High Rate of Discontinuation during Long-Acting Injectable Antipsychotic Treatment in Patients with Psychotic Disorders
Abstract
1. Introduction
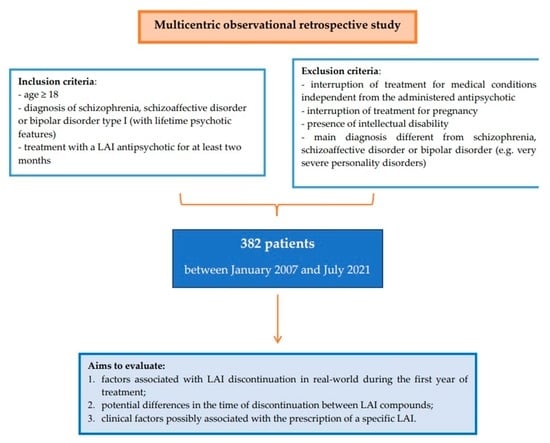
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Christensen, K.; Doblhammer, G.; Rau, R.; Vaupel, J.W. Ageing populations: The challenges ahead. Lancet 2009, 374, 1196–1208. [Google Scholar] [CrossRef] [PubMed]
- Bodenheimer, T.; Lorig, K.; Holman, H.; Grumbach, K. Patient self-management of chronic disease in primary care. JAMA 2002, 288, 2469–2475. [Google Scholar] [CrossRef] [PubMed]
- Sabaté, E. Adherence to Long-Term Therapies: Evidence for Action; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Keramatian, K.; Chakrabarty, T.; Yatham, L.N. Long-Acting Injectable Second-Generation/Atypical Antipsychotics for the Management of Bipolar Disorder: A Systematic Review. CNS Drugs 2019, 33, 431–456. [Google Scholar] [CrossRef] [PubMed]
- Sheffield, J.M.; Karcher, N.R.; Barch, D.M. Cognitive Deficits in Psychotic Disorders: A Lifespan Perspective. Neuropsychol. Rev. 2018, 28, 509–533. [Google Scholar] [CrossRef]
- Kane, J.M.; Garcia-Ribera, C. Clinical guideline recommendations for antipsychotic long-acting injections. Br. J. Psychiatry Suppl. 2009, 52, S63–S67. [Google Scholar] [CrossRef]
- Buoli, M.; Kahn, R.S.; Serati, M.; Altamura, A.C.; Cahn, W. Haloperidol versus second-generation antipsychotics in the long-term treatment of schizophrenia. Hum. Psychopharmacol. 2016, 31, 325–331. [Google Scholar] [CrossRef]
- Carbon, M.; Correll, C.U. Clinical predictors of therapeutic response to antipsychotics in schizophrenia. Dialogues Clin. Neurosci. 2014, 16, 505–524. [Google Scholar] [CrossRef]
- Shimomura, Y.; Kikuchi, Y.; Suzuki, T.; Uchida, H.; Mimura, M.; Takeuchi, H. Antipsychotic treatment in the maintenance phase of schizophrenia: An updated systematic review of the guidelines and algorithms. Schizophr. Res. 2020, 215, 8–16. [Google Scholar] [CrossRef]
- Kane, J.M.; Kishimoto, T.; Correll, C.U. Assessing the comparative effectiveness of long-acting injectable vs. oral antipsychotic medications in the prevention of relapse provides a case study in comparative effectiveness research in psychiatry. J. Clin. Epidemiol. 2013, 66, S37–S41. [Google Scholar] [CrossRef]
- Correll, C.U.; Citrome, L.; Haddad, P.M.; Lauriello, J.; Olfson, M.; Calloway, S.M.; Kane, J.M. The Use of Long-Acting Injectable Antipsychotics in Schizophrenia: Evaluating the Evidence. J. Clin. Psychiatry. 2016, 77, 1–24. [Google Scholar] [CrossRef]
- Tiihonen, J.; Mittendorfer-Rutz, E.; Majak, M.; Mehtälä, J.; Hoti, F.; Jedenius, E.; Enkusson, D.; Leval, A.; Sermon, J.; Tanskanen, A.; et al. Real-World Effectiveness of Antipsychotic Treatments in a Nationwide Cohort of 29 823 Patients With Schizophrenia. JAMA Psychiatry. 2017, 74, 686–693. [Google Scholar] [CrossRef] [PubMed]
- Fabrazzo, M.; Cipolla, S.; Camerlengo, A.; Perris, F.; Catapano, F. Second-Generation Antipsychotics’ Effectiveness and Tolerability: A Review of Real-World Studies in Patients with Schizophrenia and Related Disorders. J. Clin. Med. 2022, 11, 4530. [Google Scholar] [CrossRef] [PubMed]
- Davis, J.M.; Chen, N.; Glick, I.D. A meta-analysis of the efficacy of second-generation antipsychotics. Arch. Gen. Psychiatry. 2003, 60, 553–564. [Google Scholar] [CrossRef] [PubMed]
- McCreath, J.; Larson, E.; Bharatiya, P.; Labanieh, H.A.; Weiss, Z.; Lozovatsky, M. Long-Acting Injectable Antipsychotics for Schizophrenia: Sociodemographic Characteristics and Treatment Adherence. Prim. Care Companion CNS Disord. 2017, 19. [Google Scholar] [CrossRef]
- Gentile, S. Discontinuation rates during long-term, second-generation antipsychotic long-acting injection treatment: A systematic review. Psychiatry Clin. Neurosci. 2019, 73, 216–230. [Google Scholar] [CrossRef]
- Wu, C.S.; Hsieh, M.H.; Tang, C.H.; Chang, C.J. Comparative effectiveness of long-acting injectable risperidone vs. long-acting injectable first-generation antipsychotics in bipolar disorder. J. Affect. Disord. 2016, 197, 189–195. [Google Scholar] [CrossRef]
- Tatini, L.; D’Anna, G.; Pietrini, F.; Calligaris, E.; Ballerini, A.; Ricca, V. Predictors of long-acting injectable antipsychotic treatment discontinuation in outpatients with schizophrenia: Relevance of the Drug Attitude Inventory-10. Int. Clin. Psychopharmacol. 2021, 36, 181–187. [Google Scholar] [CrossRef]
- Aguglia, A.; Fusar-Poli, L.; Natale, A.; Amerio, A.; Espa, I.; Villa, V.; Martinotti, G.; Carrà, G.; Bartoli, F.; D’Agostino, A.; et al. Factors Associated with Medication Adherence to Long-Acting Injectable Antipsychotics: Results from the STAR Network Depot Study. Pharmacopsychiatry 2022, 55, 281–289. [Google Scholar] [CrossRef]
- Barbui, C.; Bertolini, F.; Bartoli, F.; Calandra, C.; Callegari, C.; Carrà, G.; D’Agostino, A.; Lucii, C.; Martinotti, G.; Mastromo, D.; et al. STAR Network Investigators. Reasons for initiating long-acting antipsychotics in psychiatric practice: Findings from the STAR Network Depot Study. Ther. Adv. Psychopharmacol. 2020, 10, 8102. [Google Scholar] [CrossRef]
- Perkins, D.O.; Gu, H.; Weiden, P.J.; McEvoy, J.P.; Hamer, R.M.; Lieberman, J.A. Comparison of Atypicals in First Episode study group. Predictors of treatment discontinuation and medication nonadherence in patients recovering from a first episode of schizophrenia, schizophreniform disorder, or schizoaffective disorder: A randomized, double-blind, flexible-dose, multicenter study. J. Clin. Psychiatry 2008, 69, 106–113. [Google Scholar] [CrossRef]
- Leucht, S.; Cipriani, A.; Spineli, L.; Mavridis, D.; Orey, D.; Richter, F.; Samara, M.; Barbui, C.; Engel, R.R.; Geddes, J.R.; et al. Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: A multiple-treatments meta-analysis. Lancet 2013, 382, 951–962. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5; American Psychiatric Press: Washington, DC, USA, 2013. [Google Scholar] [CrossRef]
- Lora, A.; Monzani, E.; Ibrahim, B.; Soranna, D.; Corrao, G. Routine quality care assessment of schizophrenic disorders using information systems. Int. J. Qual. Health Care. 2018, 30, 157. [Google Scholar] [CrossRef] [PubMed]
- Buoli, M.; Cesana, B.M.; Fagiolini, A.; Albert, U.; Maina, G.; de Bartolomeis, A.; Pompili, M.; Bondi, E.; Steardo, L., Jr.; Amore, M.; et al. ISBD Italian Chapter Epidemiologic Group. Which factors delay treatment in bipolar disorder? A nationwide study focussed on duration of untreated illness. Early Interv. Psychiatry. 2021, 15, 1136–1145. [Google Scholar] [CrossRef] [PubMed]
- Mahlich, J.; Olbrich, K.; Wilk, A.; Wimmer, A.; Wolff-Menzler, C. Time to Treatment Discontinuation in German Patients with Schizophrenia: Long-Acting Injectables versus Oral Antipsychotics. Clin. Drug Investig. 2021, 41, 99–113. [Google Scholar] [CrossRef] [PubMed]
- Rittmannsberger, H.; Rosenleitner, J.; Malsiner-Walli, G.; Werl, R.; Rittmannsberger, B.; Yazdi, K. Treatment Duration With Long-Acting Injectable Antipsychotics After In-hospital Initiation: A Retrospective Cohort Study. J. Clin. Psychopharmacol. 2017, 37, 250–254. [Google Scholar] [CrossRef]
- Goel, M.K.; Khanna, P.; Kishore, J. Understanding survival analysis: Kaplan-Meier estimate. Int. J. Ayurveda Res. 2010, 1, 274–278. [Google Scholar] [CrossRef]
- Buoli, M.; Dell’osso, B.; Zaytseva, Y.; Gurovich, I.Y.; Movina, L.; Dorodnova, A.; Shmuckler, A.; Altamura, A.C. Duration of untreated illness (DUI) and schizophrenia sub-types: A collaborative study between the universities of Milan and Moscow. Int. J. Soc. Psychiatry. 2013, 59, 765–770. [Google Scholar] [CrossRef]
- Stahl, S.M. Long-acting injectable antipsychotics: Shall the last be first? CNS Spectr. 2014, 19, 3–5. [Google Scholar] [CrossRef]
- Ostuzzi, G.; Mazzi, M.A.; Terlizzi, S.; Bertolini, F.; Aguglia, A.; Bartoli, F.; Bortolaso, P.; Callegari, C.; Caroleo, M.; Carrà, G.; et al. STAR Network Investigators. Factors associated with first- versus second-generation long-acting antipsychotics prescribed under ordinary clinical practice in Italy. PloS ONE 2018, 13, e0201371. [Google Scholar] [CrossRef]
- Şahin, O.Ş.; Mursalova, Z.; Gadimov, S.; Üçok, A. Predictors of long-acting injectable antipsychotic prescription at discharge in patients with schizophrenia and other psychotic disorders. Int. Clin. Psychopharmacol. 2021, 36, 251–256. [Google Scholar] [CrossRef]
- Waddell, L.; Taylor, M. Attitudes of patients and mental health staff to antipsychotic long-acting injections: Systematic review. Br. J. Psychiatry Suppl. 2009, 52, S43–S50. [Google Scholar] [CrossRef]
- Grover, S.; Sahoo, S.; Mehra, A. Perceptions of Psychiatrists Toward the Use of Long-Acting Injectable Antipsychotics: An Online Survey Study From India. J. Clin. Psychopharmacol. 2019, 39, 611–619. [Google Scholar] [CrossRef]
- Carr, C.N.; Hall, C.P.; Roche-Desilets, J.E.; Burant, C.J.; Fuller, M.A. Evaluation of adherence in patients prescribed long-acting injectable antipsychotics: A comparison of biweekly versus monthly administered neuroleptics. Ment Health Clin. 2016, 6, 248–253. [Google Scholar] [CrossRef]
- Llorca, P.M.; Bobes, J.; Fleischhacker, W.W.; Heres, S.; Moore, N.; Bent-Ennakhil, N.; Sapin, C.; Loze, J.Y.; Nylander, A.G.; Patel, M.X. Baseline results from the European non-interventional Antipsychotic Long acTing injection in schizOphrenia (ALTO) study. Eur. Psychiatry 2018, 52, 85–94. [Google Scholar] [CrossRef]
- Üçok, A.; Yağcioğlu, E.A.; Aydin, M.; Kara, İ.A.; Erbasan, V.; Türkoğlu, Ö.; Ergün, S.; Chousein, M.G.; Oktar, N.; Uçar, N.; et al. Predictors of discontinuation and hospitalization during long-acting injectable antipsychotic treatment in patients with schizophrenia spectrum disorder. Int. Clin. Psychopharmacol. 2021, 36, 89–96. [Google Scholar] [CrossRef]
- Greene, M.; Yan, T.; Chang, E.; Hartry, A.; Touya, M.; Broder, M.S. Medication adherence and discontinuation of long-acting injectable versus oral antipsychotics in patients with schizophrenia or bipolar disorder. J. Med. Econ. 2018, 21, 127–134. [Google Scholar] [CrossRef]
- Vita, A.; Perin, A.P.; Cavanna, M.; Cobelli, F.; Rosa, J.; Valsecchi, P.; Zanigni, M.; Reggiardo, G.; Sacchetti, E. Negative symptom severity at discharge from an index hospitalization and subsequent use of psychiatric care resources: A retrospective 1-year follow-up study on 450 patients with schizophrenia spectrum disorders. Schizophr. Res. 2020, 216, 243–248. [Google Scholar] [CrossRef]
- Barlati, S.; Nibbio, G.; Calzavara-Pinton, I.; Invernizzi, E.; Cadei, L.; Lisoni, J.; Valsecchi, P.; Deste, G.; Vita, A. Primary and secondary negative symptoms severity and the use of psychiatric care resources in schizophrenia spectrum disorders: A 3-year follow-up longitudinal retrospective study. Schizophr. Res. 2022, 250, 31–38. [Google Scholar] [CrossRef]
- Misawa, F.; Kishimoto, T.; Hagi, K.; Kane, J.M.; Correll, C.U. Safety and tolerability of long-acting injectable versus oral antipsychotics: A meta-analysis of randomized controlled studies comparing the same antipsychotics. Schizophr. Res. 2016, 176, 220–230. [Google Scholar] [CrossRef]
- Kishimoto, T.; Robenzadeh, A.; Leucht, C.; Leucht, S.; Watanabe, K.; Mimura, M.; Borenstein, M.; Kane, J.M.; Correll, C.U. Long-acting injectable vs oral antipsychotics for relapse prevention in schizophrenia: A meta-analysis of randomized trials. Schizophr. Bull. 2014, 40, 192–213. [Google Scholar] [CrossRef]
- Brnabic, A.J.; Kelin, K.; Ascher-Svanum, H.; Montgomery, W.; Kadziola, Z.; Karagianis, J. Medication discontinuation with depot and oral antipsychotics in outpatients with schizophrenia: Comparison of matched cohorts from a 12-month observational study. Int. J. Clin. Pract. 2011, 65, 945–953. [Google Scholar] [CrossRef] [PubMed]
- Bertolini, F.; Ostuzzi, G.; Pievani, M.; Aguglia, A.; Bartoli, F.; Bortolaso, P.; Callegari, C.; Caroleo, M.; Carrà, G.; Corbo, M.; et al. STAR Network Investigators. Comparing Long-Acting Antipsychotic Discontinuation Rates Under Ordinary Clinical Circumstances: A Survival Analysis from an Observational, Pragmatic Study. CNS Drugs 2021, 35, 655–665. [Google Scholar] [CrossRef] [PubMed]
- Yan, T.; Greene, M.; Chang, E.; Hartry, A.; Touya, M.; Broder, M.S. Medication Adherence and Discontinuation of Aripiprazole Once-Monthly 400 mg (AOM 400) Versus Oral Antipsychotics in Patients with Schizophrenia or Bipolar I Disorder: A Real-World Study Using US Claims Data. Adv. Ther. 2018, 35, 1612–1625. [Google Scholar] [CrossRef] [PubMed]
- Saucedo Uribe, E.; Carranza Navarro, F.; Guerrero Medrano, A.F.; García Cervantes, K.I.; Álvarez Villalobos, N.A.; Acuña Rocha, V.D.; Méndez Hernández, M.; Millán Alanís, J.M.; Hinojosa Cavada, C.M.; Zúñiga Hernández, J.A.; et al. Preliminary efficacy and tolerability profiles of first versus second-generation Long-Acting Injectable Antipsychotics in schizophrenia: A systematic review and meta-analysis. J. Psychiatr. Res. 2020, 129, 222–233. [Google Scholar] [CrossRef]
- Stone, J.M.; Roux, S.; Taylor, D.; Morrison, P.D. First-generation versus second-generation long-acting injectable antipsychotic drugs and time to relapse. Ther. Adv. Psychopharmacol. 2018, 8, 333–336. [Google Scholar] [CrossRef]
- Taipale, H.; Mittendorfer-Rutz, E.; Alexanderson, K.; Majak, M.; Mehtälä, J.; Hoti, F.; Jedenius, E.; Enkusson, D.; Leval, A.; Sermon, J.; et al. Antipsychotics and mortality in a nationwide cohort of 29,823 patients with schizophrenia. Schizophr. Res. 2018, 197, 274–280. [Google Scholar] [CrossRef]
- Ostuzzi, G.; Bertolini, F.; Tedeschi, F.; Vita, G.; Brambilla, P.; Del Fabro, L.; Gastaldon, C.; Papola, D.; Purgato, M.; Nosari, G.; et al. Oral and long-acting antipsychotics for relapse prevention in schizophrenia-spectrum disorders: A network meta-analysis of 92 randomized trials including 22,645 participants. World Psychiatry 2022, 21, 295–307. [Google Scholar] [CrossRef]
- Bellavia, A.; Centorrino, F.; Jackson, J.W.; Fitzmaurice, G.; Valeri, L. The role of weight gain in explaining the effects of antipsychotic drugs on positive and negative symptoms: An analysis of the CATIE schizophrenia trial. Schizophr. Res. 2019, 206, 96–102. [Google Scholar] [CrossRef]
- Ostuzzi, G.; Bertolini, F.; Del Giovane, C.; Tedeschi, F.; Bovo, C.; Gastaldon, C.; Nosé, M.; Ogheri, F.; Papola, D.; Purgato, M.; et al. Maintenance Treatment With Long-Acting Injectable Antipsychotics for People With Nonaffective Psychoses: A Network Meta-Analysis. Am. J. Psychiatry 2021, 178, 424–436. [Google Scholar] [CrossRef]
- Joo, S.W.; Shon, S.H.; Choi, G.; Koh, M.; Cho, S.W.; Lee, J. Continuation of schizophrenia treatment with three long-acting injectable antipsychotics in South Korea: A nationwide population-based study. Eur. Neuropsychopharmacol. 2019, 29, 1051–1060. [Google Scholar] [CrossRef]
- Ringen, P.A.; Reponen, E.J.; Vedal, T.S.J.; Andreassen, O.A.; Steen, N.E.; Melle, I. Predictors for Antipsychotic Dosage Change in the First Year of Treatment in Schizophrenia Spectrum and Bipolar Disorders. Front. Psychiatry 2019, 10, 649. [Google Scholar] [CrossRef]
- Ascher-Svanum, H.; Zhao, F.; Detke, H.C.; Nyhuis, A.W.; Lawson, A.H.; Stauffer, V.L.; Montgomery, W.; Witte, M.M.; McDonnell, D.P. Early response predicts subsequent response to olanzapine long-acting injection in a randomized, double-blind clinical trial of treatment for schizophrenia. BMC psychiatry 2011, 11, 152. [Google Scholar] [CrossRef]
- Velligan, D.I.; Sajatovic, M.; Hatch, A.; Kramata, P.; Docherty, J.P. Why do psychiatric patients stop antipsychotic medication? A systematic review of reasons for nonadherence to medication in patients with serious mental illness. Patient Prefer Adherence 2017, 11, 449–468. [Google Scholar] [CrossRef]
- Surace, T.; Capuzzi, E.; Caldiroli, A.; Ceresa, A.; Esposito, C.M.; Auxilia, A.M.; Tagliabue, I.; Capellazzi, M.; Legnani, F.; Di Paolo, M.; et al. Which Clinical and Biochemical Parameters Are Associated with Lifetime Suicide Attempts in Bipolar Disorder? Diagnostics 2022, 12, 2215. [Google Scholar] [CrossRef]
- Koola, M.M.; Wehring, H.J.; Kelly, D.L. The Potential Role of Long-acting Injectable Antipsychotics in People with Schizophrenia and Comorbid Substance Use. J. Dual Diagn. 2012, 8, 50–61. [Google Scholar] [CrossRef]
- Capuzzi, E.; Caldiroli, A.; Besana, F.; Cova, F.; Buoli, M.; Clerici, M. Factors associated with psychotic symptoms among a sample of male prisoners with substance use disorder: A cross-sectional study. J. Subst Abuse Treat. 2020, 118, 108104. [Google Scholar] [CrossRef]
- McCleery, A.; Nuechterlein, K.H. Cognitive impairment in psychotic illness: Prevalence, profile of impairment, developmental course, and treatment considerations. Dialogues Clin. Neurosci. 2019, 21, 239–248. [Google Scholar] [CrossRef]
- Buoli, M.; Caldiroli, A.; Panza, G.; Altamura, A.C. Prominent clinical dimension, duration of illness and treatment response in schizophrenia: A naturalistic study. Psychiatry Investig. 2012, 9, 354–360. [Google Scholar] [CrossRef]
- Gicas, K.M.; Parmar, P.K.; Fabiano, G.F.; Mashhadi, F. Substance-induced psychosis and cognitive functioning: A systematic review. Psychiatry Res. 2022, 308, 114361. [Google Scholar] [CrossRef]
- Lui, S.S.Y.; Lam, J.P.Y.; Lam, J.W.S.; Chui, W.W.H.; Mui, J.H.C.; Siu, B.W.M.; Cheng, K.M.; Cheung, E.F.C.; Chan, R.C.K. Cognitive insight is correlated with cognitive impairments and contributes to medication adherence in schizophrenia patients. Asian J. Psychiatr. 2021, 60, 102644. [Google Scholar] [CrossRef]
- Schoeler, T.; Petros, N.; Di Forti, M.; Klamerus, E.; Foglia, E.; Murray, R.; Bhattacharyya, S. Poor medication adherence and risk of relapse associated with continued cannabis use in patients with first-episode psychosis: A prospective analysis. Lancet Psychiatry 2017, 4, 627–633. [Google Scholar] [CrossRef] [PubMed]
- Capuzzi, E.; Ceresa, A.; Caldiroli, A.; Esposito, C.M.; Ossola, P.; Buoli, M. The Relation between the Plasma Concentrations of Long-Acting Atypical Antipsychotics and Clinical Effectiveness in Patients Affected by Schizophrenia or Schizoaffective Disorder: A Comprehensive Overview. Curr. Pharm Des. 2021, 27, 4070–4077. [Google Scholar] [CrossRef] [PubMed]
- Rahman, S.; Marwaha, R. Haloperidol. 2022 Jul 4. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Tang, C.T.; Chua, E.C.; Chew, Q.H.; He, Y.L.; Si, T.M.; Chiu, H.F.; Xiang, Y.T.; Kato, T.A.; Kanba, S.; Shinfuku, N.; et al. Patterns of long acting injectable antipsychotic use and associated clinical factors in schizophrenia among 15 Asian countries and region. Asia Pac. Psychiatry 2020, 12, e12393. [Google Scholar] [CrossRef] [PubMed]
- Lejoyeux, M.; Nivoli, F.; Basquin, A.; Petit, A.; Chalvin, F.; Embouazza, H. An Investigation of Factors Increasing the Risk of Aggressive Behavior among Schizophrenic Inpatients. Front. Psychiatry 2013, 4, 97. [Google Scholar] [CrossRef] [PubMed]
- Becarevic, N.; Softic, R.; Osmanovic, E. Does the Duration of the Illness Affect the Severity of Negative Symptoms of Schizophrenia? Mater. Sociomed. 2022, 34, 25–27. [Google Scholar] [CrossRef]
- Magliocco, F.; de Filippis, R.; Aloi, M.; Staltari, F.A.; Gaetano, R.; Segura-Garcia, C.; De Fazio, P. Second-generation long-acting injections anti-psychotics improve executive functions in patients with schizophrenia: A 12-month real-world study. Int. J. Psychiatry Clin. Pract. 2020, 24, 201–207. [Google Scholar] [CrossRef]
- Lin, C.H.; Chan, H.Y.; Hsu, C.C.; Chen, F.C. Time to rehospitalization in patients with bipolar mania discharged on long-acting injectable or oral antipsychotics. J. Affect. Disord. 2021, 279, 292–298. [Google Scholar] [CrossRef]
- Biagi, E.; Capuzzi, E.; Colmegna, F.; Mascarini, A.; Brambilla, G.; Ornaghi, A.; Santambrogio, J.; Clerici, M. Long-Acting Injectable Antipsychotics in Schizophrenia: Literature Review and Practical Perspective, with a Focus on Aripiprazole Once-Monthly. Adv. Ther. 2017, 34, 1036–1048. [Google Scholar] [CrossRef]
- Brown, E.S.; Jeffress, J.; Liggin, J.D.; Garza, M.; Beard, L. Switching outpatients with bipolar or schizoaffective disorders and substance abuse from their current antipsychotic to aripiprazole. J. Clin. Psychiatry 2005, 66, 756–760. [Google Scholar] [CrossRef]
- Kishi, T.; Matsuda, Y.; Iwata, N.; Correll, C.U. Antipsychotics for cocaine or psychostimulant dependence: Systematic review and meta-analysis of randomized, placebo-controlled trials. J. Clin. Psychiatry 2013, 74, e1169–e1180. [Google Scholar] [CrossRef]
- Cuomo, I.; Kotzalidis, G.D.; de Persis, S.; Piacentino, D.; Perrini, F.; Amici, E.; De Filippis, S. Head-to-head comparison of 1-year aripiprazole long-acting injectable (LAI) versus paliperidone LAI in comorbid psychosis and substance use disorder: Impact on clinical status, substance craving, and quality of life. Neuropsychiatr. Dis. Treat. 2018, 14, 1645–1656. [Google Scholar] [CrossRef]
- Szerman, N.; Basurte-Villamor, I.; Vega, P.; Martinez-Raga, J.; Parro-Torres, C.; Cambra Almerge, J.; Grau-López, L.; De Matteis, M.; Arias, F. Once-Monthly Long-Acting Injectable Aripiprazole for the Treatment of Patients with Schizophrenia and Co-occurring Substance Use Disorders: A Multicentre, Observational Study. Drugs Real. World Outcomes 2020, 7, 75–83. [Google Scholar] [CrossRef]
- Higashi, K.; Medic, G.; Littlewood, K.J.; Diez, T.; Granström, O.; De Hert, M. Medication adherence in schizophrenia: Factors influencing adherence and consequences of nonadherence, a systematic literature review. Ther. Adv. Psychopharmacol. 2013, 3, 200–218. [Google Scholar] [CrossRef]
- Vita, A.; De Peri, L.; Deste, G.; Barlati, S.; Sacchetti, E. The Effect of Antipsychotic Treatment on Cortical Gray Matter Changes in Schizophrenia: Does the Class Matter? A Meta-analysis and Meta-regression of Longitudinal Magnetic Resonance Imaging Studies. Biol. Psychiatry 2015, 78, 403–412. [Google Scholar] [CrossRef]
- Capuzzi, E.; Caldiroli, A.; Ciscato, V.; Russo, S.; Buoli, M. Experimental Serotonergic Agents for the Treatment of Schizophrenia. J. Exp. Pharmacol. 2021, 13, 49–67. [Google Scholar] [CrossRef]
- Chen, A.T.; Nasrallah, H.A. Neuroprotective effects of the second generation antipsychotics. Schizophr. Res. 2019, 208, 1–7. [Google Scholar] [CrossRef]
- Nasrallah, H.A.; Chen, A.T. Multiple neurotoxic effects of haloperidol resulting in neuronal death. Ann. Clin. Psychiatry 2017, 29, 195–202. [Google Scholar]
- Caldiroli, A.; Capuzzi, E.; Barkin, J.L.; Grassi, S.; Esposito, C.M.; Auxilia, A.M.; Russo, S.; Tagliabue, I.; Carnevali, G.S.; Mucci, F.; et al. Is there an association between inflammatory/anti-oxidant markers and the presence of psychotic symptoms or severity of illness in mood and psychotic disorders? A multi-centric study on a drug-free sample. Brain Behav. Immun. Health 2022, 22, 100453. [Google Scholar] [CrossRef]
- Capuzzi, E.; Bartoli, F.; Crocamo, C.; Clerici, M.; Carrà, G. Acute variations of cytokine levels after antipsychotic treatment in drug-naïve subjects with a first-episode psychosis: A meta-analysis. Neurosci. Biobehav. Rev. 2017, 77, 122–128. [Google Scholar] [CrossRef]
- Taipale, H.; Tanskanen, A.; Correll, C.U.; Tiihonen, J. Real-world effectiveness of antipsychotic doses for relapse prevention in patients with first-episode schizophrenia in Finland: A nationwide, register-based cohort study. Lancet Psychiatry 2022, 9, 271–279. [Google Scholar] [CrossRef]
- Kane, J.M.; Kishimoto, T.; Correll, C.U. Non-adherence to medication in patients with psychotic disorders: Epidemiology, contributing factors and management strategies. World Psychiatry 2013, 12, 216–226. [Google Scholar] [CrossRef] [PubMed]
| Variables | Total Sample N = 382 | |
|---|---|---|
| Gender | Male | 221 (57.9) |
| Female | 161 (42.1) | |
| Age (years) | 45.43 (12.79) | |
| Work status | Employed * | 304 (79.6) |
| Unemployed | 78 (20.4) | |
| Marital status | Single | 221 (57.9) |
| Married/cohabitant | 161 (42.1) | |
| Age at onset (years) | 27.04 (8.29) | |
| Diagnosis | Bipolar Disorder | 101 (26.4) |
| Schizoaffective disorder | 59 (15.4) | |
| Schizophrenia | 222 (58.2) | |
| Duration of illness (years) | 18.52 (12.70) | |
| Duration of Untreated Illness (DUI) (years) | 2.60 (5.32) | |
| Presence of personality disorders | Yes | 52 (13.6) |
| No | 330 (86.4) | |
| Family history of psychiatric disorders Missing: 10 | Yes | 144 (38.7) |
| No | 228 (61.3) | |
| Multiple family history of psychiatric disorders Missing: 11 | Yes | 42 (11.3) |
| No | 329 (88.7) | |
| Pre-onset psychiatric comorbidity | Yes | 65 (17.0) |
| No | 317 (83.0) | |
| Pre-onset psychiatric poly-comorbidity | Yes | 3 (0.8) |
| No | 379 (99.2) | |
| Post-onset psychiatric comorbidity | Yes | 14 (3.7) |
| No | 368 (96.3) | |
| Post-onset psychiatric poly-comorbidity | Yes | 2 (0.5) |
| No | 380 (99.5) | |
| Pre-onset medical comorbidity | Yes | 63 (16.5) |
| No | 319 (83.5) | |
| Pre-onset medical poly-comorbidity | Yes | 13 (3.4) |
| No | 369 (96.6) | |
| Post-onset medical comorbidity | Yes | 158 (41.4) |
| No | 224 (58.6) | |
| Post-onset medical poly-comorbidity | Yes | 82 (21.5) |
| No | 300 (78.5) | |
| Pre-onset substance misuse | Yes | 80 (20.9) |
| No | 302 (79.1) | |
| Pre-onset poly-substance misuse | Yes | 41 (10.7) |
| No | 341 (89.3) | |
| Post-onset substance misuse | Yes | 86 (22.5) |
| No | 296 (77.5) | |
| Post-onset poly-substance misuse | Yes | 49 (12.8) |
| No | 333 (87.2) | |
| Presence of previous suicide attempts | Yes | 54 (14.1) |
| No | 328 (85.9) | |
| Number of previous suicide attempts | 0.22 (0.67) | |
| Presence of previous hospitalizations | Yes | 362 (94.8) |
| No | 20 (5.2) | |
| Number of previous hospitalizations | 4.60 (4.64) | |
| History of criminal acts | Yes | 44 (11.5) |
| No | 338 (88.5) | |
| LAI antipsychotic treatment | Haloperidol decanoate | 150 (39.3) |
| Zuclopenthixol decanoate | 44 (11.5) | |
| Paliperidone palmitate | 77 (20.2) | |
| Olanzapine pamoate | 22 (5.7) | |
| Aripiprazole | 56 (14.7) | |
| Risperidone | 33 (8.6) | |
| First/Second generation LAI antipsychotic treatment | First generation | 194 (50.8) |
| Second generation | 188 (49.2) | |
| Survival at 12 months | Yes | 272 (71.2) |
| No | 110 (28.8) | |
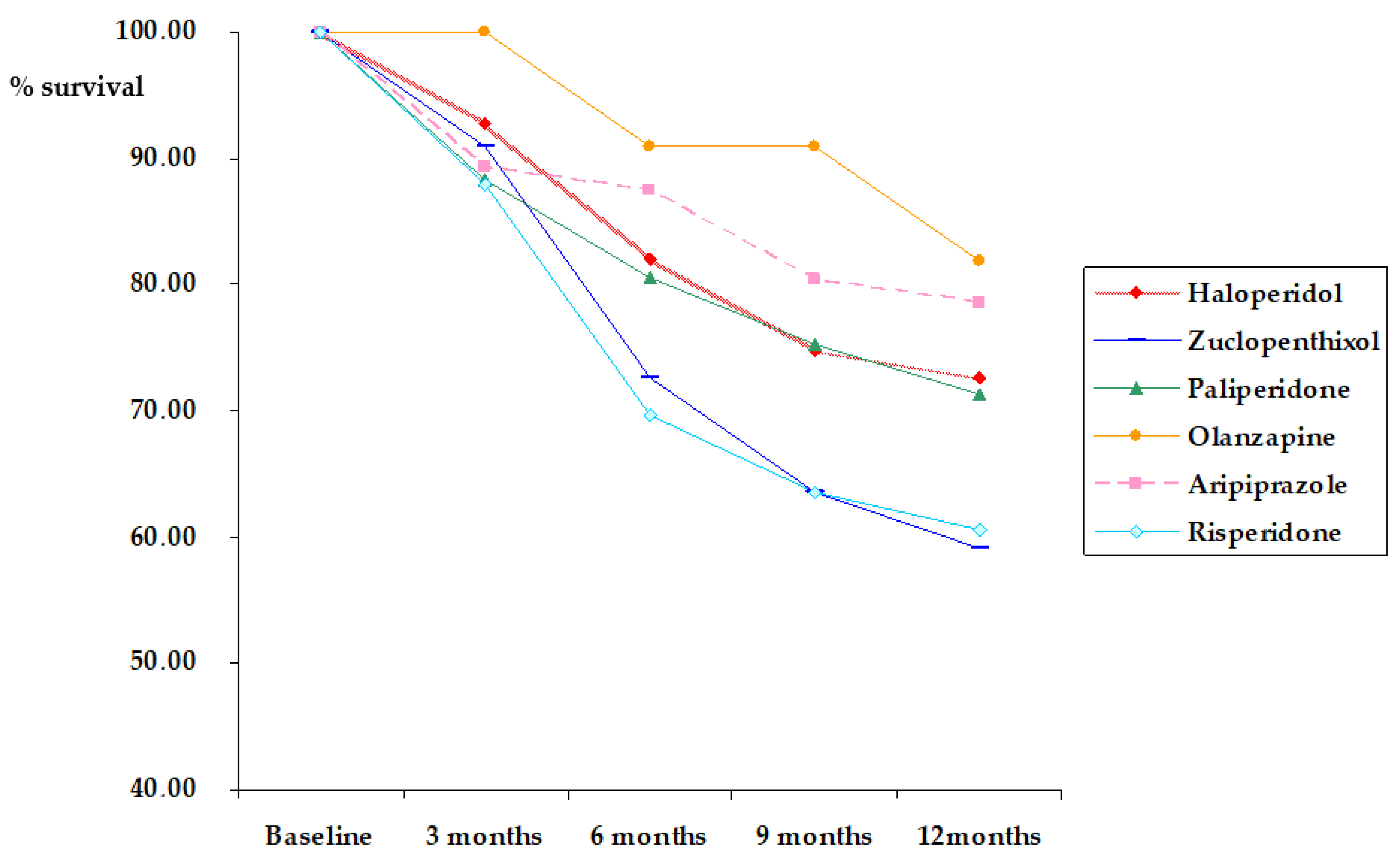
| Months of survival | Haloperidol decanoate | 10.24 (3.14) |
| Zuclopenthixol decanoate | 9.34 (3.66) | |
| Paliperidone palmitate | 10.06 (3.43) | |
| Olanzapine pamoate | 11.36 (1.76) | |
| Aripiprazole | 10.55 (3.16) | |
| Risperidone | 9.30 (3.72) | |
| Total | 10.13 (3.28) | |
| Reason for discontinuation of LAI antipsychotic | No discontinuation | 244 (63.9) |
| Recurrence (including hospitalization) | 20 (5.2) | |
| Side effects | 40 (10.5) | |
| No compliance | 78 (20.4) | |
| Current poly-pharmacotherapy | Yes | 210 (55.0) |
| No | 172 (45.0) | |
| Treatment side effects | Yes | 150 (39.3) |
| No | 232 (60.7) | |
| Presence of multiple side effects | Yes | 35 (9.2) |
| No | 347 (90.8) | |
| Lifetime psychotherapy | Yes | 63 (16.5) |
| No | 319 (83.5) | |
| Type of lifetime psychotherapy | None | 319 (83.5) |
| Psychoeducation/supportive | 40 (10.5) | |
| Cognitive-Behavioral Therapy | 16 (4.2) | |
| Psychodynamic | 7 (1.8) | |
| Current psychotherapy | Yes | 9 (2.4) |
| No | 373 (97.6) | |
| Type of current psychotherapy | None | 373 (97.6) |
| Psychoeducation/supportive | 6 (1.6) | |
| Cognitive-Behavioral Therapy | 2 (0.5) | |
| Psychodynamic | 1 (0.3) | |
| Predictors | B | p | Exp(B) | CI |
|---|---|---|---|---|
| Age | 0.204 | 0.520 | 1.226 | 0.659–2.279 |
| Age at onset | −0.207 | 0.514 | 0.813 | 0.437–1.512 |
| Duration of illness | −0.215 | 0.497 | 0.807 | 0.434–1.499 |
| Duration of untreated illness | 0.026 | 0.200 | 1.027 | 0.986–1.069 |
| Presence of personality disorders (yes/no) | −0.057 | 0.871 | 0.944 | 0.473–1.884 |
| Family history for psychiatric disorders (yes/no) | −0.051 | 0.835 | 0.950 | 0.588–1.536 |
| Work status (employed versus the others) | 0.023 | 0.929 | 1.023 | 0.619–1.691 |
| Marital status (married/in partnership versus the others) | 0.050 | 0.840 | 1.051 | 0.648–1.706 |
| Pre-onset psychiatric comorbidity (yes/no) | 0.191 | 0.549 | 1.210 | 0.648–2.259 |
| Post-onset psychiatric comorbidity (yes/no) | 0.184 | 0.764 | 1.202 | 0.360–4.013 |
| Pre-onset substance use disorders (yes/no) | −0.073 | 0.862 | 0.930 | 0.411–2.105 |
| Post-onset substance use disorders (yes/no) | 0.193 | 0.640 | 1.213 | 0.540–2.724 |
| Pre-onset medical comorbidity (yes/no) | −0.145 | 0.634 | 0.865 | 0.475–1.573 |
| Post-onset medical comorbidity (yes/no) | −0.492 | 0.098 | 0.612 | 0.342–1.095 |
| Diagnosis | NA | 0.532 | NA | NA |
| History of criminal acts (yes/no) | −0.332 | 0.290 | 0.718 | 0.388–1.328 |
| Gender | 0.191 | 0.463 | 0.463 | 0.727–2.014 |
| Multiple family history of psychiatric disorders (yes/no) | −0.037 | 0.921 | 0.964 | 0.462–2.010 |
| Pre-onset multiple substance use disorders (yes/no) | −1.049 | 0.058 | 0.350 | 0.118–1.035 |
| Post-onset multiple substance use disorders (yes/no) | 0.433 | 0.444 | 1.542 | 0.509–4.677 |
| Pre-onset multiple medical comorbidity (yes/no) | −0.061 | 0.929 | 0.941 | 0.244–3.622 |
| Post-onset multiple medical comorbidity (yes/no) | 0.424 | 0.217 | 1.528 | 0.779–2.999 |
| Type of LAI antipsychotic | NA | 0.033 | NA | NA |
| Poly-therapy (yes/no) | 0.128 | 0.556 | 1.137 | 0.743–1.739 |
| Lifetime psychotherapy (yes/no) | −0.404 | 0.158 | 0.668 | 0.381–1.169 |
| Lifetime attempted suicide (yes/no) | −0.370 | 0.288 | 0.691 | 0.349–1.368 |
| Lifetime hospitalizations (yes/no) | −0.108 | 0.812 | 0.897 | 0.369–2.185 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Auxilia, A.M.; Buoli, M.; Caldiroli, A.; Carnevali, G.S.; Tringali, A.; Nava, R.; Clerici, M.; Capuzzi, E. High Rate of Discontinuation during Long-Acting Injectable Antipsychotic Treatment in Patients with Psychotic Disorders. Biomedicines 2023, 11, 314. https://doi.org/10.3390/biomedicines11020314
Auxilia AM, Buoli M, Caldiroli A, Carnevali GS, Tringali A, Nava R, Clerici M, Capuzzi E. High Rate of Discontinuation during Long-Acting Injectable Antipsychotic Treatment in Patients with Psychotic Disorders. Biomedicines. 2023; 11(2):314. https://doi.org/10.3390/biomedicines11020314
Chicago/Turabian StyleAuxilia, Anna Maria, Massimiliano Buoli, Alice Caldiroli, Greta Silvia Carnevali, Agnese Tringali, Roberto Nava, Massimo Clerici, and Enrico Capuzzi. 2023. "High Rate of Discontinuation during Long-Acting Injectable Antipsychotic Treatment in Patients with Psychotic Disorders" Biomedicines 11, no. 2: 314. https://doi.org/10.3390/biomedicines11020314
APA StyleAuxilia, A. M., Buoli, M., Caldiroli, A., Carnevali, G. S., Tringali, A., Nava, R., Clerici, M., & Capuzzi, E. (2023). High Rate of Discontinuation during Long-Acting Injectable Antipsychotic Treatment in Patients with Psychotic Disorders. Biomedicines, 11(2), 314. https://doi.org/10.3390/biomedicines11020314