δ-Opioid Receptor as a Molecular Target for Increasing Cardiac Resistance to Reperfusion in Drug Development
Abstract
1. Introduction
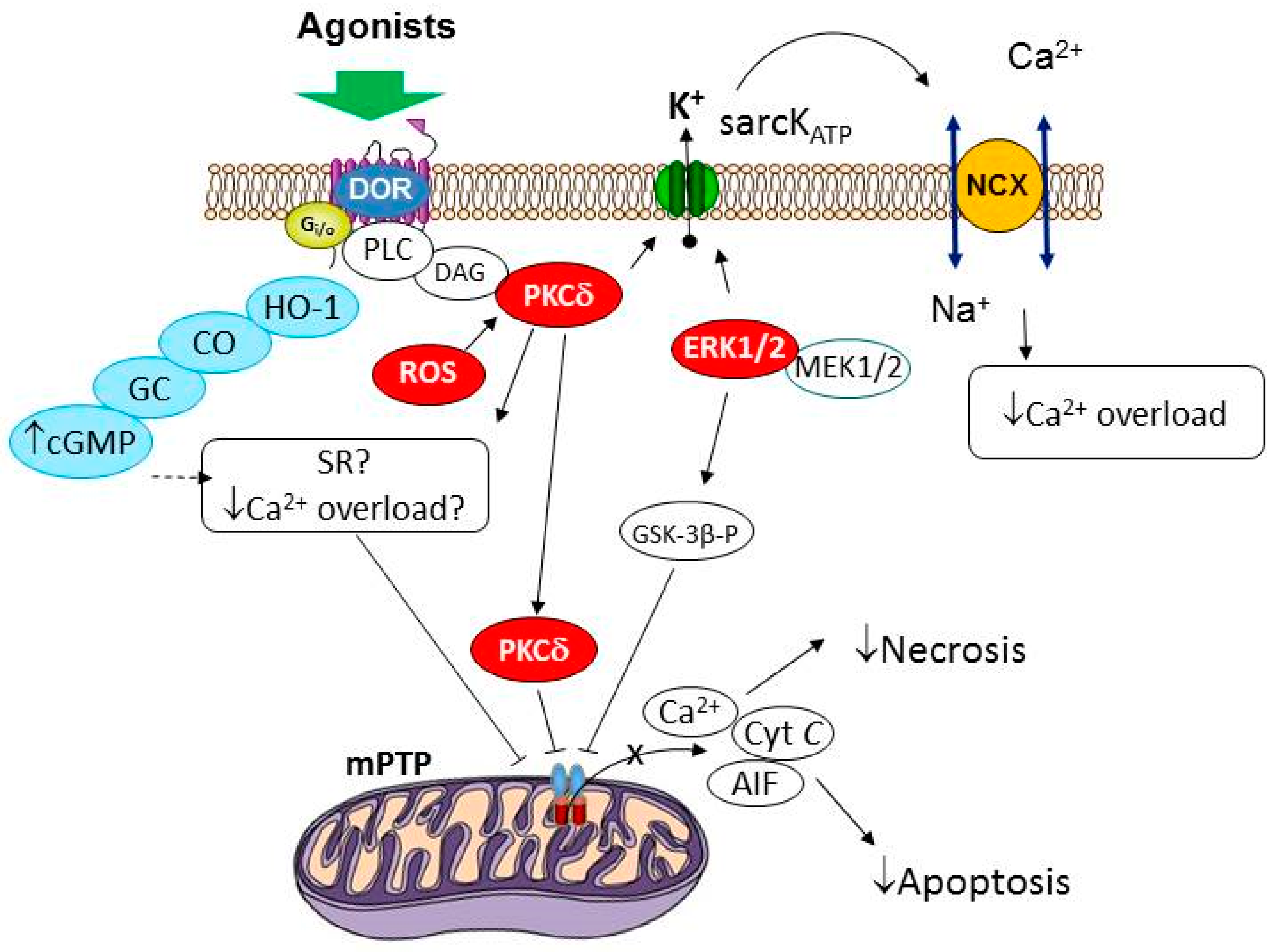
2. The Role of δ-Opioid Receptors and the Transactivation of EGFR in the Regulation of Cardiac Tolerance to Reperfusion
3. The Signal Mechanism of the Cardioprotective Effect of the Activation of δ-Opioid Receptors
3.1. The Role of Protein Kinases and NO Synthase in the Infarct-Limiting Effect of Opioids
3.2. The Role of Guanylyl Cyclase in the Cardioprotective Effect of OR Stimulation
3.3. The Role of Reactive Oxygen Species in the Cardioprotective Effect of Opioids
3.4. Hypothetical End-Effectors of the Cardioprotective Action of Opioids and Their Effect on Cell Death Pathways
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| 2-MPG | 2-mercaptopropionyl glycine |
| AMPK | AMP-activated protein kinase |
| KATP-channel | ATP-sensitive K+ channel |
| ANP | atrial natriuretic peptide |
| BKCa-channel | big conductance Ca2+-activated K+ channel |
| BBB | blood–brain barrier |
| ERK1/2 | extracellular signal-regulated kinase 1/2 |
| Jak-2 | Janus kinase 2 |
| mitoKATP channel | mitochondrial KATP channel |
| MPT pore | mitochondrial permeability transition pore |
| MEK1/2 | mitogen-activated protein kinase kinase 1/2 |
| NOS | NO synthase |
| OR | opioid receptor |
| PCI | percutaneous coronary intervention |
| PI3K | phosphatidylinositol-3-kinase |
| PKA | protein kinase A |
| PKC | protein kinase C |
| sarcKATP channel | sarcolemmal KATP channel |
| GC | soluble guanylyl cyclase |
| STEMI | ST-segment elevation myocardial infarction |
| δ2-OR | δ2-opioid receptor |
References
- Megaly, M.; Pershad, A.; Glogoza, M.; Elbadawi, A.; Omer, M.; Saad, M.; Mentias, A.; Elgendy, I.; Burke, M.N.; Capodanno, D.; et al. Use of Intravascular Imaging in Patients With ST-Segment Elevation Acute Myocardial Infarction. Cardiovasc. Revasc. Med. 2021, 30, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Garcia, S.; Schmidt, C.W.; Garberich, R.; Henry, T.D.; Bradley, S.M.; Brilakis, E.S.; Burke, N.; Chavez, I.J.; Eckman, P.; Gössl, M.; et al. Temporal Changes in Patient Characteristics and Outcomes in ST Segment Elevation Myocardial Infarction 2003–2018. Catheter. Cardiovasc. Interv. 2021, 97, 1109–1117. [Google Scholar] [CrossRef] [PubMed]
- Ya’qoub, L.; Gad, M.; Saad, A.M.; Elgendy, I.Y.; Mahmoud, A.N. National Trends of Utilization and Readmission Rates with Intravascular Ultrasound Use for ST-Elevation Myocardial Infarction. Catheter. Cardiovasc. Interv. 2021, 98, 1–9. [Google Scholar] [CrossRef]
- Maslov, L.N.; Popov, S.V.; Mukhomedzyanov, A.V.; Naryzhnaya, N.V.; Voronkov, N.S.; Ryabov, V.V.; Boshchenko, A.A.; Khaliulin, I.; Prasad, N.R.; Fu, F.; et al. Reperfusion Cardiac Injury: Receptors and the Signaling Mechanisms. Curr. Cardiol. Rev. 2022, 18, 63–79. [Google Scholar] [CrossRef] [PubMed]
- Acharya, D. Predictors of Outcomes in Myocardial Infarction and Cardiogenic Shock. Cardiol. Rev. 2018, 26, 255–266. [Google Scholar] [CrossRef]
- Sambola, A.; Elola, F.J.; Buera, I.; Fernández, C.; Bernal, J.L.; Ariza, A.; Brindis, R.; Bueno, H.; Rodríguez-Padial, L.; Marín, F.; et al. Sex Bias in Admission to Tertiary-Care Centres for Acute Myocardial Infarction and Cardiogenic Shock. Eur. J. Clin. Investig. 2021, 51, e13526. [Google Scholar] [CrossRef]
- Maslov, L.N.; Lishmanov, Y.B.; Oeltgen, P.R.; Barzakh, E.I.; Krylatov, A.V.; Govindaswami, M.; Brown, S.A. Activation of Peripheral Δ2 Opioid Receptors Increases Cardiac Tolerance to Ischemia/Reperfusion Injury. Involvement of Protein Kinase C, NO-Synthase, KATP Channels and the Autonomic Nervous System. Life Sci. 2009, 84, 657–663. [Google Scholar] [CrossRef]
- Benedict, P.E.; Benedict, M.B.; Su, T.-P.; Bolling, S.F. Opiate Drugs and -Receptor-Mediated Myocardial Protection. Circulation 1999, 100, II-357–II-360. [Google Scholar] [CrossRef]
- Takasaki, Y.; Wolff, R.A.; Chien, G.L.; van Winkle, D.M. Met 5 -Enkephalin Protects Isolated Adult Rabbit Cardiomyocytes via δ-Opioid Receptors. Am. J. Physiol.-Heart Circ. Physiol. 1999, 277, H2442–H2450. [Google Scholar] [CrossRef]
- Gross, E.R.; Hsu, A.K.; Gross, G.J. Opioid-Induced Cardioprotection Occurs via Glycogen Synthase Kinase β Inhibition During Reperfusion in Intact Rat Hearts. Circ. Res. 2004, 94, 960–966. [Google Scholar] [CrossRef]
- Gross, E.R.; Hsu, A.K.; Gross, G.J. Acute Methadone Treatment Reduces Myocardial Infarct Size via the δ-Opioid Receptor in Rats During Reperfusion. Anesth. Analg. 2009, 109, 1395–1402. [Google Scholar] [CrossRef] [PubMed]
- Parodi, G. Editor’s Choice-Chest Pain Relief in Patients with Acute Myocardial Infarction. Eur. Heart J. Acute Cardiovasc. Care 2016, 5, 277–281. [Google Scholar] [CrossRef] [PubMed]
- Maslov, L.N.; Lishmaniv, Y.B. The Blood–Brain Barrier Permeability for Opioid Peptides. Exp. Clin. Pharmacol. 2017, 80, 39–44. [Google Scholar] [CrossRef]
- Jiang, L.; Hu, J.; He, S.; Zhang, L.; Zhang, Y. Spinal Neuronal NOS Signaling Contributes to Morphine Cardioprotection in Ischemia Reperfusion Injury in Rats. J. Pharmacol. Exp. Ther. 2016, 358, 450–456. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Hu, J.; Zhang, Y.; Dong, C.S.; Wong, G.T.C. Remote Intrathecal Morphine Preconditioning Confers Cardioprotection via Spinal Cord Nitric Oxide/Cyclic Guanosine Monophosphate/Protein Kinase G Pathway. J. Surg. Res. 2015, 193, 43–51. [Google Scholar] [CrossRef]
- Lishmanov, Y.B.; Ugdyzhekova, D.S.; Maslov, L.N. Prevention of Experimental Epinephrine-Induced Arrhythmias with Agonists of Δ1- and Δ2-Opiate Receptors. Bull. Exp. Biol. Med. 1997, 124, 873–875. [Google Scholar] [CrossRef]
- Patel, H.H.; Hsu, A.; Moore, J.; Gross, G.J. BW373U86, a δ Opioid Agonist, Partially Mediates Delayed Cardioprotection via a Free Radical Mechanism That Is Independent of Opioid Receptor Stimulation. J. Mol. Cell. Cardiol. 2001, 33, 1455–1465. [Google Scholar] [CrossRef]
- Maslov, L.N.; Khaliulin, I.; Oeltgen, P.R.; Naryzhnaya, N.V.; Pei, J.-M.; Brown, S.A.; Lishmanov, Y.B.; Downey, J.M. Prospects for Creation of Cardioprotective and Antiarrhythmic Drugs Based on Opioid Receptor Agonists. Med. Res. Rev. 2016, 36, 871–923. [Google Scholar] [CrossRef]
- Mukhomedzyanov, A.V.; Popov, S.V.; Maslov, L.N.; Diez, E.R.; Azev, V.N. Role of PI3K, ERK1/2, and JAK2 Kinases in the Cardioprotective Effect of Deltorphin II during Cardiac Reperfusion. Bull Exp. Biol. Med. 2023, 175, 17–19. [Google Scholar] [CrossRef]
- Peart, J.N.; Patel, H.H.; Gross, G.J. δ-Opioid Receptor Activation Mimics Ischemic Preconditioning in the Canine Heart. J. Cardiovasc. Pharmacol. 2003, 42, 78–81. [Google Scholar] [CrossRef]
- Fryer, R.M.; Wang, Y.; Hsu, A.K.; Nagase, H.; Gross, G.J. Dependence of Delta1-Opioid Receptor-Induced Cardioprotection on a Tyrosine Kinase-Dependent but Not a Src-Dependent Pathway. J. Pharmacol. Exp. Ther. 2001, 299, 477–482. [Google Scholar] [PubMed]
- Maslov, L.N.; Mukhomedzyanov, A.V.; Tsibulnikov, S.Y.; Suleiman, M.-S.; Khaliulin, I.; Oeltgen, P.R. Activation of Peripheral Δ2-Opioid Receptor Prevents Reperfusion Heart Injury. Eur. J. Pharmacol. 2021, 907, 174302. [Google Scholar] [CrossRef] [PubMed]
- Förster, K.; Kuno, A.; Solenkova, N.; Felix, S.B.; Krieg, T. The δ-Opioid Receptor Agonist DADLE at Reperfusion Protects the Heart through Activation of pro-Survival Kinases via EGF Receptor Transactivation. Am. J. Physiol.-Heart Circ. Physiol. 2007, 293, 1604–1608. [Google Scholar] [CrossRef]
- Naryzhnaya, N.V.; Mukhomedzyanov, A.V.; Kurbatov, B.K.; Sirotina, M.A.; Kilin, M.; Azev, V.N.; Maslov, L.N. The Infarct-Limiting Efficacy of Deltorphin-II in Old Rats with Diet-Induced Metabolic Syndrome. Acta Biomed. Sci. 2022, 7, 281–289. [Google Scholar] [CrossRef]
- Xu, J.; Bian, X.; Zhao, H.; Sun, Y.; Tian, Y.; Li, X.; Tian, W. Morphine Prevents Ischemia/Reperfusion-Induced Myocardial Mitochondrial Damage by Activating δ-Opioid Receptor/EGFR/ROS Pathway. Cardiovasc. Drugs Ther. 2022, 36, 841–857. [Google Scholar] [CrossRef]
- Yao, E.; Luo, L.; Lin, C.; Wen, J.; Li, Y.; Ren, T.; Chen, Y.; Huang, J.; Jin, X. OEA Alleviates Apoptosis in Diabetic Rats with Myocardial Ischemia/Reperfusion Injury by Regulating the PI3K/Akt Signaling Pathway through Activation of TRPV1. Front. Pharmacol. 2022, 13, 964475. [Google Scholar] [CrossRef]
- Haines, D.D.; Juhasz, B.; Tosaki, A. Management of Multicellular Senescence and Oxidative Stress. J. Cell. Mol. Med. 2013, 17, 936–957. [Google Scholar] [CrossRef]
- Heusch, G. Molecular Basis of Cardioprotection. Circ. Res. 2015, 116, 674–699. [Google Scholar] [CrossRef]
- de Miranda, D.C.; de Oliveira Faria, G.; Hermidorff, M.M.; dos Santos Silva, F.C.; de Assis, L.V.M.; Isoldi, M.C. Pre- and Post-Conditioning of the Heart: An Overview of Cardioprotective Signaling Pathways. Curr. Vasc. Pharmacol. 2021, 19, 499–524. [Google Scholar] [CrossRef]
- Ishikawa, S.; Kuno, A.; Tanno, M.; Miki, T.; Kouzu, H.; Itoh, T.; Sato, T.; Sunaga, D.; Murase, H.; Miura, T. Role of Connexin-43 in Protective PI3K-AKT-GSK-3β Signaling in Cardiomyocytes. Am. J. Physiol.-Heart Circ. Physiol. 2012, 302, 2536–2544. [Google Scholar] [CrossRef]
- Gross, E.R.; Hsu, A.K.; Gross, G.J. The JAK/STAT Pathway Is Essential for Opioid-Induced Cardioprotection: JAK2 as a Mediator of STAT3, Akt, and GSK-3β. Am. J. Physiol.-Heart Circ. Physiol. 2006, 291, H827–H834. [Google Scholar] [CrossRef] [PubMed]
- Dorsch, M.; Behmenburg, F.; Raible, M.; Blase, D.; Grievink, H.; Hollmann, M.W.; Heinen, A.; Huhn, R. Morphine-Induced Preconditioning: Involvement of Protein Kinase A and Mitochondrial Permeability Transition Pore. PLoS ONE 2016, 11, e0151025. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Zhang, H.; Li, T.; Zhang, B. Involvement of Adenosine Monophosphate-Activated Protein Kinase in Morphine-Induced Cardioprotection. J. Surg. Res. 2011, 169, 179–187. [Google Scholar] [CrossRef]
- Kim, J.H.; Jang, Y.H.; Chun, K.J.; Kim, J.; Park, Y.H.; Kim, J.S.; Kim, J.M.; Lee, M.Y. Kappa-Opioid Receptor Activation during Reperfusion Limits Myocardial Infarction via ERK1/2 Activation in Isolated Rat Hearts. Korean J. Anesthesiol. 2011, 60, 351. [Google Scholar] [CrossRef]
- Wu, X.; Zhang, B.; Fan, R.; Zhao, L.; Wang, Y.; Zhang, S.; Kaye, A.D.; Huang, L.; Pei, J. U50,488H Inhibits Neutrophil Accumulation and TNF-α Induction Induced by Ischemia–Reperfusion in Rat Heart. Cytokine 2011, 56, 503–507. [Google Scholar] [CrossRef] [PubMed]
- Gross, G.J.; Hsu, A.; Nithipatikom, K.; Pfeiffer, A.W.; Bobrova, I.; Bissessar, E. Acute and Chronic Cardioprotection by the Enkephalin Analogue, Eribis Peptide 94, Is Mediated via Activation of Nitric Oxide Synthase and Adenosine Triphosphate-Regulated Potassium Channels. Pharmacology 2012, 90, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Chen, Z.; Irwin, M.G.; Wong, T. Remifentanil Mimics Cardioprotective Effect of Ischemic Preconditioning via Protein Kinase C Activation in Open Chest of Rats. Acta Pharmacol. Sin. 2005, 26, 546–550. [Google Scholar] [CrossRef]
- Popov, S.V.; Mukhomedzyanov, A.V.; Maslov, L.N.; Naryzhnaya, N.V.; Kurbatov, B.K.; Prasad, N.R.; Singh, N.; Fu, F.; Azev, V.N. The Infarct-Reducing Effect of the Δ2 Opioid Receptor Agonist Deltorphin II: The Molecular Mechanism. Membranes 2023, 13, 63. [Google Scholar] [CrossRef]
- Maslov, L.N.; Lishmanov, Y.B. The Anti-Arrhythmic Effect of d-Ala 2, Leu 5, Arg 6-Enkephalin and Its Possible Mechanism. Int. J. Cardiol. 1993, 40, 89–94. [Google Scholar] [CrossRef]
- Li, D.-Y.; Gao, S.-J.; Sun, J.; Zhang, L.-Q.; Wu, J.-Y.; Song, F.-H.; Liu, D.-Q.; Zhou, Y.-Q.; Mei, W. Targeting the Nitric Oxide/CGMP Signaling Pathway to Treat Chronic Pain. Neural Regen. Res. 2023, 18, 996. [Google Scholar] [CrossRef]
- Krylatov, A.V.; Tsibulnikov, S.Y.; Mukhomedzyanov, A.V.; Boshchenko, A.A.; Goldberg, V.E.; Jaggi, A.S.; Erben, R.G.; Maslov, L.N. The Role of Natriuretic Peptides in the Regulation of Cardiac Tolerance to Ischemia/Reperfusion and Postinfarction Heart Remodeling. J. Cardiovasc. Pharmacol. Ther. 2021, 26, 131–148. [Google Scholar] [CrossRef]
- Juhasz, B.; Varga, B.; Czompa, A.; Bak, I.; Lekli, I.; Gesztelyi, R.; Zsuga, J.; Kemeny-Beke, A.; Antal, M.; Szendrei, L.; et al. Postischemic Cardiac Recovery in Heme Oxygenase-1 Transgenic Ischemic/Reperfused Mouse Myocardium. J. Cell. Mol. Med. 2011, 15, 1973–1982. [Google Scholar] [CrossRef]
- Castany, S.; Carcolé, M.; Leánez, S.; Pol, O. The Antinociceptive Effects of a δ-Opioid Receptor Agonist in Mice with Painful Diabetic Neuropathy: Involvement of Heme Oxygenase 1. Neurosci. Lett. 2016, 614, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Stagni, E.; Bucolo, C.; Motterlini, R.; Drago, F. Morphine-Induced Ocular Hypotension Is Modulated by Nitric Oxide and Carbon Monoxide: Role of μ 3 Receptors. J. Ocul. Pharmacol. Ther. 2010, 26, 31–36. [Google Scholar] [CrossRef]
- Qin, X.; Liu, B.; Gao, F.; Hu, Y.; Chen, Z.; Xu, J.; Zhang, X. Gluconolactone Alleviates Myocardial Ischemia/Reperfusion Injury and Arrhythmias via Activating PKCε/Extracellular Signal-Regulated Kinase Signaling. Front. Physiol. 2022, 13, 455. [Google Scholar] [CrossRef] [PubMed]
- Tosaki, A. ArrhythmoGenoPharmacoTherapy. Front. Pharmacol. 2020, 11, 616. [Google Scholar] [CrossRef]
- Tosaki, A.; Blasig, I.E.; Pali, T.; Ebert, B. Heart Protection and Radical Trapping by DMPO during Reperfusion in Isolated Working Rat Hearts. Free. Radic. Biol. Med. 1990, 8, 363–372. [Google Scholar] [CrossRef] [PubMed]
- Jaggi, A.S.; Popov, S.V.; Krylatov, A.V.; Maslov, L.N.; Voronkov, N.S.; Boshchenko, A.A.; Gomez, L.; Downey, J.M.; Wang, H.; Popov, S.V.; et al. Reactive Oxygen Species as Intracellular Signaling Molecules in the Cardiovascular System. Curr. Cardiol. Rev. 2018, 14, 290–300. [Google Scholar] [CrossRef]
- Penna, C.; Alloatti, G.; Crisafulli, A. Mechanisms Involved in Cardioprotection Induced by Physical Exercise. Antioxid. Redox Signal. 2020, 32, 1115–1134. [Google Scholar] [CrossRef]
- Penna, C.; Mancardi, D.; Rastaldo, R.; Pagliaro, P. Cardioprotection: A Radical View. Free Radicals in Pre and Postconditioning. Biochim. Et Biophys. Acta-Bioenerg. 2009, 1787, 781–793. [Google Scholar] [CrossRef]
- Yao, L.-L.; Wang, Y.-G.; Cai, W.-J.; Yao, T.; Zhu, Y.-C. Survivin Mediates the Anti-Apoptotic Effect of δ-Opioid Receptor Stimulation in Cardiomyocytes. J. Cell Sci. 2007, 120, 895–907. [Google Scholar] [CrossRef] [PubMed]
- Rebrova, T.Y.; Maslov, L.N.; Lishmanov, A.Y.; Tam, S.V. Stimulation of μ- and Delta-Opiate Receptors and Tolerance of Isolated Heart to Oxidative Stress: The Role of NO-Synthase. Biochemistry 2001, 66, 520–528. [Google Scholar] [CrossRef]
- Cohen, M.V.; Philipp, S.; Krieg, T.; Cui, L.; Kuno, A.; Solodushko, V.; Downey, J.M. Preconditioning-Mimetics Bradykinin and DADLE Activate PI3-Kinase through Divergent Pathways. J. Mol. Cell. Cardiol. 2007, 42, 842–851. [Google Scholar] [CrossRef]
- Xu, J.; Tian, W.; Ma, X.; Guo, J.; Shi, Q.; Jin, Y.; Xi, J.; Xu, Z. The Molecular Mechanism Underlying Morphine-Induced Akt Activation: Roles of Protein Phosphatases and Reactive Oxygen Species. Cell Biochem. Biophys. 2011, 61, 303–311. [Google Scholar] [CrossRef] [PubMed]
- Tsutsumi, Y.M.; Yokoyama, T.; Horikawa, Y.; Roth, D.M.; Patel, H.H. Reactive Oxygen Species Trigger Ischemic and Pharmacological Postconditioning: In Vivo and in Vitro Characterization. Life Sci. 2007, 81, 1223–1227. [Google Scholar] [CrossRef] [PubMed]
- Patel, H.H.; Hsu, A.; Gross, G.J. Delayed Cardioprotection Is Mediated via a Non-Peptide δ Opioid Agonist, SNC-121, Independent of Opioid Receptor Stimulation. Basic Res. Cardiol. 2004, 99, 38–45. [Google Scholar] [CrossRef]
- Estrada, J.A.; Williams, A.G.; Sun, J.; Gonzalez, L.; Downey, H.F.; Caffrey, J.L.; Mallet, R.T. δ-Opioid Receptor (DOR) Signaling and Reactive Oxygen Species (ROS) Mediate Intermittent Hypoxia Induced Protection of Canine Myocardium. Basic Res. Cardiol. 2016, 111, 1–12. [Google Scholar] [CrossRef]
- Komarov, D.A.; Samouilov, A.; Hirata, H.; Zweier, J.L. High Fidelity Triangular Sweep of the Magnetic Field for Millisecond Scan EPR Imaging. J. Magn. Reson. 2021, 329, 107024. [Google Scholar] [CrossRef]
- Rong, F.; Peng, Z.; Ming-Xiang, Y.; Zhang, Q.-Y.; Zhao, Y.; Zhang, S.-M.; Guo, H.-T.; Bi, H.; Wang, Y.-M.; Liang, C.; et al. Myocardial Apoptosis and Infarction after Ischemia/Reperfusion Are Attenuated by κ-Opioid Receptor Agonist. Arch. Med. Res. 2009, 40, 227–234. [Google Scholar] [CrossRef]
- Patel, H.H.; Ludwig, L.M.; Fryer, R.M.; Hsu, A.K.; Warltier, D.C.; Gross, G.J. Delta Opioid Agonists and Volatile Anesthetics Facilitate Cardioprotection via Potentiation of K(ATP) Channel Opening. FASEB J. 2002, 16, 1468–1470. [Google Scholar] [CrossRef]
- Peart, J.N.; Gross, E.R.; Reichelt, M.E.; Hsu, A.; Headrick, J.P.; Gross, G.J. Activation of Kappa-Opioid Receptors at Reperfusion Affords Cardioprotection in Both Rat and Mouse Hearts. Basic Res. Cardiol. 2008, 103, 454–463. [Google Scholar] [CrossRef]
- Fryer, R.M.; Eells, J.T.; Hsu, A.K.; Henry, M.M.; Gross, G.J. Ischemic Preconditioning in Rats: Role of Mitochondrial K ATP Channel in Preservation of Mitochondrial Function. Am. J. Physiol.-Heart Circ. Physiol. 2000, 278, H305–H312. [Google Scholar] [CrossRef] [PubMed]
- Kowaltowski, A.J.; Seetharaman, S.; Paucek, P.; Garlid, K.D. Bioenergetic Consequences of Opening the ATP-Sensitive K + Channel of Heart Mitochondria. Am. J. Physiol.-Heart Circ. Physiol. 2001, 280, H649–H657. [Google Scholar] [CrossRef] [PubMed]
- Eaton, M.; Hernandez, L.A.; Schaefer, S. Ischemic Preconditioning and Diazoxide Limit Mitochondrial Ca Overload during Ischemia/Reperfusion: Role of Reactive Oxygen Species. Exp. Clin. Cardiol. 2005, 10, 96–103. [Google Scholar] [PubMed]
- Iwai, T.; Tanonaka, K.; Koshimizu, M.; Takeo, S. Preservation of Mitochondrial Function by Diazoxide during Sustained Ischaemia in the Rat Heart. Br. J. Pharmacol. 2000, 129, 1219–1227. [Google Scholar] [CrossRef] [PubMed]
- Maslov, L.N.; Popov, S.V.; Naryzhnaya, N.V.; Mukhomedzyanov, A.V.; Kurbatov, B.K.; Derkachev, I.A.; Boshchenko, A.A.; Prasad, N.R.; Ma, H.; Zhang, Y.; et al. KATP Channels Are Regulators of Programmed Cell Death and Targets for Creation of Novel Drugs against Ischemia/Reperfusion Cardiac Injury. Fundam. Clin. Pharmacol. 2023. [Google Scholar] [CrossRef]
- Yaoita, H.; Ogawa, K.; Maehara, K.; Maruyama, Y. Attenuation of Ischemia/Reperfusion Injury in Rats by a Caspase Inhibitor. Circulation 1998, 97, 276–281. [Google Scholar] [CrossRef]
- Lazou, A.; Iliodromitis, E.K.; Cieslak, D.; Voskarides, K.; Mousikos, S.; Bofilis, E.; Kremastinos, D.T. Ischemic but Not Mechanical Preconditioning Attenuates Ischemia/Reperfusion Induced Myocardial Apoptosis in Anaesthetized Rabbits: The Role of Bcl-2 Family Proteins and ERK1/2. Apoptosis 2006, 11, 2195–2204. [Google Scholar] [CrossRef]
- Liu, H.; Zhang, H.Y.; Zhu, X.; Shao, Z.; Yao, Z. Preconditioning Blocks Cardiocyte Apoptosis: Role of K ATP Channels and PKC-ε. Am. J. Physiol.-Heart Circ. Physiol. 2002, 282, H1380–H1386. [Google Scholar] [CrossRef]
- Watanabe, Y. Cardiac Na+/Ca2+ Exchange Stimulators among Cardioprotective Drugs. J. Physiol. Sci. 2019, 69, 837–849. [Google Scholar] [CrossRef]
- Baczkó, I.; Giles, W.R.; Light, P.E. Pharmacological Activation of Plasma-Membrane K ATP Channels Reduces Reoxygenation-Induced Ca2+ Overload in Cardiac Myocytes via Modulation of the Diastolic Membrane Potential. Br. J. Pharmacol. 2004, 141, 1059–1067. [Google Scholar] [CrossRef]
- Tan, X.; Chen, Y.; Zou, S.; Wang, W.; Zhang, N.; Sun, Z.-Y.; Xian, W.; Li, X.; Tang, B.; Wang, H.; et al. ALDH2 Attenuates Ischemia and Reperfusion Injury through Regulation of Mitochondrial Fusion and Fission by PI3K/AKT/MTOR Pathway in Diabetic Cardiomyopathy. Free. Radic. Biol. Med. 2023, 195, 219–230. [Google Scholar] [CrossRef]
- Jang, Y.; Xi, J.; Wang, H.; Mueller, R.A.; Norfleet, E.A.; Xu, Z. Postconditioning Prevents Reperfusion Injury by Activating δ-Opioid Receptors. Anesthesiology 2008, 108, 243–250. [Google Scholar] [CrossRef]
- Kim, J.H.; Chun, K.J.; Park, Y.H.; Kim, J.; Kim, J.S.; Jang, Y.H.; Lee, M.Y.; Park, J.H. Morphine-Induced Postconditioning Modulates Mitochondrial Permeability Transition Pore Opening via Delta-1 Opioid Receptors Activation in Isolated Rat Hearts. Korean J. Anesthesiol. 2011, 61, 69. [Google Scholar] [CrossRef]
- Ruiz-Meana, M.; Garcia-Dorado, D.; Miró-Casas, E.; Abellán, A.; Soler-Soler, J. Mitochondrial Ca2+ Uptake during Simulated Ischemia Does Not Affect Permeability Transition Pore Opening upon Simulated Reperfusion. Cardiovasc. Res. 2006, 71, 715–724. [Google Scholar] [CrossRef]
- Gomez, L.; Thiebaut, P.A.; Paillard, M.; Ducreux, S.; Abrial, M.; Crola Da Silva, C.; Durand, A.; Alam, M.R.; Van Coppenolle, F.; Sheu, S.S.; et al. The SR/ER-Mitochondria Calcium Crosstalk Is Regulated by GSK3β during Reperfusion Injury. Cell Death Differ. 2016, 23, 313–322. [Google Scholar] [CrossRef] [PubMed]
- Kroemer, G.; Galluzzi, L.; Brenner, C. Mitochondrial Membrane Permeabilization in Cell Death. Physiol. Rev. 2007, 87, 99–163. [Google Scholar] [CrossRef] [PubMed]
- Ishikita, A.; Matoba, T.; Ikeda, G.; Koga, J.; Mao, Y.; Nakano, K.; Takeuchi, O.; Sadoshima, J.; Egashira, K. Nanoparticle-Mediated Delivery of Mitochondrial Division Inhibitor 1 to the Myocardium Protects the Heart From Ischemia-Reperfusion Injury Through Inhibition of Mitochondria Outer Membrane Permeabilization: A New Therapeutic Modality for Acute Myocardial. J. Am. Heart Assoc. 2016, 5, e003872. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Wang, H.; Wu, G.; Yang, Y.; Yang, J.; Liu, C.; Wong, T.M. Protein Kinase C Mediates the Effects of Delta-Opioid Receptor Stimulation on Survival and Apoptosis in Neonatal Cardiomyocytes Cultured in Serum-Deprived Condition. Die Pharm. 2009, 64, 466–471. [Google Scholar]
- Liang, Q.; Huang, X.; Zeng, C.; Li, D.; Shi, Y.; Zhao, G.; Zhong, M. BW373U86 Upregulates Autophagy by Inhibiting the PI3k/AKT Pathway and Regulating the MTOR Pathway to Protect Cardiomyocytes from Hypoxia–Reoxygenation Injury. Can. J. Physiol. Pharmacol. 2020, 98, 684–690. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Naryzhnaya, N.V.; Mukhomedzyanov, A.V.; Sirotina, M.; Maslov, L.N.; Kurbatov, B.K.; Gorbunov, A.S.; Kilin, M.; Kan, A.; Krylatov, A.V.; Podoksenov, Y.K.; et al. δ-Opioid Receptor as a Molecular Target for Increasing Cardiac Resistance to Reperfusion in Drug Development. Biomedicines 2023, 11, 1887. https://doi.org/10.3390/biomedicines11071887
Naryzhnaya NV, Mukhomedzyanov AV, Sirotina M, Maslov LN, Kurbatov BK, Gorbunov AS, Kilin M, Kan A, Krylatov AV, Podoksenov YK, et al. δ-Opioid Receptor as a Molecular Target for Increasing Cardiac Resistance to Reperfusion in Drug Development. Biomedicines. 2023; 11(7):1887. https://doi.org/10.3390/biomedicines11071887
Chicago/Turabian StyleNaryzhnaya, Natalia V., Alexander V. Mukhomedzyanov, Maria Sirotina, Leonid N. Maslov, Boris K. Kurbatov, Alexander S. Gorbunov, Mikhail Kilin, Artur Kan, Andrey V. Krylatov, Yuri K. Podoksenov, and et al. 2023. "δ-Opioid Receptor as a Molecular Target for Increasing Cardiac Resistance to Reperfusion in Drug Development" Biomedicines 11, no. 7: 1887. https://doi.org/10.3390/biomedicines11071887
APA StyleNaryzhnaya, N. V., Mukhomedzyanov, A. V., Sirotina, M., Maslov, L. N., Kurbatov, B. K., Gorbunov, A. S., Kilin, M., Kan, A., Krylatov, A. V., Podoksenov, Y. K., & Logvinov, S. V. (2023). δ-Opioid Receptor as a Molecular Target for Increasing Cardiac Resistance to Reperfusion in Drug Development. Biomedicines, 11(7), 1887. https://doi.org/10.3390/biomedicines11071887






