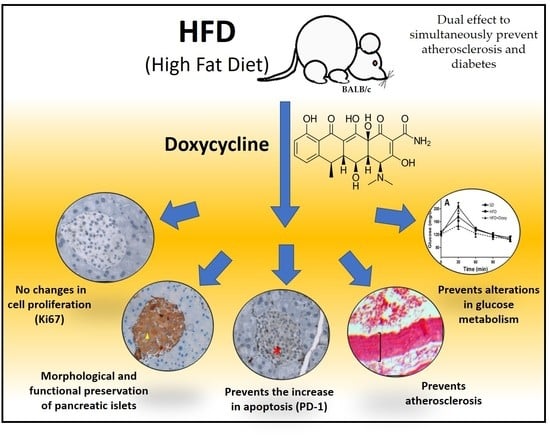
Doxycycline Prevents Preclinical Atherosclerosis, Pancreatic Islet Loss and Improves Insulin Secretion after Glycemic Stimulation: Preclinical Study in Individuals with a High-Fat Diet
Abstract
1. Introduction
2. Materials and Methods
2.1. Reactive and Animals Treatment
2.2. Histopathological Analysis
2.3. The Body and Liver Weight, and Epididymal Fat Pads
2.4. Glucose Tolerance Curve
2.5. Biochemical Analyses
2.6. Statistical Analyses
3. Results
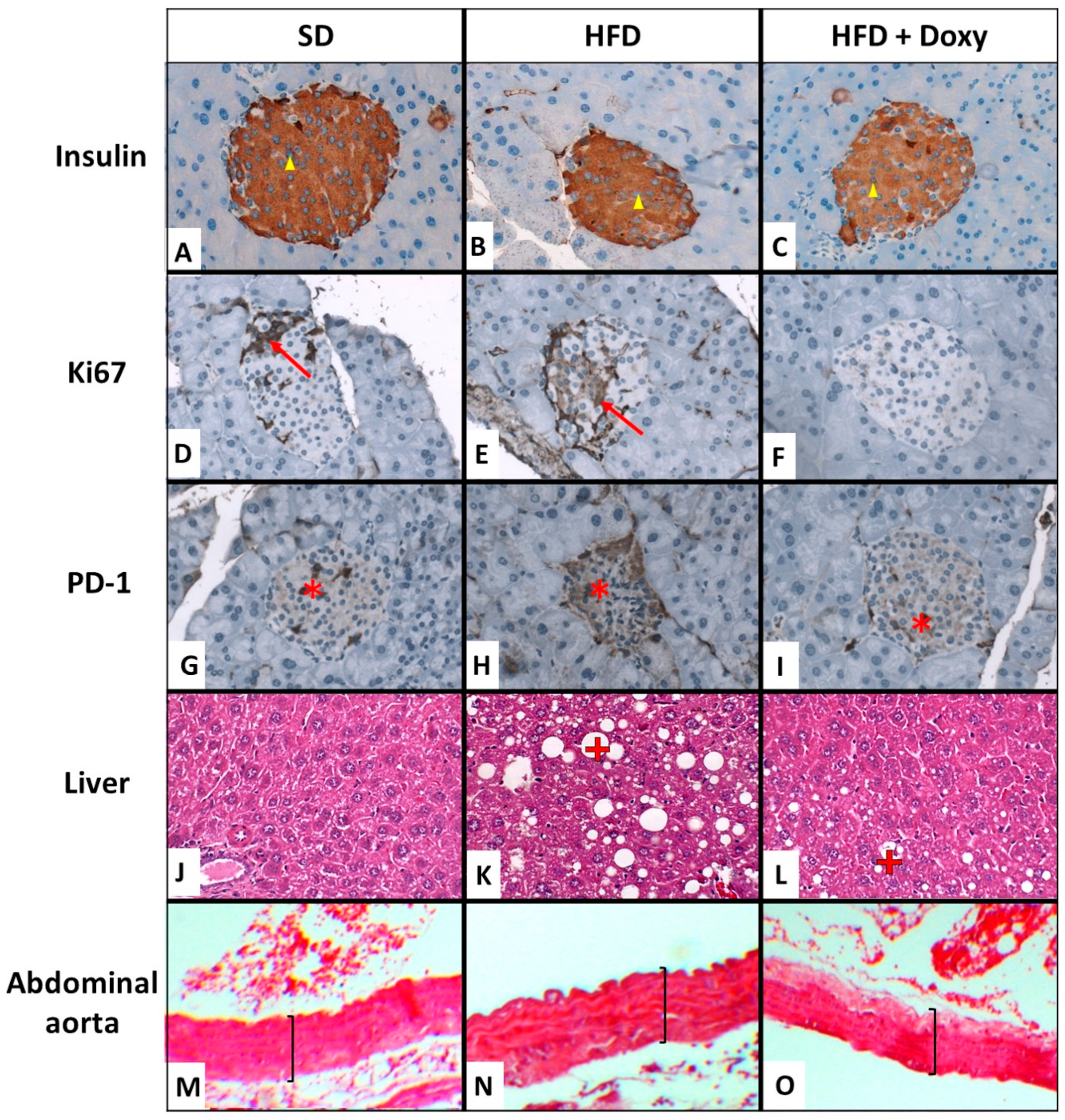
3.1. Biochemical and Histopathological Analysis
3.2. Pancreatic Morphology
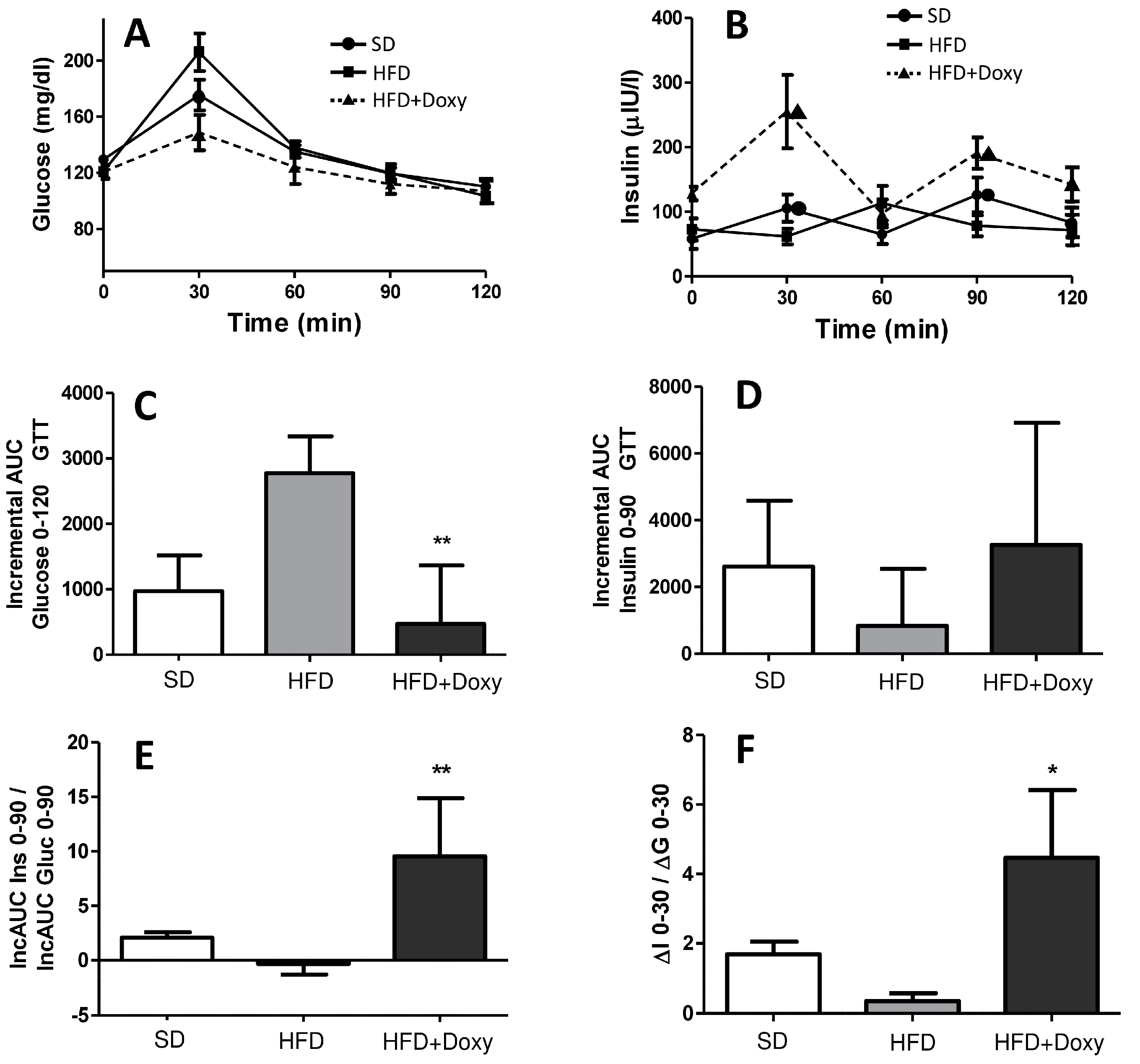
3.3. Glucose Metabolism
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Genuth, S.M.; Palmer, J.P.; Nathan, D.M. Classification and Diagnosis of Diabetes. In Diabetes in America; Cowie, C.C., Casagrande, S.S., Menke, A., Cissell, M.A., Eberhardt, M.S., Meigs, J.B., Gregg, E.W., Knowler, W.C., Barrett-Connor, E., Becker, D.J., et al., Eds.; National Institute of Diabetes and Digestive and Kidney Diseases (US): Bethesda, MD, USA, 2018. [Google Scholar]
- Primavera, M.; Giannini, C.; Chiarelli, F. Prediction and Prevention of Type 1 Diabetes. Front. Endocrinol. 2020, 11, 248. [Google Scholar] [CrossRef] [PubMed]
- Vardanyan, R.S.; Hruby, V.J. Antibiotics. In Synthesis of Essential Drugs; Elsevier: Amsterdam, The Netherlands, 2006; pp. 425–498. [Google Scholar]
- Grossi, S.G.; Genco, R.J. Periodontal Disease and Diabetes Mellitus: A Two-Way Relationship. Ann. Periodontol. 1998, 3, 51–61. [Google Scholar] [CrossRef] [PubMed]
- Basaria, S.; Braga, M.; Moore, W.T. Doxycycline-Induced Hypoglycemia in a Nondiabetic Young Man. South. Med. J. 2002, 95, 1353–1354. [Google Scholar] [CrossRef] [PubMed]
- Brugman, S.; Klatter, F.A.; Visser, J.T.J.; Wildeboer-Veloo, A.C.M.; Harmsen, H.J.M.; Rozing, J.; Bos, N.A. Antibiotic Treatment Partially Protects against Type 1 Diabetes in the Bio-Breeding Diabetes-Prone Rat. Is the Gut Flora Involved in the Development of Type 1 Diabetes? Diabetologia 2006, 49, 2105–2108. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, R.F.; Neu, J.; Schatz, D.; Atkinson, M.A.; Wasserfall, C. Comment on: Brugman S et al. (2006) Antibiotic Treatment Partially Protects against Type 1 Diabetes in the Bio-Breeding Diabetes-Prone Rat. Is the Gut Flora Involved in the Development of Type 1 Diabetes? Diabetologia 2007, 50, 220–221. [Google Scholar] [CrossRef] [PubMed]
- Wang, N.; Tian, X.; Chen, Y.; Tan, H.Q.; Xie, P.J.; Chen, S.J.; Fu, Y.C.; Chen, Y.X.; Xu, W.C.; Wei, C.J. Low Dose Doxycycline Decreases Systemic Inflammation and Improves Glycemic Control, Lipid Profiles, and Islet Morphology and Function in Db/Db Mice. Sci. Rep. 2017, 7, 14707. [Google Scholar] [CrossRef]
- Wang, B.; Chandrasekera, P.C.; Pippin, J.J. Leptin- and Leptin Receptor-Deficient Rodent Models: Relevance for Human Type 2 Diabetes. Curr. Diabetes Rev. 2014, 10, 131–145. [Google Scholar] [CrossRef]
- Sasso, F.C.; Simeon, V.; Galiero, R.; Caturano, A.; De Nicola, L.; Chiodini, P.; Rinaldi, L.; Salvatore, T.; Lettieri, M.; Nevola, R.; et al. The Number of Risk Factors Not at Target Is Associated with Cardiovascular Risk in a Type 2 Diabetic Population with Albuminuria in Primary Cardiovascular Prevention. Post-Hoc Analysis of the NID-2 Trial. Cardiovasc. Diabetol. 2022, 21, 235. [Google Scholar] [CrossRef]
- VanSaun, M.N.; Lee, I.K.; Washington, M.K.; Matrisian, L.; Gorden, D.L. High Fat Diet Induced Hepatic Steatosis Establishes a Permissive Microenvironment for Colorectal Metastases and Promotes Primary Dysplasia in a Murine Model. Am. J. Pathol. 2009, 175, 355–364. [Google Scholar] [CrossRef]
- Getz, G.S.; Reardon, C.A. Diet and Murine Atherosclerosis. ATVB 2006, 26, 242–249. [Google Scholar] [CrossRef]
- Garcìa-Rivera, A.; Madrigal-Perez, V.M.; Rodriguez-Hernandez, A.; Martinez-Martinez, R.; Martinez-Fierro, M.L.; Soriano-Hernandez, A.D.; Galvan-Salazar, H.R.; Gonzalez-Aivarez, R.; Valdez-Yelazquez, L.L.; Espinoza-Gómez, F.; et al. A Simple and Low-Cost Experimental Mouse Model for the Simultaneous Study of Steatohepatitis and Preclinical Atherosclerosis. Asian J. Anim. Vet. Adv. 2014, 9, 202–210. [Google Scholar] [CrossRef]
- Pawlowska, M.; Gajda, M.; Pyka-Fosciak, G.; Toton-Zuranska, J.; Niepsuj, A.; Kus, K.; Bujak-Gizycka, B.; Suski, M.; Olszanecki, R.; Jawien, J.; et al. The Effect of Doxycycline on Atherogenesis in ApoE-Knockout Mice. J. Physiol. Pharmacol. Off. J. Pol. Physiol. Soc. 2011, 62, 247–250. [Google Scholar]
- Madan, M.; Bishayi, B.; Hoge, M.; Messas, E.; Amar, S. Doxycycline Affects Diet- and Bacteria-Associated Atherosclerosis in an ApoE Heterozygote Murine Model: Cytokine Profiling Implications. Atherosclerosis 2007, 190, 62–72. [Google Scholar] [CrossRef] [PubMed]
- Bendeck, M.P.; Conte, M.; Zhang, M.; Nili, N.; Strauss, B.H.; Farwell, S.M. Doxycycline Modulates Smooth Muscle Cell Growth, Migration, and Matrix Remodeling after Arterial Injury. Am. J. Pathol. 2002, 160, 1089–1095. [Google Scholar] [CrossRef]
- Madrigal-Perez, V.M.; García-Rivera, A.; Rodriguez-Hernandez, A.; Ceja-Espiritu, G.; Briseño-Gomez, X.G.; Galvan-Salazar, H.R.; Soriano-Hernandez, A.D.; Guzman-Esquivel, J.; Martinez-Fierro, M.L.; Newton-Sanchez, O.A.; et al. Preclinical Analysis of Nonsteroidal Anti-Inflammatory Drug Usefulness for the Simultaneous Prevention of Steatohepatitis, Atherosclerosis and Hyperlipidemia. Int. J. Clin. Exp. Med. 2015, 8, 22477–22483. [Google Scholar]
- Powell, E.E.; Wong, V.W.-S.; Rinella, M. Non-Alcoholic Fatty Liver Disease. Lancet 2021, 397, 2212–2224. [Google Scholar] [CrossRef]
- Nishikawa, S.; Yasoshima, A.; Doi, K.; Nakayama, H.; Uetsuka, K. Involvement of Sex, Strain and Age Factors in High Fat Diet-Induced Obesity in C57BL/6J and BALB/cA Mice. Exp. Anim. 2007, 56, 263–272. [Google Scholar] [CrossRef]
- Jayaprakasam, B.; Olson, L.K.; Schutzki, R.E.; Tai, M.-H.; Nair, M.G. Amelioration of Obesity and Glucose Intolerance in High-Fat-Fed C57BL/6 Mice by Anthocyanins and Ursolic Acid in Cornelian Cherry (Cornus Mas). J. Agric. Food Chem. 2006, 54, 243–248. [Google Scholar] [CrossRef]
- Li, X.; Yu, X.; Sun, D.; Li, J.; Wang, Y.; Cao, P.; Liu, Y. Effects of Polar Compounds Generated from the Deep-Frying Process of Palm Oil on Lipid Metabolism and Glucose Tolerance in Kunming Mice. J. Agric. Food Chem. 2017, 65, 208–215. [Google Scholar] [CrossRef]
- Norris, G.H.; Porter, C.M.; Jiang, C.; Millar, C.L.; Blesso, C.N. Dietary Sphingomyelin Attenuates Hepatic Steatosis and Adipose Tissue Inflammation in High-Fat-Diet-Induced Obese Mice. J. Nutr. Biochem. 2017, 40, 36–43. [Google Scholar] [CrossRef]
- Jiménez-Maldonado, A.; Virgen-Ortiz, A.; Melnikov, V.; Rodríguez-Hernández, A.; Gamboa-Domínguez, A.; Montero, S.; Muñiz-Murguía, J.; Lemus, M.; Roces de Álvarez-Buylla, E. Effect of Moderate and High Intensity Chronic Exercise on the Pancreatic Islet Morphometry in Healthy Rats: BDNF Receptor Participation. Islets 2017, 9, 1–10. [Google Scholar] [CrossRef]
- Kim, A.; Miller, K.; Jo, J.; Kilimnik, G.; Wojcik, P.; Hara, M. Islet Architecture: A Comparative Study. Islets 2009, 1, 129–136. [Google Scholar] [CrossRef]
- Kneeman, J.M.; Misdraji, J.; Corey, K.E. Secondary Causes of Nonalcoholic Fatty Liver Disease. Ther. Adv. Gastroenterol. 2012, 5, 199–207. [Google Scholar] [CrossRef]
- Haddad, Y.; Vallerand, D.; Brault, A.; Spénard, J.; Haddad, P.S. NCX 1000 Alone or in Combination with Vitamin E Reverses Experimental Nonalcoholic Steatohepatitis in the Rat Similarly to UDCA. Int. J. Hepatol. 2011, 2011, 136816. [Google Scholar] [CrossRef]
- Kumamoto, R.; Uto, H.; Oda, K.; Ibusuki, R.; Tanoue, S.; Arima, S.; Mawatari, S.; Kumagai, K.; Numata, M.; Tamai, T.; et al. Dietary Fructose Enhances the Incidence of Precancerous Hepatocytes Induced by Administration of Diethylnitrosamine in Rat. Eur. J. Med. Res. 2013, 18, 54. [Google Scholar] [CrossRef]
- Montes-Galindo, D.A.; Espiritu-Mojarro, A.C.; Melnikov, V.; Moy-López, N.A.; Soriano-Hernandez, A.D.; Galvan-Salazar, H.R.; Guzman-Muñiz, J.; Guzman-Esquivel, J.; Martinez-Fierro, M.L.; Rodriguez-Sanchez, I.P.; et al. Adenovirus 5 Produces Obesity and Adverse Metabolic, Morphological, and Functional Changes in the Long Term in Animals Fed a Balanced Diet or a High-Fat Diet: A Study on Hamsters. Arch. Virol. 2019, 164, 775–786. [Google Scholar] [CrossRef]
- Cubeddu, L.X.; Hoffmann, I.S. One-Hour Postload Plasma Glucose Levels, a Predictor of Additional Risk for Diabetes: Prevalence, Mechanisms, and Associated Cardiovascular and Metabolic Risk Factors in Hispanics. Metab. Syndr. Relat. Disord. 2010, 8, 395–402. [Google Scholar] [CrossRef]
- Zheng, W.; Duan, M.; Jia, J.; Song, S.; Ai, C. Low-Molecular Alginate Improved Diet-Induced Obesity and Metabolic Syndrome through Modulating the Gut Microbiota in BALB/c Mice. Int. J. Biol. Macromol. 2021, 187, 811–820. [Google Scholar] [CrossRef] [PubMed]
- Hull, R.L.; Andrikopoulos, S.; Verchere, C.B.; Vidal, J.; Wang, F.; Cnop, M.; Prigeon, R.L.; Kahn, S.E. Increased Dietary Fat Promotes Islet Amyloid Formation and β-Cell Secretory Dysfunction in a Transgenic Mouse Model of Islet Amyloid. Diabetes 2003, 52, 372–379. [Google Scholar] [CrossRef] [PubMed]
- Simbolo, M.; Bilotta, M.; Mafficini, A.; Luchini, C.; Furlan, D.; Inzani, F.; Petrone, G.; Bonvissuto, D.; La Rosa, S.; Schinzari, G.; et al. Gene Expression Profiling of Pancreas Neuroendocrine Tumors with Different Ki67-Based Grades. Cancers 2021, 13, 2054. [Google Scholar] [CrossRef] [PubMed]
- Sakaguchi, K.; Takeda, K.; Maeda, M.; Ogawa, W.; Sato, T.; Okada, S.; Ohnishi, Y.; Nakajima, H.; Kashiwagi, A. Glucose Area under the Curve during Oral Glucose Tolerance Test as an Index of Glucose Intolerance. Diabetol. Int. 2016, 7, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Cobbina, E.; Akhlaghi, F. Non-Alcoholic Fatty Liver Disease (NAFLD)—Pathogenesis, Classification, and Effect on Drug Metabolizing Enzymes and Transporters. Drug Metab. Rev. 2017, 49, 197–211. [Google Scholar] [CrossRef] [PubMed]
- Clemens, D.L.; Duryee, M.J.; Hall, J.H.; Thiele, G.M.; Mikuls, T.R.; Klassen, L.W.; Zimmerman, M.C.; Anderson, D.R. Relevance of the Antioxidant Properties of Methotrexate and Doxycycline to Their Treatment of Cardiovascular Disease. Pharmacol. Ther. 2020, 205, 107413. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Granillo, G.; Rodriguez-Granillo, A.; Milei, J. Effect of Doxycycline on Atherosclerosis: From Bench to Bedside. PRC 2011, 6, 42–54. [Google Scholar] [CrossRef] [PubMed]
- Castro, M.M.; Kandasamy, A.D.; Youssef, N.; Schulz, R. Matrix Metalloproteinase Inhibitor Properties of Tetracyclines: Therapeutic Potential in Cardiovascular Diseases. Pharmacol. Res. 2011, 64, 551–560. [Google Scholar] [CrossRef] [PubMed]
- Poznyak, A.; Grechko, A.V.; Poggio, P.; Myasoedova, V.A.; Alfieri, V.; Orekhov, A.N. The Diabetes Mellitus-Atherosclerosis Connection: The Role of Lipid and Glucose Metabolism and Chronic Inflammation. Int. J. Mol. Sci. 2020, 21, 1835. [Google Scholar] [CrossRef] [PubMed]
- Kilimnik, G.; Zhao, B.; Jo, J.; Periwal, V.; Witkowski, P.; Misawa, R.; Hara, M. Altered Islet Composition and Disproportionate Loss of Large Islets in Patients with Type 2 Diabetes. PLoS ONE 2011, 6, e27445. [Google Scholar] [CrossRef]
- Tang, X.; Wang, X.; Zhao, Y.Y.; Curtis, J.M.; Brindley, D.N. Doxycycline Attenuates Breast Cancer Related Inflammation by Decreasing Plasma Lysophosphatidate Concentrations and Inhibiting NF-ΚB Activation. Mol. Cancer 2017, 16, 36. [Google Scholar] [CrossRef]
- La Sala, L.; Prattichizzo, F.; Ceriello, A. The Link between Diabetes and Atherosclerosis. Eur. J. Prev. Cardiol. 2019, 26, 15–24. [Google Scholar] [CrossRef]
- Alexander-Savino, C.V.; Hayden, M.S.; Richardson, C.; Zhao, J.; Poligone, B. Doxycycline Is an NF-ΚB Inhibitor That Induces Apoptotic Cell Death in Malignant T-Cells. Oncotarget 2016, 7, 75954–75967. [Google Scholar] [CrossRef]
- Esposito, K.; Ciotola, M.; Sasso, F.C.; Cozzolino, D.; Saccomanno, F.; Assaloni, R.; Ceriello, A.; Giugliano, D. Effect of a Single High-Fat Meal on Endothelial Function in Patients with the Metabolic Syndrome: Role of Tumor Necrosis Factor-α. Nutr. Metab. Cardiovasc. Dis. 2007, 17, 274–279. [Google Scholar] [CrossRef] [PubMed]
- Santa-Cecília, F.V.; Socias, B.; Ouidja, M.O.; Sepulveda-Diaz, J.E.; Acuña, L.; Silva, R.L.; Michel, P.P.; Del-Bel, E.; Cunha, T.M.; Raisman-Vozari, R. Doxycycline Suppresses Microglial Activation by Inhibiting the P38 MAPK and NF-KB Signaling Pathways. Neurotox. Res. 2016, 29, 447–459. [Google Scholar] [CrossRef]
- Ibrahim, A.S.; El-Remessy, A.B.; Matragoon, S.; Zhang, W.; Patel, Y.; Khan, S.; Al-Gayyar, M.M.; El-Shishtawy, M.M.; Liou, G.I. Retinal Microglial Activation and Inflammation Induced by Amadori-Glycated Albumin in a Rat Model of Diabetes. Diabetes 2011, 60, 1122–1133. [Google Scholar] [CrossRef] [PubMed]
- Hoogland, I.C.M.; Houbolt, C.; van Westerloo, D.J.; van Gool, W.A.; van de Beek, D. Systemic Inflammation and Microglial Activation: Systematic Review of Animal Experiments. J. Neuroinflammation 2015, 12, 114. [Google Scholar] [CrossRef] [PubMed]
- Delgado-Enciso, I.; Garciá-Rivera, A.; Madrigal-Pérez, M.V.M.; Rodriguez-Hernandez, A.; Lugo-Radillo, A.; Galvan-Salazar, H.R.; Soriano-Hernández, A.D.; Gómez-Tapia, F.; Martinez-Martinez, R.; Valdez-Velazquez, L.L.; et al. Protective Effect of Doxycycline on Germinal Epithelial Loss Caused by a High-Fat Diet. Int. Urol. Nephrol. 2014, 46, 895–899. [Google Scholar] [CrossRef]
- Kumar, S.; Behl, T.; Sachdeva, M.; Sehgal, A.; Kumari, S.; Kumar, A.; Kaur, G.; Yadav, H.N.; Bungau, S. Implicating the Effect of Ketogenic Diet as a Preventive Measure to Obesity and Diabetes Mellitus. Life Sci. 2021, 264, 118661. [Google Scholar] [CrossRef]
- Ahn, Y.; Jung, J.Y.; Kweon, O.; Veach, B.T.; Khare, S.; Gokulan, K.; Piñeiro, S.A.; Cerniglia, C.E. Impact of Chronic Tetracycline Exposure on Human Intestinal Microbiota in a Continuous Flow Bioreactor Model. Antibiotics 2021, 10, 886. [Google Scholar] [CrossRef]
- Davis, C.D. The Gut Microbiome and Its Role in Obesity. Nutr. Today 2016, 51, 167–174. [Google Scholar] [CrossRef]
- Fuoco, D. Classification Framework and Chemical Biology of Tetracycline-Structure-Based Drugs. Antibiotics 2012, 1, 1–13. [Google Scholar] [CrossRef]
- Wüst, R.C.I.; Coolen, B.F.; Held, N.M.; Daal, M.R.R.; Alizadeh Tazehkandi, V.; Baks-te Bulte, L.; Wiersma, M.; Kuster, D.W.D.; Brundel, B.J.J.M.; van Weeghel, M.; et al. The Antibiotic Doxycycline Impairs Cardiac Mitochondrial and Contractile Function. Int. J. Mol. Sci. 2021, 22, 4100. [Google Scholar] [CrossRef]
| Parameter | SD | HFD | HFD + Doxy | p |
|---|---|---|---|---|
| Initial food intake (g) c | 2.91 ± 0.69 | 3.16 ± 0.56 | 2.89 ± 1.21 | 0.670 |
| Final food intake (g) d | 6.86 ± 0.54 | 7.06 ± 0.94 | 6.70 ± 0.74 | 0.475 |
| Total cholesterol (mg/dL) | 138 ± 21 | 156 ± 51 | 144 ± 34 | 0.438 |
| Tryglicerids (mg/dL) | 224 ± 76 | 182 ± 49 | 191 ± 71 | 0.270 |
| Glucose (mg/dL) | 123.4 ± 11 | 119.3 ± 11 | 120.6 ± 16 | 0.276 |
| Insulin (mU/L) | 44 ± 30 | 79 ± 53 | 122 ± 24 | 0.020 |
| Body weight (g) | 31.5 ± 1.6 | 32.9 ± 2.2 | 31.9 ± 2.7 | 0.286 |
| Epididymal fat (g) | 0.8 ± 0.3 | 0.12 ± 0.3 | 0.18 ± 0.7 | <0.001 |
| Liver/Body weight ratio | 0.046 ± 0.006 | 0.055 ± 0.006 | 0.058 ± 0.007 | <0.001 |
| Steatosis | 0.4 ± 0.5 | 2.2 ± 0.4 | 1.8 ± 0.9 | <0.001 b |
| Liver inflammation | 0.3 ± 0.6 | 1.5 ± 0.5 | 1.0 ± 0.3 | <0.001 b |
| ALT (U/L) | 144 ± 21 | 190 ± 58 | 171 ± 35 | 0.030 |
| AST (U/L) | 1001 ± 166 | 933 ± 332 | 1128 ± 338 | 0.244 |
| Width of abdominal aorta (µm) | 62.9 ± 11 | 76.4 ± 18 | 60.7 ± 12 | <0.001 |
| Number of islets (per mm2) | 7.5 (6–9.5) | 4 (3–10) | 9 (8–12) | 0.030 b |
| Size of islets µm2 | 8537 (3518–16,555) | 7801 (5406–13,428) | 7171 (3435–14,121) | 0.959 b |
| Islet size distribution | ||||
| Small Medium Large | 55.3% 31.9% 12.8% | 63.2% 36.8% 0.0% | 51.6% 37.5% 10.9% | 0.528 b |
| Number of β cells (per mm2) | 1179 (622–1990) | 466 (264–932) | 1202 (819–1341) | 0.002 b |
| Single-cell area β µm2 | 95 (91–105) | 114 (95–120) | 104 (100–111) | 0.002 b |
| Beta cell cytoplasmatic area µm2 | 76.4 (69–85) | 93.7 (78–99) | 84.1 (79–89) | 0.002 b |
| Percentage of positive area per islet | ||||
| Insulin Ki67 PD-1 | 66.5 (61.3–70.7) 1.6 (0.0–3.3) 3.7 (0.0–9.6) | 66.4 (59.0–72.0) 6.2 (3.1–13.3) 6.6 (3.6–15.1) | 65.2 (53.4–70.4) 0.0 (0.0–4.4) 3.5 (0.0–8.3) | 0.554 b <0.001 b 0.148 b |
| Parameter | SD vs. HFD | SD vs. HFD + Doxy | HFD vs. HFD + Doxy |
|---|---|---|---|
| Insulin (mU/L) | 0.285 a | 0.019 a | 0.309 a |
| ALT (U/L) | 0.035 a | 0.226 a | 0.790 a |
| Liver/Body weight ratio | 0.013 a | <0.001 a | 0.802 a |
| Epididymal fat (g) | 0.205 a | 0.000 a | 0.015 a |
| Width of abdominal aorta (µm) | <0.001 a | 0.720 a | <0.001 a |
| Liver inflammation | <0.001 b | 0.002 b | 0.120 b |
| Steatosis | <0.001 b | <0.001 b | 0.403 b |
| Number of islets | 0.241 b | 0.082 b | 0.047 b |
| Number of beta cells | 0.036 b | 0.873 b | 0.030 b |
| Area of beta cells | 0.047 b | 0.042 b | 0.497 b |
| Cytoplasmic area of beta cell | 0.031 b | 0.059 b | 0.418 b |
| Ki67-positive area per islet | 0.001 b | 0.223 b | <0.001 b |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodriguez-Hernandez, A.; Delgado-Machuca, M.; Guardado-Mendoza, R.; Mendoza-Hernandez, M.A.; Melnikov, V.; Delgado-Enciso, O.G.; Tiburcio-Jimenez, D.; Ceja-Espiritu, G.; Hernandez-Fuentes, G.A.; Gamboa-Dominguez, A.; et al. Doxycycline Prevents Preclinical Atherosclerosis, Pancreatic Islet Loss and Improves Insulin Secretion after Glycemic Stimulation: Preclinical Study in Individuals with a High-Fat Diet. Biomedicines 2023, 11, 717. https://doi.org/10.3390/biomedicines11030717
Rodriguez-Hernandez A, Delgado-Machuca M, Guardado-Mendoza R, Mendoza-Hernandez MA, Melnikov V, Delgado-Enciso OG, Tiburcio-Jimenez D, Ceja-Espiritu G, Hernandez-Fuentes GA, Gamboa-Dominguez A, et al. Doxycycline Prevents Preclinical Atherosclerosis, Pancreatic Islet Loss and Improves Insulin Secretion after Glycemic Stimulation: Preclinical Study in Individuals with a High-Fat Diet. Biomedicines. 2023; 11(3):717. https://doi.org/10.3390/biomedicines11030717
Chicago/Turabian StyleRodriguez-Hernandez, Alejandrina, Marina Delgado-Machuca, Rodolfo Guardado-Mendoza, Martha A. Mendoza-Hernandez, Valery Melnikov, Osiris G. Delgado-Enciso, Daniel Tiburcio-Jimenez, Gabriel Ceja-Espiritu, Gustavo A. Hernandez-Fuentes, Armando Gamboa-Dominguez, and et al. 2023. "Doxycycline Prevents Preclinical Atherosclerosis, Pancreatic Islet Loss and Improves Insulin Secretion after Glycemic Stimulation: Preclinical Study in Individuals with a High-Fat Diet" Biomedicines 11, no. 3: 717. https://doi.org/10.3390/biomedicines11030717
APA StyleRodriguez-Hernandez, A., Delgado-Machuca, M., Guardado-Mendoza, R., Mendoza-Hernandez, M. A., Melnikov, V., Delgado-Enciso, O. G., Tiburcio-Jimenez, D., Ceja-Espiritu, G., Hernandez-Fuentes, G. A., Gamboa-Dominguez, A., Guzman-Esquivel, J., Martinez-Fierro, M. L., Rodriguez-Sanchez, I. P., & Delgado-Enciso, I. (2023). Doxycycline Prevents Preclinical Atherosclerosis, Pancreatic Islet Loss and Improves Insulin Secretion after Glycemic Stimulation: Preclinical Study in Individuals with a High-Fat Diet. Biomedicines, 11(3), 717. https://doi.org/10.3390/biomedicines11030717