Effect of Vitamin D3 on Depressive Behaviors of Rats Exposed to Chronic Unpredictable Mild Stress
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Animals
2.2. Ethical Considerations
2.3. Experimental Design
2.4. Drugs and Chemicals
2.5. Chronic Unpredictable Mild Stress Model
2.6. Behavioral Tests
2.6.1. Sucrose Preference Test (SPT)
2.6.2. Forced Swimming Test (FST)
2.6.3. Tail Suspension Test (TST)
2.6.4. Open Field Test (OFT)
2.6.5. Elevated Plus Maze Test (EPM)
2.7. Blood Collection and Analysis
2.8. Statistical Analysis
3. Results
3.1. Pre-Experiment Weight and Behavioral Tests
3.2. Post-Experiment Weight and Behavioral Tests
3.3. Differences within Each Group
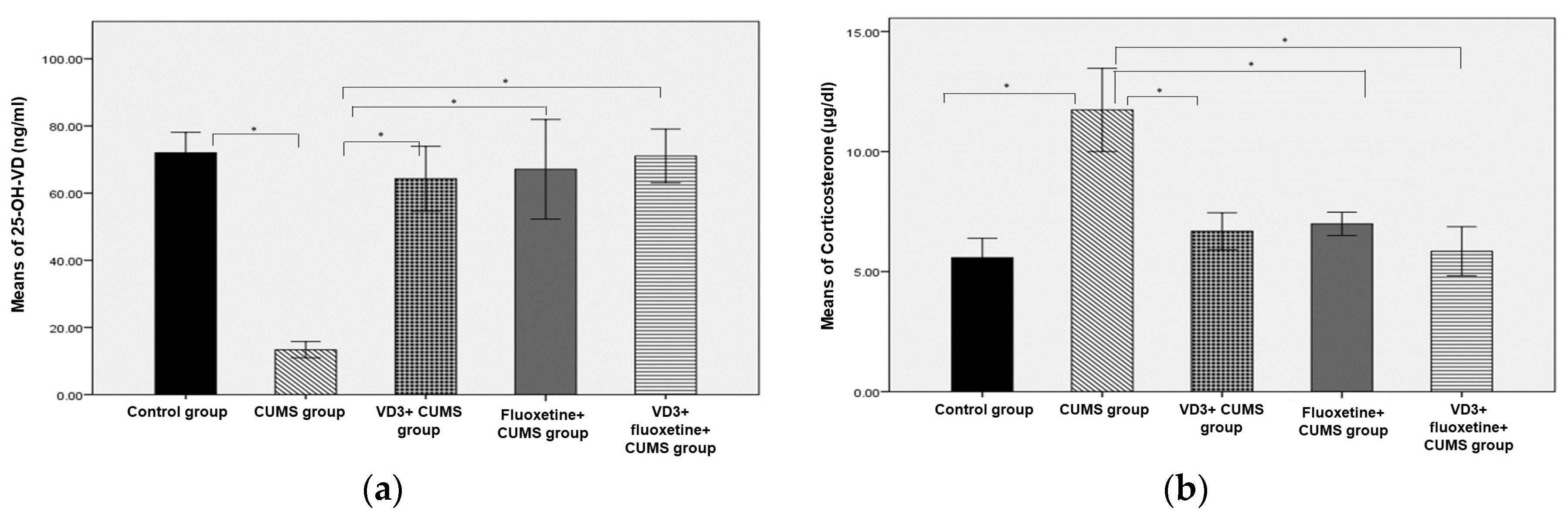
3.4. Corticosterone Hormone and Vitamin D
3.5. Correlation Analysis of Serum 25-OH-VD and Behavioral Tests
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Mental Health Gap Action Programme: Scaling Up Care for Mental, Neurological, and Substance Use Disorders. 2008. Available online: https://apps.who.int/iris/handle/10665/43809 (accessed on 23 March 2022).
- Eisch, A.J.; Cameron, H.A.; Encinas, J.M.; Meltzer, L.A.; Guo, L.M.; Overstreet-Wadiche, L.S. Adult neurogenesis, mental health, and mental illness: Hope or hype? J. Neurosci. 2008, 28, 11785–11791. [Google Scholar] [CrossRef] [PubMed]
- Lakhan, S.E.; Vieira, K.F. Nutritional therapies for mental disorders. Nutr. J. 2008, 7, 2. [Google Scholar] [CrossRef] [PubMed]
- Anglin, R.E.; Samaan, Z.; Walter, S.D.; McDonald, S.D. Vitamin D deficiency and depression in adults: Systematic review and meta-analysis. Br. J. Psychiatry 2013, 202, 100–107. [Google Scholar] [CrossRef] [PubMed]
- Eyles, D.W.; Smith, S.; Kinobe, R.; Hewison, M.; McGrath, J.J. Distribution of the vitamin D receptor and 1α-hydroxylase in the human brain. J. Chem. Neuroanat. 2005, 29, 21–30. [Google Scholar] [CrossRef] [PubMed]
- Hoogendijk, W.J.; Lips, P.; Dik, M.G.; Deeg, D.J.H.; Beekman, A.T.F.; Penninx, B.W.J.H. Depression is associated with decreased 25-hydroxyvitamin D and increased parathyroid hormone levels in older adults. Arch. Gen. Psychiatry 2008, 65, 508–512. [Google Scholar] [CrossRef] [PubMed]
- Milaneschi, Y.; Shardell, M.; Corsi, A.M.; Vazzana, R.; Bandinelli, S.; Guralnik, J.M.; Ferrucci, L. Serum 25-hydroxyvitamin D and depressive symptoms in older women and men. J. Clin. Endocrinol. Metab. 2010, 95, 3225–3233. [Google Scholar] [CrossRef]
- Almeida, O.P.; Hankey, G.J.; Yeap, B.B.; Golledge, J.; Flicker, L. Vitamin D concentration and its association with past, current and future depression in older men: The Health In Men Study. Maturitas 2015, 81, 36–41. [Google Scholar] [CrossRef]
- Rhee, S.J.; Lee, H.; Ahn, Y.M. Serum Vitamin D Concentrations Are Associated With Depressive Symptoms in Men: The Sixth Korea National Health and Nutrition Examination Survey 2014. Front. Psychiatry 2020, 11, 565586. [Google Scholar] [CrossRef]
- Pan, A.; Lu, L.; Franco, O.H.; Yu, Z.; Li, H.; Lin, X. Association between depressive symptoms and 25-hydroxyvitamin D in middle-aged and elderly Chinese. J. Affect. Disord. 2009, 118, 240–243. [Google Scholar] [CrossRef]
- Trinko, J.R.; Land, B.B.; Solecki, W.B.; Wickham, R.J.; Tellez, L.A.; Maldonado-Aviles, J.; de Araujo, I.E.; Addy, N.A.; DiLeone, R.J. Vitamin D3: A role in dopamine circuit regulation, diet-induced obesity, and drug consumption. Eneuro 2016, 3, e0122-15.2016. [Google Scholar] [CrossRef]
- Han, H.; Cui, M.; You, X.; Chen, M.; Piao, X.; Jin, G. A role of 1, 25(OH)2D3 supplementation in rats with nonalcoholic steatohepatitis induced by choline-deficient diet. Nutr. Metab. Cardiovasc. Dis. 2015, 25, 556–561. [Google Scholar] [CrossRef]
- First, M.; Gil-Ad, I.; Taler, M.; Tarasenko, I.; Novak, N.; Weizman, A. The effects of fluoxetine treatment in a chronic mild stress rat model on depression-related behavior, brain neurotrophins, and ERK expression. J. Mol. Neurosci. 2011, 45, 246–255. [Google Scholar] [CrossRef]
- Ducottet, C.; Griebel, G.; Belzung, C. Effects of the selective nonpeptide corticotropin-releasing factor receptor 1 antagonist antalarmin in the chronic mild stress model of depression in mice. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2003, 27, 625–631. [Google Scholar] [CrossRef] [PubMed]
- Burstein, O.; Franko, M.; Gale, E.; Handelsman, A.; Barak, S.; Motsan, S.; Shamir, A.; Toledano, R.; Simhon, O.; Hirshler, Y.; et al. Escitalopram and NHT normalized stress-induced anhedonia and molecular neuroadaptations in a mouse model of depression. PLoS ONE 2017, 12, e0188043. [Google Scholar] [CrossRef]
- Sedaghat, K.; Naderian, R.; Pakdel, R.; Bandegi, A.-R.; Ghods, Z. Regulatory effect of vitamin D on pro-inflammatory cytokines and anti-oxidative enzymes dysregulations due to chronic mild stress in the rat hippocampus and prefrontal cortical area. Mol. Biol. Rep. 2021, 48, 7865–7873. [Google Scholar] [CrossRef]
- Bakhtiari-Dovvombaygi, H.; Izadi, S.; Moghaddam, M.Z.; Hashemzehi, M.; Hosseini, M.; Azhdari-Zarmehri, H.; Dinpanah, H.; Beheshti, F. Beneficial effects of vitamin D on anxiety and depression-like behaviors induced by unpredictable chronic mild stress by suppression of brain oxidative stress and neuroinflammation in rats. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2021, 394, 655–667. [Google Scholar] [CrossRef]
- Liu, M.-Y.; Yin, C.-Y.; Zhu, L.-J.; Zhu, X.-H.; Xu, C.; Luo, C.-X.; Chen, H.; Zhu, D.-Y.; Zhou, Q.-G. Sucrose preference test for measurement of stress-induced anhedonia in mice. Nat. Protoc. 2018, 13, 1686–1698. [Google Scholar] [CrossRef]
- Estrada-Camarena, E.; Fernández-Guasti, A.; López-Rubalcava, C. Interaction between estrogens and antidepressants in the forced swimming test in rats. Psychopharmacology 2004, 173, 139–145. [Google Scholar] [CrossRef]
- Duan, C.-M.; Zhang, J.-R.; Wan, T.-F.; Wang, Y.; Chen, H.-S.; Liu, L. SRT2104 attenuates chronic unpredictable mild stress-induced depressive-like behaviors and imbalance between microglial M1 and M2 phenotypes in the mice. Behav. Brain Res. 2020, 378, 112296. [Google Scholar] [CrossRef]
- Fedotova, J.; Pivina, S.; Sushko, A. Effects of chronic vitamin D3 hormone administration on anxiety-like behavior in adult female rats after long-term ovariectomy. Nutrients 2017, 9, 28. [Google Scholar] [CrossRef]
- Fedotova, J. Different Effects of Fluoxetine and Paroxetine Combined with Vitamin D in Ovariectomized Rats Exposed to Unpredictable Stress. Open Biol. J. 2020, 8, 29–46. [Google Scholar] [CrossRef]
- Koshkina, A.; Dudnichenko, T.; Baranenko, D.; Fedotova, J.; Drago, F. Effects of vitamin D3 in long-term ovariectomized rats subjected to chronic unpredictable mild stress: BDNF, NT-3, and NT-4 implications. Nutrients 2019, 11, 1726. [Google Scholar] [CrossRef] [PubMed]
- Pan, Y.; Zhang, W.-Y.; Xia, X.; Kong, L.-D. Effects of icariin on hypothalamic-pituitary-adrenal axis action and cytokine levels in stressed Sprague-Dawley rats. Biol. Pharm. Bull. 2006, 29, 2399–2403. [Google Scholar] [CrossRef] [PubMed]
- Johnson, S.A.; Fournier, N.M.; Kalynchuk, L.E. Effect of different doses of corticosterone on depression-like behavior and HPA axis responses to a novel stressor. Behav. Brain Res. 2006, 168, 280–288. [Google Scholar] [CrossRef] [PubMed]
- Watson, S.; Mackin, P. HPA axis function in mood disorders. Psychiatry 2006, 5, 166–170. [Google Scholar] [CrossRef]
- Wang, H.; He, Y.; Sun, Z.; Ren, S.; Liu, M.; Wang, G.; Yang, J. Microglia in depression: An overview of microglia in the pathogenesis and treatment of depression. J. Neuroinflamm. 2022, 19, 132. [Google Scholar] [CrossRef]
- Boontanrart, M.; Hall, S.D.; Spanier, J.A.; Hayes, C.E.; Olson, J.K. Vitamin D3 alters microglia immune activation by an IL-10 dependent SOCS3 mechanism. J. Neuroimmunol. 2016, 292, 126–136. [Google Scholar] [CrossRef]
- Dell’Isola, G.B.; Tulli, E.; Sica, R.; Vinti, V.; Mencaroni, E.; Di Cara, G.; Striano, P.; Verrotti, A. The Vitamin D Role in Preventing Primary Headache in Adult and Pediatric Population. J. Clin. Med. 2021, 20, 5983. [Google Scholar] [CrossRef]
- Eyles, D.W.; Burne, T.H.; McGrath, J.J. Vitamin D, effects on brain development, adult brain function and the links between low levels of vitamin D and neuropsychiatric disease. Front. Neuroendocrinol. 2013, 34, 47–64. [Google Scholar] [CrossRef]
- Berk, M.; Sanders, K.M.; Pasco, J.A.; Jacka, F.N.; Williams, L.J.; Hayles, A.L.; Dodd, S. Vitamin D deficiency may play a role in depression. Med. Hypotheses 2007, 69, 1316–1319. [Google Scholar] [CrossRef]
- Schneider, B.; Weber, B.; Frensch, A.; Stein, J.; Fritze, J. Vitamin D in schizophrenia, major depression and alcoholism. J. Neural Transm. 2000, 107, 839–842. [Google Scholar] [CrossRef]
- Oude Voshaar, R.; Derks, W.J.; Comijs, H.C.; Schoevers, R.A.; de Borst, M.H.; Marijnissen, R.M. Antidepressants differentially related to 1, 25-(OH)2 vitamin D3 and 25-(OH) vitamin D3 in late-life depression. Transl. Psychiatry 2014, 4, e383. [Google Scholar] [CrossRef]
- Mulugeta, A.; Lumsden, A.; Hyppönen, E. Relationship between serum 25 (OH) D and depression: Causal evidence from a bi-directional Mendelian randomization study. Nutrients 2020, 13, 109. [Google Scholar] [CrossRef]
- Milaneschi, Y.; Peyrot, W.J.; Nivard, M.G.; Mbarek, H.; Boomsma, D.I.; Penninx, B.W. A role for vitamin D and omega-3 fatty acids in major depression? An exploration using genomics. Transl. Psychiatry 2019, 9, 219. [Google Scholar] [CrossRef]




| Day | Week 1 | Week 2 | Week 3 |
|---|---|---|---|
| One | Cage titling, 24 h | Swimming, 5 min | Cage titling, 24 h |
| Two | Tail pinching, 2 min | Restraint, 1 h | Tail pinching, 2 min |
| Three | Restraint, 1 h | Hot air, 10 min | Restraint, 1 h |
| Four | Hot air, 10 min | Tail pinching, 2 min | Hot air, 10 min |
| Five | Continuous light, 24 h | Continuous light, 24 h | Continuous light, 24 h |
| Six | Continuous light, 24 h | Continuous light, 24 h | Continuous light, 24 h |
| Seven | Water deprivation, 24 h | Food deprivation, 24 h | Food deprivation, 24 h |
| Variables | Control Group n = 8 | CUMS Group n = 8 | VD3 + CUMS Group n = 8 | Fluoxetine + CUMS Group n = 8 | VD3 + Fluoxetine + CUMS Group n = 8 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| r | p | r | p | r | p | r | p | r | p | |
| EPM (s) | 0.605 | 0.112 | −0.311 | 0.453 | 0.011 | 0.979 | −0.162 | 0.702 | 0.008 | 0.985 |
| FST (s) | −0.039 | 0.927 | 0.136 | 0.748 | 0.079 | 0.852 | −0.24 | 0.567 | 0.165 | 0.696 |
| OFT (s) | 0.524 | 0.182 | −0.072 | 0.865 | −0.252 | 0.547 | −0.32 | 0.44 | 0.424 | 0.295 |
| SPT (mL) | 0.245 | 0.559 | −0.566 | 0.144 | 0.047 | 0.912 | −0.335 | 0.417 | −0.707 | 0.049 |
| TST (s) | −0.641 | 0.087 | −0.467 | 0.243 | −0.395 | 0.333 | 0.59 | 0.124 | −0.387 | 0.344 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Ramadhan, F.R.; Abulmeaty, M.M.A.; Alquraishi, M.; Razak, S.; Alhussain, M.H. Effect of Vitamin D3 on Depressive Behaviors of Rats Exposed to Chronic Unpredictable Mild Stress. Biomedicines 2023, 11, 2112. https://doi.org/10.3390/biomedicines11082112
Al-Ramadhan FR, Abulmeaty MMA, Alquraishi M, Razak S, Alhussain MH. Effect of Vitamin D3 on Depressive Behaviors of Rats Exposed to Chronic Unpredictable Mild Stress. Biomedicines. 2023; 11(8):2112. https://doi.org/10.3390/biomedicines11082112
Chicago/Turabian StyleAl-Ramadhan, Fatimah R., Mahmoud M. A. Abulmeaty, Mohammed Alquraishi, Suhail Razak, and Maha H. Alhussain. 2023. "Effect of Vitamin D3 on Depressive Behaviors of Rats Exposed to Chronic Unpredictable Mild Stress" Biomedicines 11, no. 8: 2112. https://doi.org/10.3390/biomedicines11082112
APA StyleAl-Ramadhan, F. R., Abulmeaty, M. M. A., Alquraishi, M., Razak, S., & Alhussain, M. H. (2023). Effect of Vitamin D3 on Depressive Behaviors of Rats Exposed to Chronic Unpredictable Mild Stress. Biomedicines, 11(8), 2112. https://doi.org/10.3390/biomedicines11082112







