Abstract
Photoactivation of 3% hydrogen peroxide with a 445 nm diode laser represents a relatively new, insufficiently researched antimicrobial method in the treatment of peri-implantitis. The purpose of this work is to evaluate the effect of photoactivation of 3% hydrogen peroxide with a 445 nm diode laser, and to compare the obtained results with 0.2% chlorhexidine treatment and 3% hydrogen peroxide treatment without photoactivation, in vitro, on the surface of dental implants contaminated with S. aureus and C. albicans biofilms. Previously, 80 infected titanium implants with S. aureus and C. albicans cultures were divided into four groups: G1-negative control (no treatment), G2-positive control (0.2% chlorhexidine), G3 (3% hydrogen peroxide), and G4 (photoactivated 3% hydrogen peroxide). The number of viable microbes in each sample was determined by the colony forming unit (CFU) count. The results were statistically processed and analyzed, showing a statistically significant difference across all groups compared to the negative control (G1), and the absence of a statistically significant difference between groups G1–G3. The new antimicrobial treatment, according to the results, could be worthy of further analysis and research.
1. Introduction
Dental implants present a valuable therapeutic choice in the treatment of partial and complete edentulousness. However, despite the high degree of success of dental implants, vast experience and technological improvements during the last 60 years, their frequent use has also brought some very specific problems [1,2]. Peri-implant diseases (peri-implant mucositis and peri-implantitis) are probably the most significant issues associated with dental implants [3,4]. Peri-implant mucositis is defined as the presence of an inflammatory infiltrate in soft tissue induced by plaque, without loss of peri-implant bone, while peri-implantitis is a condition in which, along with soft tissue inflammation, a bone loss is present [5]. If peri-implantitis is not recognized in time and properly treated, implant loss may happen. According to Atieh et al. [6], as many as 50% of placed implants show signs of peri-mucositis, and 12–43% of implants show signs of peri-implantitis. The role of microorganisms in the development of these pathological conditions is crucial and more than 20 different species are routinely found in swabs taken from infected implants [5,7]. One specific microorganism, Staphylococcus aureus, plays a significant role in the development of peri-implantitis due to its affinity for the titanium surface of the implant and the formation of biofilms or a substrate for the growth of biofilms of other cultures, the so-called “early colonizer” [8,9]. Biofilm is defined as a microbial community of cells embedded in a polymer extracellular matrix, the creation of which is caused by microorganisms present in the matrix. Organisms inside biofilms are more resistant to different antimicrobial treatments than free, planktonic organisms [10]. Candida albicans is the most frequently isolated fungus in the human oral cavity. Despite being considered a commensal species, under certain conditions, such as periods of antibiotic use or periods of immunosuppression, it can cause mucosal infection [11]. C. albicans is often present in the peri-implant sulcus, both in healthy people and in patients with peri-implantitis, where it also creates a substrate for the formation of biofilms and supports inflammation [12].
The treatment of peri-implant diseases is a complex task due to the difficult access to the implant surface, limited visibility, the roughness of the titanium surface, and the pathogenicity of the microorganisms involved in the pathogenesis of these diseases [13,14,15]. Therefore, over time, numerous antimicrobial procedures and protocols have been developed. Scarano et al. [14] made an overview of the available treatments in a following manner: (1) mechanical debridement using plastic curettes, rubber polishers, ultrasonic scalers or air-powder abrasives; (2) chemical decontamination using chlorhexidine, citric acid, tetracycline, hydrogen peroxide, etc.; (3) dental laser-based treatments. Described procedures and techniques can also be mixed or combined, as in the newer study carried out by Alovisi et al. [16], where triple antibiotic paste and a glycine powder air-flow abrasion were used to fight microorganisms. However, none of the usual methods can completely remove or inactivate peri-implant pathogens due to previously mentioned factors, such as complex anatomical relationships and/or the specific implant surface [17]. Furthermore, it is even possible to damage this implant surface using certain antimicrobial treatments agents, which can then impair the healing of peri-implant tissues [18].
Although many treatment modalities exist, chlorhexidine digluconate (CHX) combined with manual debridement is still considered to be the golden standard in the treatment of periodontal and peri-implant diseases [19]. Hydrogen peroxide (H2O2) has been used in dentistry as a mouthwash to prevent plaque and as an antiseptic after oral surgery for more than 100 years [20], and it is also used in the treatment of peri-implantitis, but likely not as often as CHX. Photo-activation of H2O2, with the aim of improving the antimicrobial effect in periodontitis therapy, is a potentially interesting idea examined in the work of Mahdi et al. in 2015 [21].
They found a stronger disinfection potential when H2O2 was activated by LED light with a wavelength of 440–480 nm, compared to non-activated H2O2. Guided by this idea, the authors of this study wanted to examine the possibility of H2O2 activation with a 445 nm diode laser, and augmentation of its antimicrobial effect. According to authors knowledge, there is currently no research on this topic.
The purpose of this work is to evaluate the effect of photoactivation of 3% hydrogen peroxide with a 445 nm diode laser and compare the obtained values with chlorhexidine and hydrogen peroxide without photoactivation, in vitro, on the surface of implants contaminated with S. aureus and C. albicans biofilms.
The hypotheses of this study are:
- Hydrogen peroxide activated by a 445 nm diode laser shows better results in disinfection of dental implants compared to hydrogen peroxide used without 445 nm photoactivation.
- Hydrogen peroxide activated by a 445 nm diode laser shows equal or better results in disinfection of dental implants compared to chlorhexidine treatment.
2. Materials and Methods
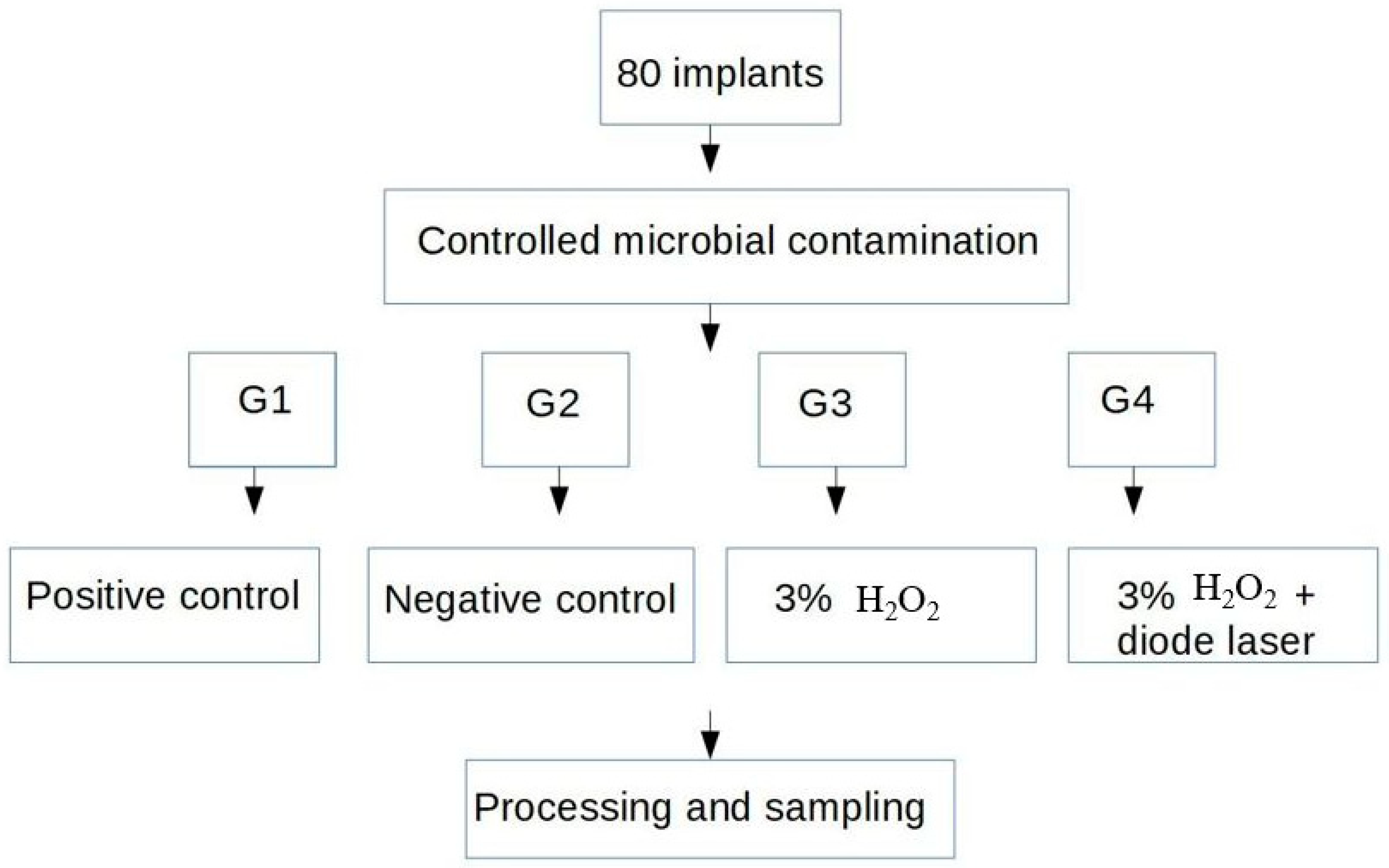
The research was conducted at the Department of Oral Surgery of the School of dental medicine in Zagreb and at the Clinical Institute for Clinical and Molecular Microbiology of KBC Zagreb, Croatia. Eighty Zimmer Biomet Tapered Screw-Vent MTX 4.1/10 mm titanium implants (Zimmer Biomet, Palm Beach Gardens, FL, USA) were used in the study. According to Ehrenfest et al. [22], these implants are grade 5 titanium core, with a surface modified by sand-blasting (resorbable blasting media—RBM like calcium phosphate). The surface was microrough, nano-smooth and homogenous. The implants used in this study were contaminated with cultures of S. aureus and C. albicans isolated from clinical samples at University hospital centre Zagreb. Bacterial and fungal strains were grown separately on Columbia agar for 72 h, after preparation of separate bacterial and fungal suspensions using a thioglycolate broth. They were then mixed into a common suspension. An optical densitometer (Densimat, Biomerieux, Marcyl’Etoile, France) determined the density at 600 nm, which corresponded to 1 × 108 CFU/mL. All dental implants were immersed in 0.3 mL of mixed bacterial–fungal suspension for 14 days under aerobic conditions, at a temperature of 35 °C. The suspension was contained with S. aureus and C. albicans, at a density of 0.5 McFarland. After that, all implants were randomly distributed into four groups, so that there were 20 implants per group (Figure 1). The implants were removed from the test tubes with sterile tweezers. The implants were then put on sterile gauze and, depending on which group they were in, went through the right cleaning process.
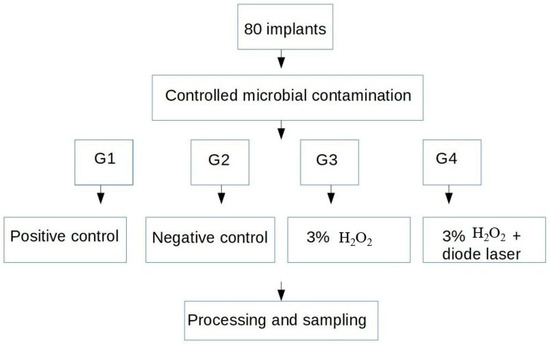
Figure 1.
Test sample distribution, contamination and disinfection outline.
2.1. Disinfection Protocols
The first group (G1) represented the negative control. This group was not subjected to any disinfection protocol and served as a reference in assessing the effectiveness of a particular disinfection protocol.
The second group (G2) represented the positive control. That group was treated with 0.2% CHX. CHX was applied on a sterile cotton pellet, and the surface of the implant was rubbed with it for 60 s.
The third group (G3) was treated with 3% hydrogen peroxide. H2O2 was applied on a sterile cotton pellet, and the surface of the implant was rubbed with it for 60 s.
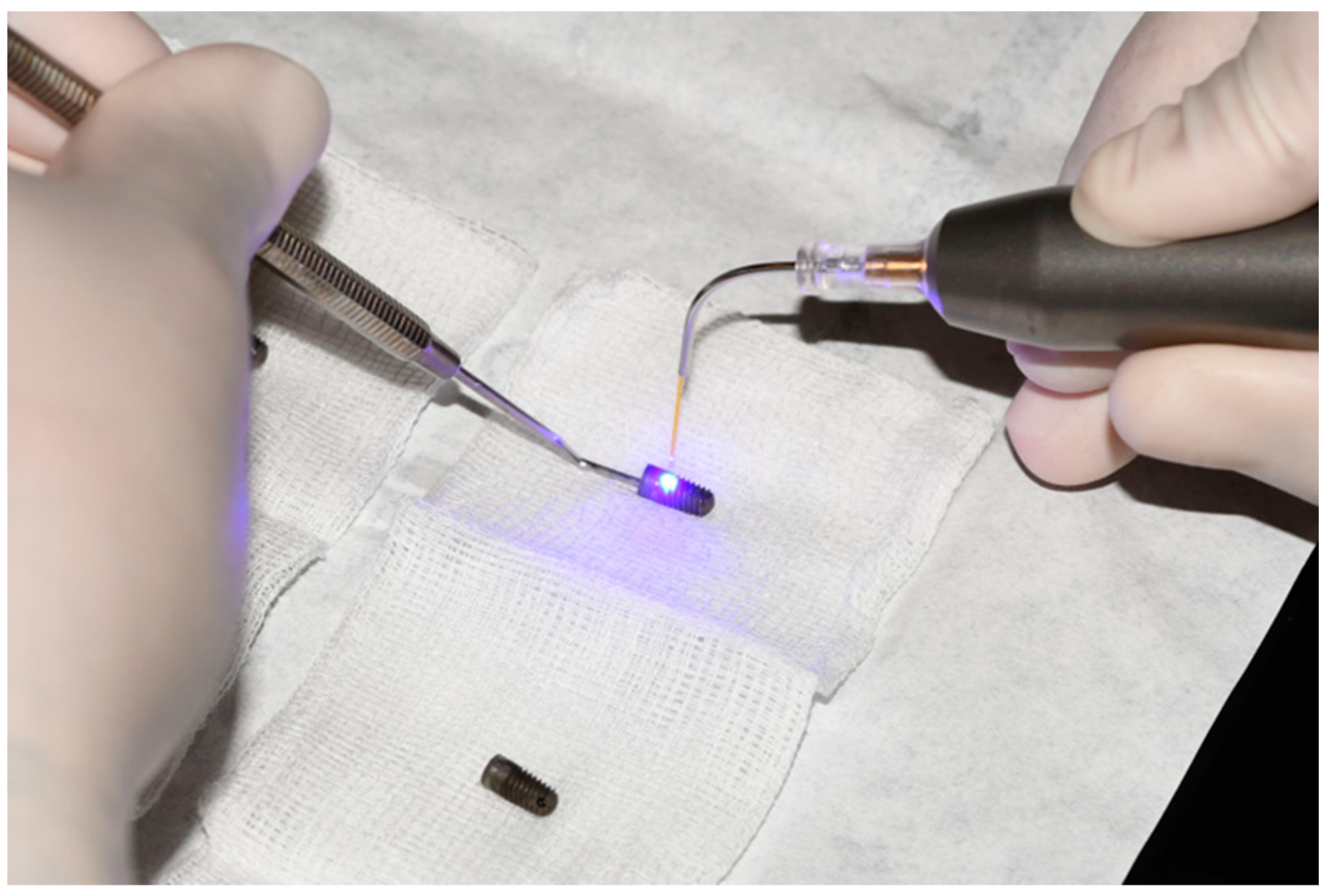
The fourth group (G4) underwent the same procedure as G3, with the following difference: 60 s after treatment with 3% hydrogen peroxide, the samples were illuminated with a SiroLaser Blue laser (Dentsply Sirona, Bensheim, Germany) with the following parameters: wavelength of 445 nm, power of 1 W, continuous beam (CW), 320 mm laser fiber tip and 60 s exposure time (Figure 2). The distance of the laser tip from the implant surface was approximately 1–2 mm, with a constant movement of 1 mm/s along the implant surface (freehand movement).
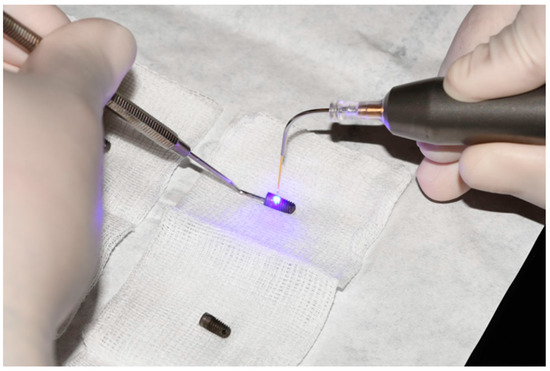
Figure 2.
Surface decontamination with SiroLaser Blue laser (Dentsply Sirona, Bensheim, Germany) after treatment with 3% hydrogen peroxide.
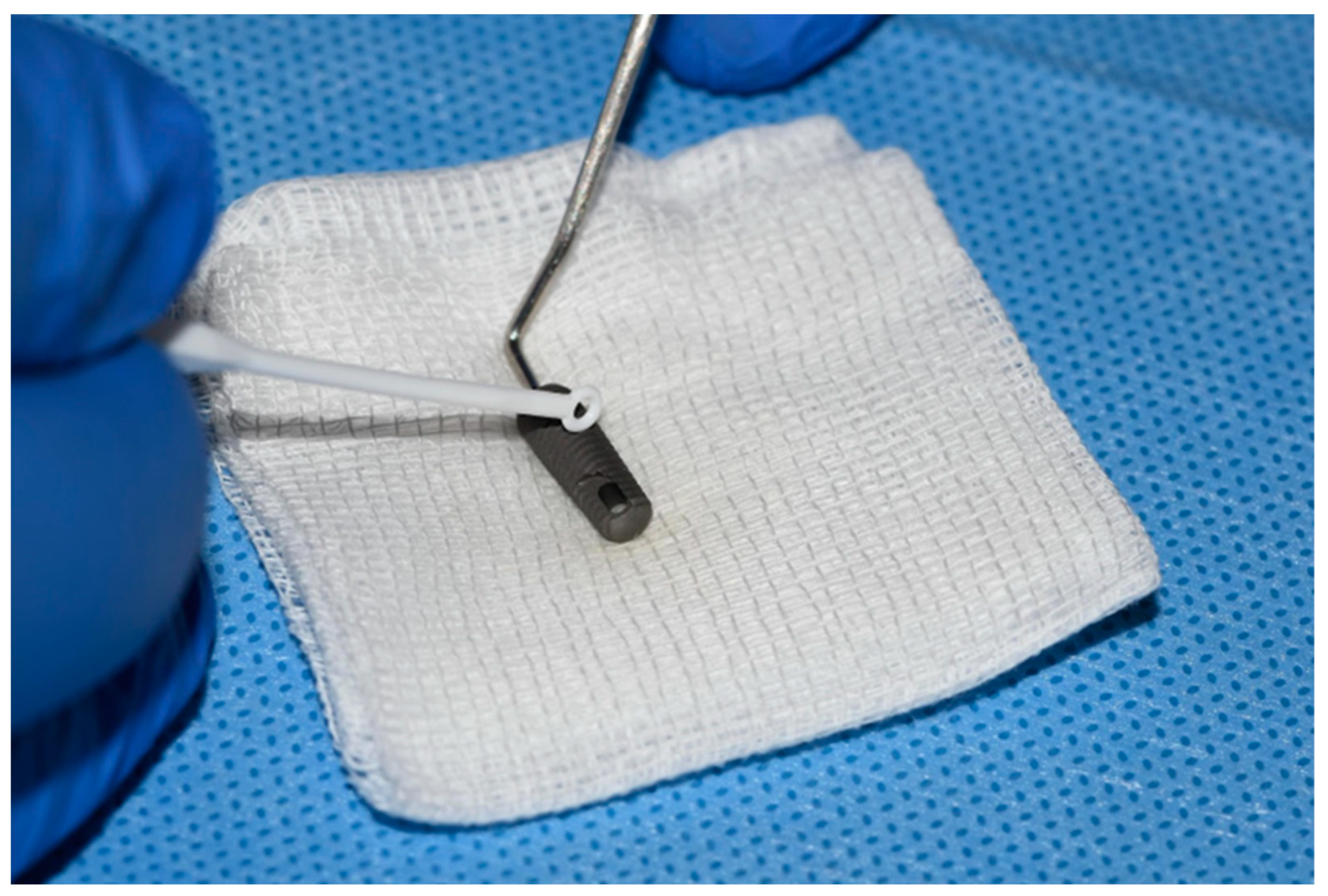
2.2. Collection of Samples
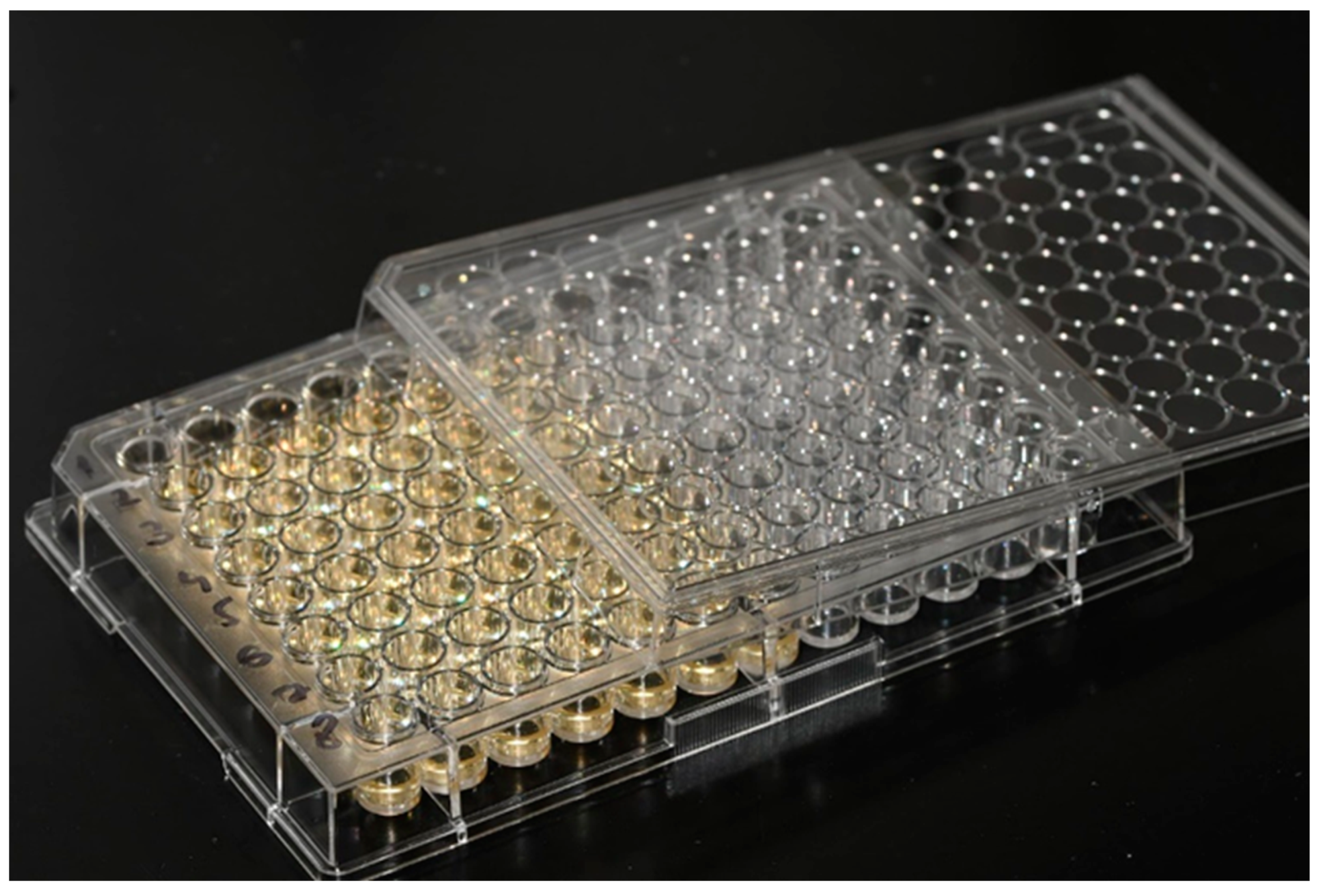
After the processing of the implants, the surface of each of them was scraped with the help of a sterile plastic inoculating loop in such a way, that the threads of the implants were scraped with it twice (Figure 3). Each sample was then placed in 250 µL of saline and vortexed on a vibro-mixer (Corning® LSETM vortex mixer, Corning, NY, USA) for 40 s to separate bacteria and fungi. Then, the loops were discarded, and the physiological solution into which the bacteria and fungi were scraped from the implant were transferred with to the blood agar, in a volume of 50 µL. Then, 100 µL of physiological solution, with suspended S. aureus and C. albicans, was transferred to the wells of a microtiter plate filled with 100 µL of brain–heart broth.

Figure 3.
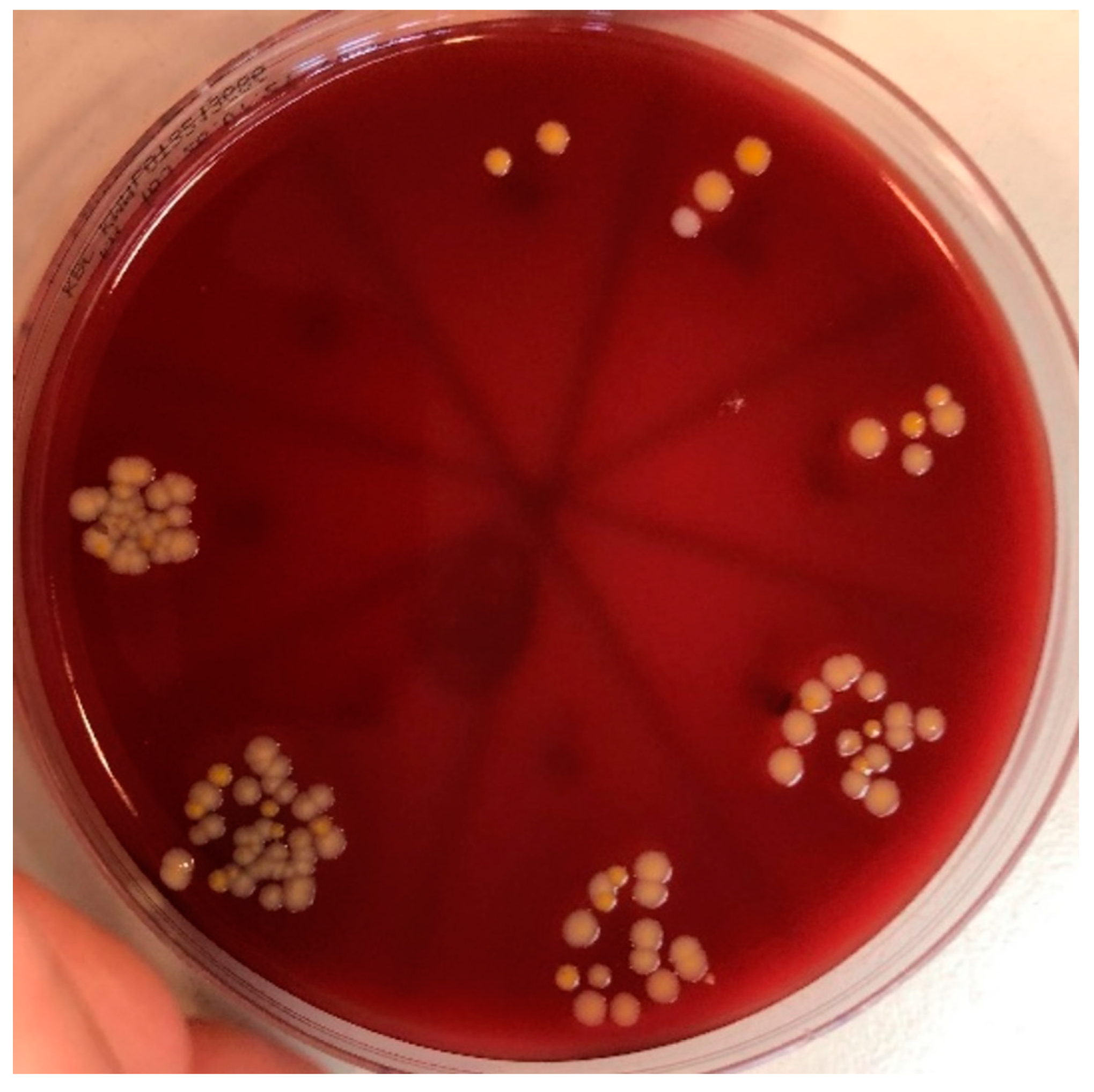
Implant surface sampling with sterile plastic inoculating loop. From the first well, which contains a total of 200 µL (100 µL suspension + 100 µL brain–heart broth), 100 µL was transferred to the next well, and so on, until a dilution of 10−7 was reached (Figure 4). From each well, 50 µL was inoculated onto blood agar. The plates were then incubated at 35 °C for 48 h. Then, the growth of microbial cultures was read in such a way, that the CFU of individual pathogens was counted, and the number was multiplied by the degree of the dilution (Figure 5).
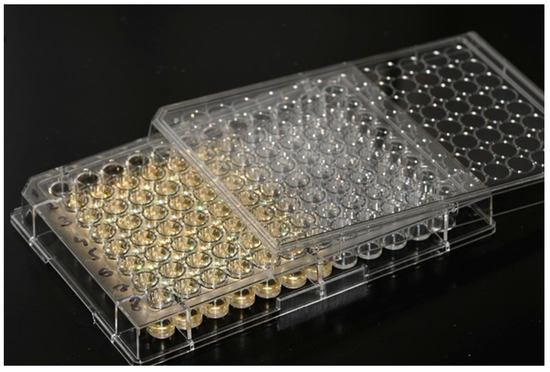
Figure 4.
Dilution of samples up to a concentration of 10−7.
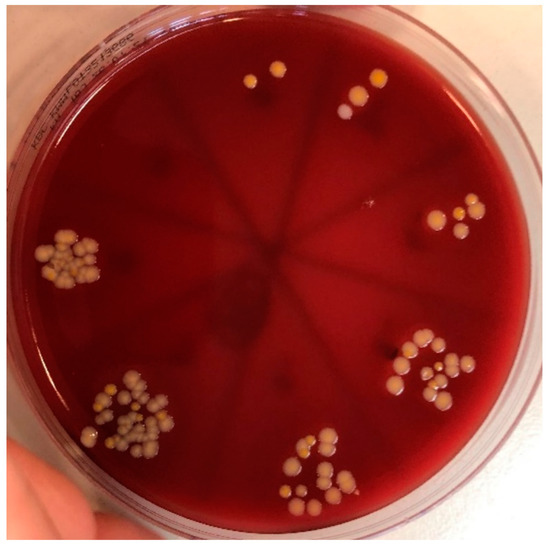
Figure 5.
The growth of microbial cultures, ready for CFU/mL counting.
Figure 3.
Implant surface sampling with sterile plastic inoculating loop. From the first well, which contains a total of 200 µL (100 µL suspension + 100 µL brain–heart broth), 100 µL was transferred to the next well, and so on, until a dilution of 10−7 was reached (Figure 4). From each well, 50 µL was inoculated onto blood agar. The plates were then incubated at 35 °C for 48 h. Then, the growth of microbial cultures was read in such a way, that the CFU of individual pathogens was counted, and the number was multiplied by the degree of the dilution (Figure 5).
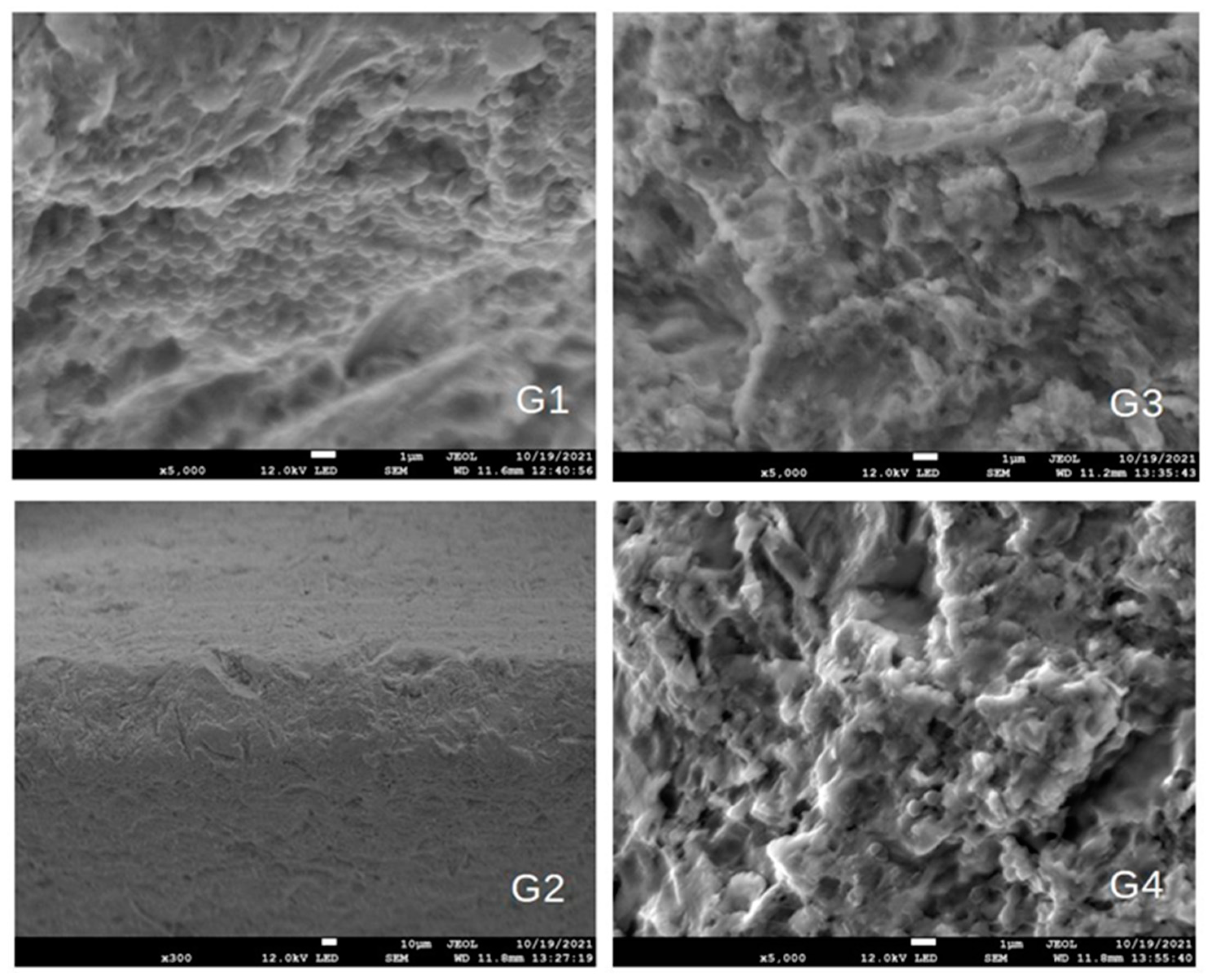
The formation of bacterial and fungal plaques was confirmed through an SEM device (JSM-7800 F Schottky Field Emission Scanning Electron Microscope, JEOL Ltd., Tokyo, Japan), as seen in Figure 6.
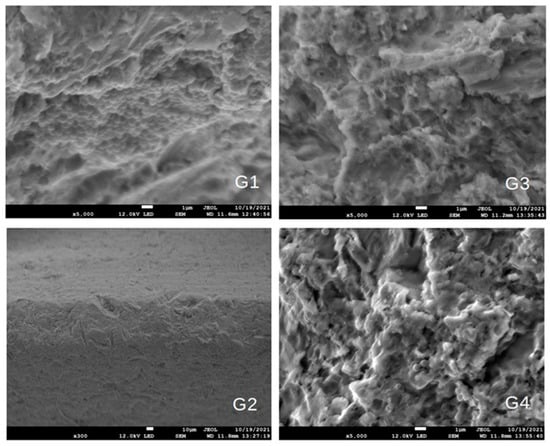
Figure 6.
SEM images of G1–G4. Microbial biofilms were visible on the surface of the implant in G1, while they were practically absent in the remaining images.
2.3. Statistical Analysis
Descriptive statistics of CFU/mL were performed for S. aureus and C. albicans, depending on the disinfection protocol implemented. Furthermore, a Kruskal–Wallis ANOVA by Ranks analysis was performed, especially for S. aureus and especially for C. albicans, to prove whether there was a difference between the studied groups. It was followed by post hoc multiple comparison p-values (2-tailed), in order to show where there is a statistically significant difference. Then, the protocol was compared individually by the Mann–Whitney U test with continuous correction. Statistical calculations were performed with the TIBCO Data Science Workbench (TIBCO Software, Inc., Palo Alto, CA, USA), software version 14.0.0.15.
3. Results
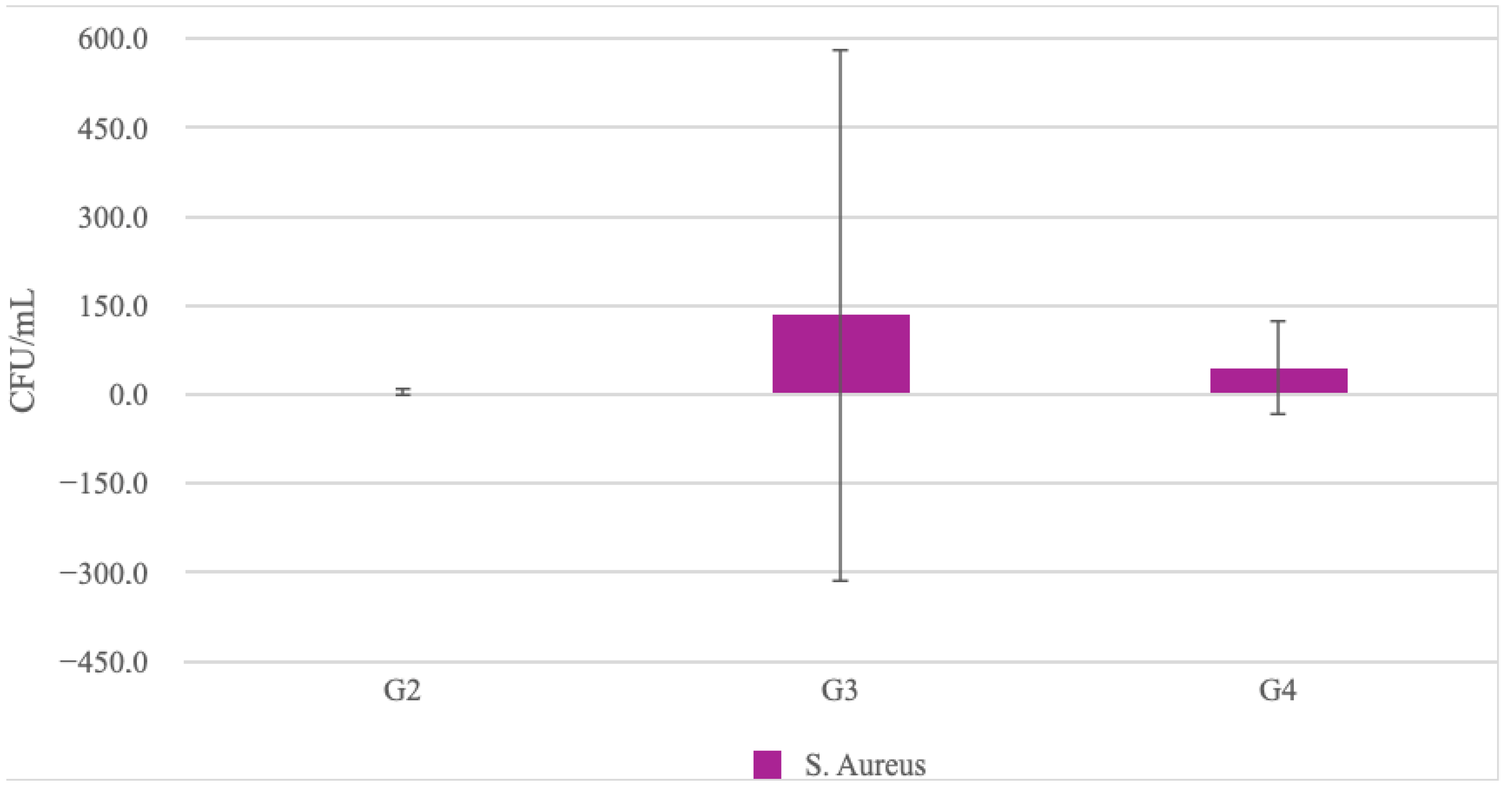
Descriptive statistics of CFU/mL for all protocols for S. aureus are shown in Table 1. In the negative control, the highest proportion of colonies per mL was present at 2.86 × 108, followed by the group disinfected with hydrogen peroxide (G3) with 134 CFU/mL, the group of laser-activated hydrogen peroxide (G4) with 45 CFU/mL, and the positive control (G2) with the smallest proportion of 4 CFU/mL. Differences between groups (Mann–Whitney U test) are shown in Table 2 and graphically in Figure 7.

Table 1.
Descriptive statistics of the amount of CFU/mL of S. aureus under different protocols.

Table 2.
Comparison of the success of individual protocols in the eradication of S. aureus: G1–negative control, G2–positive control, G3–hydrogen peroxide, and G4–laser-activated hydrogen peroxide.
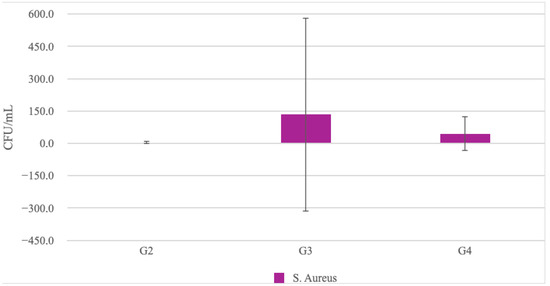
Figure 7.
Comparison of the success of individual protocols in the eradication of S. aureus: G2—positive control, G3—hydrogen peroxide, and G4—laser-activated hydrogen peroxide.
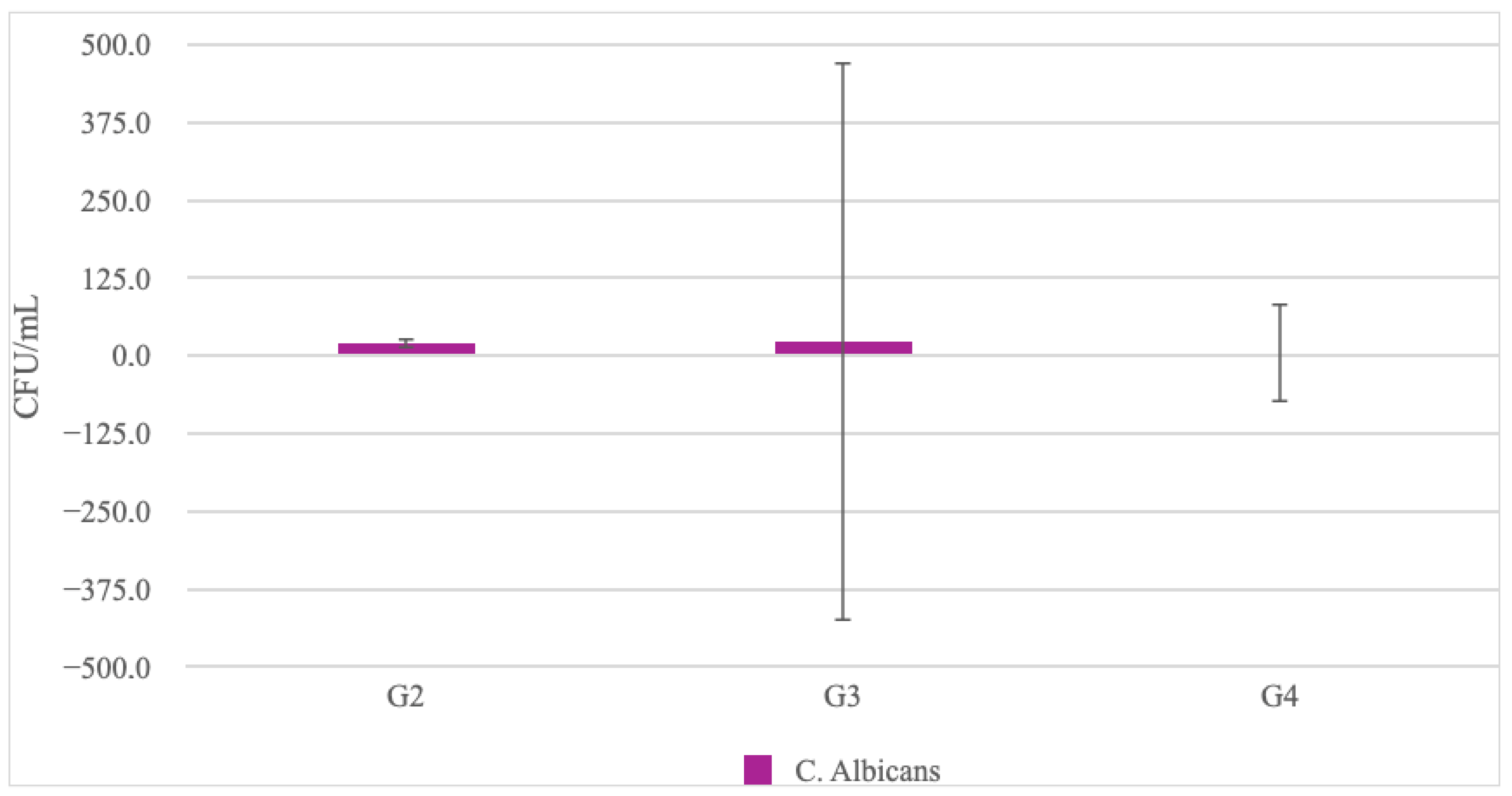
Descriptive statistics of CFU/mL for all protocols regarding C. albicans are shown in Table 3. In the negative control, the highest proportion of colonies per mL was present at 4.06 × 105, followed by the group disinfected with hydrogen peroxide (G3) with 24 CFU/mL, the positive control (G2) with 20 CFU/mL, and the laser-activated hydrogen peroxide group (G4) with the smallest proportion of 5 CFU/mL.

Table 3.
Descriptive statistics of CFU/mL of C. albicans under different protocols.
Furthermore, there was no statistically significant difference in C. albicans eradication between the individually tested protocols: positive control (G2), hydrogen peroxide (G3), and laser-activated hydrogen peroxide (G4) (Table 4 and Figure 8).

Table 4.
A performance comparison of different protocols in the reduction of the C. albicans CFU.
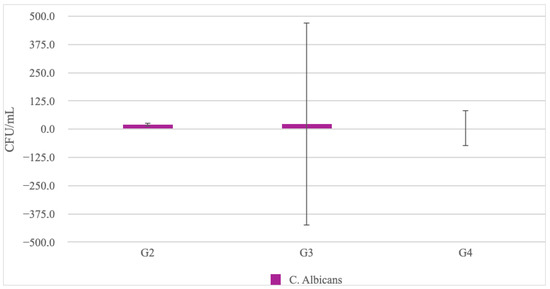
Figure 8.
Comparison of the success of individual protocols in the eradication of C. albicans: G2—positive control, G3—3% hydrogen peroxide, and G4—laser-activated 3% hydrogen peroxide.
4. Discussion
This research primarily examined the possibility of improving the antimicrobial efficiency of 3% H2O2 in peri-implantitis therapy, using diode laser activation with a wavelength of 445 nm, compared to non-activated H2O2 and the current gold standard of 0.2% CHX [23]. All tested groups showed a massive, significant reduction in microbial CFU count when compared to the negative control. As for the hypothesis, the first hypothesis was only partially accepted. Although the laser-activated group clearly showed better results in the microbial CFU count, there was no statistically significant difference after the statistical analysis, likely due to the sample size. The second hypothesis was accepted, since the analysis revealed comparable results between CHX and H2O2 groups. H2O2 is one of the disinfectants used in dental medicine. Oxygen radicals (ROS) generated by the application of H2O2 have a high affinity for bacteria and the extracellular matrix of bacteria, and a strong oxidizing effect. Additionally, they ensure the creation of active oxygen foam that also has mechanical cleaning properties. ROS (hydroxyl radicals) can theoretically damage healthy tissue cells, but ROS generated by the application of 3% H2O2 have a rapid breakdown into water and oxygen molecules [24]. Also, the incidence of ROS, which occurs with photoactivation of 3% H2O2, was examined, and it was shown that the formation of ROS stops when the photoactivation with the laser device stops [25]. In the research of Wiedmer et al. [26], a comparison of the effects of CHX and H2O2 on the biofilm mass on the implant surface was shown. It has been proven that H2O2 has a strong effect on actively removing the mass of biofilm, while CHX has a slightly weaker effect on reducing the said mass, but it certainly has a bactericidal effect on the microbial community and prevents the regrowth of bacteria. The current study showed a roughly equal effectiveness of CHX and H2O2 in eradicating S. aureus and C. albicans. This study was conducted on the surface of real dental implants rather than titanium discs, in order to simulate in vivo conditions and obtain more realistic results [27,28]. C. albicans and S. aureus cultures were chosen for research due to the simple cultivation, control of the microorganisms themselves, and also due to the fact that they create polymicrobial biofilms (“early colonizers”) and actively participate in peri-implant infections [13,29].
Diode lasers belong to the newer group of techniques combating the causative agent of periodontitis [30]. They demonstrate a disinfection effectiveness in two main ways: through photothermal and/or photodynamic therapy. The effectiveness of photothermal therapy is based on the thermal energy generated by the laser during radiation emission. The generated thermal energy transfers indirectly through the environment or directly on the bacterial cell, acting fatally on it [31]. Regarding the energy levels of lasers, proper energy dosage is crucial: too little energy will not be sufficient to eradicate enough microorganisms and too much energy could cause damage to the neighboring tissues [32]. Usual antimicrobial energy levels in peri-implant decontamination studies range from 0.5 to 3 W in continuous (CW) or pulsed-mode (energy emission types) [32,33,34,35,36,37]. Photodynamic therapy with diode lasers is based on the light activation of the photosensitive agent in presence of oxygen with a low-energy (sub-ablative) laser beam. There is no heating, and thus no risk of damage to the surrounding tissues [38]. The principles of photodynamic therapy are: photosensitive molecules (the dye) bind to target microorganisms on the implant surface, which is then irradiated with a light of a certain wavelength in the presence of oxygen. Light-excited photosensitizers undergo type I (electron transfer) and/or type II (energy transfer) reactions to produce reactive oxygen species (ROS), resulting in the disruption of the bacterial cell wall and/or normal metabolism, leading to bacterial cell damage or death [38,39]. The described mechanisms do not harm human cells, as these cells have mechanisms to survive oxidative stress (catalase and superoxide dismutase enzymes).
The development of microbial resistance to PDT is not probable, as the bactericidal effect is achieved through the action of oxygen radicals on the cellular components of the micro-organisms [38].
In the current research, a new diode laser, with a wavelength of 445 nm, was used to test the possibility of activating 3% H2O2. H2O2 exhibits maximum absorption at wavelengths of approximately 400 nm. The idea was to try to activate H2O2 photodynamically, and also photothermally (by heating) at the same time; therefore, the energy settings were set to 1 W CW for 60 s, with constant movement of the laser optical fiber (1 mm/s) along the surface of the implant, from a distance of approximately 2 mm. The thermal effect of these settings was not measured, although the settings, combined with the constant displacement/freehand movement of the laser fiber tip in a wet environment (movement prevents excessive heat accumulation on one place and allows cooling microbreaks), could be considered as relatively safe and were therefore chosen for research [32,33,34,35,36]. Nevertheless, additional testing should be done regarding the temperature rise in the specific protocol and its effects on the surrounding tissue.
Chemical reactions in the activated H2O2 environment were not assessed. Potential activation/antimicrobial augmentation was assessed only via the CFU count, which is a more basic, simpler approach. Complex chemical analysis should be done in future similar studies to closer analyze the interaction of this specific laser wavelength and H2O2.
The specified wavelength of the diode laser was first examined in the concrete disinfection protocol by Katalinic et al. [40], however not in peri-implant conditions, but on endodontic intracanal biofilms composed of E. faecalis, C. albicans, and S. aureus, where promising results were obtained. The same laser was then tested in peri-implantitis therapy, but as part of photodynamic therapy with 0.1% riboflavin, where a positive antimicrobial effect was also demonstrated [41]. By reviewing the literature available to the authors, it is not possible to find research similar to the current one. However, research examining the impact of laser energy on H2O2 and various pathogens exists. In the study by Ikai et al. [42], the authors analyzed the effect of activated hydrogen peroxide on cultures of S. mutans, A. actinomycetemcomitans, E. faecalis, and S. aureus. It has been proven that hydrogen peroxide, activated by a laser with a wavelength of 405 nm, has the ability to eliminate all four pathogens within 3 min, which is not the case when using lasers or H2O2 as independent treatments. Photoactivation of H2O2, with the aim of improving the antimicrobial effect, was also examined in the work of Mahdi et al. in 2015 [21]. The authors proved a stronger disinfection potential when H2O2 was activated by LED light with a wavelength of 440–480 nm, compared to non-activated H2O2. In contrast to the current work, the photoactivation was performed with LED light and not with a diode laser that has monochromatic, coherent, and collimated light radiation. In two scientific papers, Odor et al. [43,44] investigated the antimicrobial effect of hydroxyl radicals produced by diode laser photoactivation, in combination with conventional mechanical periodontitis therapy. A diode laser with a wavelength of 940 nm and a power of 1 W was used. The laser-activated H2O2 group showed the best results. In relation to the other research mentioned, that research was not done in vitro, but in vivo, on patients with periodontitis, and the effect on bacterial cultures was examined differently from that in the current research.
From all presented studies, it is possible to conclude that laser activation of H2O2 has a strong, positive and potentially clinically relevant antimicrobial effect, but the results cannot be directly compared with the current study due to too many differences in the design of the study (microorganisms tested, energy settings of the laser, different wavelengths, different presentation of the obtained data, etc.). Additional research is needed to determine the exact impact of 445 nm laser energy on H2O2 and most efficient laser energy settings, leading to a safe and useful clinical decontamination protocol.
5. Conclusions
The conducted research provides a preliminary insight into the protocol for treating the surface of dental implants with a combination of agents that have not been described in the literature so far. Statistical analysis revealed a significant difference between all three disinfection protocols compared to the negative control. However, in the mutual comparison of the results of the three disinfection protocols, there were no statistically significant results, although the laser-activated H2O2 group showed better antimicrobial results compared to non-activated 3% H2O2. Within the inherent limitations of this study, it is possible to conclude that all three disinfection protocols are equally powerful in the treatment of S.aureus and C.albicans biofilms. For further evaluation of efficiency, new research is needed on a larger number of implants, testing more energy settings, thermal effects of the settings and, certainly, in-clinical, “in vivo” set-ups.
Author Contributions
Formal analysis, I.K., I.S., L.M. and A.B.; writing—original draft preparation, I.K., writing—review and editing, D.G. and M.V. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Tarnow, D.P. Commentary: Replacing Missing Teeth With Dental Implants: A Century of Progress. J. Periodontol. 2014, 85, 1475–1477. [Google Scholar] [CrossRef] [PubMed]
- Buser, D.; Sennerby, L.; De Bruyn, H. Modern implant dentistry based on osseointegration: 50 years of progress, current trends and open questions. Periodontology 2000 2017, 73, 7–21. [Google Scholar] [CrossRef]
- Albrektsson, T.; Donos, N. Implant survival and complications. The Third EAO consensus conference 2012. Clin. Oral Implant. Res. 2012, 23, 63–65. [Google Scholar] [CrossRef]
- Srinivasan, M.; Vazquez, L.; Rieder, P.; Moraguez, O.; Bernard, J.-P.; Belser, U.C. Survival rates of short (6 mm) micro-rough surface implants: A review of literature and meta-analysis. Clin. Oral Implant. Res. 2014, 25, 539–545. [Google Scholar] [CrossRef]
- Smeets, R.; Henningsen, A.; Jung, O.; Heiland, M.; Hammächer, C.; Stein, J.M. Definition, etiology, prevention and treatment of pe-ri-implantitis—A review. Head Face Med. 2014, 10, 34. [Google Scholar] [CrossRef]
- Atieh, M.A.; Alsabeeha, N.H.; Faggion, C.M., Jr.; Duncan, W.J. The frequency of peri-implant diseases: A systematic review and me-ta-analysis. J Periodontol. 2013, 84, 1586–1598. [Google Scholar] [CrossRef]
- Rams, T.E.; Degener, J.E.; Van Winkelhoff, A.J. Antibiotic resistance in human peri-implantitis microbiota. Clin. Oral Implant. Res. 2014, 25, 82–90. [Google Scholar] [CrossRef]
- Salvi, G.E.; Fürst, M.M.; Lang, N.P.; Persson, G.R. One-year bacterial colonization patterns of Staphylococcus aureus and other bacteria at implants and adjacent teeth. Clin. Oral Implant. Res. 2008, 19, 242–248. [Google Scholar] [CrossRef]
- Negrini, T.C.; Koo, H.; Arthur, R.A. Candida-Bacterial Biofilms and Host-Microbe Interactions in Oral Diseases. Adv. Exp. Med. Biol. 2019, 1197, 119–141. [Google Scholar]
- Otto, M. Staphylococcal biofilms. In Gram-Positive Pathogens, 3rd ed.; Fischetti, V.A., Novick, R.P., Eds.; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2019; pp. 699–711. [Google Scholar]
- Harriott, M.M.; Noverr, M.C. Importance of Candida–bacterial polymicrobial biofilms in disease. Trends Microbiol. 2011, 19, 557–563. [Google Scholar] [CrossRef]
- De-La-Torre, J.; Quindós, G.; Marcos-Arias, C.; Marichalar-Mendia, X.; Gainza, M.L.; Eraso, E.; Acha-Sagredo, A.; Aguirre-Urizar, J.M. Oral Candida colonization in patients with chronic periodontitis. Is there any relationship? Rev. Iberoam. Micol. 2018, 35, 134–139. [Google Scholar] [CrossRef]
- Rokaya, D.; Srimaneepong, V.; Wisitrasameewon, W.; Humagain, M.; Thunyakitpisal, P. Peri-implantitis Update: Risk Indicators, Diagnosis, and Treatment. Eur. J. Dent. 2020, 14, 672–682. [Google Scholar] [CrossRef]
- Scarano, A.; Nardi, G.; Murmura, G.; Rapani, M.; Mortellaro, C. Evaluation of the Removal Bacteria on Failed Titanium Implants After Irradiation With Erbium-Doped Yttrium Aluminium Garnet Laser. J. Craniofacial Surg. 2016, 27, 1202–1204. [Google Scholar] [CrossRef]
- Memè, L.; Sartini, D.; Pozzi, V.; Emanuelli, M.; Strappa, E.M.; Bittarello, P.; Bambini, F.; Gallusi, G. Epithelial Biological Response to Machined Titanium vs. PVD Zirconium-Coated Titanium: An In Vitro Study. Materials 2022, 15, 7250. [Google Scholar] [CrossRef]
- Alovisi, M.; Carossa, M.; Mandras, N.; Roana, J.; Costalonga, M.; Cavallo, L.; Pira, E.; Putzu, M.G.; Bosio, D.; Roato, I.; et al. Disinfection and Biocompatibility of Titanium Surfaces Treated with Glycine Powder Airflow and Triple Antibiotic Mixture: An In Vitro Study. Materials 2022, 15, 4850. [Google Scholar] [CrossRef]
- Al-Hashedi, A.A.; Laurenti, M.; Benhamou, V.; Tamimi, F. Decontamination of titanium implants using physical methods. Clin. Oral Implant. Res. 2017, 28, 1013–1021. [Google Scholar] [CrossRef]
- Louropoulou, A.; Slot, D.E.; Van Der Weijden, F.A. Titanium surface alterations following the use of different mechanical instruments: A systematic review. Clin. Oral Implant. Res. 2012, 23, 643–658. [Google Scholar] [CrossRef]
- De Araújo Nobre, M.; Capelas, C.; Alves, A.; Almeida, T.; Carvalho, R.; Antunes, E.; Oliveira, D.; Cardador, A.; Maló, P. Non-surgical treatment of peri-implant pathology. Int. J. Dent. Hyg. 2006, 4, 84–90. [Google Scholar] [CrossRef]
- Marshall, M.V.; Cancro, L.P.; Fischman, S.L. Hydrogen Peroxide: A Review of Its Use in Dentistry. J. Periodontol. 1995, 66, 786–796. [Google Scholar] [CrossRef]
- Mahdi, Z.; Habiboallh, G.; Mahbobeh, N.N.; Mina, Z.J.; Majid, Z.; Nooshin, A. Lethal effect of blue light-activated hydrogen peroxide, curcumin and erythrosine as potential oral photosensitizers on the viability of Porphyromonas gingivalis and Fusobacterium nucleatum. Laser Ther. 2015, 24, 103–111. [Google Scholar] [CrossRef]
- Ehrenfest, D.M.D.; Del Corso, M.; Kang, B.S.; Leclercq, P. Identification card and codification of the chemical and morphological characteristics of 62 dental implant surfaces. Part 3: Sand-blasted/acid-etched (SLA type) and related surfaces (Group 2A, main subtractive process). Poseido 2014, 2, 37–55. [Google Scholar]
- Heitz-Mayfield, L.J.; Mombelli, A. The Therapy of Peri-implantitis: A Systematic Review. Int. J. Oral Maxillofac. Implant. 2014, 29, 325–345. [Google Scholar] [CrossRef] [PubMed]
- Chapple, I.L.C.; Matthews, J.B. The role of reactive oxygen and antioxidant species in periodontal tissue destruction. Periodontology 2000 2007, 43, 160–232. [Google Scholar] [CrossRef] [PubMed]
- Jaimes, E.A.; Sweeney, C.; Raij, L. Effects of the Reactive Oxygen Species Hydrogen Peroxide and Hypochlorite on Endothelial Nitric Oxide Production. Hypertension 2001, 38, 877–883. [Google Scholar] [CrossRef]
- Wiedmer, D.; Petersen, F.C.; Lönn-Stensrud, J.; Tiainen, H. Antibacterial effect of hydrogen peroxide-titanium dioxide suspensions in the decontamination of rough titanium surfaces. Biofouling 2017, 33, 451–459. [Google Scholar] [CrossRef]
- Teughels, W.; Van Assche, N.; Sliepen, I.; Quirynen, M. Effect of material characteristics and/or surface topography on biofilm development. Clin. Oral Implants Res. 2006, 17, 68–81. [Google Scholar] [CrossRef] [PubMed]
- Gustumhaugen, E.; Lönn-Stensrud, J.; Scheie, A.A.; Lyngstadaas, S.P.; Ekfeldt, A.; Taxt-Lamolle, S. Effect of chemical and mechanical debridement techniques on bacterial re-growth on rough titanium surfaces: An in vitro study. Clin. Oral Implants Res. 2014, 25, 707–713. [Google Scholar] [CrossRef]
- Charalampakis, G.; Belibasakis, G.N. Microbiome of peri-implant infections: Lessons from conventional, molecular and metagenomic analyses. Virulence 2015, 6, 183–187. [Google Scholar] [CrossRef] [PubMed]
- Marotti, J.; Tortamano, P.; Cai, S.; Ribeiro, M.S.; Franco, J.E.M.; De Campos, T.T. Decontamination of dental implant surfaces by means of photodynamic therapy. Lasers Med. Sci. 2013, 28, 303–309. [Google Scholar] [CrossRef]
- Olivi, G.; De Moor, R.; DiVito, E. Lasers in Endodontics: Scientific Background and Clinical Application, 1st ed.; Springer International Publishing: Cham, Switzerland; Heidelberg, Germany; New York, NY, USA; Dordrecht, The Netherlands; London, UK, 2016. [Google Scholar]
- Deppe, H.; Ahrens, M.; Behr, A.V.; Marr, C.; Sculean, A.; Mela, P.; Ritschl, L.M. Thermal effect of a 445 nm diode laser on five dental implant systems: An in vitro study. Sci. Rep. 2021, 11, 20174. [Google Scholar] [CrossRef] [PubMed]
- Malmqvist, S.; Liljeborg, A.; Qadri, T.; Johannsen, G.; Johannsen, A. Using 445 nm and 970 nm Lasers on Dental Implants—An In Vitro Study on Change in Temperature and Surface Alterations. Materials 2019, 12, 3934. [Google Scholar] [CrossRef] [PubMed]
- Valente, N.A.; Calascibetta, A.; Patianna, G.; Mang, T.; Hatton, M.; Andreana, S. Thermodynamic Effects of 3 Different Diode Lasers on an Implant-Bone Interface: An Ex-Vivo Study With Review of the Literature. J. Oral Implantol. 2017, 43, 94–99. [Google Scholar] [CrossRef] [PubMed]
- Matys, J.; Flieger, R.; Dominiak, M. Effect of diode lasers with wavelength of 445 and 980 nm on a temperature rise when un-covering implants for second stage surgery: An ex-vivo study in pigs. Adv. Clin. Exp. Med. 2017, 26, 687–693. [Google Scholar] [CrossRef]
- Geminiani, A.; Caton, J.G.; Romanos, G.E. Temperature change during non-contact diode laser irradiation of implant surfaces. Lasers Med. Sci. 2012, 27, 339–342. [Google Scholar] [CrossRef]
- Romanos, G.E. Diode laser soft-tissue surgery: Advancements aimed at consistent cutting, improved clinical outcomes. Compend. Contin. Educ. Dent. 2013, 34, 752–758. [Google Scholar] [PubMed]
- Cieplik, F.; Deng, D.; Crielaard, W.; Buchalla, W.; Hellwig, E.; Al-Ahmad, A.; Maisch, T. Antimicrobial photodynamic therapy. What we know and what we dont. Crit. Rev. Microbiol. 2018, 44, 571–589. [Google Scholar] [CrossRef] [PubMed]
- Kwiatkowski, S.; Knap, B.; Przystupski, D.; Saczko, J.; Kędzierska, E.; Knap-Czop, K.; Kotlińska, J.; Michel, O.; Kotowski, K.; Kulbacka, J. Photodynamic therapy—Mechanisms, photosensitizers and combinations. Biomed Pharmacother. 2018, 106, 1098–1107. [Google Scholar] [CrossRef]
- Katalinić, I.; Budimir, A.; Bošnjak, Z.; Jakovljević, S.; Anić, I. The photo-activated and photo-thermal effect of the 445/970 nm diode laser on the mixed biofilm inside root canals of human teeth in vitro: A pilot study. Photodiagnosis Photodyn. Ther. 2019, 26, 277–283. [Google Scholar] [CrossRef]
- Morelato, L.; Budimir, A.; Smojver, I.; Katalinić, I.; Vuletić, M.; Ajanović, M.; Gabrić, D. A Novel Technique for Disinfection Treatment of Contaminated Dental Implant Surface Using 0.1% Riboflavin and 445 nm Diode Laser-An In Vitro Study. Bioengineering 2022, 9, 308. [Google Scholar] [CrossRef]
- Ikai, H.; Nakamura, K.; Shirato, M.; Kanno, T.; Iwasawa, A.; Sasaki, K.; Niwano, Y.; Kohno, M. Photolysis of Hydrogen Peroxide, an Effective Disinfection System via Hydroxyl Radical Formation. Antimicrob. Agents Chemother. 2010, 54, 5086–5091. [Google Scholar] [CrossRef]
- Odor, A.A.; Bechir, E.S.; Forna, D.A. Effect of Hydrogen Peroxide Photoactivated Decontamination Using 940 nm Diode Laser in Periodontal Treatment: A Pilot Study. Photobiomodulation Photomed. Laser Surg. 2020, 38, 614–624. [Google Scholar] [CrossRef] [PubMed]
- Odor, A.A.; Bechir, E.S.; Violant, D.; Badea, V. Antimicrobial Effect of 940 nm Diode Laser based on Photolysis of Hydrogen Peroxide in the Treatment of Periodontal Disease. Rev. Chim. 2018, 69, 2081–2088. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).