study, disregarding the small possibility of primaquine acting in minority clones of CQR parasites, indicates that the association of double mutants with P. vivax CQR is unlikely.
As the Y976F mutant allele was not detected in our series, it was not possible to establish a relationship between chemoresistance and CQ for the TYL double mutant haplotype (T958M + Y976F + F1076L), as previously suggested in the literature [39,55,56].
Finally, the tendency toward tolerance or resistance to the drugs recommended for the treatment of vivax malaria may be more complex, including other genes in addition to P. falciparum, where pvmdr1 SNPs located in the transmembrane domain are associated with CQ vacuole efflux. It is noteworthy that striking differences in the topologies and numbers of SNPs in these transporter genes between P. vivax and P. falciparum reinforce the idea that mechanisms other than mutations may explain this CQ-resistant phenotype in P. vivax. In fact, the P. vivax CQ resistance process may also differ by its combined CQ/PQ treatment regimen, so it could be only a matter of time before more CQ-resistant P. vivax cases appear.
5. Conclusions
The results presented in this study reinforce that the mutations here investigated on pvcrt-o and pvmdr1 may not be good markers of P. vivax chemoresistance to CQ. New approaches for the identification of robust genetic markers for monitoring chloroquine resistance in P. vivax populations are needed.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/biomedicines12010141/s1, Table S1: Patients followed up at CPD-Mal and SIVEP-Malaria Database Platform, carrying P. vivax parasites containing the insertion of K10 in pvcrt-o, according to the state of infection.
Author Contributions
Conceptualization, M.d.F.F.-d.-C.; supervision, M.d.F.F.-d.-C.; methodology, R.d.A.-F., L.T.d.Q., A.R.d.L.M., B.d.O.B. and M.d.F.F.-d.-C.; epidemiological survey, J.O.-F., R.M.d.S., L.R.P.-R. and P.B.; formal analysis, R.d.A.-F., N.K.A.-d.-O., L.T.d.Q., J.d.A.B. and M.d.F.F.-d.-C.; Investigation, M.d.F.F.-d.-C. and C.T.D.-R.; resources, M.d.F.F.-d.-C.; original draft preparation, R.d.A.-F.; writing—review, M.d.F.F.-d.-C., C.T.D.-R., R.M.d.S., L.R.P.-R., J.O.-F. and P.B.; editing, R.d.A.-F.; project administration, M.d.F.F.-d.-C.; funding acquisition, M.d.F.F.-d.-C., C.T.D.-R. and P.B. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq; http://www.cnpq.br/, accessed on 10 March 2022) through Research Productivity Fellowships to C.T.D.-R. (310445/2017-5), M.d.F.F.-d.-C. (306025/2018-3) and P.B. (311562/2021-3), who are also Cientistas do Nosso Estado (C.T.D.-R.—E-26/202.921/2018; M.d.F.F.-d.-C.—E-26/203.295/2015 and P.B. E-26/200.925/2022) of the Fundação Carlos Chagas Filho de Amparo à Pesquisa do Estado de Rio de Janeiro (FAPERJ; http://www.faperj.br/, accessed on 10 March 2022). This work was also supported by the Departamento de Ciência e Tecnologia em Saúde/Ministério da Saúde (DECIT/MS) (Grant No.: 402675/2018-5), Programa Nacional de Controle e Prevenção da Malária/Secretaria de Vigilância em Saúde/Ministério da Saúde (SVS/MS) and Fiocruz (Grant No.: 026-FIO-18-2-1).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Ethical approval for this study was obtained from the Ethics and Research Committee of Research in Human Beings at Fiocruz under the number 221/03 and CAAE 46084015.1.0000.5248 for the Acre samples. Participants were informed about the study and signed a consent form.
Data Availability Statement
Data supporting the conclusions of this article are included within the article. The datasets used and/or analyzed during the present study are available from the corresponding author upon reasonable request.
Acknowledgments
We would like to thank all the patients for their participation in this study. We would also like to acknowledge the staff from the Genomic Platform for DNA sequencing facilities RPT01A/PDTIS/Fiocruz and the Coordenação de Vigilância em Saúde e Laboratórios de Referencia, Fiocruz/Coordination of Health Surveillance and Reference Laboratories, for their financial and logistical support. All authors have approved of the final manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- World Health Organization. World Malaria Report 2022; World Health Organization: Geneva, Switzerland, 2022; pp. 1–293. ISBN 9789240064898. Available online: https://www.who.int/teams/global-malaria-programme/reports/world-malaria-report-2022 (accessed on 23 May 2023).
- Rodríguez, J.A.I.; Rodríguez, S.N.I.; Olivera, M.J. Plasmodium vivax Malaria across South America: Management Guidelines and Their Quality Assessment. Rev. Soc. Bras. Med. Trop. 2020, 53, e20200179. [Google Scholar] [CrossRef] [PubMed]
- Daron, J.; Boissière, A.; Boundenga, L.; Ngoubangoye, B.; Houze, S.; Arnathau, C.; Sidobre, C.; Trape, J.-F.; Durand, P.; Renaud, F.; et al. Population Genomic Evidence of Plasmodium vivax Southeast Asian Origin. Sci. Adv. 2021, 7, 3713–3741. [Google Scholar] [CrossRef] [PubMed]
- Tableau Public. Tableau Public Dados Para Cidadão. Available online: https://public.tableau.com/app/profile/mal.ria.brasil/viz/Dadosparacidado_201925_03_2020/Incio (accessed on 14 December 2023).
- Gonçalves, L.A.; Cravo, P.; Ferreira, M.U. Emerging Plasmodium vivax Resistance to Chloroquine in South America: An Overview. Mem. Inst. Oswaldo Cruz 2014, 109, 534–539. [Google Scholar] [CrossRef] [PubMed]
- Rieckmann, K.H.; Davis, D.R.; Hutton, D.C. Plasmodium vivax Resistance to Chloroquine? Lancet 1989, 334, 1183–1184. [Google Scholar] [CrossRef] [PubMed]
- Moore, D.V.; Lanier, J.E. Observations on Two Plasmodium falciparum Infections with an Abnormal Response to Chloroquine. Am. J. Trop. Med. Hyg. 1961, 10, 5–9. [Google Scholar] [CrossRef] [PubMed]
- Gama, B.E.; Lacerda, M.V.G.; Daniel-Ribeiro, C.T.; Ferreira-da-Cruz, M.d.F. Chemoresistance of Plasmodium falciparum and Plasmodium vivax Parasites in Brazil: Consequences on Disease Morbidity and Control. Mem. Inst. Oswaldo Cruz 2011, 106, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Alecrim, M.D.G.C.; Alecrim, W.; Macêdo, V. Plasmodium vivax Resistance to Chloroquine (R2) and Mefloquine (R3) in Brazilian Amazon Region. Rev. Soc. Bras. Med. Trop. 1999, 32, 67–68. [Google Scholar] [CrossRef]
- De Santana Filho, F.S.; Arcanjo, A.R.D.L.; Chehuan, Y.M.; Costa, M.R.; Martinez-Espinosa, F.E.; Vieira, J.L.; Barbosa, M.D.G.V.; Alecrim, W.D.; Alecrim, M.D.G.C. Chloroquine-Resistant Plasmodium vivax, Brazilian Amazon. Emerg. Infect. Dis. 2007, 13, 1125–1126. [Google Scholar] [CrossRef]
- Marques, M.M.; Costa, M.R.F.; Santana Filho, F.S.; Vieira, J.L.F.; Nascimento, M.T.S.; Brasil, L.W.; Nogueira, F.; Silveira, H.; Reyes-Lecca, R.C.; Monteiro, W.M.; et al. Plasmodium vivax Chloroquine Resistance and Anemia in the Western Brazilian Amazon. Antimicrob. Agents Chemother. 2014, 58, 342–347. [Google Scholar] [CrossRef]
- Cotter, C.; Sturrock, H.J.W.; Hsiang, M.S.; Liu, J.; Phillips, A.A.; Hwang, J.; Gueye, C.S.; Fullman, N.; Gosling, R.D.; Feachem, R.G.A. The Changing Epidemiology of Malaria Elimination: New Strategies for New Challenges. Lancet 2013, 382, 900–911. [Google Scholar] [CrossRef]
- Ferreira, M.U.; Nobrega de Sousa, T.; Rangel, G.W.; Johansen, I.C.; Corder, R.M.; Ladeia-Andrade, S.; Gil, J.P. Monitoring Plasmodium vivax Resistance to Antimalarials: Persisting Challenges and Future Directions. Int. J. Parasitol. Drugs Drug Resist. 2021, 15, 9–24. [Google Scholar] [CrossRef] [PubMed]
- Cheong, F.-W.; Dzul, S.; Fong, M.-Y.; Lau, Y.-L.; Ponnampalavanar, S. Plasmodium vivax Drug Resistance Markers: Genetic Polymorphisms and Mutation Patterns in Isolates from Malaysia. Acta Trop. 2020, 206, 105454. [Google Scholar] [CrossRef] [PubMed]
- Nomura, T.; Carlton, J.M.R.; Baird, J.K.; Del Portillo, H.A.; Fryauff, D.J.; Rathore, D.; Fidock, D.A.; Su, X.Z.; Collins, W.E.; McCutchan, T.F.; et al. Evidence for Different Mechanisms of Chloroquine Resistance in 2 Plasmodium Species That Cause Human Malaria. J. Infect. Dis. 2001, 183, 1653–1661. [Google Scholar] [CrossRef] [PubMed]
- Buyon, L.E.; Elsworth, B.; Duraisingh, M.T. The Molecular Basis of Antimalarial Drug Resistance in Plasmodium vivax. Int. J. Parasitol. Drugs Drug Resist. 2021, 16, 23–27. [Google Scholar] [CrossRef] [PubMed]
- Lu, F.; Lim, C.S.; Nam, D.-H.; Kim, K.; Lin, K.; Kim, T.-S.; Lee, H.-W.; Chen, J.-H.; Wang, Y.; Sattabongkot, J.; et al. Genetic Polymorphism in Pvmdr1 and Pvcrt-o Genes in Relation to in Vitro Drug Susceptibility of Plasmodium vivax Isolates from Malaria-Endemic Countries. Acta Trop. 2011, 117, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Chehuan, Y.F.; Costa, M.R.; Costa, J.S.; Alecrim, M.G.; Nogueira, F.; Silveira, H.; Brasil, L.W.; Melo, G.C.; Monteiro, W.M.; Lacerda, M.V. In Vitro Chloroquine Resistance for Plasmodium vivax Isolates from the Western Brazilian Amazon. Malar. J. 2013, 12, 226. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Wang, L.; Soe, M.T.; Aung, P.L.; Wei, H.; Liu, Z.; Ma, T.; Huang, Y.; Menezes, L.J.; Wang, Q.; et al. Molecular Surveillance for Drug Resistance Markers in Plasmodium vivax Isolates from Symptomatic and Asymptomatic Infections at the China–Myanmar Border. Malar. J. 2020, 19, 281. [Google Scholar] [CrossRef] [PubMed]
- Melo, G.C.; Monteiro, W.M.; Siqueira, A.M.; Silva, S.R.; Magalhães, B.M.L.; Alencar, A.C.C.; Kuehn, A.; Del Portillo, H.A.; Fernandez-Becerra, C.; Lacerda, M.V.G. Expression Levels of Pvcrt-o and Pvmdr-1 Are Associated with Chloroquine Resistance and Severe Plasmodium vivax Malaria in Patients of the Brazilian Amazon. PLoS ONE 2014, 9, e105922. [Google Scholar] [CrossRef]
- Suwanarusk, R.; Chavchich, M.; Russell, B.; Jaidee, A.; Chalfein, F.; Barends, M.; Prasetyorini, B.; Kenangalem, E.; Piera, K.A.; Lek-Uthai, U.; et al. Amplification of Pvmdr1 Associated with Multidrug-Resistant Plasmodium vivax. J. Infect. Dis. 2008, 198, 1558–1564. [Google Scholar] [CrossRef][Green Version]
- Orjuela-Sánchez, P.; Filho, F.S.D.S.; Machado-Lima, A.; Chehuan, Y.F.; Costa, M.R.F.; Alecrim, M.D.G.C.; Del Portillo, H.A. Analysis of Single-Nucleotide Polymorphisms in the Crt-o and Mdr1 Genes of Plasmodium vivax among Chloroquine-Resistant Isolates from the Brazilian Amazon Region. Antimicrob. Agents Chemother. 2009, 53, 3561–3564. [Google Scholar] [CrossRef]
- Lu, F.; Wang, B.; Cao, J.; Sattabongkot, J.; Zhou, H.; Zhu, G.; Kim, K.; Gao, Q.; Han, E.-T. Prevalence of Drug Resistance-Associated Gene Mutations in Plasmodium vivax in Central China. Korean J. Parasitol. 2012, 50, 379–384. [Google Scholar] [CrossRef] [PubMed]
- Golassa, L.; Erko, B.; Baliraine, F.N.; Aseffa, A.; Swedberg, G. Polymorphisms in Chloroquine Resistance-Associated Genes in Plasmodium vivax in Ethiopia. Malar. J. 2015, 14, 64–164. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Jovel, I.T.; Mejía, R.E.; Banegas, E.; Piedade, R.; Alger, J.; Fontecha, G.; Ferreira, P.E.; Veiga, M.I.; Enamorado, I.G.; Bjorkman, A.; et al. Drug Resistance Associated Genetic Polymorphisms in Plasmodium falciparum and Plasmodium vivax Collected in Honduras, Central America. Malar. J. 2011, 10, 376. [Google Scholar] [CrossRef] [PubMed]
- Gama, B.E.; de Oliveira, N.K.A.; de Souza, J.M.; Daniel-Ribeiro, C.T.; Ferreira-da-Cruz, M.d.F. Characterisation of Pvmdr1 and Pvdhfr Genes Associated with Chemoresistance in Brazilian Plasmodium vivax Isolates. Mem. Inst. Oswaldo Cruz 2009, 104, 1009–1011. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Vargas-Rodríguez, R.D.C.M.; Bastos, M.D.S.; Menezes, M.J.; Orjuela-Sánchez, P.; Ferreira, M.U. Single-Nucleotide Polymorphism and Copy Number Variation of the Multidrug Resistance-1 Locus of Plasmodium vivax: Local and Global Patterns. Am. J. Trop. Med. Hyg. 2012, 87, 813–821. [Google Scholar] [CrossRef] [PubMed]
- Gama, B.E.; Silva-Pires, F.d.E.S.; Lopes, M.N.K.R.; Cardoso, M.A.B.; Britto, C.; Torres, K.L.; de Mendonça Lima, L.; de Souza, J.M.; Daniel-Ribeiro, C.T.; de Fátima Ferreira-da-Cruz, M. Real-Time PCR versus Conventional PCR for Malaria Parasite Detection in Low-Grade Parasitemia. Exp. Parasitol. 2007, 116, 427–432. [Google Scholar] [CrossRef] [PubMed]
- Almeida-De-Oliveira, N.K.; Moreira, O.C.; De Lavigne, A.R.; Mendonça-Lima, L.; Werneck, G.L.; Daniel-Ribeiro, C.T.; Ferreira-Da-Cruz, M.D.F. Analytical Validation of Real-Time Quantitative PCR Assays for Optimum Diagnosis of Vivax Malaria. Mem. Inst. Oswaldo Cruz 2019, 114, e180350. [Google Scholar] [CrossRef] [PubMed]
- Zalis, M.G.; Ferreira-da-Cruz, M.F.; Balthazar-Guedes, H.C.; Banic, D.M.; Alecrim, W.; Souza, J.M.; Druilhe, P.; Daniel-Ribeiro, C.T. Malaria Diagnosis: Standardization of a Polymerase Chain Reaction for the Detection of Plasmodium falciparum Parasites in Individuals with Low-Grade Parasitemia. Parasitol. Res. 1996, 82, 612–616. [Google Scholar] [CrossRef]
- Snounou, G.; Viriyakosol, S.; Zhu, X.P.; Jarra, W.; Pinheiro, L.; do Rosario, V.E.; Thaithong, S.; Brown, K.N. High Sensitivity of Detection of Human Malaria Parasites by the Use of Nested Polymerase Chain Reaction. Mol. Biochem. Parasitol. 1993, 61, 315–320. [Google Scholar] [CrossRef]
- Brega, S.; Meslin, B.; De Monbrison, F.; Severini, C.; Gradoni, L.; Udomsangpetch, R.; Sutanto, I.; Peyron, F.; Picot, S. Identification of the Plasmodium vivax Mdr-like Gene (Pvmdr1) and Analysis of Single-Nucleotide Polymorphisms among Isolates from Different Areas of Endemicity. J. Infect. Dis. 2005, 191, 272–277. [Google Scholar] [CrossRef][Green Version]
- Phyo, A.P.; Dahal, P.; Mayxay, M.; Ashley, E.A. Clinical Impact of Vivax Malaria: A Collection Review. PLoS Med. 2022, 19, e1003890. [Google Scholar] [CrossRef] [PubMed]
- Spotin, A.; Mahami-Oskouei, M.; Ahmadpour, E.; Parsaei, M.; Rostami, A.; Emami, S.; Gholipour, S.; Farmani, M. Global Assessment of Genetic Paradigms of Pvmdr1 Mutations in Chloroquine-Resistant Plasmodium vivax Isolates. Trans. R. Soc. Trop. Med. Hyg. 2020, 114, 339–345. [Google Scholar] [CrossRef] [PubMed]
- Cubides, J.R.; Camargo-Ayala, P.A.; Niño, C.H.; Garzón-Ospina, D.; Ortega-Ortegón, A.; Ospina-Cantillo, E.; Orduz-Durán, M.F.; Patarroyo, M.E.; Patarroyo, M.A. Simultaneous Detection of Plasmodium vivax Dhfr, Dhps, Mdr1 and Crt-o Resistance-Associated Mutations in the Colombian Amazonian Region. Malar. J. 2018, 17, 130. [Google Scholar] [CrossRef] [PubMed]
- Habtamu, K.; Petros, B.; Yan, G. Plasmodium vivax: The Potential Obstacles It Presents to Malaria Elimination and Eradication. Trop. Dis. Travel Med. Vaccines 2022, 8, 27. [Google Scholar] [CrossRef]
- De Souza-Neiras, W.C.; De Melo, L.M.S.; Machado, R.L.D. The Genetic Diversity of Plasmodium vivax: A Review. Mem. Inst. Oswaldo Cruz 2007, 102, 245–254. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Musset, L.; Heugas, C.; Naldjinan, R.; Blanchet, D.; Houze, P.; Abboud, P.; Volney, B.; Walter, G.; Lazrek, Y.; Epelboin, L.; et al. Emergence of Plasmodium vivax Resistance to Chloroquine in French Guiana. Antimicrob. Agents Chemother. 2019, 63, e02116-18. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Zhang, J.; Li, Q.; Hu, Y.; Ruan, Y.; Tao, Z.; Xia, H.; Qiao, J.; Meng, L.; Zeng, W.; et al. Ex Vivo Susceptibilities of Plasmodium vivax Isolates from the China-Myanmar Border to Antimalarial Drugs and Association with Polymorphisms in Pvmdr1 and Pvcrt-o Genes. PLoS Negl. Trop. Dis. 2020, 14, e0008255. [Google Scholar] [CrossRef]
- Joy, S.; Mukhi, B.; Ghosh, S.K.; Achur, R.N.; Gowda, D.C.; Surolia, N. Drug Resistance Genes: Pvcrt-o and Pvmdr-1 Polymorphism in Patients from Malaria Endemic South Western Coastal Region of India. Malar. J. 2018, 17, 40. [Google Scholar] [CrossRef]
- Noisang, C.; Prosser, C.; Meyer, W.; Chemoh, W.; Ellis, J.; Sawangjaroen, N.; Lee, R. Molecular Detection of Drug Resistant Malaria in Southern Thailand. Malar. J. 2019, 18, 275. [Google Scholar] [CrossRef]
- Bansal, D.; Acharya, A.; Bharti, P.K.; Abdelraheem, M.H.; Elmalik, A.; Abosalah, S.; Khan, F.Y.; ElKhalifa, M.; Kaur, H.; Mohapatra, P.K.; et al. Distribution of Mutations Associated with Antifolate and Chloroquine Resistance among Imported Plasmodium vivax in the State of Qatar. Am. J. Trop. Med. Hyg. 2017, 97, 1797–1803. [Google Scholar] [CrossRef]
- Roesch, C.; Mairet-Khedim, M.; Kim, S.; Lek, D.; Popovici, J.; Witkowski, B. Impact of the first-line treatment shift from dihydroartemisinin/piperaquine to artesunate/mefloquine on Plasmodium vivax drug susceptibility in Cambodia. J. Antimicrob. Chemother. 2020, 75, 1766–1771. [Google Scholar] [CrossRef] [PubMed]
- Rumaseb, A.; Moraes Barros, R.R.; Sá, J.M.; Juliano, J.J.; William, T.; Braima, K.A.; Barber, B.E.; Anstey, N.M.; Price, R.N.; Grigg, M.J.; et al. No Association between the Plasmodium vivax crt-o MS334 or In9pvcrt Polymorphisms and Chloroquine Failure in a Pre-Elimination Clinical Cohort from Malaysia with a Large Clonal Expansion. Antimicrob. Agents Chemother. 2023, 67, e0161022. [Google Scholar] [CrossRef] [PubMed]
- Silva, S.R.; Almeida, A.C.G.; Da Silva, G.A.V.; Ramasawmy, R.; Lopes, S.C.P.; Siqueira, A.M.; Costa, G.L.; Sousa, T.N.; Vieira, J.L.F.; Lacerda, M.V.G.; et al. Chloroquine Resistance Is Associated to Multi-Copy Pvcrt-o Gene in Plasmodium vivax Malaria in the Brazilian Amazon. Malar. J. 2018, 17, 267. [Google Scholar] [CrossRef] [PubMed]
- Noisang, C.; Meyer, W.; Sawangjaroen, N.; Ellis, J.; Lee, R. Molecular Detection of Antimalarial Drug Resistance in Plasmodium vivax from Returned Travellers to NSW, Australia during 2008–2018. Pathogens 2020, 9, 101. [Google Scholar] [CrossRef] [PubMed]
- Chaorattanakawee, S.; Lon, C.; Chann, S.; Thay, K.H.; Kong, N.; You, Y.; Sundrakes, S.; Thamnurak, C.; Chattrakarn, S.; Praditpol, C.; et al. Measuring Ex Vivo Drug Susceptibility in Plasmodium vivax Isolates from Cambodia. Malar. J. 2017, 16, 392. [Google Scholar] [CrossRef] [PubMed]
- Benavente, E.D.; Manko, E.; Phelan, J.; Campos, M.; Nolder, D.; Fernandez, D.; Velez-Tobon, G.; Castaño, A.T.; Dombrowski, J.G.; Marinho, C.R.F.; et al. Distinctive Genetic Structure and Selection Patterns in Plasmodium vivax from South Asia and East Africa. Nat. Commun. 2021, 12, 3160. [Google Scholar] [CrossRef] [PubMed]
- Price, R.N.; Marfurt, J.; Chalfein, F.; Kenangalem, E.; Piera, K.A.; Tjitra, E.; Anstey, N.M.; Russell, B. In Vitro Activity of Pyronaridine against Multidrug-Resistant Plasmodium falciparum and Plasmodium vivax. Antimicrob. Agents Chemother. 2010, 54, 5146–5150. [Google Scholar] [CrossRef]
- Gomes, L.R.; Almeida-De-Oliveira, N.K.; De Lavigne, A.R.; De Lima, S.R.F.; De Pina-Costa, A.; Brasil, P.; Daniel-Ribeiro, C.T.; Ménard, D.; Ferreira-Da-Cruz, M.D.F. Plasmodium vivax mdr1 Genotypes in Isolates from Successfully Cured Patients Living in Endemic and Non-Endemic Brazilian Areas. Malar. J. 2016, 15, 96. [Google Scholar] [CrossRef]
- Schousboe, M.L.; Ranjitkar, S.; Rajakaruna, R.S.; Amerasinghe, P.H.; Morales, F.; Pearce, R.; Ord, R.; Leslie, T.; Rowland, M.; Gadalla, N.B.; et al. Multiple Origins of Mutations in the Mdr1 Gene—A Putative Marker of Chloroquine Resistance in P. Vivax. PLoS Negl. Trop. Dis. 2015, 9, e0004196. [Google Scholar] [CrossRef]
- Kaur, H.; Sehgal, R.; Kumar, A.; Bharti, P.K.; Bansal, D.; Mohapatra, P.K.; Mahanta, J.; Sultan, A.A. Distribution Pattern of Amino Acid Mutations in Chloroquine and Antifolate Drug Resistance Associated Genes in Complicated and Uncomplicated Plasmodium vivax Isolates from Chandigarh, North India. BMC Infect. Dis. 2020, 20, 671. [Google Scholar] [CrossRef]
- Tang, T.; Xu, Y.; Cao, L.; Tian, P.; Shao, J.; Deng, Y.; Zhou, H.; Xiao, B. Ten-Year Molecular Surveillance of Drug-Resistant Plasmodium Spp. Isolated From the China–Myanmar Border. Front. Cell Infect. Microbiol. 2021, 11, 733788. [Google Scholar] [CrossRef] [PubMed]
- Ould Ahmedou Salem, M.S.; Mint Lekweiry, K.; Bouchiba, H.; Pascual, A.; Pradines, B.; Ould Mohamed Salem Boukhary, A.; Briolant, S.; Basco, L.K.; Bogreau, H. Characterization of Plasmodium Falciparum Genes Associated with Drug Resistance in Hodh Elgharbi, a Malaria Hotspot near Malian–Mauritanian Border. Malar. J. 2017, 16, 140. [Google Scholar] [CrossRef] [PubMed]
- Lê, H.G.; Naw, H.; Kang, J.-M.; Võ, T.C.; Myint, M.K.; Htun, Z.T.; Lee, J.; Yoo, W.G.; Kim, T.-S.; Shin, H.-J.; et al. Molecular Profiles of Multiple Antimalarial Drug Resistance Markers in Plasmodium Falciparum and Plasmodium vivax in the Mandalay Region, Myanmar. Microorganisms 2022, 10, 2021. [Google Scholar] [CrossRef] [PubMed]
- Ding, H.; Dong, Y.; Deng, Y.; Xu, Y.; Liu, Y.; Wu, J.; Chen, M.; Zhang, C.; Zheng, W. Characteristics of Molecular Markers Associated with Chloroquine Resistance in Plasmodium vivax Strains from Vivax Malaria Cases in Yunnan Province, China. Malar. J. 2023, 22, 181. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).