Management Strategies in Arrhythmogenic Cardiomyopathy across the Spectrum of Ventricular Involvement
Abstract
:1. Introduction
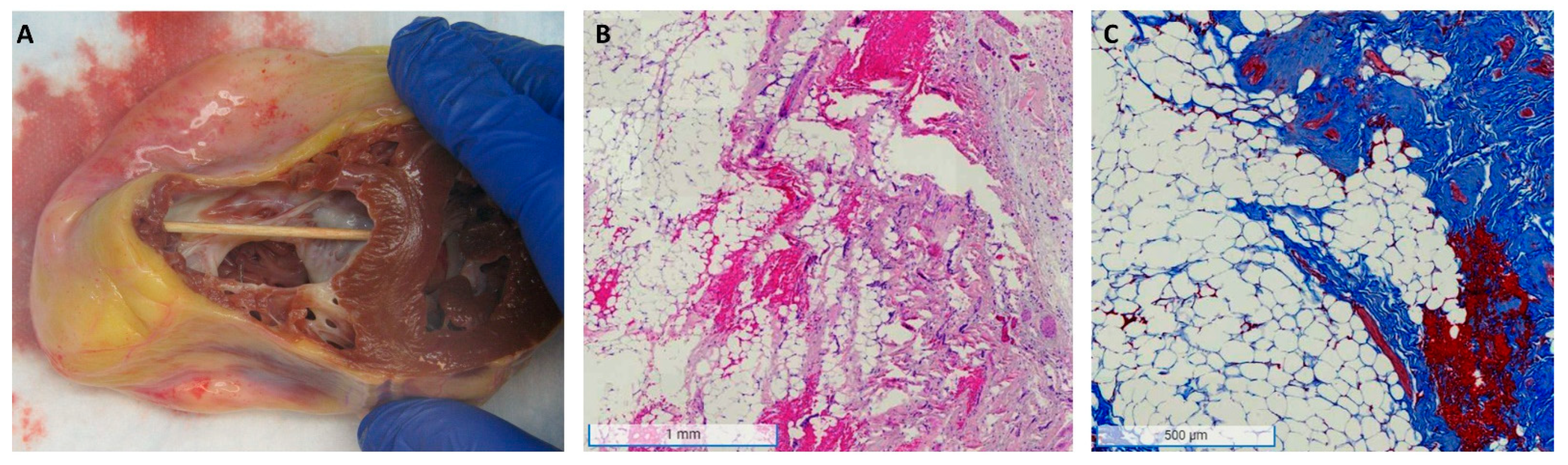
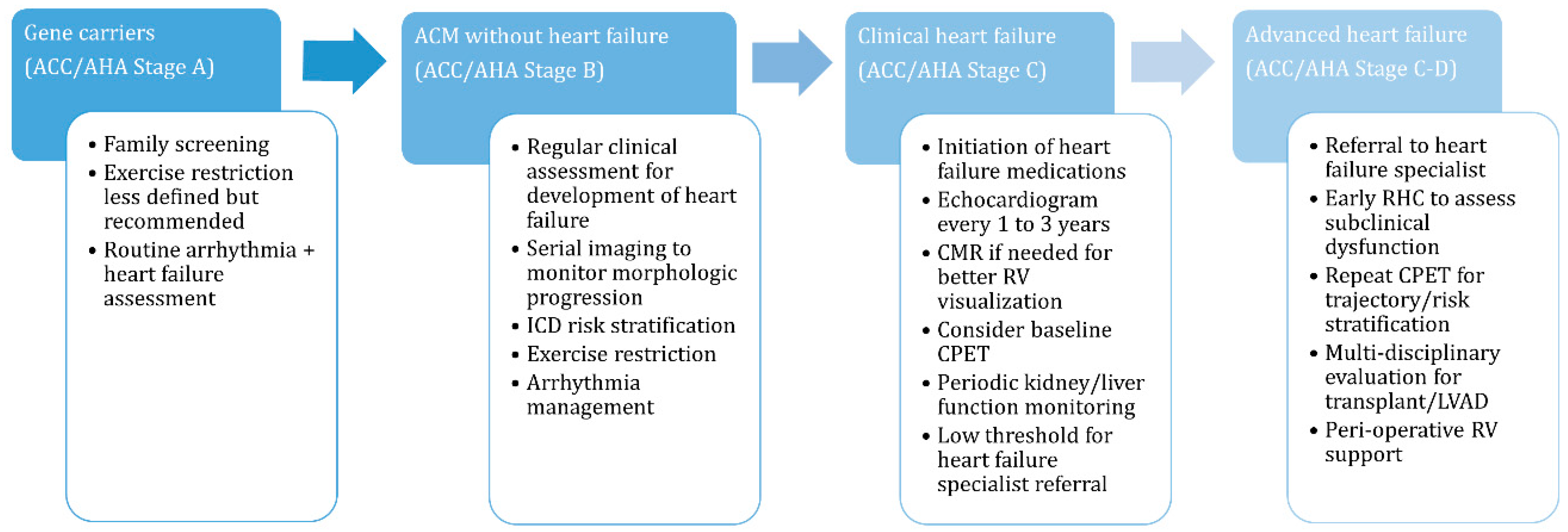
2. Epidemiology and Pathophysiology
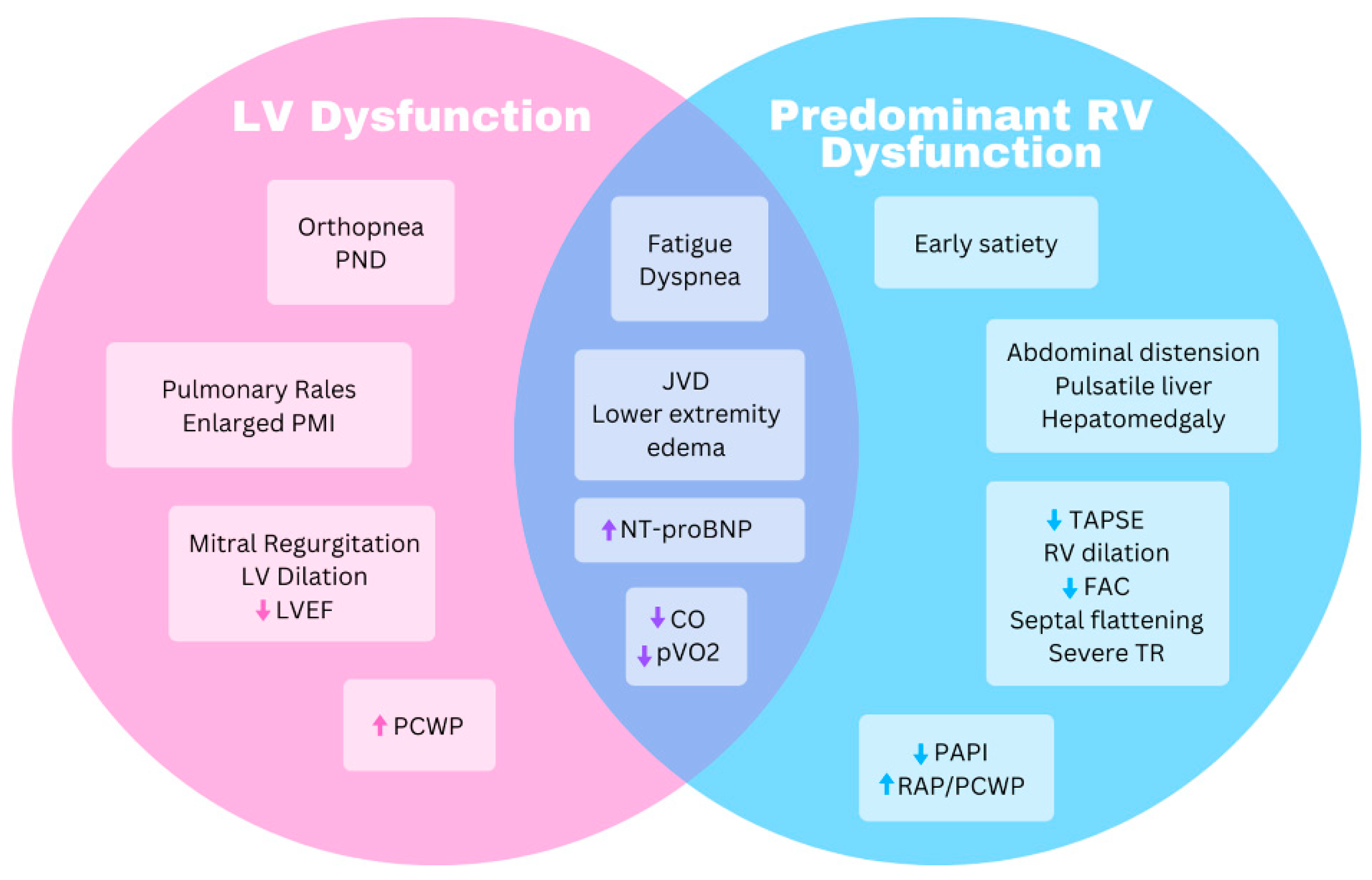
3. Heart Failure Diagnosis and Assessment
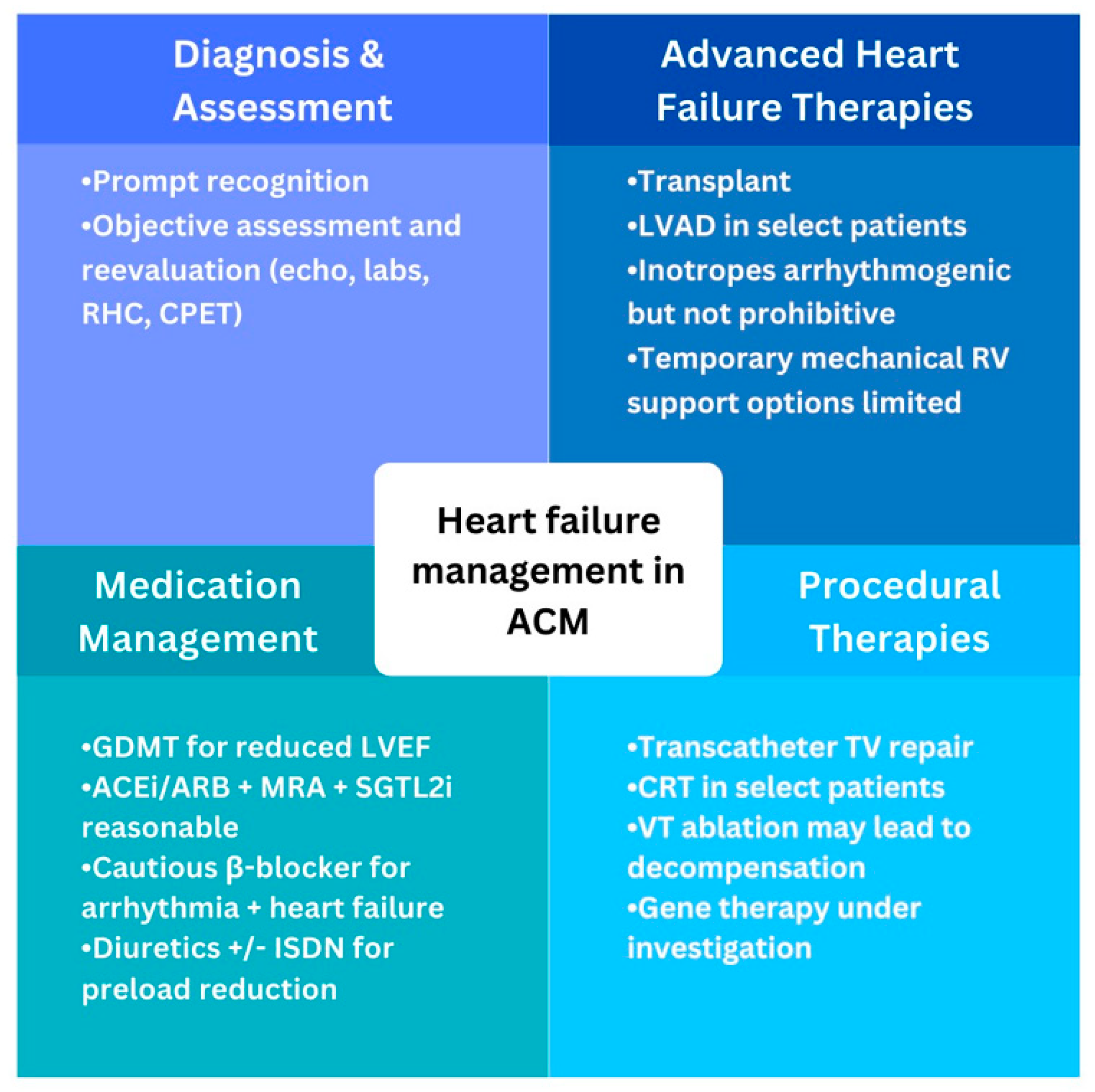
4. Heart Failure Management
4.1. Medical Management
4.2. Procedural Therapies
4.3. Advanced Heart Failure Surgical Therapies
4.4. Emerging Therapies
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| ACEi | angiotensin converting enzyme inhibitor |
| ACM | arrhythmogenic cardiomyopathy |
| ALVC | arrhythmogenic left ventricular cardiomyopathy |
| ARB | angiotensin receptor blocker |
| ARNI | angiotensin receptor neprilysin inhibitor |
| ARVC | arrhythmogenic right ventricular cardiomyopathy |
| βB | beta-blocker |
| CMR | cardiac magnetic resonance |
| CO | cardiac output |
| CPET | cardiopulmonary exercise test |
| CRT | cardiac resynchronization therapy |
| DSG2 | desmoglein-2 |
| DSP | desmoplakin |
| ECMO | extracorporeal membrane oxygenator |
| FAC | fractional area change |
| GDMT | guideline-directed medical therapy |
| ICD | implantable cardioverter defibrillator |
| ISDN | isosorbide dinitrate |
| IVC | inferior vena cava |
| LGE | late gadolinium enhancement |
| LV | left ventricle |
| LVAD | left ventricular assist device |
| LVEF | left ventricle ejection fraction |
| MRA | mineralocorticoid receptor antagonist |
| NT-proBNP | N-terminal prohormone brain natriuretic peptide |
| PAPI | pulmonary artery pulsatility index |
| PCWP | pulmonary capillary wedge pressure |
| PKP2 | plakophilin-2 |
| PMI | point of maximal impulse |
| PND | paroxysmal nocturnal dyspnea |
| pVO2 | peak oxygen uptake |
| RAP | right atrial pressure |
| RER | respiratory exchange ratio |
| RHC | right heart catheterization |
| RV | right ventricle |
| SCD | sudden cardiac death |
| SGTL2i | sodium/glucose cotransporter-2 inhibitor |
| TAPSE | tricuspid annular plane systolic excursion |
| TR | tricuspid regurgitation |
| Ve/VCO2 | ventilation to carbon dioxide production ratio |
References
- Corrado, D.; Basso, C.; Thiene, G.; McKenna, W.J.; Davies, M.J.; Fontaliran, F.; Nava, A.; Silvestri, F.; Blomstrom-Lundqvist, C.; Wlodarska, E.K.; et al. Spectrum of clinicopathologic manifestations of arrhythmogenic right ventricular cardiomyopathy/dysplasia: A multicenter study. J. Am. Coll. Cardiol. 1997, 30, 1512–1520. [Google Scholar] [CrossRef]
- Marcus, F.I.; Fontaine, G.H.; Guiraudon, G.; Frank, R.; Laurenceau, J.L.; Malergue, C. Right ventricular dysplasia: A report of 24 adult cases. In Myocarditis Cardiomyopathy; Springer: Berlin/Heidelberg, Germany, 1983; pp. 81–93. [Google Scholar] [CrossRef]
- Thiene, G.; Nava, A.; Corrado, D.; Rossi, L.; Pennelli, N. Right ventricular cardiomyopathy and sudden death in young people. N. Engl. J. Med. 1982, 65, 384–398. [Google Scholar] [CrossRef]
- Gandjbakhch, E.; Redheuil, A.; Pousset, F.; Charron, P.; Frank, R. Clinical diagnosis, imaging, and genetics of arrhythmogenic right ventricular cardiomyopathy/dysplasia. J. Am. Coll. Cardiol. 2018, 72, 784–804. [Google Scholar] [CrossRef] [PubMed]
- James, C.A.; Syrris, P.; van Tintelen, J.P.; Calkins, H. The role of genetics in cardiovascular disease: Arrhythmogenic cardiomyopathy. Eur. Heart J. 2020, 41, 1393–1400. [Google Scholar] [CrossRef] [PubMed]
- Corrado, D.; Van Tintelen, P.J.; McKenna, W.J.; Hauer, R.N.W.; Anastastakis, A.; Asimaki, A.; Basso, C.; Bauce, B.; Brunckhorst, C.; Bucciarelli-Ducci, C.; et al. International Experts. Arrhythmogenic right ventricular cardiomyopathy: Evaluation of the current diagnostic criteria and differential diagnosis. Eur. Heart J. 2020, 41, 1414–1429. [Google Scholar] [CrossRef] [PubMed]
- Groeneweg, J.A.; van der Zwaag, P.A.; Jongbloed, J.D.; Cox, M.G.; Vreeker, A.; de Boer, R.A.; van der Heijden, J.F.; van Veen, T.A.; McKenna, W.J.; van Tintelen, J.P.; et al. Left-dominant arrhythmogenic cardiomyopathy in a large family: Associated desmosomal or nondesmosomal genotype? Heart Rhythm. 2013, 10, 548–559. [Google Scholar] [CrossRef] [PubMed]
- Saguner, A.M. Arrhythmogenic ventricular cardiomyopathy: A paradigm shift from right to biventricular disease. World J. Cardiol. 2014, 6, 154–174. [Google Scholar] [CrossRef] [PubMed]
- Gilotra, N.A.; Bhonsale, A.; James, C.A.; Te Riele, A.S.J.; Murray, B.; Tichnell, C.; Sawant, A.; Ong, C.S.; Judge, D.P.; Russell, S.D.; et al. Heart failure is common and under-recognized in patients with arrhythmogenic right ventricular cardiomyopathy/dysplasia. Circ. Heart Fail. 2017, 10, e003819. [Google Scholar] [CrossRef] [PubMed]
- Kimura, Y.; Noda, T.; Matsuyama, T.-A.; Otsuka, Y.; Kamakura, T.; Wada, M.; Ishibashi, K.; Inoue, Y.; Miyamoto, K.; Okamura, H.; et al. Heart failure in patients with arrhythmogenic right ventricular cardiomyopathy: What are the risk factors? Int. J. Cardiol. 2017, 241, 288–294. [Google Scholar] [CrossRef]
- Kimura, Y.; Noda, T.; Otsuka, Y.; Wada, M.; Nakajima, I.; Ishibashi, K.; Miyamoto, K.; Okamura, H.; Aiba, T.; Kamakura, S.; et al. Potentially lethal ventricular arrhythmias and heart failure in arrhythmogenic Right Ventricular cardiomyopathy. JACC Clin. Electrophysiol. 2016, 2, 546–555. [Google Scholar] [CrossRef]
- Towbin, J.A.; McKenna, W.J.; Abrams, D.J.; Ackerman, M.J.; Calkins, H.; Darrieux, F.C.; Daubert, J.P.; de Chillou, C.; DePasquale, E.C.; Desai, M.Y.; et al. 2019 HRS expert consensus statement on evaluation, risk stratification, and management of arrhythmogenic cardiomyopathy. Heart Rhythm. 2019, 16, e301–e372. [Google Scholar] [CrossRef]
- Castrichini, M.; Eldemire, R.; Groves, D.W.; Taylor, M.R.; Miyamoto, S.; Mestroni, L. Clinical and genetic features of arrhythmogenic cardiomyopathy: Diagnosis, management and the heart failure perspective. Prog. Pediatr. Cardiol. 2021, 63, 101459. [Google Scholar] [CrossRef]
- Gaine, S.P.; Calkins, H. Antiarrhythmic drug therapy in arrhythmogenic right ventricular cardiomyopathy. Biomedicines 2023, 11, 1213. [Google Scholar] [CrossRef] [PubMed]
- Heidenreich, P.A.; Bozkurt, B.; Aguilar, D.; Allen, L.A.; Byun, J.J.; Colvin, M.M.; Deswal, A.; Drazner, M.H.; Dunlay, S.M.; Evers, L.R.; et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: A report of the american college of cardiology/american heart association joint committee on clinical practice guidelines. J. Am. Coll. Cardiol. 2022, 79, e263–e421. [Google Scholar] [CrossRef] [PubMed]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2023 focused update of the 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2023, 44, 3627–3639. [Google Scholar] [CrossRef]
- Calkins, H. Arrhythmogenic right ventricular dysplasia/cardiomyopathy—Three decades of progress. Circ. J. 2015, 79, 901–913. [Google Scholar] [CrossRef] [PubMed]
- Corrado, D.; Thiene, G. Arrhythmogenic right ventricular cardiomyopathy/dysplasia: Clinical impact of molecular genetic studies. Circulation 2006, 113, 1634–1637. [Google Scholar] [CrossRef] [PubMed]
- Marcus, F.I.; McKenna, W.J.; Sherrill, D.; Basso, C.; Bauce, B.; Bluemke, D.A.; Calkins, H.; Corrado, D.; Cox, M.G.; Daubert, J.P.; et al. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia. Circulation 2010, 121, 1533–1541. [Google Scholar] [CrossRef] [PubMed]
- Groeneweg, J.A.; Bhonsale, A.; James, C.A.; Te Riele, A.S.; Dooijes, D.; Tichnell, C.; Murray, B.; Wiesfeld, A.C.; Sawant, A.C.; Kassamali, B.; et al. Clinical presentation, long-term follow-up, and outcomes of 1001 arrhythmogenic right ventricular dysplasia/cardiomyopathy patients and family members. Circ. Cardiovasc. Genet. 2015, 8, 437–446. [Google Scholar] [CrossRef]
- Bhonsale, A.; Groeneweg, J.A.; James, C.A.; Dooijes, D.; Tichnell, C.; Jongbloed, J.D.H.; Murray, B.; Te Riele, A.S.J.M.; Van Den Berg, M.P.; Bikker, H.; et al. Impact of genotype on clinical course in arrhythmogenic right ventricular dysplasia/cardiomyopathy-associated mutation carriers. Eur. Heart J. 2015, 36, 847–855. [Google Scholar] [CrossRef]
- Gerull, B.; Brodehl, A. Insights into genetics and pathophysiology of arrhythmogenic cardiomyopathy. Curr. Heart Fail. Rep. 2021, 18, 378–390. [Google Scholar] [CrossRef] [PubMed]
- McKoy, G.; Protonotarios, N.; Crosby, A.; Tsatsopoulou, A.; Anastasakis, A.; Coonar, A.; Norman, M.; Baboonian, C.; Jeffery, S.; McKenna, W.J. Identification of a deletion in plakoglobin in arrhythmogenic right ventricular cardiomyopathy with palmoplantar keratoderma and woolly hair (naxos disease). Lancet 2000, 355, 2119–2124. [Google Scholar] [CrossRef]
- Nehme, N.; El Malti, R.; Roux-Buisson, N.; Caignault, J.-R.; Bouvagnet, P. Evidence for genetic heterogeneity in carvajal syndrome. Cell Tissue Res. 2012, 348, 261–264. [Google Scholar] [CrossRef] [PubMed]
- Castelletti, S.; Vischer, A.S.; Syrris, P.; Crotti, L.; Spazzolini, C.; Ghidoni, A.; Parati, G.; Jenkins, S.; Kotta, M.-C.; McKenna, W.J.; et al. Desmoplakin missense and non-missense mutations in arrhythmogenic right ventricular cardiomyopathy: Genotype-phenotype correlation. Int. J. Cardiol. 2017, 249, 268–273. [Google Scholar] [CrossRef]
- Hermida, A.; Fressart, V.; Hidden-Lucet, F.; Donal, E.; Probst, V.; Deharo, J.C.; Chevalier, P.; Klug, D.; Mansencal, N.; Delacretaz, E.; et al. High risk of heart failure associated with desmoglein-2 mutations compared to plakophilin-2 mutations in arrhythmogenic right ventricular cardiomyopathy/dysplasia. Eur. J. Heart Fail. 2019, 21, 792–800. [Google Scholar] [CrossRef] [PubMed]
- Protonotarios, A.; Bariani, R.; Cappelletto, C.; Pavlou, M.; García-García, A.; Cipriani, A.; Protonotarios, I.; Rivas, A.; Wittenberg, R.; Graziosi, M.; et al. Importance of genotype for risk stratification in arrhythmogenic right ventricular cardiomyopathy using the 2019 ARVC risk calculator by guest on 12 August 2023. Eur. Heart J. 2022, 43, 3053. [Google Scholar] [CrossRef] [PubMed]
- Smith, E.D.; Lakdawala, N.K.; Papoutsidakis, N.; Aubert, G.; Mazzanti, A.; McCanta, A.C.; Agarwal, P.P.; Arscott, P.; Dellefave-Castillo, L.M.; Vorovich, E.E.; et al. Desmoplakin cardiomyopathy, a fibrotic and inflammatory form of cardiomyopathy distinct from typical dilated or arrhythmogenic right ventricular cardiomyopathy. Circulation 2020, 141, 1872–1884. [Google Scholar] [CrossRef]
- Ammirati, E.; Raimondi, F.; Piriou, N.; Infirri, L.S.; Mohiddin, S.A.; Mazzanti, A.; Shenoy, C.; Cavallari, U.A.; Imazio, M.; Aquaro, G.D.; et al. Acute myocarditis associated with desmosomal gene variants. JACC Heart Fail. 2022, 10, 714–727. [Google Scholar] [CrossRef]
- Kelly, M.A.; Caleshu, C.; Morales, A.; Buchan, J.; Wolf, Z.; Harrison, S.M.; Cook, S.; Dillon, M.W.; Garcia, J.; Haverfield, E.; et al. Adaptation and validation of the ACMG/AMP variant classification framework for MYH7-associated inherited cardiomyopathies: Recommendations by ClinGen’s inherited cardiomyopathy expert panel. Anesth. Analg. 2018, 20, 351–359. [Google Scholar] [CrossRef]
- Richards, S.; Aziz, N.; Bale, S.; Bick, D.; Das, S.; Gastier-Foster, J.; Grody, W.W.; Hegde, M.; Lyon, E.; Spector, E.; et al. Standards and guidelines for the interpretation of sequence variants: A joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Anesth. Analg. 2015, 17, 405–424. [Google Scholar] [CrossRef]
- Wilde, A.A.M.; Semsarian, C.; Márquez, M.F.; Shamloo, A.S.; Ackerman, M.J.; Ashley, E.A.; Eduardo, B.S.; Barajas-Martinez, H.; Behr, E.R.; Bezzina, C.R.; et al. European Heart Rhythm Association (EHRA)/Heart Rhythm Society (HRS)/Asia Pacific Heart Rhythm Society (APHRS)/Latin American Heart Rhythm Society (LAHRS) Expert Consensus Statement on the state of genetic testing for cardiac diseases. J. Arrhythmia 2022, 38, 491–553. [Google Scholar] [CrossRef] [PubMed]
- Campuzano, O.; Sarquella-Brugada, G.; Fernandez-Falgueras, A.; Coll, M.; Iglesias, A.; Ferrer-Costa, C.; Cesar, S.; Arbelo, E.; García-Álvarez, A.; Jordà, P.; et al. Reanalysis and reclassification of rare genetic variants associated with inherited arrhythmogenic syndromes. EBioMedicine 2020, 54, 102732. [Google Scholar] [CrossRef] [PubMed]
- Barrios, E.M.; Brugada, G.S.; Gomez, J.C.; Diaz, S.C.; Ccasani, F.C.; Greco, A.; Fiol, V.; Cerralbo, P.; Terradellas, J.B.; Larrea, O.C. Update on rare variants in inherited arrhythmogenic syndromes: When to reclassify? EP Eur. 2023, 25. [Google Scholar] [CrossRef]
- Engel, M.; Shiel, E.; Chelko, S.P. Basic and translational mechanisms in inflammatory arrhythmogenic cardiomyopathy. Int. J. Cardiol. 2023, 131602. [Google Scholar] [CrossRef] [PubMed]
- Boogerd, C.J.; Lacraz, G.P.A.; Vértesy, Á.; van Kampen, S.J.; Perini, I.; de Ruiter, H.; Versteeg, D.; Brodehl, A.; van der Kraak, P.; Giacca, M.; et al. Spatial transcriptomics unveils ZBTB11 as a regulator of cardiomyocyte degeneration in arrhythmogenic cardiomyopathy. Cardiovasc. Res. 2022, 119, 477–491. [Google Scholar] [CrossRef] [PubMed]
- Dalal, D.; Nasir, K.; Bomma, C.; Prakasa, K.; Tandri, H.; Piccini, J.; Roguin, A.; Tichnell, C.; James, C.; Russell, S.D.; et al. Arrhythmogenic right ventricular dysplasia: A united states experience. Circulation 2005, 112, 3823–3832. [Google Scholar] [CrossRef]
- Scheel, P.J.; Giuliano, K.; Tichnell, C.; James, C.; Murray, B.; Tandri, H.; Carter, D.; Fehr, T.; Umapathi, P.; Vaishnav, J.; et al. Heart transplantation strategies in arrhythmogenic right ventricular cardiomyopathy: A tertiary ARVC centre experience. ESC Heart Fail. 2021, 9, 1008–1017. [Google Scholar] [CrossRef]
- Bozkurt, B.; Coats, A.J.; Tsutsui, H.; Abdelhamid, M.; Adamopoulos, S.; Albert, N.; Anker, S.D.; Atherton, J.; Böhm, M.; Butler, J.; et al. Universal definition and classification of heart failure. J. Card. Fail. 2021, 27, 387–413. [Google Scholar] [CrossRef]
- James, C.A.; Bhonsale, A.; Tichnell, C.; Murray, B.; Russell, S.D.; Tandri, H.; Tedford, R.J.; Judge, D.P.; Calkins, H. Exercise increases age-related penetrance and arrhythmic risk in arrhythmogenic right ventricular dysplasia/cardiomyopathy–associated desmosomal mutation carriers. J. Am. Coll. Cardiol. 2013, 62, 1290–1297. [Google Scholar] [CrossRef]
- Borowiec, K.; Woźniak, O.; Wróbel, A.; Śmigielski, W.; Skrzypczyńska-Banasik, U.; Kowalik, E.; Lutyńska, A.; Hoffman, P.; Biernacka, E.K. NT-proBNP is superior to novel plasma biomarkers for predicting adverse outcome in arrhythmogenic right ventricular cardiomyopathy. Pol. Arch. Intern. Med. 2023, 133, 16443. [Google Scholar] [CrossRef]
- Cheng, H.; Lu, M.; Hou, C.; Chen, X.; Wang, J.; Yin, G.; Chu, J.; Zhang, S.; Prasad, S.K.; Pu, J.; et al. Relation between n-terminal pro-brain natriuretic peptide and cardiac remodeling and function assessed by cardiovascular magnetic resonance imaging in patients with arrhythmogenic right ventricular cardiomyopathy. Am. J. Cardiol. 2015, 115, 341–347. [Google Scholar] [CrossRef] [PubMed]
- Akdis, D.; Saguner, A.M.; Shah, K.; Wei, C.; Medeiros-Domingo, A.; von Eckardstein, A.; Lüscher, T.F.; Brunckhorst, C.; Chen, H.V.; Duru, F. Sex hormones affect outcome in arrhythmogenic right ventricular cardiomyopathy/dysplasia: From a stem cell derived cardiomyocyte-based model to clinical biomarkers of disease outcome. Eur. Heart J. 2017, 38, 1498–1508. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Yang, F.; Chen, X.; Rao, M.; Zhang, N.-N.; Chen, K.; Deng, H.; Song, J.-P.; Hu, S.-S. Comprehensive myocardial proteogenomics profiling reveals C/EBPα as the key factor in the lipid storage of ARVC. J. Proteome Res. 2017, 16, 2863–2876. [Google Scholar] [CrossRef] [PubMed]
- Ren, J.; Chen, L.; Chen, X.; Zhang, N.; Sun, X.; Song, J. Acylation-stimulating protein and heart failure progression in arrhythmogenic right ventricular cardiomyopathy. ESC Heart Fail. 2022, 10, 492–501. [Google Scholar] [CrossRef] [PubMed]
- Qasem, M.; Utomi, V.; George, K.; Somauroo, J.; Zaidi, A.; Forsythe, L.; Bhattacharrya, S.; Lloyd, G.; Rana, B.; Ring, L.; et al. A meta-analysis for the echocardiographic assessment of right ventricular structure and function in ARVC: A study by the research and audit committee of the british society of echocardiography. Echo Res. Pract. 2016, 3, 95–104. [Google Scholar] [CrossRef] [PubMed]
- Pinamonti, B.; Dragos, A.M.; Pyxaras, S.A.; Merlo, M.; Pivetta, A.; Barbati, G.; Di Lenarda, A.; Morgera, T.; Mestroni, L.; Sinagra, G. Prognostic predictors in arrhythmogenic right ventricular cardiomyopathy: Results from a 10-year registry. Eur. Heart J. 2011, 32, 1105–1113. [Google Scholar] [CrossRef] [PubMed]
- Saguner, A.M.; Vecchiati, A.; Baldinger, S.H.; Rüeger, S.; Medeiros-Domingo, A.; Mueller-Burri, A.S.; Haegeli, L.M.; Biaggi, P.; Manka, R.; Lüscher, T.F.; et al. Different prognostic value of functional right ventricular parameters in arrhythmogenic right ventricular cardiomyopathy/dysplasia. Circ. Cardiovasc. Imaging 2014, 7, 230–239. [Google Scholar] [CrossRef]
- Lemola, K.; Brunckhorst, C.; Helfenstein, U.; Oechslin, E.; Jenni, R.; Duru, F. Predictors of adverse outcome in patients with arrhythmogenic right ventricular dysplasia/cardiomyopathy: Long term experience of a tertiary care centre. Heart 2005, 91, 1167–1172. [Google Scholar] [CrossRef]
- Malik, N.; Mukherjee, M.; Wu, K.C.; Zimmerman, S.L.; Zhan, J.; Calkins, H.; James, C.A.; Gilotra, N.A.; Sheikh, F.H.; Tandri, H.; et al. Multimodality imaging in arrhythmogenic right ventricular cardiomyopathy. Circ. Cardiovasc. Imaging 2022, 15, 106–121. [Google Scholar] [CrossRef]
- Mast, T.P.; James, C.A.; Calkins, H.; Teske, A.J.; Tichnell, C.; Murray, B.; Loh, P.; Russell, S.D.; Velthuis, B.K.; Judge, D.P.; et al. Evaluation of structural progression in arrhythmogenic right ventricular dysplasia/cardiomyopathy. JAMA Cardiol. 2017, 2, 293–302. [Google Scholar] [CrossRef]
- Hsu, S.; Fang, J.C.; Borlaug, B.A. Hemodynamics for the heart failure clinician: A state-of-the-art review. J. Card. Fail. 2021, 28, 133–148. [Google Scholar] [CrossRef]
- Malhotra, R.; Bakken, K.; D’elia, E.; Lewis, G.D. Cardiopulmonary exercise testing in heart failure. JACC Heart Fail. 2016, 4, 607–616. [Google Scholar] [CrossRef]
- Corrà, U.; Piepoli, M.F.; Adamopoulos, S.; Agostoni, P.; Coats, A.J.; Conraads, V.; Lambrinou, E.; Pieske, B.; Piotrowicz, E.; Schmid, J.-P.; et al. Cardiopulmonary exercise testing in systolic heart failure in 2014: The evolving prognostic role. Eur. J. Heart Fail. 2014, 16, 929–941. [Google Scholar] [CrossRef] [PubMed]
- Guazzi, M.; Raimondo, R.; Vicenzi, M.; Arena, R.; Proserpio, C.; Braga, S.S.; Pedretti, R. Exercise oscillatory ventilation may predict sudden cardiac death in heart failure patients. J. Am. Coll. Cardiol. 2007, 50, 299–308. [Google Scholar] [CrossRef]
- Scheel, P.J.; Florido, R.; Hsu, S.; Murray, B.; Tichnell, C.; James, C.; Judge, D.P.; Russell, S.D.; Tedford, R.J.; Calkins, H.; et al. Safety and utility of cardiopulmonary exercise testing in arrhythmogenic right ventricular cardiomyopathy/dysplasia. J. Card. Fail. 2018, 24, S50–S51. [Google Scholar] [CrossRef]
- Tu, B.; Wu, L.; Zheng, L.; Liu, S.; Sheng, L.; Liu, L.; Zhu, Z.; Yao, Y. Angiotensin-converting enzyme inhibitors/angiotensin receptor blockers: Anti-arrhythmic drug for arrhythmogenic right ventricular cardiomyopathy. Front. Cardiovasc. Med. 2021, 8, 769138. [Google Scholar] [CrossRef] [PubMed]
- Domínguez, F.; Lalaguna, L.; López-Olañeta, M.; Villalba-Orero, M.; Padrón-Barthe, L.; Román, M.; Bello-Arroyo, E.; Briceño, A.; Gonzalez-Lopez, E.; Segovia-Cubero, J.; et al. Early preventive treatment with enalapril improves cardiac function and delays mortality in mice with arrhythmogenic right ventricular cardiomyopathy type 5. Circ. Heart Fail. 2021, 14, e007616. [Google Scholar] [CrossRef]
- Fabritz, L.; Hoogendijk, M.G.; Scicluna, B.P.; van Amersfoorth, S.C.; Fortmueller, L.; Wolf, S.; Laakmann, S.; Kreienkamp, N.; Piccini, I.; Breithardt, G.; et al. Load-reducing therapy prevents development of arrhythmogenic right ventricular cardiomyopathy in plakoglobin-deficient mice. J. Am. Coll. Cardiol. 2011, 57, 740–750. [Google Scholar] [CrossRef]
- Mentz, R.J.; Anstrom, K.J.; Eisenstein, E.L.; Sapp, S.; Greene, S.J.; Morgan, S.; Testani, J.M.; Harrington, A.H.; Sachdev, V.; Ketema, F.; et al. Effect of torsemide vs. furosemide after discharge on all-cause mortality in patients hospitalized with heart failure: The TRANSFORM-HF randomized clinical trial. JAMA 2023, 329, 214–223. [Google Scholar] [CrossRef]
- Sorajja, P.; Whisenant, B.; Hamid, N.; Naik, H.; Makkar, R.; Tadros, P.; Price, M.J.; Singh, G.; Fam, N.; Kar, S.; et al. Transcatheter repair for patients with tricuspid regurgitation. N. Engl. J. Med. 2023, 388, 1833–1842. [Google Scholar] [CrossRef]
- Abraham, W.T.; Stevenson, L.W.; Bourge, R.C.; Lindenfeld, J.A.; Bauman, J.G.; Adamson, P.B.; CHAMPION Trial Study Group. Sustained efficacy of pulmonary artery pressure to guide adjustment of chronic heart failure therapy: Complete follow-up results from the CHAMPION randomised trial. Lancet 2016, 387, 453–461. [Google Scholar] [CrossRef] [PubMed]
- Baumwol, J. “I Need Help”—A mnemonic to aid timely referral in advanced heart failure. J. Heart Lung Transplant. 2017, 36, 593–594. [Google Scholar] [CrossRef] [PubMed]
- Giuliano, K.; Scheel, P.; Etchill, E.; Fraser, C.D.; Suarez-Pierre, A.; Hsu, S.; Wittstein, I.S.; Kasper, E.K.; Florido, R.; Tandri, H.; et al. Heart transplantation outcomes in arrhythmogenic right ventricular cardiomyopathy: A contemporary national analysis. ESC Heart Fail. 2022, 9, 988–997. [Google Scholar] [CrossRef] [PubMed]
- Tedford, R.J.; James, C.; Judge, D.P.; Tichnell, C.; Murray, B.; Bhonsale, A.; Philips, B.; Abraham, T.; Dalal, D.; Halushka, M.K.; et al. Cardiac transplantation in arrhythmogenic right ventricular dysplasia/cardiomyopathy. J. Am. Coll. Cardiol. 2012, 59, 289–290. [Google Scholar] [CrossRef] [PubMed]
- Lewsey, S.C.; Sharma, K.; Kilic, A.; Halushka, M.K.; Vaishnav, J.; Wittstein, I.S.; Tandri, H.; Calkins, H.; James, C.A.; Gilotra, N.A. Dual-organ transplantation in a Woman with right ventricular failure secondary to arrhythmogenic Right Ventricular cardiomyopathy. JACC Case Rep. 2020, 2, 59–63. [Google Scholar] [CrossRef] [PubMed]
- Chelko, S.P.; Asimaki, A.; Andersen, P.; Bedja, D.; Amat-Alarcon, N.; DeMazumder, D.; Jasti, R.; MacRae, C.A.; Leber, R.; Kleber, A.G.; et al. Central role for GSK3β in the pathogenesis of arrhythmogenic cardiomyopathy. J. Clin. Investig. 2016, 1, e85923. [Google Scholar] [CrossRef]
- Chelko, S.; Asimaki, A.; Lowenthal, J.; Bueno-Beti, C.; Bedja, D.; Scalco, A.; Amat-Alarcon, N.; Andersen, P.; Judge, D.P.; Tung, L.; et al. Therapeutic modulation of the immune response in arrhythmogenic cardiomyopathy. Circulation 2019, 140, 1491–1505. [Google Scholar] [CrossRef]
- Reisqs, J.; Moreau, A.; Charrabi, A.; Sleiman, Y.; Meli, A.C.; Millat, G.; Briand, V.; Beauverger, P.; Richard, S.; Chevalier, P. The PPARγ pathway determines electrophysiological remodelling and arrhythmia risks in DSC2 arrhythmogenic cardiomyopathy. Clin. Transl. Med. 2022, 12, e748. [Google Scholar] [CrossRef]
- Qiu, Z.; Zhao, Y.; Tao, T.; Guo, W.; Liu, R.; Huang, J.; Xu, G. Activation of PPARα Ameliorates Cardiac Fibrosis in Dsg2-Deficient arrhythmogenic cardiomyopathy. Cells 2022, 11, 3184. [Google Scholar] [CrossRef]
- Shiba, M.; Higo, S.; Kondo, T.; Li, J.; Liu, L.; Ikeda, Y.; Kohama, Y.; Kameda, S.; Tabata, T.; Inoue, H.; et al. Phenotypic recapitulation and correction of desmoglein-2-deficient cardiomyopathy using human-induced pluripotent stem cell-derived cardiomyocytes. Hum. Mol. Genet. 2021, 30, 1384–1397. [Google Scholar] [CrossRef]
- Romeo, F.J.; Mavropoulos, S.A.; Ishikawa, K. Progress in clinical gene therapy for cardiac disorders. Mol. Diagn. Ther. 2023, 27, 179–191. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maniar, Y.; Gilotra, N.A.; Scheel, P.J., III. Management Strategies in Arrhythmogenic Cardiomyopathy across the Spectrum of Ventricular Involvement. Biomedicines 2023, 11, 3259. https://doi.org/10.3390/biomedicines11123259
Maniar Y, Gilotra NA, Scheel PJ III. Management Strategies in Arrhythmogenic Cardiomyopathy across the Spectrum of Ventricular Involvement. Biomedicines. 2023; 11(12):3259. https://doi.org/10.3390/biomedicines11123259
Chicago/Turabian StyleManiar, Yash, Nisha A. Gilotra, and Paul J. Scheel, III. 2023. "Management Strategies in Arrhythmogenic Cardiomyopathy across the Spectrum of Ventricular Involvement" Biomedicines 11, no. 12: 3259. https://doi.org/10.3390/biomedicines11123259
APA StyleManiar, Y., Gilotra, N. A., & Scheel, P. J., III. (2023). Management Strategies in Arrhythmogenic Cardiomyopathy across the Spectrum of Ventricular Involvement. Biomedicines, 11(12), 3259. https://doi.org/10.3390/biomedicines11123259





