Conservative Treatment of Dental Non-Carious Cervical Lesions: A Scoping Review
Abstract
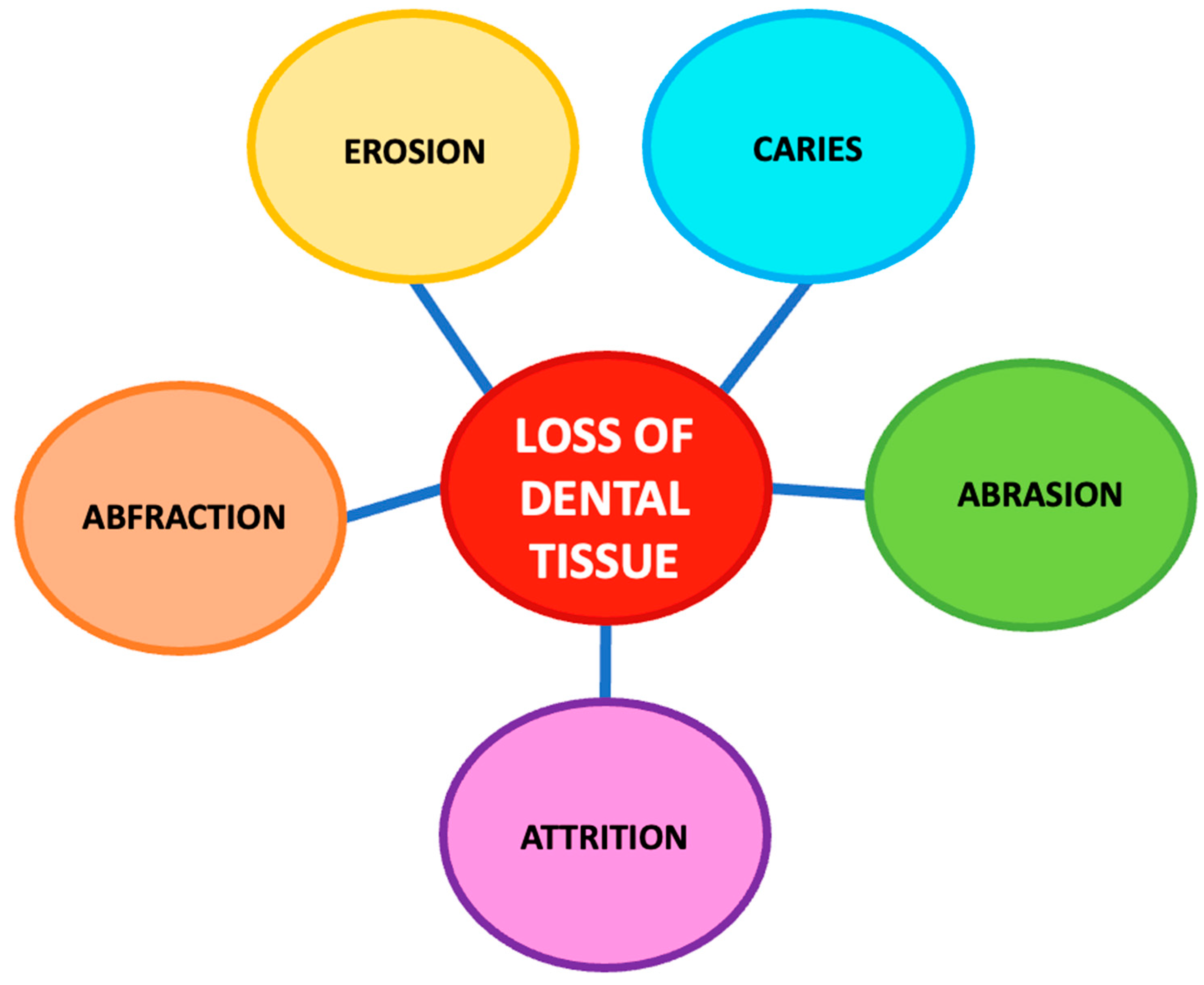
1. Introduction
1.1. Dental Abrasion
1.2. Dental Abfraction
1.3. Dental Erosion
1.4. Dental Attrition
1.5. Management of NCCLs
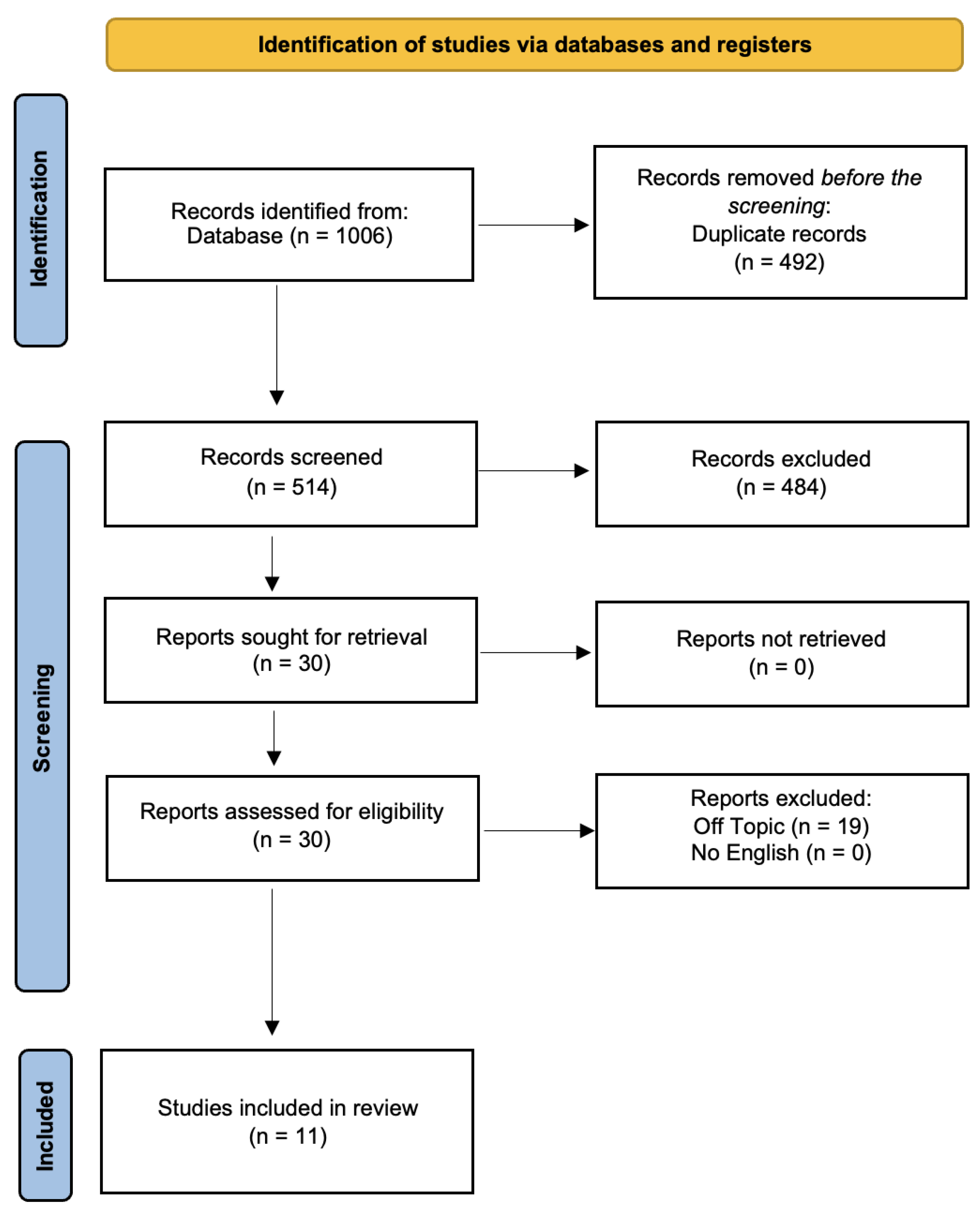
2. Materials and Methods
2.1. Protocol and Registration
2.2. Search Processing
2.3. Inclusion Criteria
2.4. Data Processing
2.5. PICOS Criteria
3. Results
4. Discussion
4.1. Analysis of Conservative Methods
4.2. Effect of Diode Laser Application
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| DH | dentin hypersensitivity |
| EC | enamel conditioning |
| EDTA | ethylenediaminetetraacetic acid pretreatment |
| GH | glass hybrid |
| NCCL | non-carious cervical lesion |
| NCCLs | non-carious cervical lesions |
| NR | New restoration |
| RBC | nano-ceramic composite resin |
| RC | composite restoration |
| RMGIC | glass ionomer cement control repair |
| RMGIC | Resin-modified glass-ionomer cements |
| SBU | Single bond universal/Filtek Z350xt |
References
- Walter, C.; Kress, E.; Götz, H.; Taylor, K.; Willershausen, I.; Zampelis, A. The anatomy of non-carious cervical lesions. Clin. Oral Investig. 2014, 18, 139–146. [Google Scholar] [CrossRef] [PubMed]
- Dipalma, G.; Inchingolo, A.D.; Inchingolo, F.; Charitos, I.A.; Cosola, M.D.; Cazzolla, A.P. Focus on the cariogenic process: Microbial and biochemical interactions with teeth and oral environment. J. Biol. Regul. Homeost. Agents 2021, 35, 429–440. [Google Scholar] [CrossRef]
- Osborne-Smith, K.L.; Burke, F.J.; Wilson, N.H. The aetiology of the non-carious cervical lesion. Int. Dent. J. 1999, 49, 139–143. [Google Scholar] [CrossRef] [PubMed]
- Goodacre, C.J.; Eugene Roberts, W.; Munoz, C.A. Noncarious cervical lesions: Morphology and progression, prevalence, etiology, pathophysiology, and clinical guidelines for restoration. J. Prosthodont. 2023, 32, e1–e18. [Google Scholar] [CrossRef] [PubMed]
- Levitch, L.C.; Bader, J.D.; Shugars, D.A.; Heymann, H.O. Non-carious cervical lesions. J. Dent. 1994, 22, 195–207. [Google Scholar] [CrossRef] [PubMed]
- Borcic, J.; Anic, I.; Urek, M.M.; Ferreri, S. The prevalence of non-carious cervical lesions in permanent dentition. J. Oral Rehabil. 2004, 31, 117–123. [Google Scholar] [CrossRef]
- Yang, J.; Cai, D.; Wang, F.; He, D.; Ma, L.; Jin, Y.; Que, K. Non-carious cervical lesions (NCCLs) in a random sampling community population and the association of NCCLs with occlusive wear. J. Oral Rehabil. 2016, 43, 960–966. [Google Scholar] [CrossRef]
- Kolak, V.; Pešić, D.; Melih, I.; Lalović, M.; Nikitović, A.; Jakovljević, A. Epidemiological investigation of non-carious cervical lesions and possible etiological factors. J. Clin. Exp. Dent. 2018, 10, e648–e656. [Google Scholar] [CrossRef]
- Skośkiewicz-Malinowska, K.; Noack, B.; Kaderali, L.; Malicka, B.; Lorenz, K.; Walczak, K.; Weber, M.-T.; Mendak-Ziółko, M.; Hoffmann, T.; Ziętek, M.; et al. Oral Health and Quality of Life in Old Age: A Cross-Sectional Pilot Project in Germany and Poland. Adv. Clin. Exp. 2016, 25, 951–959. [Google Scholar] [CrossRef]
- Kaidonis, J.A. Tooth wear: The view of the anthropologist. Clin. Oral Investig. 2008, 12, 21–26. [Google Scholar] [CrossRef]
- Davies, S.J.; Gray, R.J.M.; Qualtrough, A.J.E. Management of tooth surface loss. Br. Dent. J. 2002, 192, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Bartlett, D.W.; Fares, J.; Shirodaria, S.; Chiu, K.; Ahmad, N.; Sherriff, M. The association of tooth wear, diet and dietary habits in adults aged 18-30 years old. J. Dent. 2011, 39, 811–816. [Google Scholar] [CrossRef] [PubMed]
- Marinelli, G.; Inchingolo, A.D.; Inchingolo, A.M.; Malcangi, G.; Limongelli, L.; Montenegro, V.; Coloccia, G.; Laudadio, C.; Patano, A.; Inchingolo, F.; et al. White spot lesions in orthodontics: Prevention and treatment. A descriptive review. J. Biol. Regul. Homeost. Agents 2021, 35, 227–240. [Google Scholar] [CrossRef] [PubMed]
- Van’t Spijker, A.; Rodriguez, J.M.; Kreulen, C.M.; Bronkhorst, E.M.; Bartlett, D.W.; Creugers, N.H.J. Prevalence of tooth wear in adults. Int. J. Prosthodont. 2009, 22, 35–42. [Google Scholar]
- Pecie, R.; Krejci, I.; García-Godoy, F.; Bortolotto, T. Noncarious cervical lesions (NCCL)—A clinical concept based on the literature review. Part 2: Restoration. Am. J. Dent. 2011, 24, 183–192. [Google Scholar]
- Santacroce, L.; Charitos, I.A.; Ballini, A.; Inchingolo, F.; Luperto, P.; De Nitto, E.; Topi, S. The Human Respiratory System and its Microbiome at a Glimpse. Biology 2020, 9, 318. [Google Scholar] [CrossRef]
- Wood, I.; Jawad, Z.; Paisley, C.; Brunton, P. Non-carious cervical tooth surface loss: A literature review. J. Dent. 2008, 36, 759–766. [Google Scholar] [CrossRef]
- Michael, J.A.; Kaidonis, J.A.; Townsend, G.C. Non-carious cervical lesions: A scanning electron microscopic study. Aust. Dent. J. 2010, 55, 138–142. [Google Scholar] [CrossRef]
- Yılmaz, N.; Baygin, O.; Tüzüner, T.; Turgut, S.N.; Erbek, Ş.M. Evaluation of the effect of pediatric drugs and an oral rinse on primary teeth discoloration. Dent. Med. Probl. 2022, 59, 225–231. [Google Scholar] [CrossRef]
- Dababneh, R.H.; Khouri, A.T.; Addy, M. Dentine hypersensitivity-an enigma? A review of terminology, mechanisms, aetiology and management. Br. Dent. J. 1999, 187, 606–611. [Google Scholar] [CrossRef]
- Addy, M.; Hunter, M.L. Can tooth brushing damage your health? Effects on oral and dental tissues. Int. Dent. J. 2003, 53 (Suppl. S3), 177–186. [Google Scholar] [CrossRef] [PubMed]
- Takamizawa, T.; Barkmeier, W.W.; Sai, K.; Tsujimoto, A.; Imai, A.; Erickson, R.L.; Latta, M.A.; Miyazaki, M. Influence of different smear layers on bond durability of self-etch adhesives. Dent. Mater. 2018, 34, 246–259. [Google Scholar] [CrossRef] [PubMed]
- Addy, M.; Shellis, R.P. Interaction between attrition, abrasion and erosion in tooth wear. Monogr. Oral Sci. 2006, 20, 17–31. [Google Scholar] [CrossRef]
- Casu, C.; Mosaico, G.; Natoli, V.; Scarano, A.; Lorusso, F.; Inchingolo, F. Microbiota of the Tongue and Systemic Connections: The Examination of the Tongue as an Integrated Approach in Oral Medicine. Hygiene 2021, 1, 56–68. [Google Scholar] [CrossRef]
- Litonjua, L.A.; Andreana, S.; Cohen, R.E. Toothbrush abrasions and noncarious cervical lesions: Evolving concepts. Compend. Contin. Educ. Dent. (Jamesburg NJ 1995) 2005, 26, 767–768, 770–774, 776 passim. [Google Scholar]
- Bergström, J.; Lavstedt, S. An epidemiologic approach to toothbrushing and dental abrasion. Community Dent. Oral Epidemiol. 1979, 7, 57–64. [Google Scholar] [CrossRef]
- Jiang, H.; Du, M.Q.; Huang, W.; Peng, B.; Bian, Z.; Tai, B.J. The prevalence of and risk factors for non-carious cervical lesions in adults in Hubei Province, China. Community Dent. Health 2011, 28, 22–28. [Google Scholar]
- Rapone, B.; Ferrara, E.; Santacroce, L.; Topi, S.; Gnoni, A.; Dipalma, G.; Mancini, A.; Di Domenico, M.; Tartaglia, G.M.; Scarano, A.; et al. The Gaseous Ozone Therapy as a Promising Antiseptic Adjuvant of Periodontal Treatment: A Randomized Controlled Clinical Trial. Int. J. Environ. Res. Public. Health 2022, 19, 985. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Malcangi, G.; Semjonova, A.; Inchingolo, A.M.; Patano, A.; Coloccia, G.; Ceci, S.; Marinelli, G.; Di Pede, C.; Ciocia, A.M.; et al. Oralbiotica/Oralbiotics: The Impact of Oral Microbiota on Dental Health and Demineralization: A Systematic Review of the Literature. Children 2022, 9, 1014. [Google Scholar] [CrossRef]
- Rees, J.S. The biomechanics of abfraction. Proc. Inst. Mech. Eng. H 2006, 220, 69–80. [Google Scholar] [CrossRef]
- Chu, F.C.S.; Yip, H.K.; Newsome, P.R.H.; Chow, T.W.; Smales, R.J. Restorative management of the worn dentition: I. Aetiology and diagnosis. Dent. Update 2002, 29, 162–168. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, A.D.; Inchingolo, A.M.; Malcangi, G.; Avantario, P.; Azzollini, D.; Buongiorno, S.; Viapiano, F.; Campanelli, M.; Ciocia, A.M.; De Leonardis, N.; et al. Effects of Resveratrol, Curcumin and Quercetin Supplementation on Bone Metabolism-A Systematic Review. Nutrients 2022, 14, 3519. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.E.; Lin, C.L.; Wang, C.H.; Cheng, C.H.; Chang, C.H. Stresses at the cervical lesion of maxillary premolar--a finite element investigation. J. Dent. 2002, 30, 283–290. [Google Scholar] [CrossRef] [PubMed]
- Rees, J.S.; Hammadeh, M.; Jagger, D.C. Abfraction lesion formation in maxillary incisors, canines and premolars: A finite element study. Eur. J. Oral Sci. 2003, 111, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Bernhardt, O.; Gesch, D.; Schwahn, C.; Mack, F.; Meyer, G.; John, U.; Kocher, T. Epidemiological evaluation of the multifactorial aetiology of abfractions. J. Oral Rehabil. 2006, 33, 17–25. [Google Scholar] [CrossRef]
- West, N.X.; Hughes, J.A.; Addy, M. Erosion of dentine and enamel in vitro by dietary acids: The effect of temperature, acid character, concentration and exposure time. J. Oral Rehabil. 2000, 27, 875–880. [Google Scholar] [CrossRef]
- Johansson, A.-K.; Lingström, P.; Imfeld, T.; Birkhed, D. Influence of drinking method on tooth-surface pH in relation to dental erosion. Eur. J. Oral Sci. 2004, 112, 484–489. [Google Scholar] [CrossRef]
- Barbour, M.E.; Rees, G.D. The role of erosion, abrasion and attrition in tooth wear. J. Clin. Dent. 2006, 17, 88–93. [Google Scholar]
- Asadian, F.; Hoseini, A.P.; Ahmadian, L.; Rafeie, N.; Rezaei, S.; Moradi, Z. In vitro attrition wear resistance of four types of paste-like bulk-fill composite resins. BMC Oral Health 2022, 22, 360. [Google Scholar] [CrossRef]
- Roberts, W.E.; Mangum, J.E.; Schneider, P.M. Pathophysiology of Demineralization, Part I: Attrition, Erosion, Abfraction, and Noncarious Cervical Lesions. Curr. Osteoporos. Rep. 2022, 20, 90–105. [Google Scholar] [CrossRef]
- Rees, J.S. The effect of variation in occlusal loading on the development of abfraction lesions: A finite element study. J. Oral Rehabil. 2002, 29, 188–193. [Google Scholar] [CrossRef] [PubMed]
- Salem, M.N.; Hafez, S. Aesthetic Management of Erosive Tooth Wear in a Young Egyptian Swimmer: A Case Report. Clin. Cosmet. Investig. Dent. 2021, 13, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Lussi, A.; Carvalho, T.S. Erosive tooth wear: A multifactorial condition of growing concern and increasing knowledge. Monogr. Oral Sci. 2014, 25, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Heintze, S.D.; Ruffieux, C.; Rousson, V. Clinical performance of cervical restorations—A meta-analysis. Dent. Mater. 2010, 26, 993–1000. [Google Scholar] [CrossRef]
- Santos, M.J.M.C.; Ari, N.; Steele, S.; Costella, J.; Banting, D. Retention of tooth-colored restorations in non-carious cervical lesions--a systematic review. Clin. Oral Investig. 2014, 18, 1369–1381. [Google Scholar] [CrossRef]
- Peumans, M.; Politano, G.; Van Meerbeek, B. Treatment of noncarious cervical lesions: When, why, and how. Int. J. Esthet. Dent. 2020, 15, 16–42. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 88, 105906. [Google Scholar] [CrossRef]
- Saghir, A.; Rehman, T.; Irum, B.; Afreen, Z.; Ammarah; Nawaz, F.N. 12 Month’s Assessment Of Clinical Efficacy Of Resin Modified Glass Ionomer Cement And Flowable Composites In Restoration Of Non-Carious Cervical Lesions, A Randomized Clinical Trial. J. Ayub Med. Coll. Abbottabad 2023, 35, 7–10. [Google Scholar] [CrossRef]
- Caneppele, T.M.F.; Meirelles, L.C.F.; Rocha, R.S.; Gonçalves, L.L.; Ávila, D.M.S.; Gonçalves, S.E.d.P.; Bresciani, E. A 2-year clinical evaluation of direct and semi-direct resin composite restorations in non-carious cervical lesions: A randomized clinical study. Clin. Oral Investig. 2020, 24, 1321–1331. [Google Scholar] [CrossRef]
- Oz, F.D.; Ergin, E.; Canatan, S. Twenty-four-month clinical performance of different universal adhesives in etch-and-rinse, selective etching and self-etch application modes in NCCL—A randomized controlled clinical trial. J. Appl. Oral Sci. 2019, 27, e20180358. [Google Scholar] [CrossRef]
- Reddy, S.; Mandadi, L.R.; Mala, K.; Abhinav, T.N.; Dave, A.; Thomas, M.S. Clinical Effectiveness of Composite Resin Bonded with Universal Adhesive for the Restoration of Non-Carious Cervical Lesions Using Air Abrasion: A Randomised Controlled Trial. Arch. Orofac. Sci. 2022, 17, 123–135. [Google Scholar] [CrossRef]
- Canali, G.D.; Ignácio, S.A.; Rached, R.N.; Souza, E.M. One-year clinical evaluation of bulk-fill flowable vs. regular nanofilled composite in non-carious cervical lesions. Clin. Oral Investig. 2019, 23, 889–897. [Google Scholar] [CrossRef] [PubMed]
- Jassal, M.; Mittal, S.; Tewari, S. Clinical Effectiveness of a Resin-modified Glass Ionomer Cement and a Mild One-step Self-etch Adhesive Applied Actively and Passively in Noncarious Cervical Lesions: An 18-Month Clinical Trial. Oper. Dent. 2018, 43, 581–592. [Google Scholar] [CrossRef] [PubMed]
- Lührs, A.; Jacker-Guhr, S.; Günay, H.; Herrmann, P. Composite restorations placed in non-carious cervical lesions—Which cavity preparation is clinically reliable? Clin. Exp. Dent. Res. 2020, 6, 558–567. [Google Scholar] [CrossRef] [PubMed]
- Schwendicke, F.; Müller, A.; Seifert, T.; Jeggle-Engbert, L.-M.; Paris, S.; Göstemeyer, G. Glass hybrid versus composite for non-carious cervical lesions: Survival, restoration quality and costs in randomized controlled trial after 3 years. J. Dent. 2021, 110, 103689. [Google Scholar] [CrossRef]
- Koc Vural, U.; Meral, E.; Ergin, E.; Gürgan, S. Twenty-four-month clinical performance of a glass hybrid restorative in non-carious cervical lesions of patients with bruxism: A split-mouth, randomized clinical trial. Clin. Oral Investig. 2020, 24, 1229–1238. [Google Scholar] [CrossRef]
- Akarsu, S.; Karademir, S.A.; Ertas, E.; Atasoy, S. The Effect of Diode Laser Application on Restoration of Non Carious Cervical Lesion: Clinical Follow Up. Niger. J. Clin. Pract. 2020, 23, 165. [Google Scholar] [CrossRef]
- Gonçalves, D.F.M.; Shinohara, M.S.; de Andrade Carvalho, P.R.M.; Ramos, F.D.S.; Oliveira, L.D.C.; Omoto, É.M.; Fagundes, T.C. Three-year evaluation of different adhesion strategies in non-carious cervical lesion restorations: A randomized clinical trial. J. Appl. Oral Sci. 2021, 29, e20210192. [Google Scholar] [CrossRef]
- Beerens, M.W.; Ten Cate, J.M.; Buijs, M.J.; van der Veen, M.H. Long-term remineralizing effect of MI Paste Plus on regression of early caries after orthodontic fixed appliance treatment: A 12-month follow-up randomized controlled trial. Eur. J. Orthod. 2018, 40, 457–464. [Google Scholar] [CrossRef]
| Criteria | Application in the Present Study |
| Population | Subjects with NCCLs |
| Intervention | Conservative treatments of NCCLs |
| Comparisons | Comparing before and post intervention |
| Outcomes | Improvements as a result of the techniques used |
| Study design | Clinical Trial |
| Authors | Type of Study | Object | Study Design and Timeline | Type of Initial Restoration Placement or Repair of Existing Restorations | Lesions Sensitive or Not before Restoration | Conditioning Protocol Used for the Surface | Mechanical Preparation of the Surface | Results |
|---|---|---|---|---|---|---|---|---|
| Atikah Saghir et al. [48] | Randomized Clinical Trial | Comparison of the clinical efficacy of resin-modified glass ionomer and flowable composite in the treatment of NCCLs. | 60 patients with at least 2 NCCLs divided into 2 groups: (1) treatment with flowable composite; (2) treatment with resin-modified glass ionomer cement. | Placement of new restoration in NCCLs with depth of 1–2 mm | Not specified | Tooth etching with 37% phosphoric acid | Not specified | NCCLs treated with Resin modified glass ionomer cement is superior to flowable composite in terms of retention and surface texture. |
| Taciana Marco Ferraz Caneppele et al. [49] | Randomized Clinical Study | To assess the effectiveness of resin composite restorations in NCCLs after 2 years utilizing direct or semi-direct techniques. | 30 volunteers with at least 2 NCCLs. Each participant received one restoration with direct technique and one with indirect technique. Follow-up: baseline, 7 days, 6, 12 and 24 months. | New restorations have been made | Not specified | The surface was etched with 37% phosphoric acid gel | No tooth preparation was performed. | The tested restorative methods produce comparable effects for NCCLs during the study periods. |
| Fatma Dilsad OZ et al. [50] | Randomized Clinical Trial | To assess the effectiveness of two distinct universal adhesives and one etch-rinse glue for NCCL restoration. | 20 patients with at least 7 NCCLs divided into 7 groups according to adhesive systems and application modes. Follow-up: 1 week, 6, 12 and 24 months. | New restorations of NCCLs have been made | Patients who rated their hypersensitivity with a maximum value of 7 on a scale of 0 to 10 | Phosphoric acid etching gel (37%) was applied to enamel for 30s then rinsed and dried | Not specified | In terms of retention, GLUMA Universal and All- Bond Universal outperformed the self-etch mode in etch-and-rinse and selective etching modes. |
| Shanthana Reddy et al. [51] | Randomized Controlled trial | To assess the clinical efficacy of nanocomposite restorations for NCCLs bonded with universal adhesive in self-etch mode with and without air abrasive surface treatment. | 70 NCCLs divided into 2 groups: (1) surface treatment with alumina air abrasion; (2) control group. NCCLs were restored with nanocomposite using universal bonding (self-etch mode). Follow-up: baseline, 3, 6, 12 months. | Teeth with cervical carious lesions and previously restored teeth. | Pre-operative sensistivity with Schiff’s scale: = (no response); 1 (mild response), 2 (moderate response); 3 (severe response) | Not specified | Lesion cleaned using pumice slurry | The clinical efficacy of nanocomposite resin bonded with universal adhesive was not improved by airborne particle abrasion of NCCLs. |
| Gabriela D. Canali et al. [52] | Randomized trial | To assess the efficacy of a bulk-fill flowable and a regular nanofilled composite in NCCLs after one year. | 22 patients with at least 2 NCCLs. A universal adhesive was used with a self-etching approach in dentin. Follow-up: baseline (7 days), 6 months and 1 year. | New restorations of lesions | Not specified | 32% phosphoric acid for 15 s on enamel | Enamel margins beveled with a diamond bur at high speed | After one year, both composite resins demonstrated acceptable clinical efficacy in the restoration of NCCLs. |
| M. Jassal et al. [53] | Randomized Clinical Trial | To compare the clinical efficacy of two techniques of applying a moderate one-step self-etch adhesive and composite resin in NCCLs with a resin-modified glass ionomer cement control repair (RMGIC). | 294 restorations in 56 patients divided into 3 groups: (1) G-Bond active application combined with Solare-X composite resin; (2) G-Bond passive application combined with Solare-X composite resin; (3) GC II LC RMGIC. Follow-up: 6, 12 and 18 months. | New restorations of lesions ≥ 1 mm | 18 of 294 NCCLs had preoperative sensitivity | Dentin conditioner for 10 s before RMGIC | Lesions were cleaned using rubber cup with pumice. No additional bevel | In the repair of NCCLs, a mild one-step self-etch adhesive followed by a resin composite restoration might be an alternative to RMGIC with comparable retention and enhanced aesthetics. |
| Anne-Katrin Lührs et al. [54] | Randomized Clinical Trial | To assess the clinical performance of restorations placed in NCCLs using different cavity preparation strategies. | 85 NCCLs were treated with different cavity preparations and subsequent restoration. | New restorations of NCCLs have been made | Not specified | Selective enamel etching for 30 s with 36% phosphoric acid gel | In group 2 and 3 dentin surface is bevelled with round bur | Composites are long-lasting materials for NCCL restoration. Restorations that were put without any dentin preparation (just cavity cleaning) had the greatest loss rate. |
| Falk Schwendicke et al. [55] | Randomized Clinical Trial | To evaluate the survivability, restoration quality, and costs of glass hybrid and resin restorations on sclerotic NCCLs. | 88 patients with 175 NCCLs were were randomized to receive glass hybrid (GH) or composite restorations (RC). | New restorations have been made | Not specified | For RC etching with 37% phosphoric acid gel | Surfaces cleaned using a polishing brush. No mechanical preparation | There was no significant difference between GH and RC in the survival and quality of NCCLs restorations. In addition, GH was found to be less expensive than RC. |
| Uzay Koc Vural et al. [56] | Randomized Clinical Trial | To compare the clinical efficacy of a glass hybrid restorative to that of a nano-ceramic composite resin in non-carious cervical lesions (NCCLs) of bruxism patients. | A total of 148 NCCLs were restored in a random order using either a glass hybrid (GH) restorative system or a nano-ceramic composite resin (RBC). Follow-up: at baseline, six, twelve, and twenty-four months later. | New restorations | 61 of 148 NCCLs had preoperative sensitivity | RBC restorations was etched for 15 s with 37% phosphoric acid gel | Not specified | After 24 months both evaluated restoratives demonstrated clinically acceptable performance for the restoration of NCCLs in bruxism patients. |
| S Akarsu et al. [57] | Clinical Trial | To assess the impact of the diode laser used for DH on the clinical success of NCCLs repaired with various adhesive solutions. | 20 NCCLs were restored with Universal Single Bond and Grandio after diode laser application, and 20 NCCLs were restored with Universal Single Bond (Total Etch) and Grandio. Follow-up: baseline, 6, and 18 months. | New restorations | NCCLs with tolarable sensitivity | Group 1: self-etch; Group 2: etch-and-rinse; Group 3: diode laser + self-etch; Group 4: diode laser + etch-and-rinse | No preparation on dentin or enamel. | Diode laser use prior to NCCL restoration of teeth does not reduce restoration retention rate, may decrease DH, and may affect restoration success. |
| Diego Felipe Mardegan GONÇALVES et al. [58] | Randomized Clinical Trial | To assess NCCLs restored with different adhesion techniques. | 200 NCCLs were restored with Universal Single Bond with and without enamel conditioning; resin-modified glass-ionomer cements with EDTA. Follow-up: baseline and 3 years after. | New restorations | Visual analogue scale (VAS) was used to score pain: 1 (no pain); 2 (mild); 3 (moderate); 4 (slightly worse); 5 (much worse); 6 (severe pain) | Single Bond Universal was assessed both with or without enamel conditioning | No cavity preparation | NCCL restoration retention was impacted by selective enamel etching. The EDTA-based adhesive approach followed by RMGIC postponed marginal flaws over time. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Patano, A.; Malcangi, G.; De Santis, M.; Morolla, R.; Settanni, V.; Piras, F.; Inchingolo, A.D.; Mancini, A.; Inchingolo, F.; Dipalma, G.; et al. Conservative Treatment of Dental Non-Carious Cervical Lesions: A Scoping Review. Biomedicines 2023, 11, 1530. https://doi.org/10.3390/biomedicines11061530
Patano A, Malcangi G, De Santis M, Morolla R, Settanni V, Piras F, Inchingolo AD, Mancini A, Inchingolo F, Dipalma G, et al. Conservative Treatment of Dental Non-Carious Cervical Lesions: A Scoping Review. Biomedicines. 2023; 11(6):1530. https://doi.org/10.3390/biomedicines11061530
Chicago/Turabian StylePatano, Assunta, Giuseppina Malcangi, Matteo De Santis, Roberta Morolla, Vito Settanni, Fabio Piras, Alessio Danilo Inchingolo, Antonio Mancini, Francesco Inchingolo, Gianna Dipalma, and et al. 2023. "Conservative Treatment of Dental Non-Carious Cervical Lesions: A Scoping Review" Biomedicines 11, no. 6: 1530. https://doi.org/10.3390/biomedicines11061530
APA StylePatano, A., Malcangi, G., De Santis, M., Morolla, R., Settanni, V., Piras, F., Inchingolo, A. D., Mancini, A., Inchingolo, F., Dipalma, G., & Inchingolo, A. M. (2023). Conservative Treatment of Dental Non-Carious Cervical Lesions: A Scoping Review. Biomedicines, 11(6), 1530. https://doi.org/10.3390/biomedicines11061530














