Clinical Approaches to Nestorone Subdermal Implant Therapy in Women’s Health
Abstract
1. Introduction
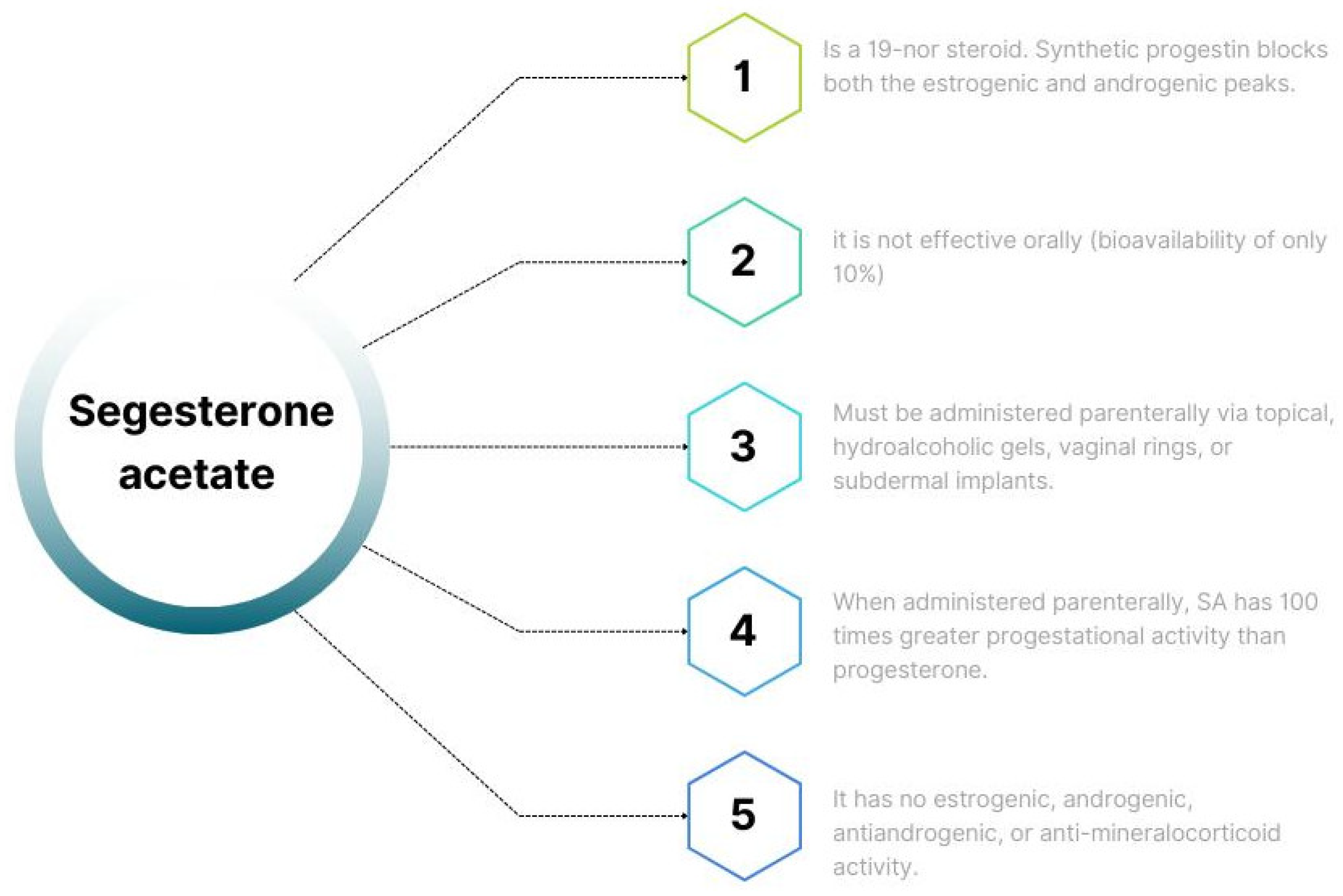
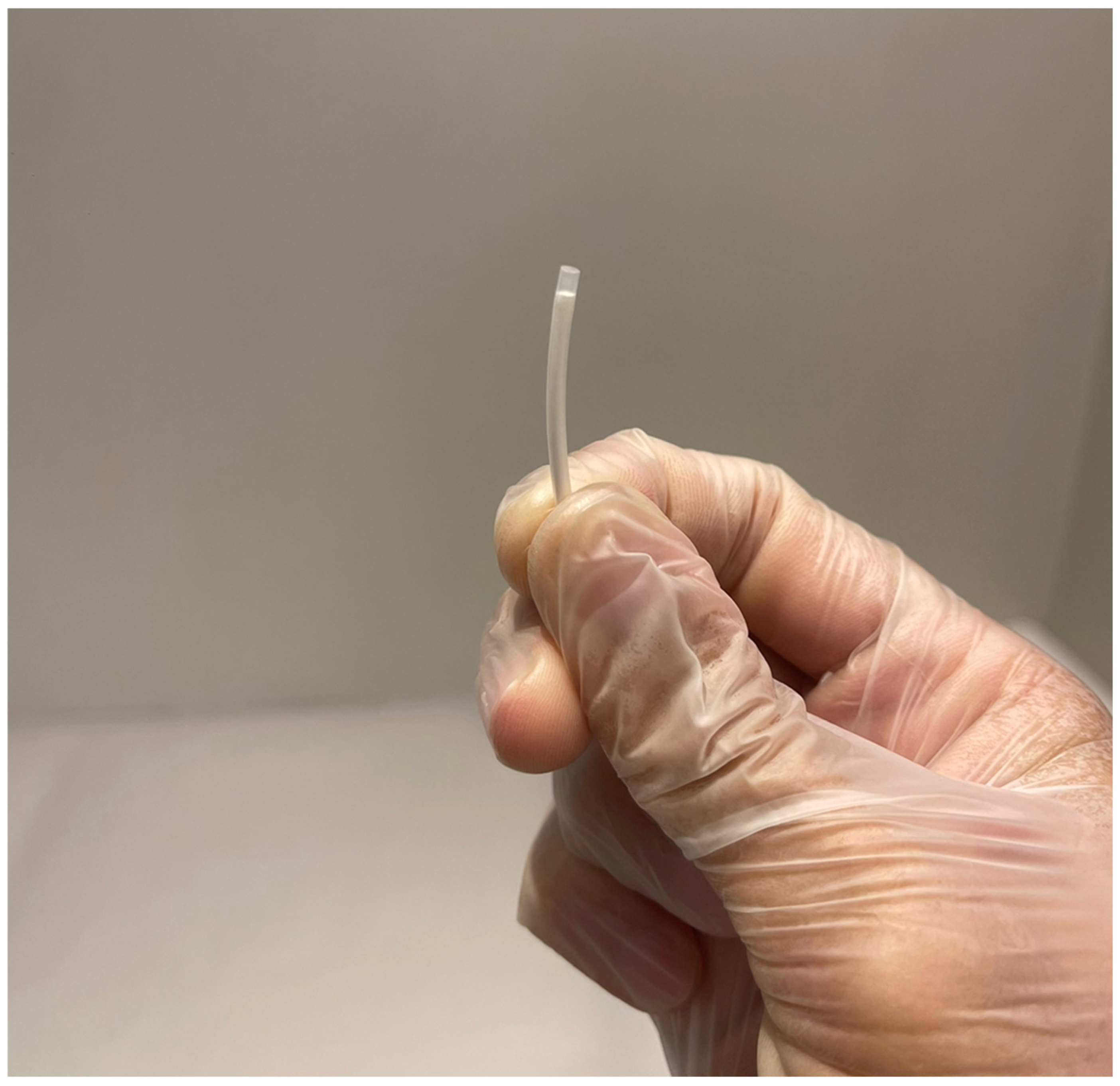
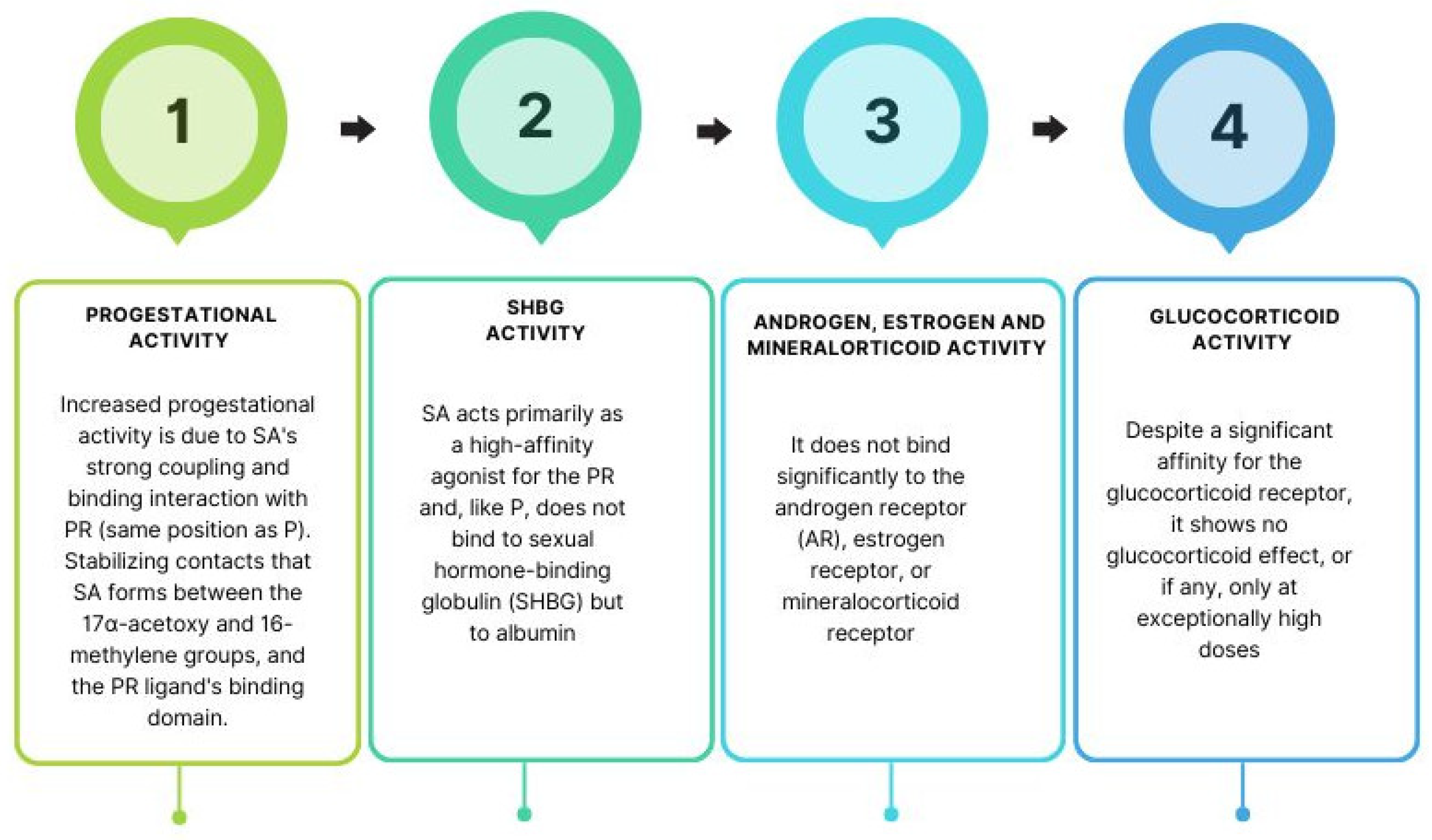
1.1. Subcutaneous SA Implant Therapy
Contraception
1.2. Endometriosis
1.3. Menopause
1.4. Advancing of SA as a Neuroprotective Drug
1.5. Limitations and Adverse Effects
2. Discussion
3. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ambacher, K.; Secter, M. The use of progestin subdermal implants in the management of endometriosis-related pain symptoms and quality of life: A systematic review. Curr. Med. Res. Opin. 2022, 38, 479–486. [Google Scholar] [CrossRef] [PubMed]
- Sitruk-Ware, R. Pharmacological profile of progestins. Maturitas 2004, 47, 277–283. [Google Scholar] [CrossRef] [PubMed]
- Kumar, N.; Koide, S.S. Nestorone: A progestin with a unique pharmacological profile. Steroids 2000, 65, 629–636. [Google Scholar] [CrossRef] [PubMed]
- Gemzell-Danielsson, K.; Sitruk-Ware, R. Segesterone acetate/ethinyl estradiol 12-month contraceptive vaginal system safety evaluation. Contraception 2019, 99, 323–328. [Google Scholar] [CrossRef]
- Weisberg, E.; Brache, V. Clinical performance and menstrual bleeding patterns with three dosage combinations of a Nestorone progestogen/ethynil estradiol contraceptive vaginal ring used on a bleeding-signaled regimen. Contraception 2005, 72, 46–52. [Google Scholar] [CrossRef]
- Sitruk-Ware, R.; Small, M. Nestorone: Clinical applications for contraception and HRT. Steroids 2003, 68, 907–913. [Google Scholar] [CrossRef]
- Stanczyk, F.Z.; Hapgood, J.P. Progestogens Used in Postmenopausal Hormone Therapy: Differences in Their Pharmacological Properties, Intracellular Actions, and Clinical Effects. Endocr. Rev. 2003, 34, 171–208. [Google Scholar] [CrossRef]
- Greenblatt, R.B.; Suran, R.R. Indications for Hormonal Pellets in the Therapy of Endocrine and Genetic Disorders. Am. J. Obstet. Gynecol. 1949, 57, 294–301. [Google Scholar] [CrossRef]
- Coutinho, E.M.; Da Silva, A.R. Contraceptive effectiveness of Silastic implants containing the progestin R-2323. Contraception 1975, 11, 625–635. [Google Scholar] [CrossRef]
- Bick, A.J.; Louw-du Toit, R.; Skosana, S.B.; Africander, D.; Hapgood, J.P. Pharmacokinetics, metabolism and serum concentrations of progestins used in contraception. Pharmacol. Ther. 2021, 222, 107789. [Google Scholar] [CrossRef]
- Brache, V.; Merkatz, R. A dose-finding, cross-over study to evaluate the effect of a Nestorone®/Estradiol transdermal gel delivery on ovulation suppression in normal ovulating women. Contraception 2015, 92, 289–297. [Google Scholar] [CrossRef] [PubMed]
- Haukkamaa, M.; Laurikka-Routti, M. Contraception with subdermal implants releasing the progestin ST-1435: A dose-finding study. Contraception 1992, 45, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Lähteenmäki, P.L.; Lähteenmäki, P. Concentration-dependent mechanisms of ovulation inhibition by the progestin ST-1435. Fertil. Steril. 1985, 44, 20–24. [Google Scholar] [CrossRef] [PubMed]
- Lähteenmäki, P.; Weiner, E. Pituitary and ovarian function during contraception with one subcutaneous implant releasing a progestin, ST-1435. Contraception 1982, 25, 299–306. [Google Scholar] [CrossRef]
- Mischell, S.; Cabrera, K. Barriers to and Facilitators of Contraceptive Implant Training in New Jersey Family Medicine Residencies: A Qualitative Study. Fam. Med. 2023, 55, 1–7. [Google Scholar] [CrossRef]
- Coutinho, E.M. One year contraception with a single subdermal implant containing nomegestrol acetate (Uniplant). Contraception 1993, 47, 97–105. [Google Scholar] [CrossRef]
- Coutinho, E.M.; da Silva, A.R.; Carreira, C.M. Long-term contraception with a single implant of the progestin ST-1435. Fertil. Steril. 1981, 36, 737–740. [Google Scholar] [CrossRef]
- Barbosa, I.; Coutinho, E. Effects of a single contraceptive Silastic implant containing nomegestrol acetate on ovarian function and cervical mucus production during 2 years. Fertil. Steril. 1996, 65, 724–729. [Google Scholar] [CrossRef]
- Renke, G.; Tostes, F. Cardiovascular Safety and Benefits of Testosterone Implant Therapy in Postmenopausal Women: Where Are We? Pharmaceuticals 2023, 16, 619. [Google Scholar] [CrossRef]
- Donovitz, G.S. Low complication rates of testosterone and estradiol implants for androgen and estrogen replacement therapy in over 1 million procedures. Ther. Adv. Endocrinol. Metab. 2021, 12, 1–11. [Google Scholar] [CrossRef]
- Archer, D.F. Efficacy of the 1-year (13-cycle) segesterone acetate and ethinylestradiol contraceptive vaginal system: Results of two multicentre, open-label, single-arm, phase 3 trials. Lancet Glob. Health 2019, 7, e1054–e1064. [Google Scholar] [CrossRef] [PubMed]
- Kumar, N.; Fagart, J. Nestorone® as a Novel Progestin for Nonoral Contraception: Structure-Activity Relationships and Brain Metabolism Studies. Endocrinology 2017, 158, 170–182. [Google Scholar] [CrossRef] [PubMed]
- Coutinho, E.M.; Athayde, C. Use of a single implant of elcometrine (ST-1435), a nonorally active progestin, as a long-acting contraceptive for postpartum nursing women. Contraception 1999, 59, 115–122. [Google Scholar] [CrossRef]
- Chen, S.; Kumar, N.; Mao, Z.B.; Sitruk-Ware, R.; Brinton, R.D. Therapeutic progestin segesterone acetate promotes neurogenesis. Menopause 2018, 25, 1138–1151. [Google Scholar] [CrossRef] [PubMed]
- Sivin, I.; Croxatto, H. Two-year performance of a Nestorone-releasing contraceptive implant: A three-center study of 300 women. Contraception 2004, 69, 137–144. [Google Scholar] [CrossRef]
- Krattenmacher, R. Drospirenone: Pharmacology and pharmacokinetics of a unique progestogen. Contraception 2000, 62, 29–38. [Google Scholar] [CrossRef]
- Zitzmann, M.; Rohayem, J. Impact of various progestins with or without transdermal testosterone on gonadotropin levels for non-invasive hormonal male contraception: A randomized clinical trial. Andrology 2017, 5, 516–526. [Google Scholar] [CrossRef]
- Long, J.E.; Lee, M.S. Update on Novel Hormonal and Nonhormonal Male Contraceptive Development. J. Clin. Endocrinol. Metab. 2021, 106, e2381–e2392. [Google Scholar] [CrossRef]
- Long, J.E.; Lee, M.S. Male Contraceptive Development: Update on Novel Hormonal and Nonhormonal Methods. Clin. Chem. 2019, 65, 153–160. [Google Scholar] [CrossRef]
- Thirumalai, A.; Amory, J.K. Emerging approaches to male contraception. Fertil. Steril. 2021, 115, 1369–1376. [Google Scholar] [CrossRef]
- Anawalt, B.D.; Roth, M.Y. Combined nestorone-testosterone gel suppresses serum gonadotropins to concentrations associated with effective hormonal contraception in men. Andrology 2019, 7, 878–887. [Google Scholar] [CrossRef] [PubMed]
- Yuen, F.; Wu, S. Preventing secondary exposure to women from men applying a novel nestorone/testosterone contraceptive gel. Andrology 2019, 7, 235–243. [Google Scholar] [CrossRef] [PubMed]
- Lue, Y.; Swerdloff, R. Male contraception development: Monitoring effective spermatogenesis suppression utilizing a user-controlled sperm concentration test compared with standard semen analysis. Fertil. Steril. 2023, 119, 208–217. [Google Scholar] [CrossRef] [PubMed]
- Ylänen, K.; Laatikainen, T. Subdermal progestin implant (Nestorone) in the treatment of endometriosis: Clinical response to various doses. Acta Obstet. Gynecol. Scand. 2003, 82, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Heidari, M.; Ghodusi, M.; Rezaei, P.; Abyaneh, S.K.; Sureshjani, E.H.; Sheikhi, R.A. Sexual Function and Factors Affecting Menopause: A Systematic Review. J. Menopausal Med. 2019, 25, 15. [Google Scholar] [CrossRef]
- Pardini, D. Hormone replacement therapy in menopause. Arq. Bras. Endocrinol. Metabol. 2014, 58, 172–181. [Google Scholar] [CrossRef]
- Hill, D.A.; Crider, M. Hormone Therapy and Other Treatments for Symptoms of Menopause. Am. Fam. Physician 2016, 94, 884–889. [Google Scholar]
- Manica, D.; Nucci, M. Sob a pele: Implantes subcutâneos, hormônios e gênero. Horiz. Antropológicos 2017, 23, 93–129. [Google Scholar] [CrossRef][Green Version]
- Renke, G.; Kemen, E. Cardio-Metabolic Health and HRT in Menopause: Novel Insights in Mitochondrial Biogenesis and RAAS. Curr. Cardiol. Rev. 2023, 19, e060223213459. [Google Scholar] [CrossRef]
- Cho, L.; Kaunitz, A.M. Rethinking Menopausal Hormone Therapy: For Whom, What, When, and How Long? Circulation 2023, 147, 597–610. [Google Scholar] [CrossRef]
- Anand, D.A.; Chitterusu, R.R. Cardioprotective function of progesterone: A new perspective. Natl. J. Physiol. Pharm. Pharmacol. 2017, 7, 136–142. [Google Scholar]
- Pramod, V.P. Cardioprotection: A Neo-Perspective for Clinical Implication of Nestorone®. J. Gynecol. Women’s Health 2017, 5, 555652. [Google Scholar] [CrossRef]
- Sitruk-Ware, R.; Bonsack, B. Progress in progestin-based therapies for neurological disorders. Neurosci. Biobehav. Rev. 2021, 122, 38–65. [Google Scholar] [CrossRef]
- Tuazon, J.P.; Sitruk-Ware, R.; Borlongan, C.V. Beyond contraception and hormone replacement therapy: Advancing Nestorone to a neuroprotective drug in the clinic. Brain Res. 2019, 1704, 161–163. [Google Scholar] [CrossRef]
- Liu, L.; Zhao, L. Clinically relevant progestins regulate neurogenic and neuroprotective responses in vitro and in vivo. Endocrinology 2010, 151, 5782–5794. [Google Scholar] [CrossRef] [PubMed]
- Fréchou, M.; Zhu, X. Sex differences in the cerebroprotection by Nestorone intranasal delivery following stroke in mice. Neuropharmacology 2021, 198, 108760. [Google Scholar] [CrossRef]
- Castelnovo, L.F.; Thomas, P. Progesterone exerts a neuroprotective action in a Parkinson’s disease human cell model through membrane progesterone receptor alpha (mPRalpha/PAQR7). Front. Endocrinol. 2023, 14, 1125962. [Google Scholar] [CrossRef]
- Lee, A.L. Segesterone Acetate and Ethinyl Estradiol Vaginal Ring (Annovera) for Contraception. Am. Fam. Physician 2020, 101, 618–620. [Google Scholar]
- Nelson, A.L. Comprehensive overview of the recently FDA-approved contraceptive vaginal ring releasing segesterone acetate and ethinylestradiol: A new year-long, patient controlled, reversible birth control method. Expert. Rev. Clin. Pharmacol. 2019, 12, 953–963. [Google Scholar] [CrossRef]
- Paton, D.M. Contraceptive vaginal ring containing segesterone acetate and ethinyl estradiol: Long-acting, patient-controlled, procedure-free, reversible prescription birth control. Drugs Today 2019, 55, 449–457. [Google Scholar] [CrossRef] [PubMed]
| Author(s), Year, Reference Number | SA Dose | Characteristics of Study/Participants | Results |
|---|---|---|---|
| Gemzell-Danielsson et al. (2019) [4] | CVS releasing an average of SA 150 mcg and EE 13 mcg daily. | A 12-month prospective study, including 3052 pre-menopausal women. | The 1-year SA/EE CVS has an acceptable safety profile. |
| Weisberg et al. (2005) [5] | CVS releasing 50 mcg/day of SA and either 10 (50/10) or 20 (50/20) mcg/day of EE. | A 6-month prospective study, two-stage trial, including 246 pre-menopause women. | CVS used with a bleeding-signaled regimen led to few terminations attributed to bleeding problems and to acceptable continuation rates. |
| Brache et al. (2015) [11] | Transdermal gel with doses of 1.5 mg SA/0.5 mg E2, 3.0 mg SA/1.0 mg E2, and 4.5 mg SA/1.5 mg E2). Participants applied gel daily on the abdomen for 21 consecutive days. | A randomized, open-label, three-treatment-period cross-over study, including 18 pre-menopausal women, to evaluate the effects of SA/E2 transdermal gel. | All three doses of SA/E2 transdermal gel blocked ovulation effectively with good safety and acceptable profile. |
| Lähteenmäki et al. (1985) [13] | Contraceptive SA subcutaneous silastic implant containing 20 mg or 40 mg. | A prospective study with 18 pre-menopausal women. | Both single subcutaneous implants of SA with 20 or 40 mg cause ovulation inhibition, decreasing the plasma LH/FSH ratio. |
| Coutinho et al. (1981) [17] | Contraceptive SA subcutaneous silastic implant containing 35 mg. | A prospective study with 282 pre-menopausal women. | The single subcutaneous implant of SA presents full protection for a period of 6 months or longer,
providing an alternative for long-acting injectable contraceptives. |
| Archer et al. (2019) [21] | CVS designed to last 1 year (13 cycles), delivering a daily average of 0.15 mg SA and 0.013 mg EE. | A multicentre, open-label, single-arm study with 2278 pre-menopausal women. | The SA and EE CVS is an effective contraceptive for 13 consecutive cycles of use with an excellent safety profile. |
| Coutinho et al. (1999) [23] | Contraceptive SA subcutaneous silastic implant containing 50 mg. | A prospective study with 135 pre-menopausal women (66 breast-feeding women receiving SA implants and 69 women who chose to use Copper-T380 IUD as control subjects). | A single SA silastic implant placed subcutaneously at 6-month intervals appears to be an effective method of contraception for lactating women and results in blood concentrations of nursing infants at or near undetectable levels. |
| Silvin et al. (2005) [25] | Contraceptive SA subcutaneous silastic implant containing 92.7 mg ± 2.4 mg. | A 2-year multicentre prospective study enrolling 300 pre-menopausal women in Latin America. | The 2-year cumulative pregnancy rate was 1.7 per 100, with a Pearl index of 0.6 per 100 for the 2-year period. The 1-year and 2-year continuation rates were 80.5 and 66.7 per 100, respectively. |
| Ylänen et al. (2003) [34] | Two to four SA implants were inserted subcutaneously for 7 months. Each implant contained 15 mg, 20 mg, or 40 mg of SA. | A prospective study with 21 pre-menopausal women in whom endometriosis was diagnosed and treated. | All three doses of SA silastic implant effectively alleviated endometriosis-related pain. No significant changes in the serum levels of total, HDL, or LDL cholesterol were observed. |
| Application | Ref. |
|---|---|
| Neuroprotection | [43,44,45,46,47] |
| Female Contraception | [1,2,3,4,5,6,7,12,21,22,23,24,25,26,48,49,50] |
| Male Contraception | [27,28,29,30,31,32,33] |
| PCOS | [3,21,26] |
| Menopause | [19,20,35,36,37,38,39,40,41,42,43,44] |
| Endometriosis | [1,3,34] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Renke, G.; Callizo, C.; Paes, R.; Antunes, M.; Michels, G.; Concha, L.; Almeida, O.; Valente, C.; Baesso, T.; Giovannoni, B. Clinical Approaches to Nestorone Subdermal Implant Therapy in Women’s Health. Biomedicines 2023, 11, 2586. https://doi.org/10.3390/biomedicines11092586
Renke G, Callizo C, Paes R, Antunes M, Michels G, Concha L, Almeida O, Valente C, Baesso T, Giovannoni B. Clinical Approaches to Nestorone Subdermal Implant Therapy in Women’s Health. Biomedicines. 2023; 11(9):2586. https://doi.org/10.3390/biomedicines11092586
Chicago/Turabian StyleRenke, Guilherme, Consuelo Callizo, Raphaela Paes, Mariana Antunes, Glaycon Michels, Luana Concha, Ordânio Almeida, Christiane Valente, Thomaz Baesso, and Bruna Giovannoni. 2023. "Clinical Approaches to Nestorone Subdermal Implant Therapy in Women’s Health" Biomedicines 11, no. 9: 2586. https://doi.org/10.3390/biomedicines11092586
APA StyleRenke, G., Callizo, C., Paes, R., Antunes, M., Michels, G., Concha, L., Almeida, O., Valente, C., Baesso, T., & Giovannoni, B. (2023). Clinical Approaches to Nestorone Subdermal Implant Therapy in Women’s Health. Biomedicines, 11(9), 2586. https://doi.org/10.3390/biomedicines11092586







