Plasma Osteopontin Reflects Tissue Damage in Acute Pancreatitis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Subjects
2.2. Laboratory Analyses
2.3. Statistics
3. Results
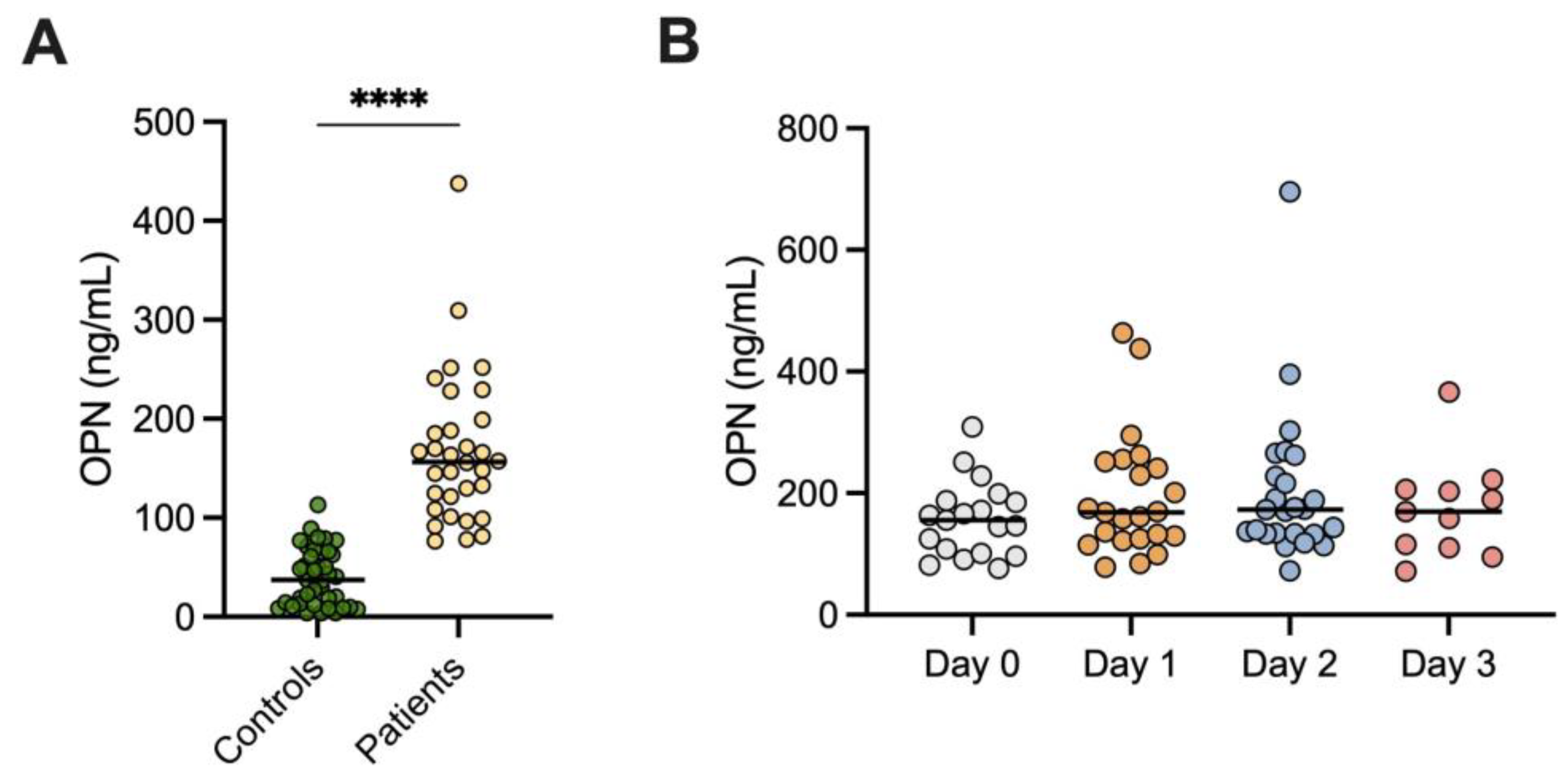
3.1. OPN Levels in AP and Controls
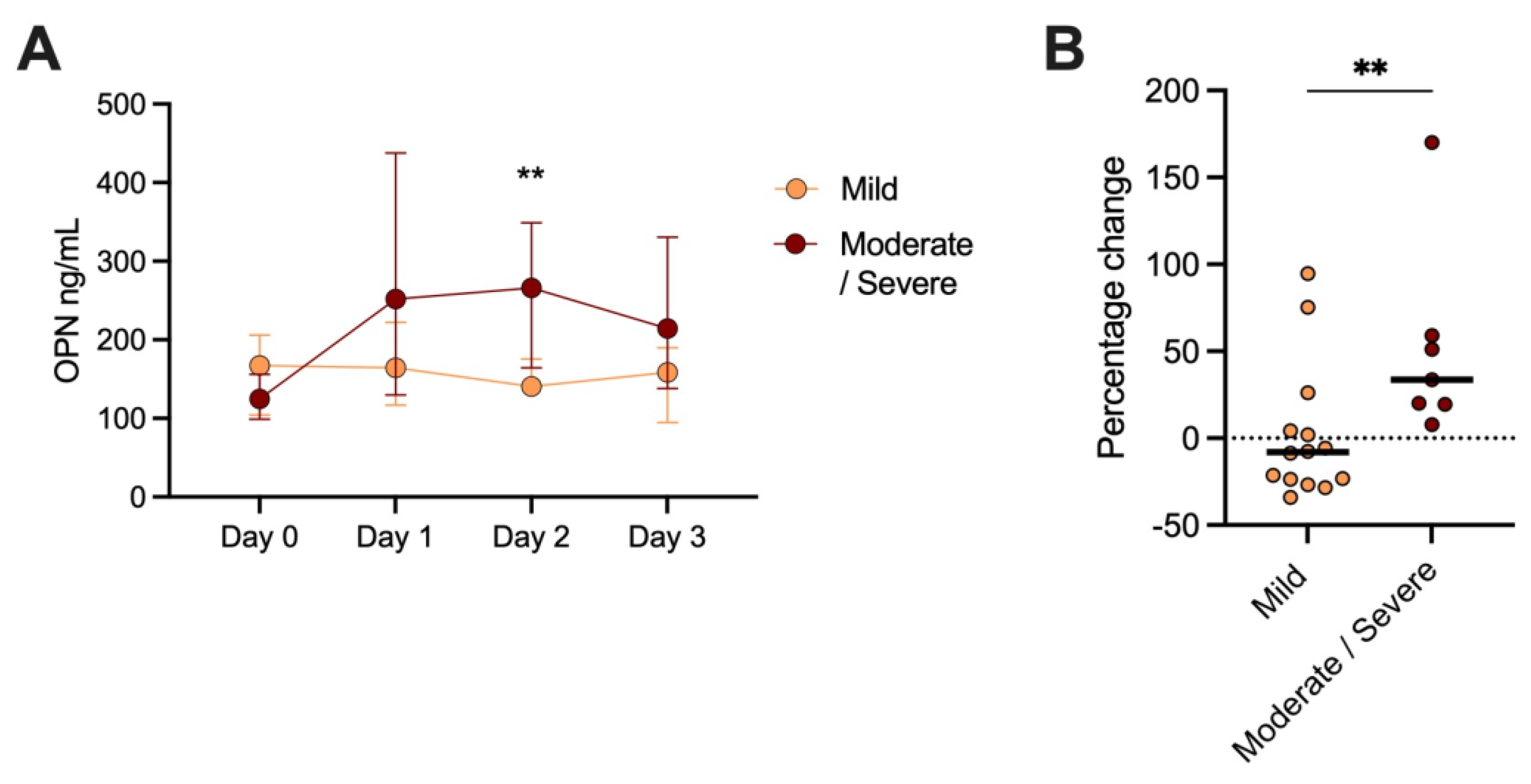
3.2. OPN Levels and AP Severity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AP | acute pancreatitis |
| APACHE | acute physiology and chronic health evaluation |
| CRP | C-reactive protein |
| OPN | osteopontin |
| SIRS | systemic inflammatory response syndrome |
| SLE | systemic lupus erythematosus |
References
- Mederos, M.A.; Reber, H.A.; Girgis, M.D. Acute Pancreatitis: A Review. JAMA 2021, 325, 382–390. [Google Scholar] [CrossRef]
- Staubli, S.M.; Oertli, D.; Nebiker, C.A. Laboratory markers predicting severity of acute pancreatitis. Crit. Rev. Clin. Lab. Sci. 2015, 52, 273–283. [Google Scholar] [CrossRef]
- Harshit Kumar, A.; Singh Griwan, M. A comparison of APACHE II, BISAP, Ranson’s score and modified CTSI in predicting the severity of acute pancreatitis based on the 2012 revised Atlanta Classification. Gastroenterol. Rep. 2018, 6, 127–131. [Google Scholar] [CrossRef] [Green Version]
- Enocsson, H.; Karlsson, J.; Li, H.Y.; Wu, Y.; Kushner, I.; Wetterö, J.; Sjöwall, C. The Complex Role of C-Reactive Protein in Systemic Lupus Erythematosus. J. Clin. Med. 2021, 10, 5837. [Google Scholar] [CrossRef] [PubMed]
- Alford, A.I.; Hankenson, K.D. Matricellular proteins: Extracellular modulators of bone development, remodeling, and regeneration. Bone 2006, 38, 749–757. [Google Scholar] [CrossRef] [PubMed]
- Vaschetto, R.; Nicola, S.; Olivieri, C.; Boggio, E.; Piccolella, F.; Mesturini, R.; Damnotti, F.; Colombo, D.; Navalesi, P.; Della Corte, F.; et al. Serum levels of osteopontin are increased in SIRS and sepsis. Intensive Care Med. 2008, 34, 2176–2184. [Google Scholar] [CrossRef]
- Lund, S.A.; Giachelli, C.M.; Scatena, M. The role of osteopontin in inflammatory processes. J. Cell Commun. Signal. 2009, 3, 311–322. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ashkar, S.; Weber, G.F.; Panoutsakopoulou, V.; Sanchirico, M.E.; Jansson, M.; Zawaideh, S.; Rittling, S.R.; Denhardt, D.T.; Glimcher, M.J.; Cantor, H. Eta-1 (osteopontin): An early component of type-1 (cell-mediated) immunity. Science 2000, 287, 860–864. [Google Scholar] [CrossRef]
- Martin-Marquez, B.T.; Sandoval-Garcia, F.; Corona-Meraz, F.I.; Petri, M.H.; Gutierrez-Mercado, Y.K.; Vazquez-Del Mercado, M. Osteopontin: Another piece in the systemic lupus erythematosus immunopathology puzzle. Clin. Exp. Rheumatol. 2022, 40, 173–182. [Google Scholar] [CrossRef]
- Frittoli, R.B.; Vivaldo, J.F.; Costallat, L.T.L.; Appenzeller, S. Gastrointestinal involvement in systemic lupus erythematosus: A systematic review. J. Transl. Autoimmun. 2021, 4, 100106. [Google Scholar] [CrossRef]
- Wirestam, L.; Frodlund, M.; Enocsson, H.; Skogh, T.; Wetterö, J.; Sjöwall, C. Osteopontin is associated with disease severity and antiphospholipid syndrome in well characterised Swedish cases of SLE. Lupus Sci. Med. 2017, 4, e000225. [Google Scholar] [CrossRef] [Green Version]
- Swärd, P.; Bertilsson, S.; Struglics, A.; Kalaitzakis, E. Serum Osteopontin Is Associated with Organ Failure in Patients with Acute Pancreatitis. Pancreas 2018, 47, e7–e10. [Google Scholar] [CrossRef] [PubMed]
- Rao, C.; Bush, N.; Rana, S.S.; Sharma, R.K.; Rana, S.; Jeyashree, K.; Gupta, R. Plasma Osteopontin Levels as an Early Predictor of Mortality in Acute Pancreatitis: A Preliminary Study. Pancreas 2022, 51, e77–e79. [Google Scholar] [CrossRef]
- Banks, P.A.; Bollen, T.L.; Dervenis, C.; Gooszen, H.G.; Johnson, C.D.; Sarr, M.G.; Tsiotos, G.G.; Vege, S.S.; Acute Pancreatitis Classification Working Group. Classification of acute pancreatitis—2012: Revision of the Atlanta classification and definitions by international consensus. Gut 2013, 62, 102–111. [Google Scholar] [CrossRef] [PubMed]
- Balthazar, E.J.; Freeny, P.C.; van Sonnenberg, E. Imaging and intervention in acute pancreatitis. Radiology 1994, 193, 297–306. [Google Scholar] [CrossRef] [PubMed]
- Marshall, J.C.; Cook, D.J.; Christou, N.V.; Bernard, G.R.; Sprung, C.L.; Sibbald, W.J. Multiple organ dysfunction score: A reliable descriptor of a complex clinical outcome. Crit. Care Med. 1995, 23, 1638–1652. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Sjöwall, C.; Ernerudh, J.; Bengtsson, A.A.; Sturfelt, G.; Skogh, T. Reduced anti-TNFα autoantibody levels coincide with flare in systemic lupus erythematosus. J. Autoimmun. 2004, 22, 315–323. [Google Scholar] [CrossRef]
- Rullo, O.J.; Woo, J.M.; Parsa, M.F.; Hoftman, A.D.; Maranian, P.; Elashoff, D.A.; Niewold, T.B.; Grossman, J.M.; Hahn, B.H.; McMahon, M.; et al. Plasma levels of osteopontin identify patients at risk for organ damage in systemic lupus erythematosus. Arthritis Res. Ther. 2013, 15, R18. [Google Scholar] [CrossRef] [Green Version]
- Wirestam, L.; Enocsson, H.; Skogh, T.; Padyukov, L.; Jönsen, A.; Urowitz, M.B.; Gladman, D.D.; Romero-Diaz, J.; Bae, S.C.; Fortin, P.R.; et al. Osteopontin and Disease Activity in Patients with Recent-onset Systemic Lupus Erythematosus: Results from the SLICC Inception Cohort. J. Rheumatol. 2019, 46, 492–500. [Google Scholar] [CrossRef]
- Ismail, O.Z.; Bhayana, V. Lipase or amylase for the diagnosis of acute pancreatitis? Clin. Biochem. 2017, 50, 1275–1280. [Google Scholar] [CrossRef] [PubMed]
| All Patients | Mild (n = 26) | Moderate/Severe (n = 11) | ||
|---|---|---|---|---|
| Sex, female, n (%) | 20 (54) | 14 (54) | 6 (55) | ns |
| Age, median (IQR), years | 54 (34–60) | 54 (28–60) | 56 (46–67) | ns |
| BMI, median (IQR) | 28 (26–33.5) | 28 (26–33) | 29 (25–34.5) | ns |
| Prior AP, n (%) | 10 (27) | 9 (15) | 1 (9) | ns |
| SIRS, n (%) | 9 (24) | 4 (15) | 5 (46) | ns |
| CRP, median (IQR), mg/L | 5 (5–19) | 9 (5–27) | 5 (5–7.5) | ns |
| IL-6, median (IQR), ng/L | 45 (10–87) | 35 (10–81) | 55 (31–168) | ns |
| Procalcitonin (IQR), µg/L | 0.13 (0.05–0.65) | 0.2 (0.05–0.4) | 0.05 (0.05–0.83) | ns |
| Amylase (IQR), µkat/L | 18.3 (5.9–32.0) | 20.5 (6.1–32.9) | 10.1 (5.8–27.4) | ns |
| Length of hospital stay, median (IQR), days | 5 (4–8) | 5 (3–6) | 10 (7.5–16.5) | <0.001 |
| ICU care, n (%) | 2 (5) | 0 (0) | 2 (18) | ns |
| Rehospitalization within 90 days, n (%) | 4 (11) | 2 (8) | 2 (18) | ns |
| Charlson comorbidity index [17] | 0 (0–1) | 0 (0–0) | 0 (0–1) | ns |
| Marshall score [16] | 0 (0–0) | 0 (0–0) | 0 (0–0) | ns |
| Computed Tomography performed, n (%) | 19 (51) | 11 (42) | 8 (73) | ns |
| Balthazar score [15] | 2 (1–4) | 2 (0–2) | 4 (2–6) | ns |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wirestam, L.; Nyberg, P.B.; Dzhendov, T.; Gasslander, T.; Sandström, P.; Sjöwall, C.; Björnsson, B. Plasma Osteopontin Reflects Tissue Damage in Acute Pancreatitis. Biomedicines 2023, 11, 1627. https://doi.org/10.3390/biomedicines11061627
Wirestam L, Nyberg PB, Dzhendov T, Gasslander T, Sandström P, Sjöwall C, Björnsson B. Plasma Osteopontin Reflects Tissue Damage in Acute Pancreatitis. Biomedicines. 2023; 11(6):1627. https://doi.org/10.3390/biomedicines11061627
Chicago/Turabian StyleWirestam, Lina, Pernilla Benjaminsson Nyberg, Todor Dzhendov, Thomas Gasslander, Per Sandström, Christopher Sjöwall, and Bergthor Björnsson. 2023. "Plasma Osteopontin Reflects Tissue Damage in Acute Pancreatitis" Biomedicines 11, no. 6: 1627. https://doi.org/10.3390/biomedicines11061627
APA StyleWirestam, L., Nyberg, P. B., Dzhendov, T., Gasslander, T., Sandström, P., Sjöwall, C., & Björnsson, B. (2023). Plasma Osteopontin Reflects Tissue Damage in Acute Pancreatitis. Biomedicines, 11(6), 1627. https://doi.org/10.3390/biomedicines11061627







