Landscape of Adrenal Tumours in Patients with Congenital Adrenal Hyperplasia
Abstract
1. Introduction
Aim
2. Material and Methods
3. Results
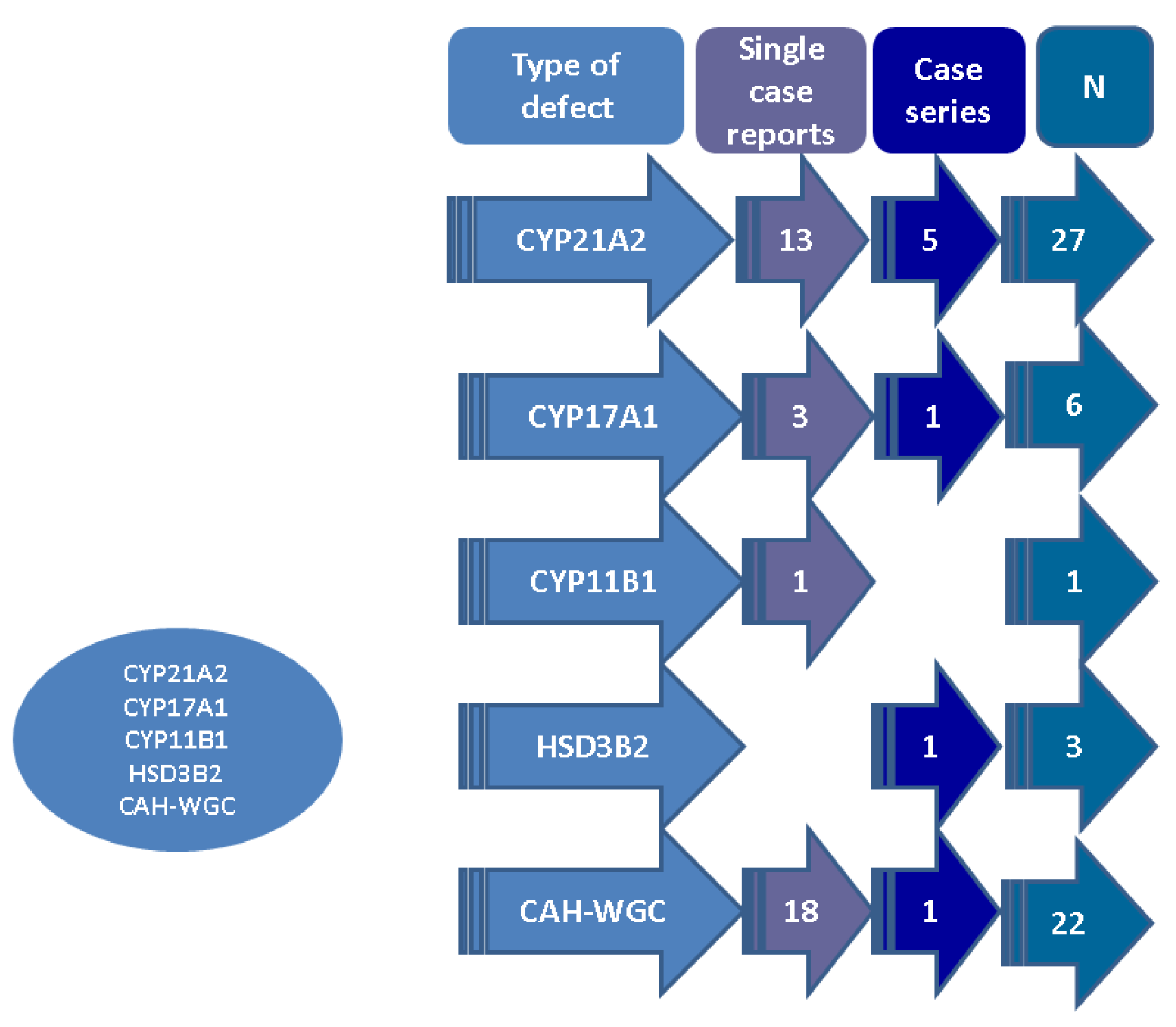
3.1. Case-Based Analysis of Synchronous CAH and Adrenal Tumours
3.1.1. CYP21A2 Deficiency
3.1.1.1. Characteristics of the Patients
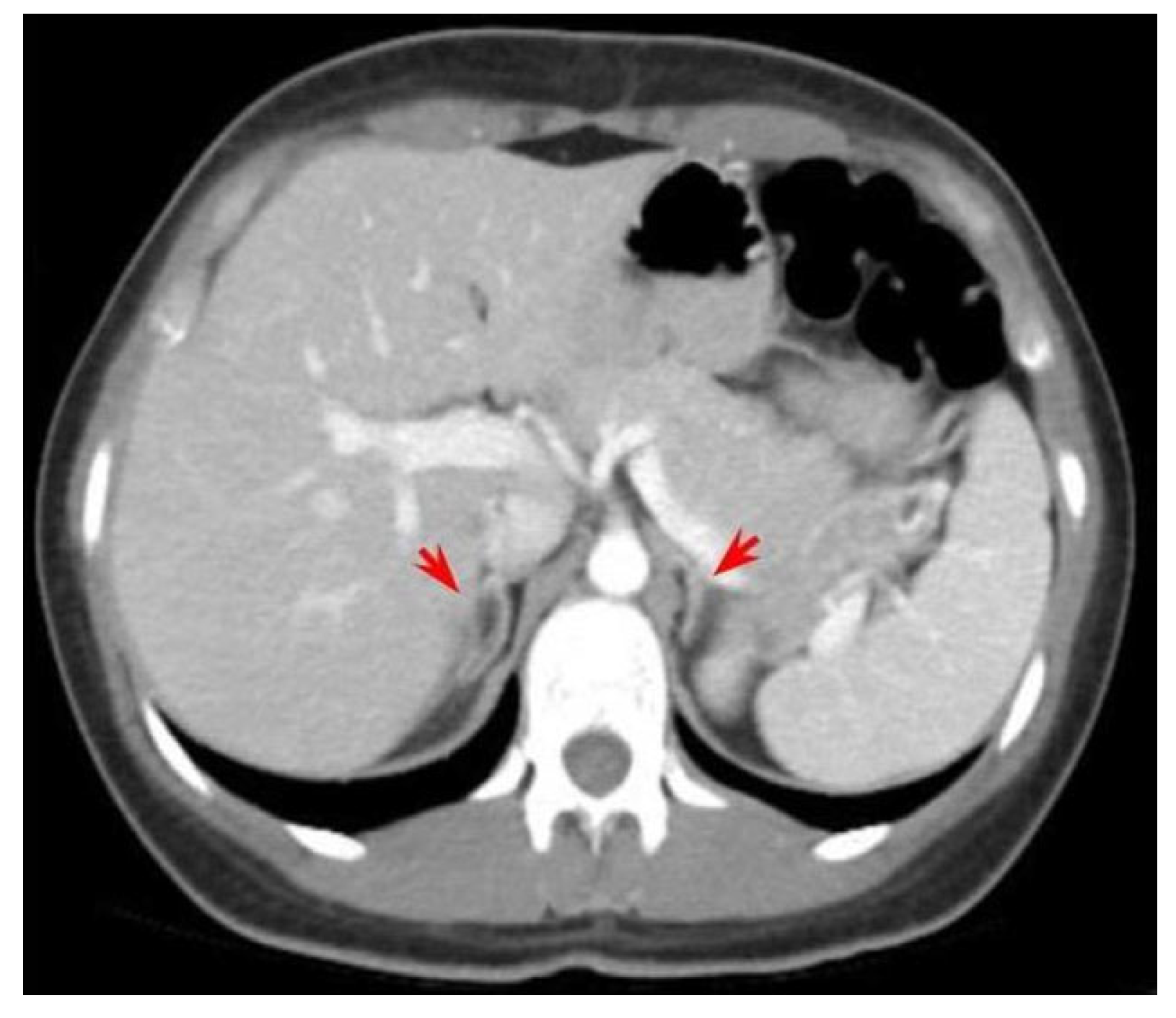
3.1.1.2. Features of the Adrenal Tumours/Masses in Patients with CYP21A2 Deficiency
3.1.1.3. Management and Outcome of the Adrenal Tumours/Masses in Patients with CYP21A2 Deficiency
3.1.1.4. The Analysis of CAH (Disease) Control in Relationship with Tumour Status
3.1.2. CYP17A1 Deficiency
3.1.3. CYP11B1 Deficiency
3.1.4. HSD3B2 Deficiency
3.1.5. Adrenal Tumours in Patients Diagnosed with CAH without a Genetic Confirmation
3.2. Prevalence Studies on CAH and Adrenal Tumours
4. Discussion
4.1. From Case-Sample Analysis to Prevalence Studies
4.2. Histological Profile of CAH-Associated Adrenal Tumours
4.3. A Matter of Surgery or Surgery Matters
4.4. Limits of the Topic and Further Expansion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ACTH | Adrenocorticotropic Hormone |
| CAH | congenital adrenal hyperplasia |
| CYP21A2 | 21-hydroxylase |
| CYP17A1 | 17alpha-hydroxylase/17,20-lyase |
| CYP11B1 | 11-beta hydroxylase |
| HSD3B2 | 3-beta-hydroxysteroid dehydrogenase type II |
| CI | confidence interval |
| NC | non-classical |
| SV | simple virilizing |
| OR | odds ratio |
| SW | salt-wasting |
References
- Claahsen-van der Grinten, H.L.; Speiser, P.W.; Ahmed, S.F.; Arlt, W.; Auchus, R.J.; Falhammar, H.; Flück, C.E.; Guasti, L.; Huebner, A.; Kortmann, B.B.M.; et al. Congenital Adrenal Hyperplasia-Current Insights in Pathophysiology, Diagnostics, and Management. Endocr. Rev. 2022, 43, 91–159. [Google Scholar] [CrossRef] [PubMed]
- Auer, M.K.; Nordenström, A.; Lajic, S.; Reisch, N. Congenital adrenal hyperplasia. Lancet 2023, 401, 227–244. [Google Scholar] [CrossRef] [PubMed]
- Witchel, S.F. Congenital Adrenal Hyperplasia. J. Pediatr. Adolesc. Gynecol. 2017, 30, 520–534. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, B.; Marques, C.J.; Santos-Silva, R.; Fontoura, M.; Carvalho, D.; Carvalho, F. Congenital Adrenal Hyperplasia Due to 21-Hydroxylase Deficiency: An Update on Genetic Analysis of CYP21A2 Gene. Exp. Clin. Endocrinol. Diabetes 2021, 129, 477–481. [Google Scholar] [CrossRef] [PubMed]
- Pignatelli, D.; Carvalho, B.L.; Palmeiro, A.; Barros, A.; Guerreiro, S.G.; Macut, D. The Complexities in Genotyping of Congenital Adrenal Hyperplasia: 21-Hydroxylase Deficiency. Front. Endocrinol. 2019, 10, 432. [Google Scholar] [CrossRef] [PubMed]
- Parajes, S.; Quinteiro, C.; Domínguez, F.; Loidi, L. High frequency of copy number variations and sequence variants at CYP21A2 locus: Implication for the genetic diagnosis of 21-hydroxylase deficiency. PLoS ONE 2008, 3, e2138. [Google Scholar] [CrossRef] [PubMed]
- Parajes, S.; Quinterio, C.; Domínguez, F.; Loidi, L. A simple and robust quantitative PCR assay to determine CYP21A2 gene dose in the diagnosis of 21-hydroxylase deficiency. Clin. Chem. 2007, 53, 1577–1584. [Google Scholar] [CrossRef] [PubMed]
- Nordenström, A.; Lajic, S.; Falhammar, H. Long-Term Outcomes of Congenital Adrenal Hyperplasia. Endocrinol. Metab. 2022, 37, 587–598. [Google Scholar] [CrossRef]
- Auchus, R.J. The uncommon forms of congenital adrenal hyperplasia. Curr. Opin. Endocrinol. Diabetes Obes. 2022, 29, 263–270. [Google Scholar] [CrossRef]
- Asirvatham, A.R.; Balachandran, K.; Jerome, P.; Venkatesan, V.; Koshy, T.; Mahadevan, S. Clinical, biochemical and genetic characteristics of children with congenital adrenal hyperplasia due to 17α-hydroxylase deficiency. J. Pediatr. Endocrinol. Metab. 2020, 33, 1051–1056. [Google Scholar] [CrossRef]
- Krone, N.; Arlt, W. Genetics of congenital adrenal hyperplasia. Best Pract. Res. Clin. Endocrinol. Metab. 2009, 23, 181–192. [Google Scholar] [CrossRef] [PubMed]
- Uslar, T.; Olmos, R.; Martínez-Aguayo, A.; Baudrand, R. Clinical Update on Congenital Adrenal Hyperplasia: Recommendations from a Multidisciplinary Adrenal Program. J. Clin. Med. 2023, 12, 3128. [Google Scholar] [CrossRef] [PubMed]
- Speiser, P.W.; Azziz, R.; Baskin, L.S.; Ghizzoni, L.; Hensle, T.W.; Merke, D.P.; Meyer-Bahlburg, H.F.; Miller, W.L.; Montori, V.M.; Oberfield, S.E.; et al. Congenital adrenal hyperplasia due to steroid 21-hydroxylase deficiency: An Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 2010, 95, 4133–4160. [Google Scholar] [CrossRef] [PubMed]
- Arriba, M.; Ezquieta, B. Molecular Diagnosis of Steroid 21-Hydroxylase Deficiency: A Practical Approach. Front. Endocrinol. 2022, 13, 834549. [Google Scholar] [CrossRef] [PubMed]
- Podgórski, R.; Aebisher, D.; Stompor, M.; Podgórska, D.; Mazur, A. Congenital adrenal hyperplasia: Clinical symptoms and diagnostic methods. Acta Biochim. Pol. 2018, 65, 25–33. [Google Scholar] [CrossRef] [PubMed]
- Török, D. Congenital Adrenal Hyperplasia. Exp. Suppl. 2019, 111, 245–260. [Google Scholar] [CrossRef] [PubMed]
- Therrell, B.L.; Padilla, C.D.; Loeber, J.G.; Kneisser, I.; Saadallah, A.; Borrajo, G.J.; Adams, J. Current status of newborn screening worldwide: 2015. Semin. Perinatol. 2015, 39, 171–187. [Google Scholar] [CrossRef]
- Van der Linde, A.A.A.; Schönbeck, Y.; van der Kamp, H.J.; van den Akker, E.L.T.; van Albada, M.E.; Boelen, A.; Finken, M.J.J.; Hannema, S.E.; Hoorweg-Nijman, G.; Odink, R.J.; et al. Evaluation of the Dutch neonatal screening for congenital adrenal hyperplasia. Arch. Dis. Child. 2019, 104, 653–657. [Google Scholar] [CrossRef]
- Frasier, S.D.; Thorneycroft, I.H.; Weiss, B.A.; Horton, R. Letter: Elevated amniotic fluid concentration of 17 alpha-hydroxyprogesterone in congenital adrenal hyperplasia. J. Pediatr. 1975, 86, 310–312. [Google Scholar] [CrossRef]
- New, M.I.; Tong, Y.K.; Yuen, T.; Jiang, P.; Pina, C.; Chan, K.C.; Khattab, A.; Liao, G.J.; Yau, M.; Kim, S.M.; et al. Noninvasive prenatal diagnosis of congenital adrenal hyperplasia using cell-free fetal DNA in maternal plasma. J. Clin. Endocrinol. Metab. 2014, 99, E1022–E1030. [Google Scholar] [CrossRef]
- Knorr, D.; Albert, E.D.; Bidlingmaier, F.; Höller, W.; Scholz, S. Different gene defects in the salt-wasting (SW), simple virilizing (SV), and nonclassical (NC) types of congenital adrenal hyperplasia (CAH). Ann. N. Y. Acad. Sci. 1985, 458, 71–75. [Google Scholar] [CrossRef] [PubMed]
- Held, P.K.; Bird, I.M.; Heather, N.L. Newborn Screening for Congenital Adrenal Hyperplasia: Review of Factors Affecting Screening Accuracy. Int. J. Neonatal. Screen. 2020, 6, 67. [Google Scholar] [CrossRef] [PubMed]
- Parsa, A.A.; New, M.I. Steroid 21-hydroxylase deficiency in congenital adrenal hyperplasia. J. Steroid. Biochem. Mol. Biol. 2017, 165 Pt A, 2–11. [Google Scholar] [CrossRef]
- Carmina, E.; Dewailly, D.; Escobar-Morreale, H.F.; Kelestimur, F.; Moran, C.; Oberfield, S.; Witchel, S.F.; Azziz, R. Non-classic congenital adrenal hyperplasia due to 21-hydroxylase deficiency revisited: An update with a special focus on adolescent and adult women. Hum. Reprod. Update 2017, 23, 580–599. [Google Scholar] [CrossRef] [PubMed]
- Spandri, A.; Cogliardi, A.; Maggi, P.; De Giorgi, A.; Masperi, R.; Beccaria, L. Congenital adrenal hyperplasia. Arch. Ital. Urol. Androl. 2004, 76, 143–146. [Google Scholar] [PubMed]
- Nordenström, A.; Falhammar, H. Management of Endocrine Disease: Diagnosis and management of the patient with non-classic CAH due to 21-hydroxylase deficiency. Eur. J. Endocrinol. 2019, 180, R127–R145. [Google Scholar] [CrossRef] [PubMed]
- Nermoen, I.; Rørvik, J.; Holmedal, S.H.; Hykkerud, D.L.; Fougner, K.J.; Svartberg, J.; Husebye, E.S.; Løvås, K. High frequency of adrenal myelolipomas and testicular adrenal rest tumours in adult Norwegian patients with classical congenital adrenal hyperplasia because of 21-hydroxylase deficiency. Clin. Endocrinol. 2011, 75, 753–759. [Google Scholar] [CrossRef] [PubMed]
- Nermoen, I.; Falhammar, H. Prevalence and Characteristics of Adrenal Tumors and Myelolipomas in Congenital Adrenal Hyperplasia: A Systematic Review and Meta-Analysis. Endocr. Pract. 2020, 26, 1351–1365. [Google Scholar] [CrossRef]
- Calissendorff, J.; Juhlin, C.C.; Sundin, A.; Bancos, I.; Falhammar, H. Adrenal myelolipomas. Lancet Diabetes Endocrinol. 2021, 9, 767–775. [Google Scholar] [CrossRef]
- Campbell, M.J.; Obasi, M.; Wu, B.; Corwin, M.T.; Fananapazir, G. The radiographically diagnosed adrenal myelolipoma: What do we really know? Endocrine 2017, 58, 289–294. [Google Scholar] [CrossRef]
- Reginelli, A.; Vacca, G.; Belfiore, M.; Sangiovanni, A.; Nardone, V.; Vanzulli, A.; Grassi, R.; Cappabianca, S. Pitfalls and differential diagnosis on adrenal lesions: Current concepts in CT/MR imaging: A narrative review. Gland Surg. 2020, 9, 2331–2342. [Google Scholar] [CrossRef]
- Dogra, P.; Sundin, A.; Juhlin, C.C.; Calissendorff, J.; Falhammar, H.; Bancos, I. Rare benign adrenal lesions. Eur. J. Endocrinol. 2023, 188, 407–420. [Google Scholar] [CrossRef] [PubMed]
- Daneshmand, S.; Quek, M.L. Adrenal myelolipoma: Diagnosis and management. Urol. J. 2006, 3, 71–74. [Google Scholar] [PubMed]
- Sharma, M.C.; Kashyap, S.; Sharma, R.; Chumber, S.; Sood, R.; Chahal, R. Symptomatic adrenal myelolipoma. Clinicopathological analysis of 7 cases and brief review of the literature. Urol. Int. 1997, 59, 119–124. [Google Scholar] [CrossRef] [PubMed]
- Bnaya, A.; Benjaminov, O.; Shavit, L. Bilateral extra-adrenal perirenal myelolipoma associated with obstructive uropathy. Am. J. Med. Sci. 2023, 365, e10–e11. [Google Scholar] [CrossRef] [PubMed]
- Hamidi, O.; Raman, R.; Lazik, N.; Iniguez-Ariza, N.; McKenzie, T.J.; Lyden, M.L.; Thompson, G.B.; Dy, B.M.; Young, W.F., Jr.; Bancos, I. Clinical course of adrenal myelolipoma: A long-term longitudinal follow-up study. Clin. Endocrinol. 2020, 93, 11–18. [Google Scholar] [CrossRef] [PubMed]
- McGeoch, S.C.; Olson, S.; Krukowski, Z.H.; Bevan, J.S. Giant bilateral myelolipomas in a man with congenital adrenal hyperplasia. J. Clin. Endocrinol. Metab. 2012, 97, 343–344. [Google Scholar] [CrossRef] [PubMed]
- Auchus, R.J.; Arlt, W. Approach to the patient: The adult with congenital adrenal hyperplasia. J. Clin. Endocrinol. Metab. 2013, 98, 2645–2655. [Google Scholar] [CrossRef]
- Decmann, Á.; Perge, P.; Tóth, M.; Igaz, P. Adrenal myelolipoma: A comprehensive review. Endocrine 2018, 59, 7–15. [Google Scholar] [CrossRef]
- Ramdani, A.; Aissaoui, A.; Bouhout, T.; Bennani, A.; Latrech, H.; Serji, B.; El Harroudi, T. Giant symptomatic adrenal myelolipoma: A case report. Ann. Med. Surg. 2022, 75, 103333. [Google Scholar] [CrossRef]
- Finkielstain, G.P.; Kim, M.S.; Sinaii, N.; Nishitani, M.; Van Ryzin, C.; Hill, S.C.; Reynolds, J.C.; Hanna, R.M.; Merke, D.P. Clinical characteristics of a cohort of 244 patients with congenital adrenal hyperplasia. J. Clin. Endocrinol. Metab. 2012, 97, 4429–4438. [Google Scholar] [CrossRef] [PubMed]
- Schröder, M.A.M.; Claahsen-van der Grinten, H.L. Novel treatments for congenital adrenal hyperplasia. Rev. Endocr. Metab. Disord. 2022, 23, 631–645. [Google Scholar] [CrossRef] [PubMed]
- Itonaga, T.; Hasegawa, Y. Monitoring treatment in pediatric patients with 21-hydroxylase deficiency. Front. Endocrinol. 2023, 14, 1102741. [Google Scholar] [CrossRef] [PubMed]
- Shariq, O.A.; McKenzie, T.J. Adrenocortical carcinoma: Current state of the art, ongoing controversies, and future directions in diagnosis and treatment. Ther. Adv. Chronic. Dis. 2021, 12, 20406223211033103. [Google Scholar] [CrossRef] [PubMed]
- Bancos, I.; Taylor, A.E.; Chortis, V.; Sitch, A.J.; Jenkinson, C.; Davidge-Pitts, C.J.; Lang, K.; Tsagarakis, S.; Macech, M.; Riester, A.; et al. Urine steroid metabolomics for the differential diagnosis of adrenal incidentalomas in the EURINE-ACT study: A prospective test validation study. Lancet Diabetes Endocrinol. 2020, 8, 773–781. [Google Scholar] [CrossRef] [PubMed]
- Albano, D.; Agnello, F.; Midiri, F.; Pecoraro, G.; Bruno, A.; Alongi, P.; Toia, P.; Di Buono, G.; Agrusa, A.; Sconfienza, L.M.; et al. Imaging features of adrenal masses. Insights Imaging 2019, 10, 1. [Google Scholar] [CrossRef] [PubMed]
- Moran, C.; Azziz, R.; Carmina, E.; Dewailly, D.; Fruzzetti, F.; Ibañez, L.; Knochenhauer, E.S.; Marcondes, J.A.; Mendonca, B.B.; Pignatelli, D.; et al. 21-Hydroxylase-deficient nonclassic adrenal hyperplasia is a progressive disorder: A multicenter study. Am. J. Obstet. Gynecol. 2000, 183, 1468–1474. [Google Scholar] [CrossRef]
- Cera, G.; Locantore, P.; Novizio, R.; Maggio, E.; Ramunno, V.; Corsello, A.; Policola, C.; Concolino, P.; Paragliola, R.M.; Pontecorvi, A. Pregnancy and Prenatal Management of Congenital Adrenal Hyperplasia. J. Clin. Med. 2022, 11, 6156. [Google Scholar] [CrossRef]
- New, M.I.; Ghizzoni, L.; Meyer-Bahlburg, H.; Khattab, A.; Reichman, D.; Rosenwaks, Z. Fertility in patients with nonclassical congenital adrenal hyperplasia. Fertil. Steril. 2019, 111, 13–20. [Google Scholar] [CrossRef]
- Almeida, M.Q.; Kaupert, L.C.; Brito, L.P.; Lerario, A.M.; Mariani, B.M.; Ribeiro, M.; Monte, O.; Denes, F.T.; Mendonca, B.B.; Bachega, T.A. Increased expression of ACTH (MC2R) and androgen (AR) receptors in giant bilateral myelolipomas from patients with congenital adrenal hyperplasia. BMC Endocr. Disord. 2014, 14, 42. [Google Scholar] [CrossRef]
- Falhammar, H. Non-functioning adrenal incidentalomas caused by 21-hydroxylase deficiency or carrier status? Endocrine 2014, 47, 308–314. [Google Scholar] [CrossRef] [PubMed]
- Libé, R.; Arlt, W.; Louiset, E.; Waintrop, C.; Guibourdenche, J.; Sibony, M.; Clauser, E.; Groussin, L. A feminizing adrenocortical carcinoma in the context of a late onset 21-hydroxylase deficiency. J. Clin. Endocrinol. Metab. 2014, 99, 1943–1944. [Google Scholar] [CrossRef] [PubMed]
- Falhammar, H.; Torpy, D.J. A 42-year-old man presented with adrenal incidentaloma due to non-classic congenital adrenal hyperplasia with a novel CYP21A2 mutation. Intern. Med. J. 2016, 46, 1115–1116. [Google Scholar] [CrossRef]
- Kocak, M.; Nuhoglu, I.; Mungan, S.; Duman, P.; Coskun, H.; Turkyılmaz, S. Bilateral adrenal myelolipomas secondary to congenital adrenal hyperplasia: A rare case of typical asymmetrical 18F-FDG avid. Acta Endocrinol. 2016, 12, 491–492. [Google Scholar] [CrossRef] [PubMed]
- Buitenwerf, E.; Links, T.P.; Kema, I.P.; Haadsma, M.L.; Kerstens, M.N. Congenital adrenal hyperplasia as a cause of adrenal incidentaloma. Neth. J. Med. 2017, 75, 298–300. [Google Scholar] [PubMed]
- Feng, X.; Kline, G. Massive adrenal incidentalomas and late diagnosis of congenital adrenal hyperplasia in prostate cancer. Endocrinol. Diabetes Metab. Case Rep. 2017, 2017, 17–0108. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hui, E.; Lee, A.C.; Lang, B.H.; Chan, A.O.; Lam, K.S.; Tan, K.C. Congenital adrenal hyperplasia presenting as a large adrenal incidentaloma in an elderly man. ANZ J. Surg. 2017, 87, 310–312. [Google Scholar] [CrossRef] [PubMed]
- Mallappa, A.; Millo, C.M.; Quezado, M.; Merke, D.P. Congenital Adrenal Hyperplasia Presenting as an Adrenal Mass With Increased 18F-FDG Positron Emission Tomography Uptake. J. Endocr. Soc. 2017, 1, 1110–1112. [Google Scholar] [CrossRef]
- Hirai, H.; Kuwana, K.; Kusano, Y. Late onset adrenal insufficiency after adrenalectomy due to latent nonclassical 21-hydroxylase deficiency: A case report. Medicine 2018, 97, e11888. [Google Scholar] [CrossRef]
- Liu, Q.; Wang, L.A.; Su, J.; Tong, D.; Lan, W.; Wang, L.; Liu, G.; Zhang, J.; Zhang, V.W.; Zhang, D.; et al. Giant bilateral adrenal myelolipomas in two Chinese families with congenital adrenal hyperplasia. Endocr. Connect. 2018, 7, 1136–1141. [Google Scholar] [CrossRef]
- Kim, H.J. Adrenal myelolipoma in association with congenital adrenal hyperplasia. Endocrine 2019, 63, 403–404. [Google Scholar] [CrossRef] [PubMed]
- Suchartlikitwong, S.; Jasti, R.; Lado-Abeal, J.; Rivas Mejia, A.M. Bilateral adrenal myelolipomas presenting as acute adrenal insufficiency in an adult with congenital adrenal hyperplasia. BMJ Case Rep. 2019, 12, e226826. [Google Scholar] [CrossRef] [PubMed]
- Aveiro-Lavrador, M.; De Sousa Lages, A.; Barros, L.; Paiva, I. Late diagnosis of classic congenital adrenal hyperplasia: Long-term consequences during adulthood. Endocrinol. Diabetes Metab. Case Rep. 2021, 2021, 21–0032. [Google Scholar] [CrossRef]
- San Martín, P.; Eugenio Russmann, M.L.; Mendeluk, G.; Fierro, M.F.; Marino, R.; Pardes, E. Classical congenital adrenal hyperplasia due to 21-hydroxylase deficiency (21-OHD) in adult males: Clinical presentation, hormone function and the detection of adrenal and testicular adrenal rest tumors (TARTs). Endocrinol. Diabetes Nutr. 2021, 68, 227–235. [Google Scholar] [CrossRef] [PubMed]
- Burman, P.; Falhammar, H.; Waldenström, E.; Sundin, A.; Bitzén, U. 11C-Metomidate PET/CT Detected Multiple Ectopic Adrenal Rest Tumors in a Woman With Congenital Adrenal Hyperplasia. J. Clin. Endocrinol. Metab. 2021, 106, e675–e679. [Google Scholar] [CrossRef]
- Robinson, D.A.; Kemeny, M.; Muchinyi, J.E.; Yasin, M.; Montes, N.I.; Tuli, S.; Jaiswal, R.; Carter, A.; Derezil, M.A.; Jang, H.; et al. Adrenal Myelolipoma Masquerading as an Adrenal Malignancy. Case Rep. Endocrinol. 2022, 2022, 4044602. [Google Scholar] [CrossRef] [PubMed]
- Tang, P.; Zhang, J.; Peng, S.; Wang, Y.; Li, H.; Wang, Z.; Zhang, Y.; Huang, Y.; Xu, J.; Zhang, D.; et al. Genotype-phenotype correlation in patients with 21-hydroxylase deficiency. Front. Endocrinol. 2023, 14, 1095719. [Google Scholar] [CrossRef]
- Lee, S.J.; Song, J.E.; Hwang, S.; Lee, J.Y.; Park, H.S.; Han, S.; Rhee, Y. Untreated Congenital Adrenal Hyperplasia with 17-α Hydroxylase/17,20-Lyase Deficiency Presenting as Massive Adrenocortical Tumor. Endocrinol. Metab. 2015, 30, 408–413. [Google Scholar] [CrossRef]
- Yang, F.; Zhao, Y.; Lv, J.; Sheng, X.; Wang, L. A new compound heterozygous mutation in a female with 17α-hydroxylase/17,20-lyase deficiency, slipped capital femoral epiphysis, and adrenal myelolipoma. Gynecol. Endocrinol. 2019, 35, 385–389. [Google Scholar] [CrossRef]
- Chang, L.; Yu, D.; Wang, F. 17α-hydroxylase deficiency associated with adrenal myelolipoma. Pol. Arch. Intern. Med. 2023, 133, 16369. [Google Scholar] [CrossRef]
- Ozbas, B.; Demir, M.; Dursun, H.; Sahin, I.; Hacioglu, A.; Karaca, Z.; Dundar, M.; Unluhizarci, K. Case Report: A Novel Mutation Leading to 11-β Hydroxylase Deficiency in a Female Patient. Endocr. Metab. Immune Disord. Drug Target 2023, 23, 721–726. [Google Scholar] [CrossRef]
- Ladjouze, A.; Donaldson, M.; Plotton, I.; Djenane, N.; Mohammedi, K.; Tardy-Guidollet, V.; Mallet, D.; Boulesnane, K.; Bouzerar, Z.; Morel, Y.; et al. Genotype, Mortality, Morbidity, and Outcomes of 3β-Hydroxysteroid Dehydrogenase Deficiency in Algeria. Front. Endocrinol. 2022, 13, 867073. [Google Scholar] [CrossRef] [PubMed]
- Al-Bahri, S.; Tariq, A.; Lowentritt, B.; Nasrallah, D.V. Giant bilateral adrenal myelolipoma with congenital adrenal hyperplasia. Case Rep. Surg. 2014, 2014, 728198. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Alvarez, J.F.; Goldstein, L.; Samreen, N.; Beegle, R.; Carter, C.; Shaw, A.; Ben-David, K. Giant adrenal myelolipoma. J. Gastrointest. Surg. 2014, 18, 1716–1718. [Google Scholar] [CrossRef] [PubMed]
- Kale, G.; Pelley, E.M.; Davis, D.B. Giant myelolipomas and inadvertent bilateral adrenalectomy in classic congenital adrenal hyperplasia. Endocrinol. Diabetes Metab. Case Rep. 2015, 2015, 150079. [Google Scholar] [CrossRef] [PubMed]
- Altieri, V.M.; Altieri, B.; Castellucci, R.; Alba, S.; Bottone, F.; Fragalà, E.; Mirone, V.; Greco, F. Leydig cell tumour and giant adrenal myelolipoma associated with adrenogenital syndrome: A case report with a review of the literature. Urologia 2016, 83, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Meng, X.; Yu, Y. Non-classical 21-hydroxylase deficiency presented as Addison’s disease and bilateral adrenal incidentalomas. Acta Endocrinol. 2017, 13, 232–236. [Google Scholar] [CrossRef]
- Łebek-Szatańska, A.; Nowak, K.M.; Samsel, R.; Roszkowska-Purska, K.; Zgliczyński, W.; Papierska, L. Adrenocortical carcinoma associated with giant bilateral myelolipomas in classic congenital adrenal hyperplasia. Pol. Arch. Intern. Med. 2019, 129, 549–550. [Google Scholar] [CrossRef]
- Piskinpasa, H.; Ciftci Dogansen, S.; Kusku Cabuk, F.; Guzey, D.; Sahbaz, N.A.; Akdeniz, Y.S.; Mert, M. Bilateral adrenal and testicular mass in a patient with congenital adrenal hyperplasia. Acta Endocrinol. 2019, 5, 113–117. [Google Scholar] [CrossRef]
- Lim, E.; Jeon, J.Y. Congenital adrenal hyperplasia presenting as pelvic inflammatory disease in a phenotypic male: A case report. Medicine 2020, 99, e18387. [Google Scholar] [CrossRef]
- Pakalniskis, M.G.; Ishigami, K.; Pakalniskis, B.L.; Fujita, N. Adrenal collision tumour comprised of adrenocortical carcinoma and myelolipoma in a patient with congenital adrenal hyperplasia. J. Med. Imaging Radiat. Oncol. 2020, 64, 67–68. [Google Scholar] [CrossRef] [PubMed]
- Khalil, N.; Bizdikian, A.J.; Nasr, S.; Fakih, F.; Hajj, P. Suspicious adrenal incidentaloma in a patient with Congenital Adrenal Hyperplasia: A case report. Urol. Case Rep. 2021, 36, 101569. [Google Scholar] [CrossRef] [PubMed]
- Kienitz, T.; Schwander, J.; Bogner, U.; Schwabe, M.; Steinmüller, T.; Quinkler, M. Giant bilateral adrenal lipoma in a patient with congenital adrenal hyperplasia. Endocrinol. Diabetes Metab. Case Rep. 2021, 2021, 20–0204. [Google Scholar] [CrossRef] [PubMed]
- Vemula, B.R.; Olajide, O.B.; Adepoju, Y. Bilateral Adrenal Myelolipomas in a Female Patient With Undiagnosed Non-classic Congenital Adrenal Hyperplasia. Cureus 2023, 15, e35017. [Google Scholar] [CrossRef] [PubMed]
- Longoria-Dubocq, T.; Torres-Aguiar, R.; Ruiz-Vega, K.; De Ayala-Hillmann, R.; Lopez-Enriquez, R. A Rare Case of Congenital Adrenal Hyperplasia with Giant Adrenal Myelolipoma. Puerto Rico Health Sci. J. 2020, 39, 226–228. [Google Scholar]
- La, B.; Tung, C.; Choi, E.A.; Nguyen, H. A Gigantic Uterine Leiomyoma and Big Bilateral Adrenal Myelolipomas as a Result of Untreated Congenital Adrenal Hyperplasia. AACE Clin. Case Rep. 2021, 7, 342–345. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.; Khoo, T.K.; Voelschow, E.R.; Viets, Z.J. Compliance Issues in Managing 21 Hydroxylase Deficiency and their Short/Long-Term Consequences. Eur. J. Case Rep. Intern. Med. 2021, 8, 003048. [Google Scholar] [CrossRef]
- Jacobson, A.; Koberlein, E.; Thomay, A.; Lombard, C.B.; Adelanwa, A.; Lakhani, D.A.; Smith, K.T. Congenital adrenal hyperplasia with associated giant adrenal myelolipoma, testicular adrenal rest tumors and primary pigmented nodular adrenocortical disease: A case report and brief review of the literature. Radiol. Case Rep. 2021, 17, 710–716. [Google Scholar] [CrossRef]
- Soveid, M.; Rais-Jalali, G.A. Seventeen Alpha-Hydroxylase Deficiency Associated with Absent Gonads and Myelolipoma: A Case Report and Review of Literature. Iran J. Med. Sci. 2016, 41, 543–547. [Google Scholar]
- Askitis, D.; Kloos, C.; Battefeld, W.; Müller, N.; Wolf, G.; Dirsch, O.; Müller, U.A. Complete evaluation of adrenal tumours in a tertiary care institution in Thuringia, Germany. Exp. Clin. Endocrinol. Diabetes 2015, 123, 347–352. [Google Scholar] [CrossRef]
- Kiedrowicz, B.; Binczak-Kuleta, A.; Lubikowski, J.; Koziolek, M.; Andrysiak-Mamos, E.; Ostanek-Panka, M.; Ciechanowicz, A.; Syrenicz, A. Prevalence and Clinical Outcome of CYP21A2 Gene Mutations in Patients with Nonfunctional Adrenal Incidentalomas. Horm. Metab. Res. 2015, 47, 662–667. [Google Scholar] [CrossRef] [PubMed]
- Patrova, J.; Jarocka, I.; Wahrenberg, H.; Falhammar, H. Clinical outcomes in adrenal incidentaloma: Experience from one center. Endocr. Pract. 2015, 21, 870–877. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Choi, J.H.; Kang, E.; Kim, Y.M.; Lee, B.H.; Yoo, H.W. Long-term Consequences of Congenital Adrenal Hyperplasia due to Classic 21-hydroxylase Deficiency in Adolescents and Adults. Exp. Clin. Endocrinol. Diabetes 2017, 125, 196–201. [Google Scholar] [CrossRef] [PubMed]
- Goh, Z.; Phillips, I.; Hunt, P.J.; Soule, S.; Cawood, T.J. Characteristics of adrenal incidentalomas in a New Zealand centre. Intern. Med. J. 2018, 48, 173–178. [Google Scholar] [CrossRef] [PubMed]
- El-Maouche, D.; Hannah-Shmouni, F.; Mallappa, A.; Hargreaves, C.J.; Avila, N.A.; Merke, D.P. Adrenal morphology and associated comorbidities in congenital adrenal hyperplasia. Clin. Endocrinol. 2019, 91, 247–255. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.M.; Kim, J.H.; Jang, H.N.; Choi, M.H.; Cho, J.Y.; Kim, S.Y. Adrenal Morphology as an Indicator of Long-Term Disease Control in Adults with Classic 21-Hydroxylase Deficiency. Endocrinol. Metab. 2022, 37, 124–137. [Google Scholar] [CrossRef] [PubMed]
- Sahlander, F.; Bensing, S.; Falhammar, H. Congenital adrenal hyperplasia is a very rare cause of adrenal incidentalomas in Sweden. Front. Endocrinol. 2022, 13, 1017303. [Google Scholar] [CrossRef] [PubMed]
- Sahlander, F.; Patrova, J.; Mannheimer, B.; Lindh, J.D.; Falhammar, H. Congenital adrenal hyperplasia in patients with adrenal tumors: A population-based case-control study. J. Endocrinol. Invest. 2023, 46, 559–565. [Google Scholar] [CrossRef]
- Jin, H.Y.; Choi, J.H.; Kim, D.Y.; Yoo, H.W. Adrenocortical Carcinoma in a Patient with Congenital Adrenal Hyperplasia. J. Korean Soc. Pediatr. Endocrinol. 2010, 15, 193–197. [Google Scholar]
- Falhammar, H.; Thorén, M. An 88-year-old woman diagnosed with adrenal tumor and congenital adrenal hyperplasia: Connection or coincidence? J. Endocrinol. Invest. 2005, 28, 449–453. [Google Scholar] [CrossRef]
- Hao, M.; Lopez, D.; Luque-Fernandez, M.A.; Cote, K.; Newfield, J.; Connors, M.; Vaidya, A. The Lateralizing Asymmetry of Adrenal Adenomas. J. Endocr. Soc. 2018, 2, 374–385. [Google Scholar] [CrossRef]
- Kim, J.; Bae, K.H.; Choi, Y.K.; Jeong, J.Y.; Park, K.G.; Kim, J.G.; Lee, I.K. Clinical characteristics for 348 patients with adrenal incidentaloma. Endocrinol. Metab. 2013, 28, 20–25. [Google Scholar] [CrossRef] [PubMed]
- Debono, M.; Bradburn, M.; Bull, M.; Harrison, B.; Ross, R.J.; Newell-Price, J. Cortisol as a marker for increased mortality in patients with incidental adrenocortical adenomas. J. Clin. Endocrinol. Metab. 2014, 99, 4462–4470. [Google Scholar] [CrossRef] [PubMed]
- Sangwaiya, M.J.; Boland, G.W.; Cronin, C.G.; Blake, M.A.; Halpern, E.F.; Hahn, P.F. Incidental adrenal lesions: Accuracy of characterization with contrast-enhanced washout multidetector CT--10-minute delayed imaging protocol revisited in a large patient cohort. Radiology 2010, 256, 504–510. [Google Scholar] [CrossRef] [PubMed]
- Gupta, P.; Bhalla, A.; Sharma, R. Bilateral adrenal lesions. J. Med. Imaging Radiat. Oncol. 2012, 56, 636–645. [Google Scholar] [CrossRef] [PubMed]
- Khater, N.; Khauli, R. Myelolipomas and other fatty tumours of the adrenals. Arab. J. Urol. 2011, 9, 259–265. [Google Scholar] [CrossRef] [PubMed]
- AlSaffar, A.H.; AlEssa, A.M.; AlSharkawy, T.; Alamoudi, N.B.; Makhdom, F.A. Anterior Mediastinal Myelolipoma: A Case Report and Review of the Literature. Am. J. Case Rep. 2022, 23, e936005. [Google Scholar] [CrossRef] [PubMed]
- Fattahi, N.; Moeini, A.; Morani, A.C.; Elsayes, K.M.; Bhosale, H.R.; Badawy, M.; Menias, C.O.; Rezvani, M.; Gaballah, A.H.; Shaaban, A.M. Fat-containing pelvic lesions in females. Abdom. Radiol. 2022, 47, 362–377. [Google Scholar] [CrossRef]
- Anbardar, M.H.; Soleimani, N.; Nikeghbalian, S.; Mohebbi, M. Adrenocortical adenoma with myelolipomatous metaplasia: A potential diagnostic pitfall: A case report and review of the literature. J. Med. Case Rep. 2021, 15, 333. [Google Scholar] [CrossRef]
- Kenney, L.; Hughes, M. Adrenocortical Carcinoma: Role of Adjuvant and Neoadjuvant Therapy. Surg. Oncol. Clin. N. Am. 2023, 32, 279–287. [Google Scholar] [CrossRef]
- Ławnicka, H. Current Prospects for Adrenocortical Carcinoma Pharmacotherapy. Recent Pat. Anti-Cancer Drug Discov. 2023, 18, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Mete, O.; Erickson, L.A.; Juhlin, C.C.; de Krijger, R.R.; Sasano, H.; Volante, M.; Papotti, M.G. Overview of the 2022 WHO Classification of Adrenal Cortical Tumors. Endocr. Pathol. 2022, 33, 155–196. [Google Scholar] [CrossRef] [PubMed]
- Rowe, N.E.; Kumar, R.; Schieda, N.; Siddiqi, F.; McGregor, T.; McAlpine, K.; Violette, P.; Bathini, V.; Eng, M.; Izard, J. Diagnosis, management, and follow-up of the incidentally discovered adrenal mass: CUA Guideline Endorsed by the AUA. J. Urol. 2023, 210, 590–599. [Google Scholar] [CrossRef] [PubMed]
- Dumitru, N.; Ghemigian, A.; Carsote, M.; Albu, S.E.; Terzea, D.; Valea, A. Thyroid nodules after initial evaluation by primary health care practitioners: An ultrasound pictorial essay. Arch. Balk. Med. Union. 2016, 51, 434–438. [Google Scholar]
- Nistor, C.E.; Pantile, D.; Stanciu-Gavan, C.; Ciuche, A.; Moldovan, H. Diagnostic and Therapeutic Characteristics in Patients with Pneumotorax Associated with COVID-19 versus Non-COVID-19 Pneumotorax. Medicina 2022, 58, 1242. [Google Scholar] [CrossRef] [PubMed]
- Nistor, C.E.; Gavan, C.S.; Pantile, D.; Tanase, N.V.; Ciuche, A. Cervico-Thoracic Air Collections in COVID-19 Pneumonia Patients—Our Experience and Brief Review. Chirurgia 2022, 117, 317–327. [Google Scholar] [CrossRef] [PubMed]
- Parazzoli, C.; Favero, V.; Aresta, C.; Morelli, V. Predicting morphological and functional variations of benign adrenal incidentalomas in relation to initial characteristics. Front. Endocrinol. 2023, 14, 1179817. [Google Scholar] [CrossRef]
- Trolle, C.; Fjeldborg, K.; Shukla, A.; Ebbehøj, A.; Poulsen, P.L.; Hansen, K.W. Adrenal incidentalomas and effectiveness of patient pathway transformation. Dan. Med. J. 2023, 70, A10220645. [Google Scholar]
- Okroj, D.; Rzepecka, A.; Kłosowski, P.; Babińska, A.; Sworczak, K. Review of Diagnostic Modalities for Adrenal Incidentaloma. J. Clin. Med. 2023, 12, 3739. [Google Scholar] [CrossRef]
- Sconfienza, E.; Tetti, M.; Forestiero, V.; Veglio, F.; Mulatero, P.; Monticone, S. Prevalence of Functioning Adrenal Incidentalomas: A Systematic Review and Meta-analysis. J. Clin. Endocrinol. Metab. 2023, 108, 1813–1823. [Google Scholar] [CrossRef]
- Ioannidis, O.; Papaemmanouil, S.; Chatzopoulos, S.; Paraskevas, G.; Konstantara, A.; Kotronis, A.; Kakoutis, E.; Makrantonakis, A. Giant bilateral symptomatic adrenal myelolipomas associated with congenital adrenal hyperplasia. Pathol. Oncol. Res. 2011, 17, 775–778. [Google Scholar] [CrossRef]
- Conzo, G.; Tartaglia, E.; Gambardella, C.; Esposito, D.; Sciascia, V.; Mauriello, C.; Nunziata, A.; Siciliano, G.; Izzo, G.; Cavallo, F.; et al. Minimally invasive approach for adrenal lesions: Systematic review of laparoscopic versus retroperitoneoscopic adrenalectomy and assessment of risk factors for complications. Int. J. Surg. 2016, 28 (Suppl. S1), S118–S123. [Google Scholar] [CrossRef]
- Conzo, G.; Pasquali, D.; Gambardella, C.; Della Pietra, C.; Esposito, D.; Napolitano, S.; Tartaglia, E.; Mauriello, C.; Thomas, G.; Pezzolla, A.; et al. Long-term outcomes of laparoscopic adrenalectomy for Cushing disease. Int. J. Surg. 2014, 12 (Suppl. S1), S107–S111. [Google Scholar] [CrossRef]
- Falhammar, H.; Torpy, D.J. Congenital Adrenal Hyperplasia Due to 21-Hydroxylase Deficiency Presenting as Adrenal Incidentaloma: A Systematic Review and Meta-Analysis. Endocr. Pract. 2016, 22, 736–752. [Google Scholar] [CrossRef]

| First Author/Reference/Year | Studied Population/Age (Years)/Gender | CAH Form | Age at CAH Diagnosis (Years) | Age at Tumour Diagnosis (Years) | |
|---|---|---|---|---|---|
| Almeida [50] 2014 | N = 4 with ML (2/4 with SV-CAH) | 35/F | SV | <20 | 35 |
| 52/F | SV | NA | 52 | ||
| Falhammar [51] 2014 | N = 9 (5/9 with genetic confirmation) | 88/F | NC | 88 | 88 |
| 48/F | NC | 48 | 48 | ||
| 21/F | NC | 21 | 21 | ||
| 41/F | carrier | 41 | 41 | ||
| 67/M | SV | 67 | 67 | ||
| Libé [52] 2014 | 77/M | NC | 77 | 77 | |
| Falhammar [53] 2016 | 42/M | NC | 42 | 42 | |
| Kocak [54] 2016 | 46/M | NC | 43 | 46 | |
| Buitenwerf [55] 2017 | 43/M | SV | 43 | 43 | |
| Feng [56] 2017 | 61/M | SV | 61 | 61 | |
| Hui [57] 2017 | 65/phenotypically male (46,XX karyotype) | SV | 65 | 65 | |
| Mallappa [58] 2017 | 29/F | SV | 29 | 29 | |
| Hirai [59] 2018 | 71/M | NC | 71 | 49 | |
| Liu [60] 2018 | N = 5 with ML | 59/M | NC | 59 | 46 |
| his brother | NC | NA | 50 | ||
| Kim [61] 2019 | 64/M | SV | 64 | 56 | |
| Suchartlikitwong [62] 2019 | 39/M (46,XX karyotype) | SV | 39 | 39 | |
| Aveiro-Lavrador [63] 2021 | 37/M | SV | 37 | 35 | |
| San Martín [64] 2021 | N = 4 with adrenal tumours (out of 8 males with CAH) | 21/M | SW | NA | 21 |
| 23/M | SV | 3 months | 23 | ||
| 28/M | SV | 28 | 28 | ||
| Burman [65] 2021 | 31/F | SW | at birth | 28 | |
| Robinson [66] 2022 | 48/M | SV | 48 | 48 | |
| Tang [67] 2023 | N = 3 with CAH and 2 with adrenal tumours | 37/M | NC | 37 | 37 |
| 59/M | NC | 59 | 59 | ||
| Reference | Tumour: Uni/Bilateral; Size (cm); Site (Left/Right) | Type | Clinical Presentation → Treatment |
|---|---|---|---|
| [50] | BAT: 14 × 14 × 10 cm (L) + 8.9 × 8.3 × 8.0 cm (R) | ML | Abdominal pain → adrenalectomy |
| BAT: 16 × 13 × 9.0 cm (L) + 5.3 × 4.3 × 6.9 cm (R) | ML | Abdominal pain → adrenalectomy | |
| [51] | LAT: 3 × 4 × 5 cm | I | Abdominal pain, constipation → prednisolone 5 mg/day |
| two LAT: 1.3 × 1 cm + 1.4 × 1.5 cm | I | CT performed due to pneumonia; oligomenorrhea (PCOS) → prednisolone 5 mg (when needed) | |
| LAT: 1 cm | I | Diffuse abdominal discomfort (PCOS)→ patient declined any treatment | |
| BAT: 1 cm (L) + 0.9 cm (R) | I | Hirsutism, fertility issues (PCOS), abdominal discomfort → lifestyle changes (carrier) | |
| RAT: 8 cm | I | Abdominal discomfort → right adrenalectomy (benign) | |
| [52] | LAT: 2 cm | ACC | Gynecomastia → adrenalectomy (causality cannot be established) → ↗ post-operatory 17OHP |
| [53] | LAT: 5.5 cm × 3.6 cm × 4.5 cm | I | Asymptomatic → hydrocortisone (at stress) |
| [54] | BAT: 10.6 × 7.0 × 5.5 cm (L) + 8.1 × 4.2 x3.3 cm (R) | ML | Palpable mass → bilateral adrenalectomy |
| [55] | LAT: 5.2 × 4.4 cm | I | Fatigue and myalgia → dexamethasone 0.5 mg/day |
| [56] | BAT: 18.2 × 16.2 × 14 cm (L) + 6.4 × 8.7 × 7.8 cm (R) | ML | Short stature, azoospermia, precocious puberty, increased testosterone in spite of anti-androgenic treatment for prostate cancer → glucocorticoid replacement |
| [57] | RAT:5.8 × 3.9 × 4.5 cm | HMA | Lower urinary tract symptoms, empty scrotum, small penile length, short stature → right adrenalectomy (the patient also had small uterine-like structure, small ovaries and prostate) |
| [58] | LAT: 10 × 7 cm | ML | Hyperpigmentation, abdominal pain, kidney compression → left adrenalectomy |
| [59] | LAT: 3–4 cm | I (ACA) | Left adrenalectomy at 49 years of age → adrenal insufficiency 22 years after adrenalectomy |
| [60] | giant BAT (R > L) | ML | Abdominal pain → bilateral adrenalectomy → 1.56 kg (L) and 3.05 kg (R) |
| giant BAT | ML | Bilateral adrenalectomy | |
| [61] | LAT: 12.5 × 7.5 cm RAT: diffuse nodular enlargement | ML | Adrenal hyperplasia identified on CT, early puberty → left adrenalectomy at 56 years of age |
| [62] | BAT: 2.3 × 1.4 × 2.5 cm (L) + 6 × 4.5 × 5cm (R) | ML | Adrenal insufficiency → glucocorticoid replacement ML were diagnosed based on CT and MRI findings |
| [63] | ML: 3 cm (R); ML: 2 cm (L) | ML + EACA | Consanguinity; personal history of precocious puberty, infertility, back pain → right adrenalectomy |
| [64] | RAT: 0.6 cm × 1.2 cm | NA | Three patients had genetic testing, while one patient did not |
| LAT: 1.5 cm × 1.7 cm | NA | NA | |
| RAT: 4.9 cm × 3.4 cm | I (ACA) | Mass incidentally found during work-up for biliary colic → surgery | |
| [65] | BAT: 11 cm (R) + 11 × 8.5 × 13 cm (L) | ML | RAT growth → right adrenalectomy → left adrenalectomy after 7 years |
| [66] | BAT: 8.4 × 6.2 × 7.5 cm (L) + 1.6 × 2 × 2.5 cm + 1.7 × 1.5 × 1.8 cm (R) | I (ML) | Short stature → left adrenalectomy and distal pancreatectomy → hydrocortisone therapy |
| [67] | RAT: 4.3 × 3.7 cm | AH | Azoospermia, small testes, hypospadias, premature pubarche, short stature → replacement therapy (the patient also had secondary hypogonadotropic hypogonadism) |
| BAT: 20 × 25 cm (L) and 30 × 40 cm (R) | ML | Abdominal distension, surgical resection → glucocorticoid and mineralocorticoid replacement (the patient’s brother also underwent surgery for bilateral giant MLs at the age of 50) |
| Reference | Genetic Testing Results |
|---|---|
| [50] | Compound heterozygote p.E351V, p.I236N, p.V237E, and p.M239K genetic variants in the CYP21A2 gene |
| IVS2-13A/C>G/p.I172N | |
| [51] | V281L and I172N |
| V281L | |
| V281L/V281L | |
| I172N | |
| I172N/deletion | |
| [52] | Biallelic micro-conversion between the promoter regions of CYP21A2 and the pseudogene CYP21A1 |
| [53] | Compound heterozygous genetic variants: Pro30Leu genetic variant on one allele and a novel heterozygous duplication (c.264_276dup (p.Glu93Cysfs*5)) on the second allele |
| [54] | Homozygous g.656A/C>G point genetic variant |
| [55] | Compound heterozygous genetic variants: c.518T>A (p.Ile173Asn) and c.710T>A, c.713T>A, c.719T>A (p.lIe237Asn), (p.Val238Glu), (p.Met240Lys) |
| [56] | Complete gene deletion on one allele and a C518T>A (I172N) genetic variant on the other |
| [57] | Compound heterozygous p.Ile172Asn, p.Arg483Pro, and p.Met485Trpfs*56 genetic variants |
| [58] | Heterozygosity for intron 2 IVS2-13A/C>G splice site genetic variant/p.R483P (c.1451_1452 deletion insertion of C) |
| [59] | Micro genetic variant I172N and heterozygous large gene deletion or conversion |
| [60] | Compound heterozygous genetic variant: c.293-13C>G and c.518T>A, p.I173N |
| Compound heterozygous genetic variant: c.293-13C>G and c.518T>A, p.I173N | |
| [61] | IVS2-13A/C>G and p.I173N |
| [62] | Compound heterozygous R356W and intron 2G genetic variant |
| [63] | Variant g.655C>G |
| [64] | Heterozygosity: p.Gln318Ter (Q318) and p.Gly110ValfsTer21 (Del8bpE3) |
| Homozygous genetic variant c.293-13C>G | |
| p.Ile172Asn (p I172N) and Del/Conv | |
| [65] | Gln318stop/deletion in the CYP21A2 gene |
| [66] | c.293–13C>G genetic variant on both alleles |
| [67] | Compound heterozygous genetic variant c.293-13C>G and c.518T>A, p.I173N |
| Compound heterozygous genetic variant c.293-13C>G and c.518T>A, p.I173N |
| Reference | Tumour Size (cm) | Hormonal Panel at Presentation for Adrenal Tumour | ||
|---|---|---|---|---|
| ACTH | 17-hydroxyprogesterone | Other Hormonal Assays or Observations | ||
| (pg/mL) | (ng/mL or nmol/L) | |||
| [50] | >10 | 1172 | 192 ng/mL | Testosterone = 949 ng/dL; Androstendione = 17 ng/mL |
| >10 | NA | 120 ng/mL | Testosterone = 720 ng/dL; Androstendione = 39 ng/mL | |
| [51] | 5–10 | NA | NA | Late diagnosis |
| <5 | NA | 37 nmol/L | ||
| <5 | NA | 32 nmol/L | ||
| <5 | NA | 11.1 nmol/L | ||
| 5–10 | NA | 338 nmol/L | ||
| [52] | <5 | NA | 42 nmol/L | Late diagnosis |
| [53] | 5–10 | normal | 51 nmol/L | Patient received diagnosis after incidentaloma was discovered |
| [54] | >10 | 214 | 28.6 ng/mL | DHEA-S = 29 (N:80-560) μg/dL |
| [55] | 5–10 | 27 | 426 nmol/L | Testosterone = 13 nmol/L; Androstendione = 14 nmol/L |
| [56] | >10 | NA | NA | Late diagnosis |
| [57] | 5–10 | NA | markedly raised | Testosterone normal (late diagnosis) |
| [58] | 5–10 | NA | 17,900 ng/dL | Late diagnosis |
| [59] | <5 | 1820 | 9.4 ng/mL | Testosterone = 3.26 ng/mL; Androstendione = 1.15 ng/mL |
| Late diagnosis, poor compliance with treatment | ||||
| [61] | >10 | 157.6 | 27,500 ng/dL | Late diagnosis |
| [62] | 5–10 | 10,445 | 2003 ng/dL | Late diagnosis |
| [63] | <5 | 1351 | 57 ng/mL | Testosterone = 0.7 ng/mL; Androstenedione = 4.5 µg/mL; late diagnosis |
| [64] | <5 | NA | NA | |
| <5 | NA | NA | Irregular adherence to treatment during childhood | |
| <5 | NA | NA | ||
| [65] | >10 | 3 | 269 nmol/L | Androstenedione and 17-hydroxyprogesterone with fluctuant pattern |
| [66] | 5–10 | 160 | 6078 ng/dL | Testosterone = 447.0 ng/dL; DHEA-S = 598 ug/dL; late diagnosis |
| [67] | <5 | 1131 | 485.20 nmol/L | Testosterone = 4.05 (normal: 1.75–7.81) ng/mL; DHEA = 7.99 ng/mL; late diagnosis |
| >10 | NA | NA | Late diagnosis | |
| First Author/Reference/Year | Patient Age/Gender | Genetic Testing (CYP17A1 Deficiency) | Age at CAH Diagnosis /Tumour Diagnosis (Years) | Tumour Features | Clinical Features | Therapy | |
|---|---|---|---|---|---|---|---|
| Lee [68] 2015 | 36/F | Compound heterozygous genetic variant for p.Tyr329fs (c.985_987delTACinsAA) + missense genetic variant p.His373Leu (c.1118A > T) | 36/36 | 10 × 6.3 × 8.6 cm Adrenal cortical adenoma | Abdominal pain Tanner 1 | Left adrenalectomy | |
| Liu [60] 2018 | Patient 3: 36/F | Compound heterozygous genetic variant: c.1118A>T, p.H373L, and c.1459_1467del9, p.D487_F489del | 36/36 | Giant bilateral adrenal masses, the largest (left) of 20 cm × 15 cm × 10 cm Myelolipoma | Headaches, hypokalaemia since childhood, +hypertension (prior 6 years) | Left and right adrenalectomies | |
| Patient 4: 32/F | Compound heterozygous genetic variant: c.1118A>T, p.H373L, and c.1459_1467del9, p.D487_F489del | 32/32 | Myelolipoma | Fatigue, hypokalaemia | Left adrenalectomy | ||
| Patient 5: 37/F | Compound heterozygous genetic variant: c.1118A>T, p.H373L, and c.1459_1467del9, p.D487_F489del | 37/37 | Myelolipoma | Hypertension, hypokalaemia (3 years prior) | Left and right adrenalectomies | ||
| Yang [69] 2019 | 27/F (46,XX karyotype) | Compound heterozygous genetic variant: c.985_987delTACinsAA (p.Tyr329fs) in exon 6 (frame-shift genetic variant) and c.1270C>T (p.Gln424) in exon 8 (nonsense genetic variant) | 27/27 | Myelolipoma | Persistent hypokalaemia, primary amenorrhoea | Dexamethasone 0.75 mg/day | |
| Chang [70] 2023 | 31/F (46,XY karyotype) | Heterozygous variant of c.985_987delinsAA (p.Y329Kfs*90) and p.R96W genetic variant | 31/31 | Left adrenal mass of 5 × 9 cm myelolipoma | Hypokalaemia, hypertension, primary amenorrhea, hypoplastic breasts, vaginal infantilism, lack of axillary and pubic hair | Surgical treatment of the adrenal myelolipoma and resection of gonads | |
| First Author Reference Number Year of Publication | Type of Study | Patient | Gene-Enzyme Deficiency | Gene Testing | Age at CAH Diagnosis (Years) | Age at Tumour Diagnosis (Years) | |
|---|---|---|---|---|---|---|---|
| Ozbas [71] 2023 | Case report | 35-year-old female (C1) | CYP11B1 | Homozygous missense genetic variant (c.1385T >C L462P variant (NM_000497.3) | 35 | 35 | |
| Ladjouze [72] 2022 | Mixed longitudinal and cross-sectional study | 14 patients from 10 families with HSD3B2 deficiency | 16-year-old female (C2) | HSD3B2 | p.(Pro222GIn) | 14 days | 16 |
| 13-year-old female (C3) | HSD3B2 | p.(Thr152_Pro155del) | 3 months | 13 | |||
| 15-year-old female (C4) | HSD3B2 | p.(Thr152_Pro155del) | 4 weeks | 15 | |||
| Tumour features and outcome | |||||||
| Reference | Patient | Tumour size | Pathological report | Clinical presentation | Surgery | Observations | |
| [71] | C1 | Left adrenal mass of 7.4 × 5.5 cm | Myelolipoma | Hypertension, adrenal mass, clitoromegaly, deep voice, hirsutism, hypokalaemia history of 2 genital reconstruction during childhood | Left adrenalectomy | The patient was prescribed glucocorticoids during childhood, but did not follow it regularly (for the previous 5 years the patient did not take glucocorticoids) | |
| [72] | C2 | Right adrenal mass of 2.7 × 3 cm | Adrenocortical hyperplasia | NA | Adrenalectomy | Initially, misdiagnosed as 21OHD mass had high suspicion of malignancy (unconfirmed) | |
| C3 * | Left adrenal mass of 6.3 × 5.2 × 5.1 cm | Adrenocortical hyperplasia | NA | Adrenalectomy | |||
| Reference | Hormonal Panel at Presentation for Adrenal Tumour | ||
|---|---|---|---|
| ACTH | Plasma Cortisol | Other Parameters | |
| [68] | 75.94 (normal: 7.2 to 63.6) pg/mL | NA | Na = 141 (normal: 135 to 145) mmol/L K = 3.3 (normal: 3.5 to 5.5) mmol/L Renin = 0.80 (normal: 1.31 to 3.95) ng/mL/hr Aldosterone = 183.31 (normal: 29.9 to 158.8) pg/mL Aldosterone to renin ratio = 22.9 |
| [60] | >1250 pg/mL (↗) | <2 μg/dL (↘) | Hypokalaemia |
| 271 pg/mL (↗) | <2 μg/dL (↘) | Hypokalaemia | |
| 503 pg/mL (↗) | <3.1 μg/dL (↘) | Hypokalaemia | |
| [69] | 41.56 (normal: 0–40) pg/mL | 171.39 (normal: 268.94–579.39) nmol/L | Hypokalaemia (K = 2.1 mmol/L) 17OHP < 0.05 (0.05–1.02) ng/mL |
| [70] | 225.80 (normal: 7.20–63.30) pg/mL | 0.1 (normal: 50–250) ng/mL | Hypokalaemia (K = 2.10 mmol/L, normal = 3.50–5.30) mmol/L Plasma renin activity = 0.91 (normal: 4–38) pg/mL Aldosterone = 76.78 (normal: 40–310) pg/mL Estradiol = 1.4 (normal: 15–350) pg/mL Testosterone = 10.4 (normal: 80–600) pg/mL DHEA-S = 0.9 (normal: 830–3770) ng/mL |
| [71] | 279 (normal: 0–246) pg/mL | 4.8 (normal: 6.2–18) μg/dL | K = 2.7 mmol/L, Na = 140 mmol/L Androstenedione>10 (normal: 0.3–3.3) ng/dL Total testosterone = 236 (normal: 6–82) ng/dL 17OHP = 8.31 (normal: 0.2–1) ng/dL |
| [72] | NA | NA | 17OHP = 2.14 (normal: 0.48–1.87) nmol/L 17OHPreg = 93 (normal: 0.13–13.7) nmol/L (one patient) |
| First Author/Reference | Population | CAH Form | Method of CAH Diagnosis | Age at CAH Diagnosis | Age at Tumour Diagnosis |
|---|---|---|---|---|---|
| Al-Bahri [73] | 39-year-old male | NA | Unclear | Childhood | 39 |
| Alvarez [74] | 44-year-old female | SV | Virilizing CAH | Infancy/childhood | 44 |
| Kale [75] | 51-year-old male | SW | NA | Infancy | 51 |
| Altieri [76] | 42-year-old male | SV | Precocious puberty | 4 years | 42 |
| Meng [77] | 40-year-old male | NC | Hormonal work-up | 40 | 31 |
| Łebek-Szatańska [78] | 32-year-old male | SW | Salt waste | Neonate | 30 |
| Piskinpasa [79] | 41-year-old male | SV | ACTH stimulation test | 41 | 41 |
| Lim [80] | 58-year-old male | SV | Hormonal + ACTH stimulation test | 58 | 58 |
| Pakalniskis [81] | 61-year-old male | SV | NA | NA (known CAH) | 61 |
| Khalil [82] | 27-year-old phenotypic male, 46,XX karyotype | SV | NA | Late childhood | 27 |
| Kienitz [83] | 50-year-old male | SW | Salt waste | Childhood | 50 |
| San Martín [65] | 42-year-old male | SV | Infancy | 42 | |
| Falhammar [51] | 56-year-old male | NC | ACTH stimulation test | 56 | 56 |
| 66-year-old male | NC | ACTH stimulation test | 66 | 66 | |
| 48-year-old female | NC | ACTH stimulation test | 48 | 48 | |
| 53-year-old female | carrier | ACTH stimulation test | 53 | 53 | |
| Vemula [84] | 68-year-old female | NC | Clinically and biochemically | 68 | 68 |
| Longoria-Dubocq [85] | 36-year-old male | NA | NA | NA (known CAH) | 36 |
| La [86] | 37-year-old born female with ambiguous genitalia identifying as male | SW | Salt waste | Neonate | 27 |
| Lin [87] | 36-year-old male | SW | At birth | 36 | |
| Jacobson [88] | 49-year-old male | SW | Salt waste | Infancy | 49 |
| Soveid [89] | 26-year-old female, XY karyotype | Hormonal work-up following hypertension diagnosis | 26 | 26 |
| Reference/ Age/Sex/ Enzyme Defect/ CAH Form | Tumour → Decision of Surgery (If Any) | Clinical Picture | Hormonal Panel at the Moment of Tumour Evaluation + Other Highlights |
|---|---|---|---|
| [73] 39/M CYP21A2 NA | BAT: 20 × 20 × 25 cm (L) + 16 × 12 × 15 cm (R) → ↗ size despite therapy → bilateral adrenalectomy | Abdominal distension, discomfort | ACTH = 42 (normal:6–50) pg/mL 17OHPg = 14,076 (normal: 42–196) ng/dL Testosterone = 506 (normal: 241–827) ng/dL |
| [74] 44/F CYP21A2 SV-CAH | 26 × 24 × 9.5 cm (L) → surgery (exploratory laparotomy and mass excision) | Abdominal distension, nausea, vomiting | NA |
| [75] 51/M CYP21A2 SW-CAH | BAT: 31.1 × 18.1 × 16.1 cm (L) + 13.7 × 6.6 × 10.6 cm (R) → bilateral adrenalectomy | Chronic back pain, lower limbs parasthesiasis | The patient was under long-term supra physiological glucocorticoid replacement, without biochemical monitoring |
| [76] 42/M CYP21A2 SV-CAH | BAT: 16 × 13 × 9.0 cm (L) + 5.3 × 4.3 × 6.9 cm (R) → left adrenalectomy | Recurrent abdominal pain, digestive symptoms | Despite right tumour growth, the patient remained asymptomatic and denied a second surgical intervention |
| [77] 40/M CYP21A2 NC-CAH | 5 × 4 cm (R) 4.1 × 3.9 cm (L) (diagnosis: 9 years after right adrenalectomy) | Adrenal insufficiency after initial right adrenalectomy | ACTH > 2000 (normal: 5.0–78) pg/mL 17OHPg = 21.13 (normal: 0.31–2.01) ng/mL Testosterone = 1.81 (normal: 2.49–8.36) ng/mL Cortisol = 157.8 (normal: 147.3–609.3) nmol/L |
| [78] 32/M CYP21A2 SW-CAH | BAT: 6.7 × 4.8 × 2.7 cm (R) + 19.8 × 19.1 × 12 cm (L) → left adrenalectomy → adrenal carcinoma → mitotane (The patient was awaiting for the right adrenalectomy) | Rapidly enlarging BAT | NA |
| [79] 41/M CYP21A2 SV-CAH | BAT: 4.1 × 2.2 cm (L) + 8.8 × 5.5 cm (R) (incidentally detected during follow-up of testes tumours) → right adrenalectomy → myelolipoma | Incidental imaging diagnosis | ACTH = 80.4 (normal: 9–46) pg/mL 17OHPg = 14 (normal: 0.2–2.3) ng/mL Testosterone = 1.79 (normal: 2.18–9.06) ng/mL Cortisol = 3.75 (normal: 6.2–19.4) μg/dL |
| [80] 58/M CYP21A2 SV-CAH | 10 cm (L) → planned surgery | ACTH = 181 (normal: 0–60) pg/mL 17OHPg = 13,800 (normal: 20–172) ng/dL Testosterone = 6.75 (normal: 2.5–10.63) ng/mL Cortisol = 8.6 (normal: 9.4–26.1) μg/dL | |
| [81] 61/M CYP21A2 SV-CAH | 10.3 cm (R) with calcifications + 2.9 cm (L) suggestive of myelolipoma → right adrenalectomy | Pressor-dependent shock | High ACTH High 17OHPg The patient had Mullerian structures (prior known with pseudo hermaphroditism |
| [82] 27/M * CYP21A2 SV-CAH | 9 × 8 × 7 cm (L) with calcifications and central necrosis measuring (of 5.5 cm) → left adrenalectomy | Incidentaloma on abdominal ultrasound | Normal ACTH High 17OHPg |
| [83] 50/M CYP21A2 SW-CAH | BAT with septic lobular appearance of 10 × 11 × 6 cm (L) + 14 × 19 × 11 cm (R) → right adrenalectomy | Polakidisuria | ACTH = 37.5 (normal: 1.6–45) pg/mL 17OHPg = 0.6 to 1.5 (normal: 0.2–1.4) ng/mL Testosterone = 1.7(normal:1.3–7.7) ng/mL Cortisol = 0.24 to 0.5 (normal: 0.5–3.5 ng/mL) |
| [64] 42/M CYP21A2 SV-CAH | Bilateral thickening with left predominance <1.3 cm | NA | |
| [51] 56/M CYP21A2 NC-CAH | BAT: 1.2 cm (L) + 0.9 cm (R) | Abdominal pain | 17OHPg = 14 nmol/L |
| [51] 66/M CYP21A2 NC-CAH | BAT of 1.5 cm the largest | 17OHPg = 3.4 nmol/L | |
| [51] 48/F CYP21A2 NC-CAH | BAT: 1.5 × 2 cm (L) + “minor” tumours (R) | Abdominal discomfort | 17OHPg = 6.9 nmol/L |
| [51] 53/F CYP21A2 carrier | BAT: 3.3 × 3 cm (L) + 1.3 × 3.3 (R) | Abdominal pain | 17OHPg = 2.3 nmol/L |
| [84] 68/F CYP21A2 NC-CAH | BAT: 6.6 × 9.7 × 10.5 cm (L) + 3 × 7.6 × 6.8 cm (right) → myelolipoma diagnosis was based on CT findings | Chest discomfort, virilization, hirsutism, excessive labial folds | ACTH = 266.7 (normal: 7.2–63.3) pg/mL 17OHPg = 25,018 (normal: 15–70) ng/dL Testosterone = 1195 (normal: 60–80) ng/mL Cortisol ** = 2.8 (normal: <1.8) µg/dL |
| [85] 36/M NA NA | left retroperitoneal mass of 30 × 23.6 × 16.7 cm → tumour developed despite of adequate CAH management → tumour resection | Abdominal pain, difficulty breathing | NA |
| [86] 37/ *** NA SW-CAH | BAT: 11.8 × 8.8 cm (L) + 5.9 × 2.4 cm (R) → bilateral adrenalectomy & hysterectomy with bilateral salpingo-oophorectomy | Abdominal distension, hypotension, virilization | ACTH = 166 (normal: 6–50) pg/mL 17OHPg = 4356 (normal: 285) ng/dL Testosterone = 737 (normal: 2–45) ng/dL Cortisol = 78.5 (normal: 3.7–19.4) mg/dL |
| [87] 36/M NA SW-CAH | Adrenal mass of 23 cm (L) + adrenal nodule of 2.5 cm (R) → the tumours were incidentally found → adrenalectomy → glucocorticoid/mineralocorticoid treatment | Admission for dyspnoea (pulmonary embolism) | ACTH = 128 (normal: 6–50) pg/mL 17OHPg = 17,300 ng/dL Myelolipoma was diagnosed based on CT findings |
| [88] 39/M NA SW-CAH | BAT: 18 × 13.4 × 12cm (L) + 7.3 × 2.7 × 5.8 cm (R) → bilateral adrenalectomy due to abdominal pain | Salt craving, hyperpigmentation, small testes, abdominal pain | 17OHPg = 8230 (normal < 220) ng/dL |
| [89] 26/F **** CYP17A1 hypertension | BAT: 6.5 cm (L) + 3 cm (R) → left adrenalectomy due to asymmetric enlargement and abdominal pain | Hypertension, Tanner 1 | ACTH = 185 (normal: 6–76) pg/mL 17OHPg < 10 (normal: 20–100) ng/dL Testosterone = <0.02 (normal: 0.084–0.481) ng/mL Cortisol = 0.9 (normal: 5.4–28.7) μg/dL |
| First Author Reference Number/Year | Study Design | Study Population | Results |
|---|---|---|---|
| Askitis [90] 2015 | Retrospective | 187 patients with adrenal tumours, including 49-year-old male patient with CAH | Prevalence of CAH among adrenal tumours: 0.53% |
| Kiedrowicz [91] 2015 | Retrospective | 100 patients with AI, out of whom 8 had CAH | Prevalence of CAH genetic variants among AIs: 0.8% |
| Patrova [92] 2015 | Retrospective | 637 patients with AI, out of whom 2 had CAH | Prevalence of CAH among AIs: 0.3% |
| Kim [93] 2017 | Retrospective | 53 patients with CAH due to CYP21A2 deficiency | Long-term consequences of CAH due to CYP21A2 deficiency: prevalence of adrenal tumours among CAH: 0.9% |
| Goh [94] 2018 | Prospective | 228 patients with AI, out of whom 4 had CAH | Prevalence of CAH genetic variants among AIs: 1.8% |
| El-Maouche [95] 2019 | Retrospective | 88 patients with CAH | Myelolipoma prevalence among CAH:12.5% |
| Kim [96] 2022 | Retrospective | 90 adults with 21OHD and 270 healthy controls | CAH control and adrenal morphology → prevalence of adrenal tumour among CAH/21OHD: 13.3% |
| Sahlander [97] 2022 | Prospective | 320 individuals with AI, out of whom 8 had CAH | Prevalence of CAH among patients with adrenal incidentalomas: 3.6% |
| Sahlander [98] 2023 | Retrospective (register-based) | 26,573 individuals with adrenal tumours, out of whom 20 had CAH and 144,124 controls without adrenal tumours, out of whom 1 had CAH | Prevalence of CAH among patients with adrenal tumours: 0.75‰ |
| Sahlander [98] 2023 | Retrospective (register-based) | 26,573 individuals with adrenal tumours, out of whom 20 had CAH and 144,124 controls without adrenal tumours, out of whom 1 had CAH | Prevalence of CAH among patients with adrenal tumours: 0.75‰ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carsote, M.; Gheorghe, A.-M.; Nistor, C.; Trandafir, A.-I.; Sima, O.-C.; Cucu, A.-P.; Ciuche, A.; Petrova, E.; Ghemigian, A. Landscape of Adrenal Tumours in Patients with Congenital Adrenal Hyperplasia. Biomedicines 2023, 11, 3081. https://doi.org/10.3390/biomedicines11113081
Carsote M, Gheorghe A-M, Nistor C, Trandafir A-I, Sima O-C, Cucu A-P, Ciuche A, Petrova E, Ghemigian A. Landscape of Adrenal Tumours in Patients with Congenital Adrenal Hyperplasia. Biomedicines. 2023; 11(11):3081. https://doi.org/10.3390/biomedicines11113081
Chicago/Turabian StyleCarsote, Mara, Ana-Maria Gheorghe, Claudiu Nistor, Alexandra-Ioana Trandafir, Oana-Claudia Sima, Anca-Pati Cucu, Adrian Ciuche, Eugenia Petrova, and Adina Ghemigian. 2023. "Landscape of Adrenal Tumours in Patients with Congenital Adrenal Hyperplasia" Biomedicines 11, no. 11: 3081. https://doi.org/10.3390/biomedicines11113081
APA StyleCarsote, M., Gheorghe, A.-M., Nistor, C., Trandafir, A.-I., Sima, O.-C., Cucu, A.-P., Ciuche, A., Petrova, E., & Ghemigian, A. (2023). Landscape of Adrenal Tumours in Patients with Congenital Adrenal Hyperplasia. Biomedicines, 11(11), 3081. https://doi.org/10.3390/biomedicines11113081










