Role of Cardio-Renal Dysfunction, Inflammation Markers, and Frailty on In-Hospital Mortality in Older COVID-19 Patients: A Cluster Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Ethics Statement
2.3. Clinical Parameters
2.4. Statistical Analysis
3. Results
3.1. General Characteristics and Cluster Characterization
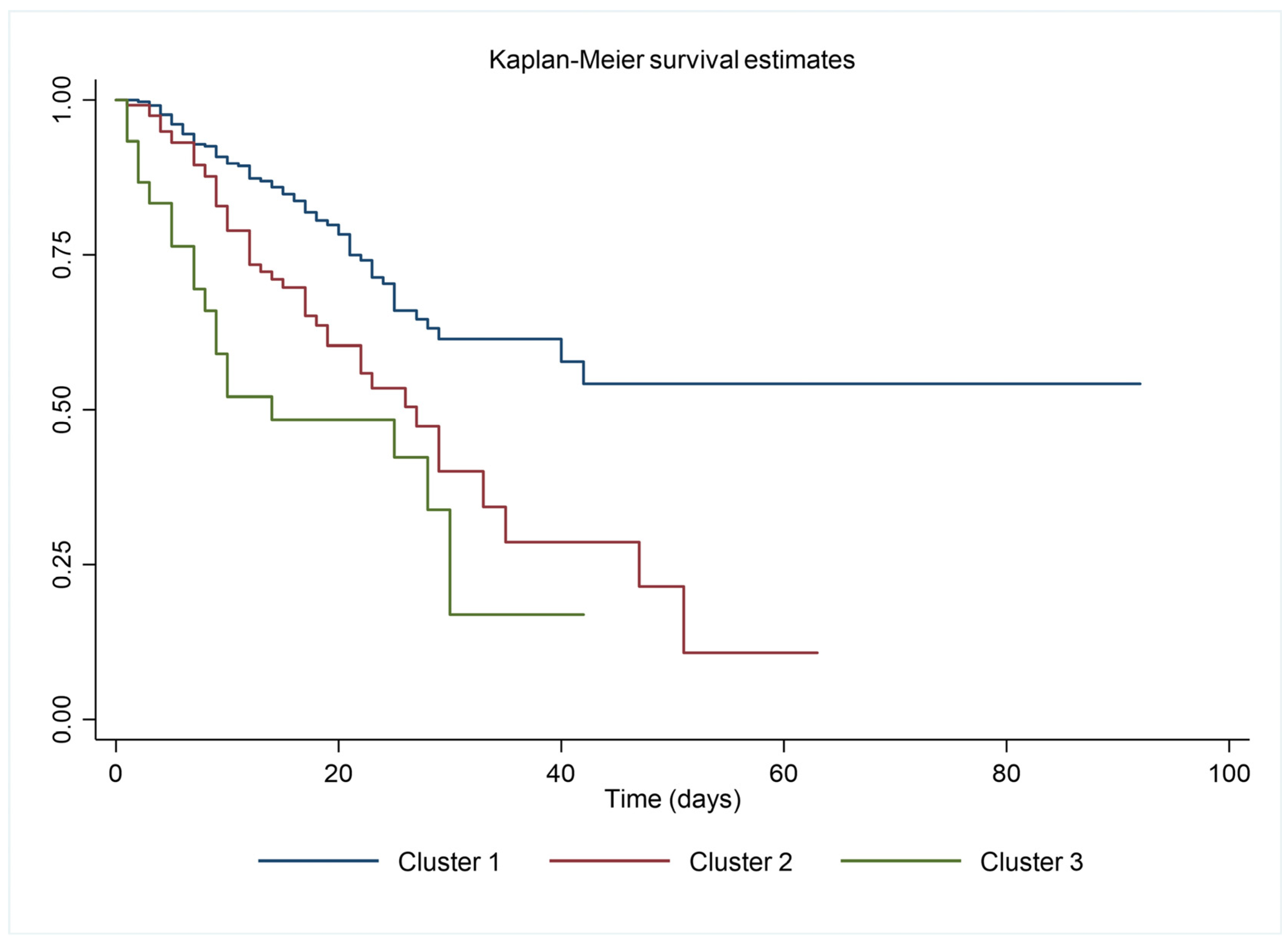
3.2. In-Hospital Mortality
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sarzani, R.; Allevi, M.; Giulietti, F.; Di Pentima, C.; Re, S.; Giordano, P.; Spannella, F. The Identikit of Patient at Risk for Severe COVID-19 and Death: The Dysregulation of Renin-Angiotensin System as the Common Theme. J. Clin. Med. 2021, 10, 5883. [Google Scholar] [CrossRef]
- Corradini, E.; Ventura, P.; Ageno, W.; Cogliati, C.B.; Muiesan, M.L.; Girelli, D.; Pirisi, M.; Gasbarrini, A.; Angeli, P.; Querini, P.R.; et al. Clinical factors associated with death in 3044 COVID-19 patients managed in internal medicine wards in Italy: Results from the SIMI-COVID-19 study of the Italian Society of Internal Medicine (SIMI). Intern. Emerg. Med. 2021, 16, 1005–1015. [Google Scholar] [CrossRef]
- Wei, C.; Liu, Y.; Liu, Y.; Zhang, K.; Su, D.; Zhong, M.; Meng, X. Clinical characteristics and manifestations in older patients with COVID-19. BMC Geriatr. 2020, 20, 395. [Google Scholar] [CrossRef]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Sarzani, R.; Spannella, F.; Giulietti, F.; Fedecostante, M.; Giordano, P.; Gattafoni, P.; Espinosa, E.; Busco, F.; Piccinini, G.; Dessi-Fulgheri, P. NT-proBNP and its correlation with in-hospital mortality in the very elderly without an admission diagnosis of heart failure. PLoS ONE 2016, 11, e0153759. [Google Scholar] [CrossRef] [PubMed]
- Bhatt, A.S.; Jering, K.S.; Vaduganathan, M.; Claggett, B.L.; Cunningham, J.W.; Rosenthal, N.; Signorovitch, J.; Thune, J.J.; Vardeny, O.; Solomon, S.D. Clinical Outcomes in Patients With Heart Failure Hospitalized With COVID-19. JACC Heart Fail. 2021, 9, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Franczuk, P.; Tkaczyszyn, M.; Kulak, M.; Domenico, E.; Ponikowski, P.; Jankowska, E.A. Cardiovascular Complications of Viral Respiratory Infections and COVID-19. Biomedicines 2022, 11, 71. [Google Scholar] [CrossRef]
- Becerra-Muñoz, V.M.; Núñez-Gil, I.J.; Eid, C.M.; García Aguado, M.; Romero, R.; Huang, J.; Mulet, A.; Ugo, F.; Rametta, F.; Liebetrau, C.; et al. Clinical profile and predictors of in-hospital mortality among older patients hospitalised for COVID-19. Age Ageing 2021, 50, 326–334. [Google Scholar] [CrossRef] [PubMed]
- Olivieri, F.; Sabbatinelli, J.; Bonfigli, A.R.; Sarzani, R.; Giordano, P.; Cherubini, A.; Antonicelli, R.; Rosati, Y.; Prete, S.D.; Rosa, M.D.; et al. Routine laboratory parameters, including complete blood count, predict COVID-19 in-hospital mortality in geriatric patients. Mech. Ageing Dev. 2022, 204, 111674. [Google Scholar] [CrossRef]
- Kastora, S.; Kounidas, G.; Perrott, S.; Carter, B.; Hewitt, J.; Myint, P.K. Clinical frailty scale as a point of care prognostic indicator of mortality in COVID-19: A systematic review and meta-analysis. eClinicalMedicine 2021, 36, 100896. [Google Scholar] [CrossRef]
- Polidori, M.C.; Sies, H.; Ferrucci, L.; Benzing, T. COVID-19 mortality as a fingerprint of biological age. Ageing Res. Rev. 2021, 67, 101308. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef] [PubMed]
- Rockwood, K.; Theou, O. Using the Clinical Frailty Scale in Allocating Scarce Health Care Resources. Can. Geriatr. J. 2020, 23, 210–215. [Google Scholar] [CrossRef]
- Dadras, O.; SeyedAlinaghi, S.; Karimi, A.; Shamsabadi, A.; Qaderi, K.; Ramezani, M.; Mirghaderi, S.P.; Mahdiabadi, S.; Vahedi, F.; Saeidi, S.; et al. COVID-19 mortality and its predictors in the elderly: A systematic review. Health Sci. Rep. 2022, 5, e657. [Google Scholar] [CrossRef]
- Damayanthi, H.D.W.T.; Prabani, K.I.P.; Weerasekara, I. Factors Associated for Mortality of Older People With COVID 19: A Systematic Review and Meta-analysis. Gerontol. Geriatr. Med. 2021, 7, 23337214211057390. [Google Scholar] [CrossRef]
- Mahmoud, M.; Carmisciano, L.; Tagliafico, L.; Muzyka, M.; Rosa, G.; Signori, A.; Bassetti, M.; Nencioni, A.; Monacelli, F. Patterns of Comorbidity and In-Hospital Mortality in Older Patients With COVID-19 Infection. Front. Med. 2021, 8, 726837. [Google Scholar] [CrossRef] [PubMed]
- Kadowaki, T.; Maegawa, H.; Watada, H.; Yabe, D.; Node, K.; Murohara, T.; Wada, J. Interconnection between cardiovascular, renal and metabolic disorders: A narrative review with a focus on Japan. Diabetes Obes. Metab. 2022, 24, 2283–2296. [Google Scholar] [CrossRef] [PubMed]
- Marini, S.; Georgakis, M.K.; Anderson, C.D. Interactions Between Kidney Function and Cerebrovascular Disease: Vessel Pathology That Fires Together Wires Together. Front. Neurol. 2021, 12, 785273. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; Wu, D.; Chen, H.; Yan, W.; Yang, D.; Chen, G.; Ma, K.; Xu, D.; Yu, H.; Wang, H.; et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: Retrospective study. BMJ 2020, 368, m1091. [Google Scholar] [CrossRef]
- Henry, B.M.; de Oliveira, M.H.S.; Benoit, S.; Plebani, M.; Lippi, G. Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): A meta-analysis. Clin. Chem. Lab. Med. 2020, 58, 1021–1028. [Google Scholar] [CrossRef]
- O’Donnell, C.; Ashland, M.D.; Vasti, E.C.; Lu, Y.; Chang, A.Y.; Wang, P.; Daniels, L.B.; de Lemos, J.A.; Morrow, D.A.; Rodriguez, F.; et al. N-Terminal Pro-B-Type Natriuretic Peptide as a Biomarker for the Severity and Outcomes With COVID-19 in a Nationwide Hospitalized Cohort. J. Am. Heart Assoc. 2021, 10, e022913. [Google Scholar] [CrossRef] [PubMed]
- Shi, S.; Qin, M.; Shen, B.; Cai, Y.; Liu, T.; Yang, F.; Gong, W.; Liu, X.; Liang, J.; Zhao, Q.; et al. Association of Cardiac Injury With Mortality in Hospitalized Patients With COVID-19 in Wuhan, China. JAMA Cardiol. 2020, 5, 802–810. [Google Scholar] [CrossRef] [PubMed]
- Orlando, L.; Bagnato, G.; Ioppolo, C.; Franzè, M.S.; Perticone, M.; Versace, A.G.; Sciacqua, A.; Russo, V.; Cicero, A.F.G.; De Gaetano, A.; et al. Natural Course of COVID-19 and Independent Predictors of Mortality. Biomedicines 2023, 11, 939. [Google Scholar] [CrossRef] [PubMed]
- Caro-Codón, J.; Rey, J.R.; Buño, A.; Iniesta, A.M.; Rosillo, S.O.; Castrejon-Castrejon, S.; Rodriguez-Sotelo, L.; Martinez, L.A.; Marco, I.; Merino, C.; et al. Characterization of NT-proBNP in a large cohort of COVID-19 patients. Eur. J. Heart Fail. 2021, 23, 456–464. [Google Scholar] [CrossRef] [PubMed]
- Rath, D.; Petersen-Uribe, Á.; Avdiu, A.; Witzel, K.; Jaeger, P.; Zdanyte, M.; Heinzmann, D.; Tavlaki, E.; Müller, K.; Gawaz, M.P. Impaired cardiac function is associated with mortality in patients with acute COVID-19 infection. Clin. Res. Cardiol. 2020, 109, 1491–1499. [Google Scholar] [CrossRef] [PubMed]
- Palazzuoli, A.; Beltrami, M.; McCullough, P.A. Acute COVID-19 Management in Heart Failure Patients: A Specific Setting Requiring Detailed Inpatient and Outpatient Hospital Care. Biomedicines 2023, 11, 790. [Google Scholar] [CrossRef]
- Basso, C.; Leone, O.; Rizzo, S.; De Gaspari, M.; van der Wal, A.C.; Aubry, M.-C.; Bois, M.C.; Lin, P.T.; Maleszewski, J.J.; Stone, J.R. Pathological features of COVID-19-associated myocardial injury: A multicentre cardiovascular pathology study. Eur. Heart J. 2020, 41, 3827–3835. [Google Scholar] [CrossRef] [PubMed]
- Tsutsui, H.; Albert, N.M.; Coats, A.J.S.; Anker, S.D.; Bayes-Genis, A.; Butler, J.; Chioncel, O.; Defilippi, C.R.; Drazner, M.H.; Felker, G.M.; et al. Natriuretic peptides: Role in the diagnosis and management of heart failure: A scientific statement from the Heart Failure Association of the European Society of Cardiology, Heart Failure Society of America and Japanese Heart Failure Society. Eur. J. Heart Fail. 2023, 25, 616–631. [Google Scholar] [CrossRef] [PubMed]
- Cai, X.; Wu, G.; Zhang, J.; Yang, L. Risk Factors for Acute Kidney Injury in Adult Patients With COVID-19: A Systematic Review and Meta-Analysis. Front. Med. 2021, 8, 719472. [Google Scholar] [CrossRef]
- Wang, B.; Luo, Q.; Zhang, W.; Yu, S.; Cheng, X.; Wang, L.; Chen, X.; Chen, Y. The Involvement of Chronic Kidney Disease and Acute Kidney Injury in Disease Severity and Mortality in Patients with COVID-19: A Meta-Analysis. Kidney Blood Press. Res. 2021, 46, 17–30. [Google Scholar] [CrossRef]
- Zheng, X.; Yang, H.; Li, X.; Li, H.; Xu, L.; Yu, Q.; Dong, Y.; Zhao, Y.; Wang, J.; Hou, W.; et al. Prevalence of Kidney Injury and Associations with Critical Illness and Death in Patients with COVID-19. Clin. J. Am. Soc. Nephrol. 2020, 15, 1549–1556. [Google Scholar] [CrossRef]
- Asgharpour, M.; Zare, E.; Mubarak, M.; Alirezaei, A. COVID-19 and Kidney Disease: Update on Epidemiology, Clinical Manifestations, Pathophysiology and Management. J. Coll. Physicians Surg. Pak. 2020, 30, 19–25. [Google Scholar] [PubMed]
- Cheng, Y.; Luo, R.; Wang, K.; Zhang, M.; Wang, Z.; Dong, L.; Li, J.; Yao, Y.; Ge, S.; Xu, G. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020, 97, 829–838. [Google Scholar] [CrossRef]
- Luo, X.; Zhou, W.; Yan, X.; Guo, T.; Wang, B.; Xia, H.; Ye, L.; Xiong, J.; Jiang, Z.; Liu, Y.; et al. Prognostic Value of C-Reactive Protein in Patients With Coronavirus 2019. Clin. Infect. Dis. 2020, 71, 2174–2179. [Google Scholar] [CrossRef] [PubMed]
- Ji, P.; Zhu, J.; Zhong, Z.; Li, H.; Pang, J.; Li, B.; Zhang, J. Association of elevated inflammatory markers and severe COVID-19: A meta-analysis. Medicine 2020, 99, e23315. [Google Scholar] [CrossRef]
- Vijay, S.; Bansal, N.; Rao, B.K.; Veeraraghavan, B.; Rodrigues, C.; Wattal, C.; Goyal, J.P.; Tadepalli, K.; Mathur, P.; Venkateswaran, R.; et al. Secondary Infections in Hospitalized COVID-19 Patients: Indian Experience. Infect. Drug Resist. 2021, 14, 1893–1903. [Google Scholar] [CrossRef] [PubMed]
- Saragih, I.D.; Advani, S.; Saragih, I.S.; Suarilah, I.; Susanto, I.; Lin, C.-J. Frailty as a mortality predictor in older adults with COVID-19: A systematic review and meta-analysis of cohort studies. Geriatr. Nurs. 2021, 42, 983–992. [Google Scholar] [CrossRef]
- Marengoni, A.; Zucchelli, A.; Vetrano, D.L.; Armellini, A.; Botteri, E.; Nicosia, F.; Romanelli, G.; Beindorf, E.A.; Giansiracusa, P.; Garrafa, E.; et al. Beyond Chronological Age: Frailty and Multimorbidity Predict In-Hospital Mortality in Patients With Coronavirus Disease 2019. J. Gerontol. A Biol. Sci. Med. Sci. 2021, 76, e38–e45. [Google Scholar] [CrossRef]
| Total | Cluster 1 | Cluster 2 | Cluster 3 | p | |
|---|---|---|---|---|---|
| N = 485 | N = 337 | N = 118 | N = 30 | ||
| Female sex | 287 (59.2%) | 205 (60.8%) | 64 (54.2%) | 18 (60.0%) | 0.453 |
| Age | 87 (83–91) | 86 (82–90) | 89 (84–94) | 88 (84–91) | <0.001 |
| CFS | 6 (4–8) | 6 (4–8) | 7 (4–8) | 7 (6–8) | 0.025 |
| Comorbidities | |||||
| Diabetes Mellitus | 100 (20.6%) | 63 (18.7%) | 33 (28%) | 4 (13.3%) | 0.060 |
| Hypertension | 318 (65.6%) | 211 (62.6%) | 90 (76.3%) | 17 (56.7%) | 0.015 |
| Atrial Fibrillation | 130 (26.8%) | 64 (19%) | 52 (44.1%) | 14 (46.7%) | <0.001 |
| Dementia | 168 (34.6%) | 111 (32.9%) | 45 (38.1%) | 12 (40%) | 0.485 |
| Chronic Lung Diseases | 70 (14.4%) | 44 (13.1%) | 22 (18.6%) | 4 (13.3%) | 0.326 |
| Myocardial Infarction | 7 (1.4%) | 2 (0.6%) | 4 (3.4%) | 1 (3.3%) | 0.061 |
| Concurrent Bacterial Infection | 25 (5.2%) | 13 (3.9%) | 8 (6.8%) | 4 (13.3%) | 0.052 |
| Stroke | 33 (6.8%) | 21 (6.2%) | 9 (7.6%) | 3 (10%) | 0.676 |
| Dyslipidemia | 160 (33%) | 114 (33.8%) | 35 (29.7%) | 11 (36.7%) | 0.643 |
| Charlson Index (points) | 1 (0–2) | 1 (0–1) | 1 (0–2) | 1 (0–2) | 0.032 |
| Lab Parameters | |||||
| NT-proBNP (pg/mL) | 1541 (569–4174) | 830 (376–1627) | 5302.5 (4260–8512) | 29,480.5 (21,250–40,161) | <0.001 |
| Creatinine (mg/dL) | 1.03 (0.66–1.45) | 1.08 (0.72–1.5) | 0.92 (0.58–1.29) | 0.91 (0.57–1.2) | 0.008 |
| eGFR (ml/min/1.73 m2) | 69 (45–84) | 79 (56–86) | 47 (30–74) | 33.5 (18–49) | <0.001 |
| Neutrophil count (n/microl) | 6.14 (4.35–9.4) | 5.92 (4.28–8.67) | 6.665 (4.53–10.61) | 6.88 (4.56–11.31) | 0.095 |
| CRP (mg/dL) | 3.65 (1.31–8.44) | 3.06 (1.17–7.54) | 4.31 (1.89–10.01) | 6.66 (2.19–13.07) | 0.003 |
| Systolic BP (mmHg) | 135.5 ± 21.5 | 136.9 ± 20.5 | 134.9 ± 22.7 | 122.2 ± 24.5 | 0.203 |
| End-points | |||||
| Length of stay (days) | 14 (9–22) | 14 (9–22) | 13.5 (9–21) | 10.5 (5–25) | 0.437 |
| In-hospital mortality | 138 (28.5%) | 71 (21.1%) | 48 (40.7%) | 19 (63.3%) | <0.001 |
| HR (95%CI) | |
|---|---|
| Comorbidities | |
| Diabetes Mellitus | 0.86 (0.54–1.37) |
| Hypertension | 0.82 (0.54–1.24) |
| Atrial Fibrillation | 1.34 (0.90–1.99) |
| Dementia | 1.01 (0.68–1.50) |
| Chronic Lung Diseases | 1.43 (0.91–2.23) |
| Myocardial Infarction | 1.49 (0.37–6.08) |
| Concurrent Bacterial Infection | 0.77 (0.37–1.59) |
| Stroke | 0.68 (0.32–1.48) |
| Dyslipidemia | 0.64 (0.41–0.99) |
| Lab Parameters | |
| NT-proBNP (pg/mL) | 1.000028 (1.000015–1.000041) |
| Creatinine (mg/dL) | 1.11 (1.04–1.19) |
| Neutrophil count (n/microl) | 1.10 (1.07–1.13) |
| eGFR (ml/min/1.73 m2) | 0.98 (0.97–0.99) |
| CRP (mg/dL) | 1.07 (1.05–1.10) |
| Systolic BP (mmHg) | 0.99 (0.98–1.00) |
| Cluster (ref. 1) | |
| 2 | 1.96 (1.28–3.01) |
| 3 | 2.87 (1.62–5.07) |
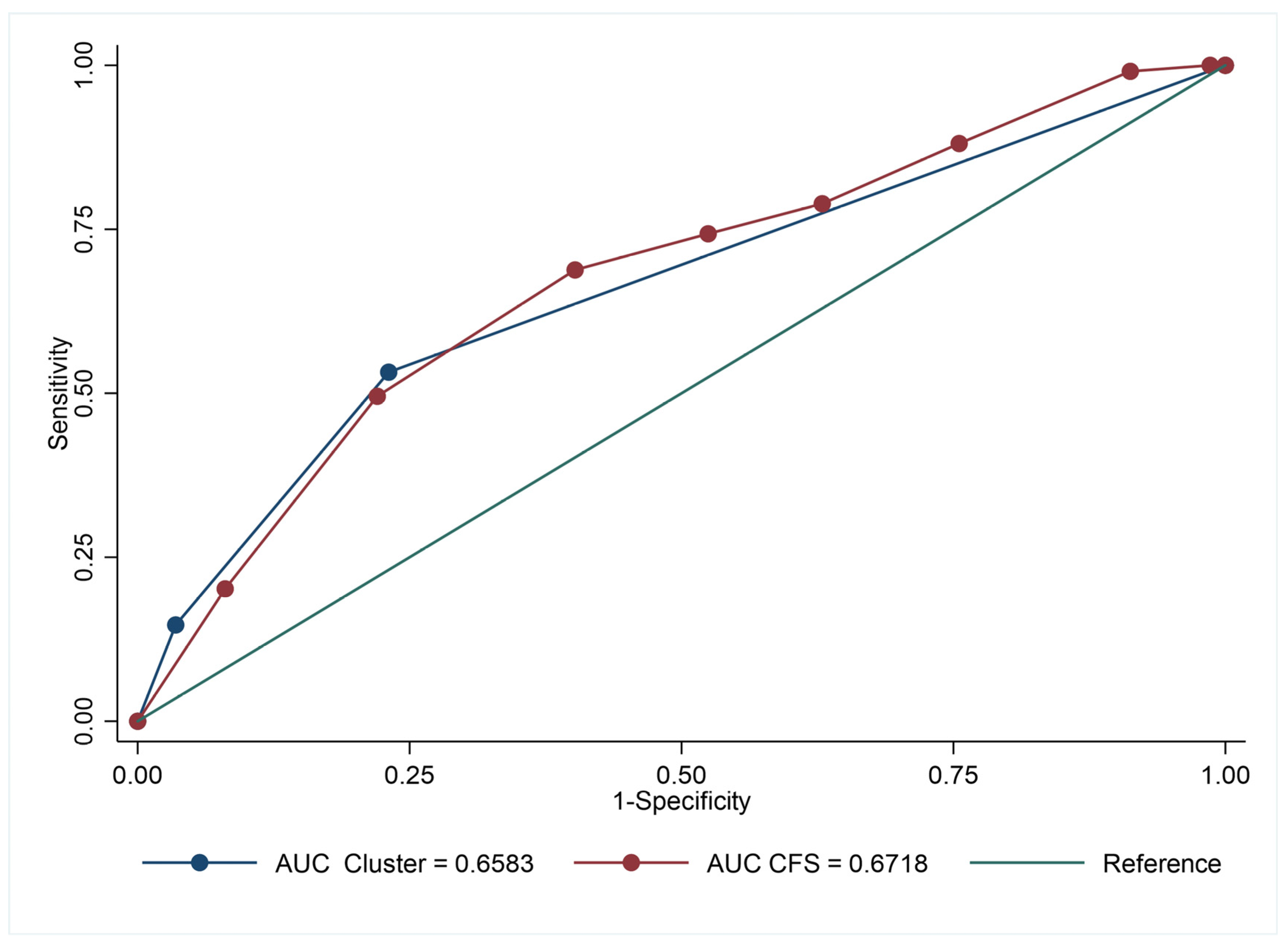
| Outcome | Addition | AUC (95% CI) | Overall NRI (95%CI) | ΔAUC (95%CI) | p |
|---|---|---|---|---|---|
| Death (n = 138) | 0.60 (0.54–0.66) | ||||
| CFS | 0.57 (0.24–0.76) | 0.12 (0.07–0.17) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Spannella, F.; Giulietti, F.; Laureti, G.; Di Rosa, M.; Di Pentima, C.; Allevi, M.; Garbuglia, C.; Giordano, P.; Landolfo, M.; Ferrara, L.; et al. Role of Cardio-Renal Dysfunction, Inflammation Markers, and Frailty on In-Hospital Mortality in Older COVID-19 Patients: A Cluster Analysis. Biomedicines 2023, 11, 2473. https://doi.org/10.3390/biomedicines11092473
Spannella F, Giulietti F, Laureti G, Di Rosa M, Di Pentima C, Allevi M, Garbuglia C, Giordano P, Landolfo M, Ferrara L, et al. Role of Cardio-Renal Dysfunction, Inflammation Markers, and Frailty on In-Hospital Mortality in Older COVID-19 Patients: A Cluster Analysis. Biomedicines. 2023; 11(9):2473. https://doi.org/10.3390/biomedicines11092473
Chicago/Turabian StyleSpannella, Francesco, Federico Giulietti, Giorgia Laureti, Mirko Di Rosa, Chiara Di Pentima, Massimiliano Allevi, Caterina Garbuglia, Piero Giordano, Matteo Landolfo, Letizia Ferrara, and et al. 2023. "Role of Cardio-Renal Dysfunction, Inflammation Markers, and Frailty on In-Hospital Mortality in Older COVID-19 Patients: A Cluster Analysis" Biomedicines 11, no. 9: 2473. https://doi.org/10.3390/biomedicines11092473
APA StyleSpannella, F., Giulietti, F., Laureti, G., Di Rosa, M., Di Pentima, C., Allevi, M., Garbuglia, C., Giordano, P., Landolfo, M., Ferrara, L., Fumagalli, A., Lattanzio, F., Bonfigli, A. R., & Sarzani, R. (2023). Role of Cardio-Renal Dysfunction, Inflammation Markers, and Frailty on In-Hospital Mortality in Older COVID-19 Patients: A Cluster Analysis. Biomedicines, 11(9), 2473. https://doi.org/10.3390/biomedicines11092473






