High-Altitude Hypoxia Induces Excessive Erythrocytosis in Mice via Upregulation of the Intestinal HIF2a/Iron-Metabolism Pathway
Abstract
:1. Introduction
2. Materials and Methods
2.1. Animals and Treatments
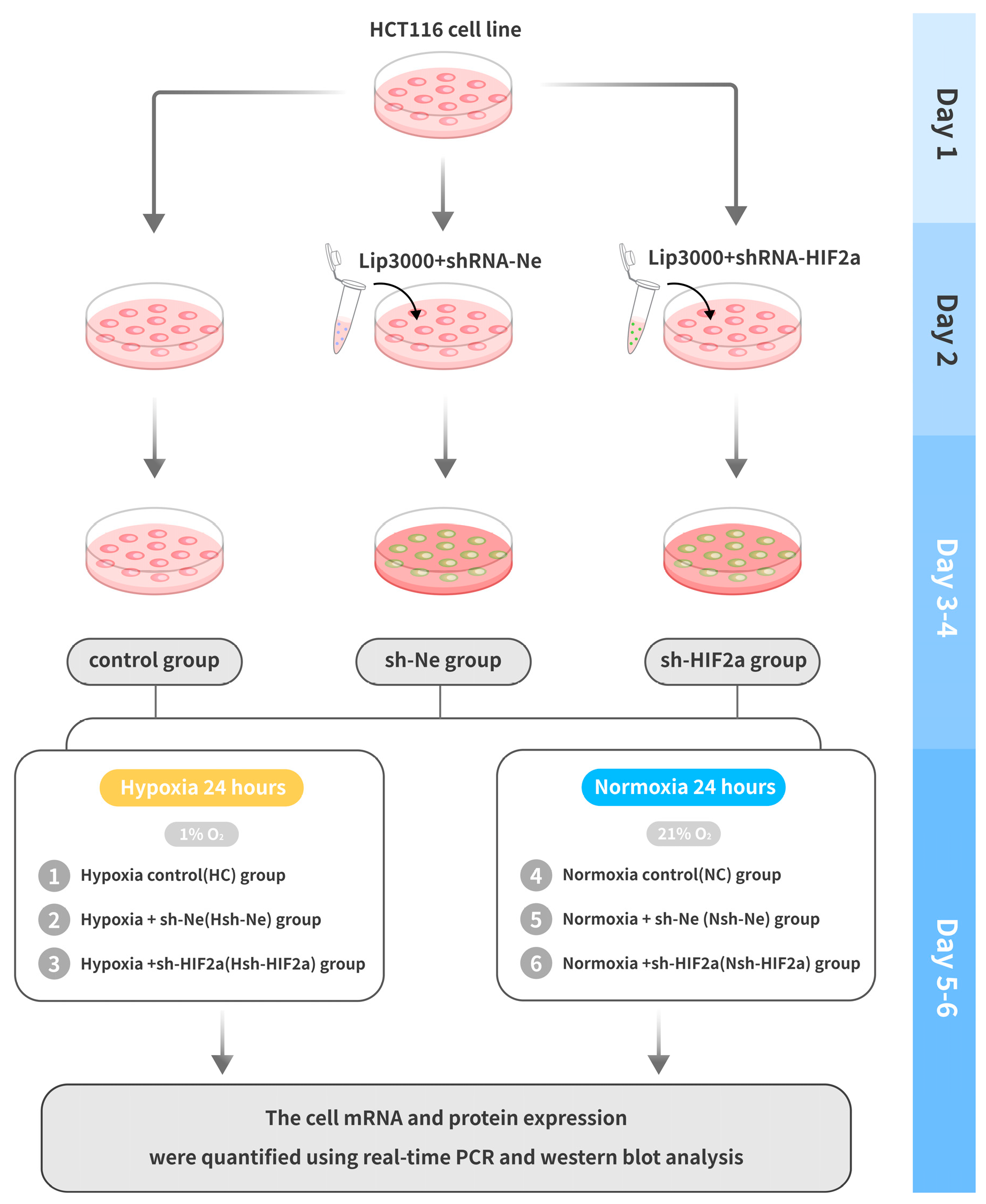
2.2. Cell Culture and Transfection
2.3. Hematological and Iron Analysis
2.4. Histology, Immunofluorescence Staining, and Tissue Iron Staining
2.5. Real-Time Quantitative PCR
2.6. Western Blot Analysis
2.7. Statistical Analysis
3. Results
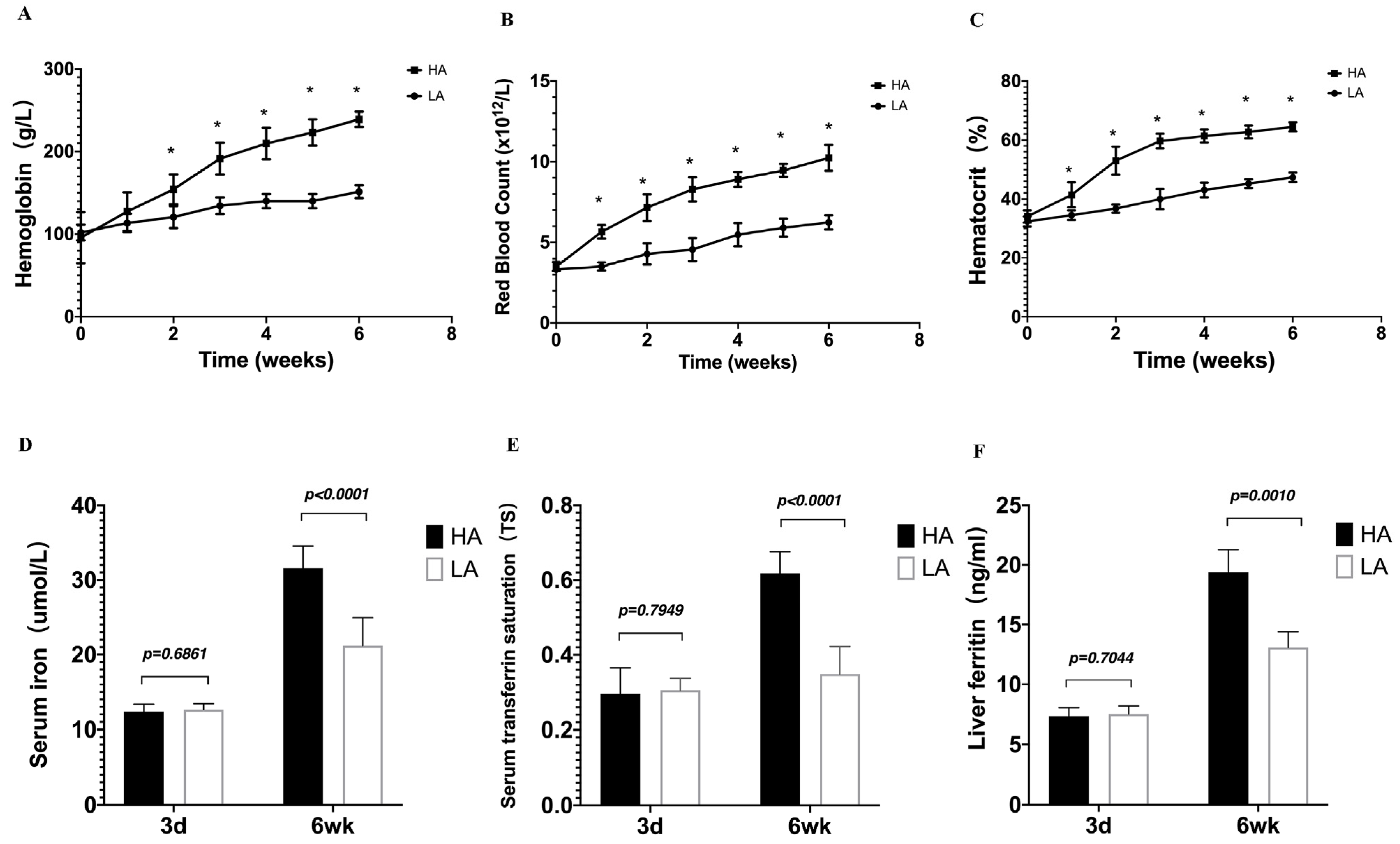
3.1. EE in High-Altitude Hypoxia Mice Is Accompanied by Enhanced Iron Availability
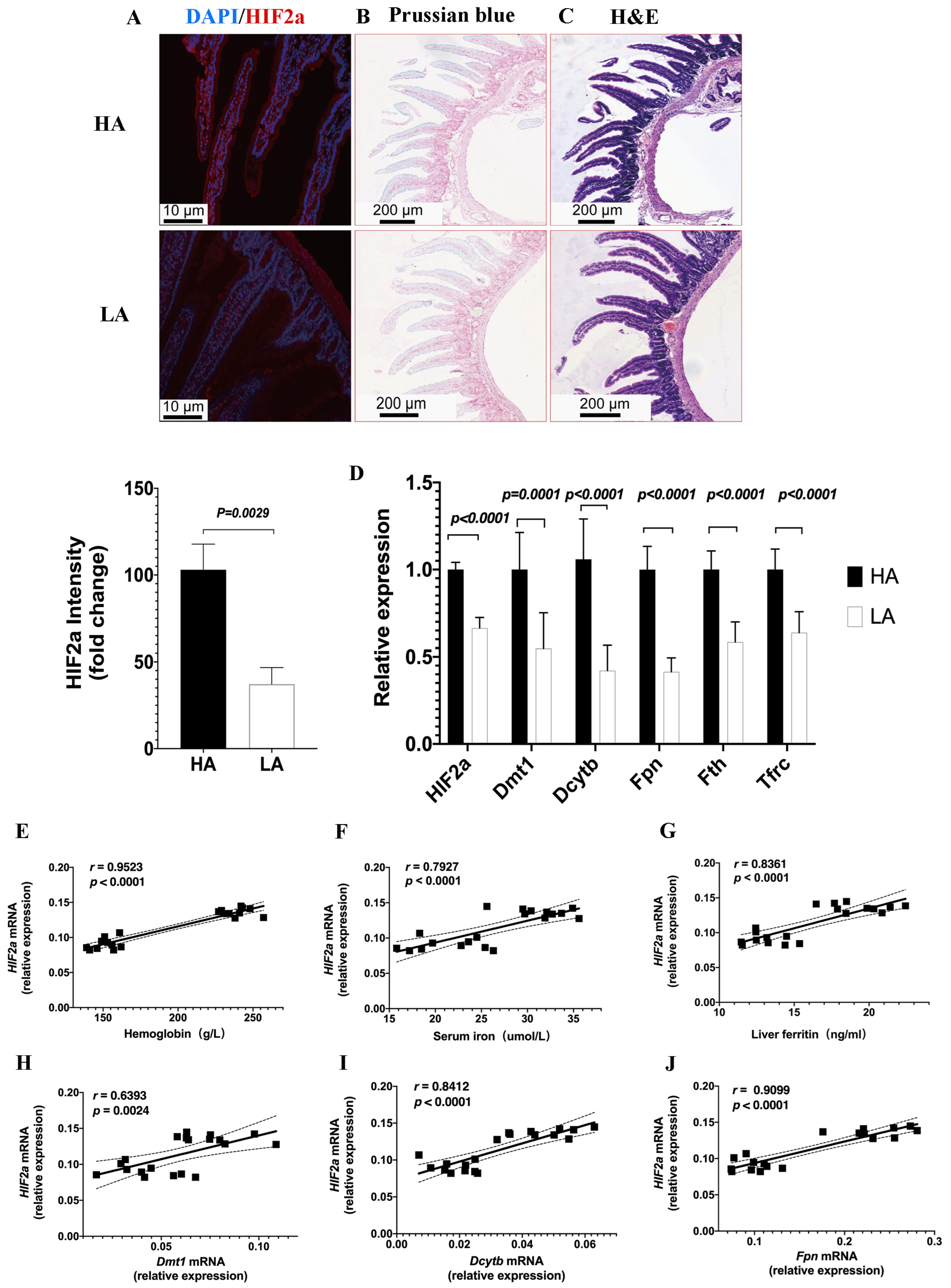
3.2. Intestinal HIF2α Signaling Is Associated with Iron Regulation in High-Altitude EE Mice
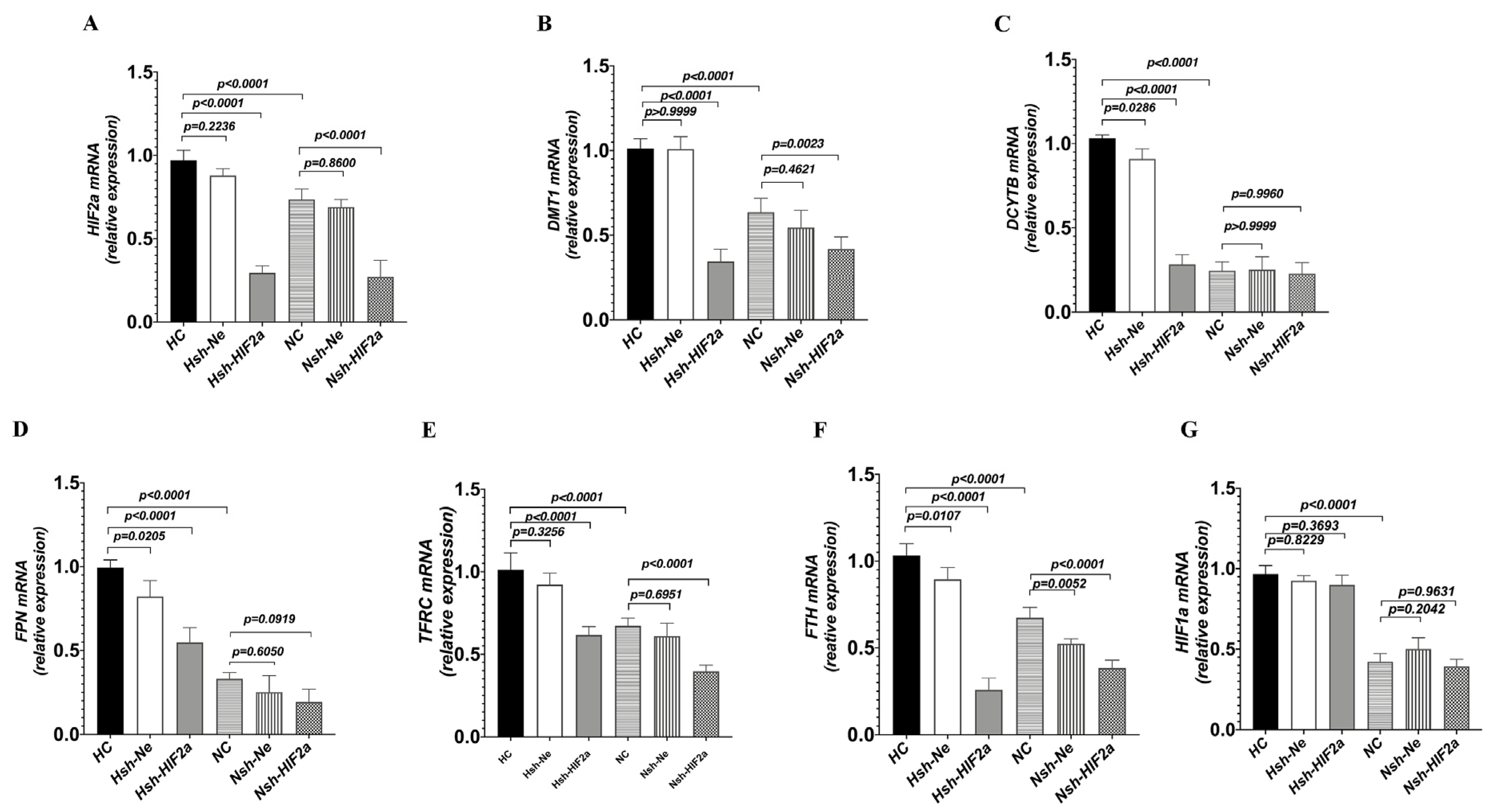
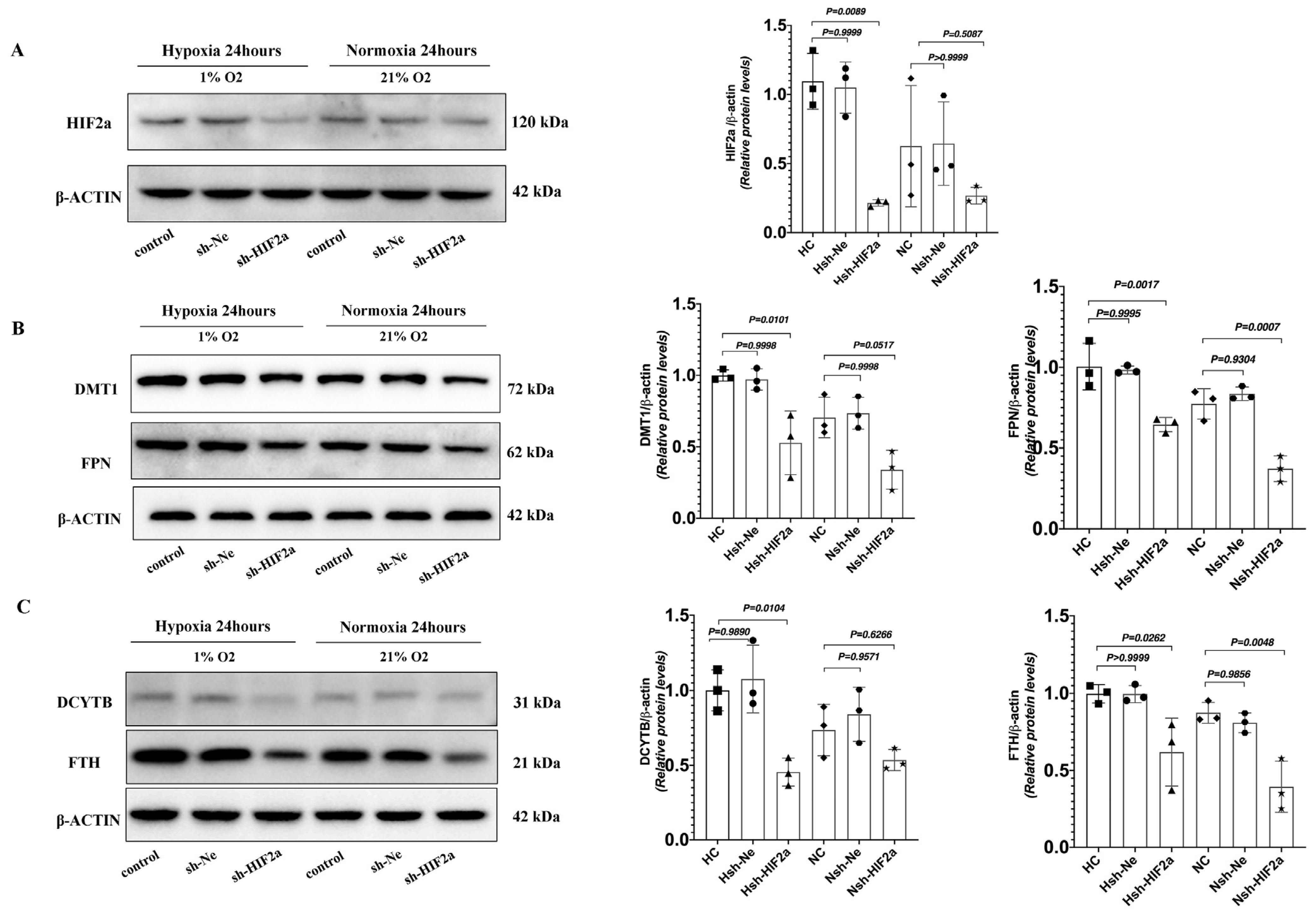
3.3. Knockdown of HIF2a Downregulates Genes Related to Iron Metabolism in HCT116 Cells under Hypoxic Conditions
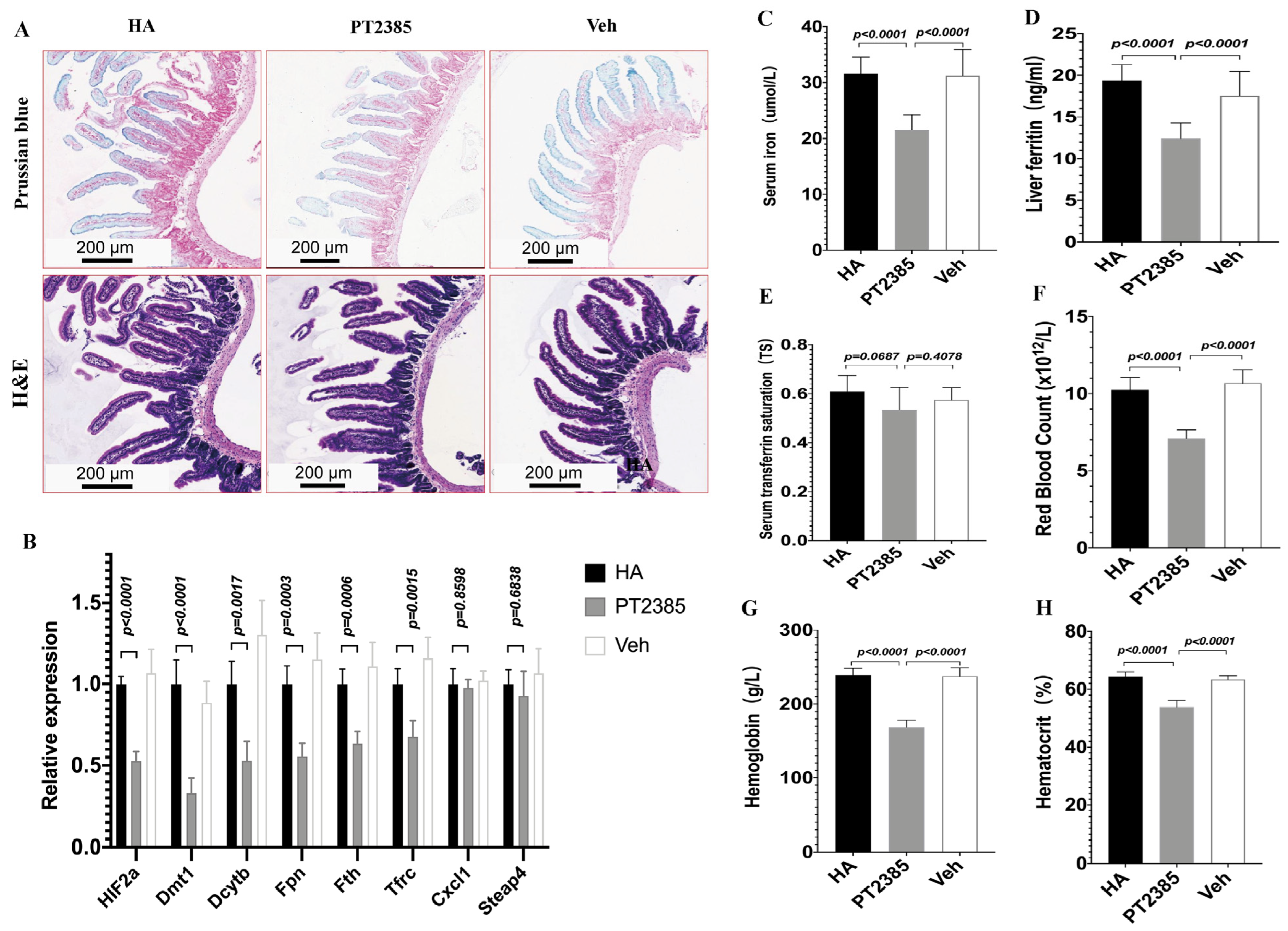
3.4. Inhibition of Intestinal HIF2α Transcription Decreases Iron Metabolism Gene Expression and Improves Excessive Erythrocytosis in High-Altitude Mice
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CMS | Chronic Mountain sickness |
| EE | Excessive erythrocytosis |
| HA | High-altitude |
| HC | Hypoxia control |
| HIF | Hypoxia-inducible factors |
| DMT1 | Divalent metal transporter |
| DCYTB | Duodenal cytochrome b |
| FPN | Ferroportin |
| TFRC | Transferrin receptor |
| FTH | Ferritin |
| CXCL1 | C-X-C motif chemokine ligand 1 |
| STEAP4 | STEAP family member 4 |
| LA | Low-altitude |
| NC | Normoxia control |
| RBC | Red blood cells |
| Hb | Hemoglobin |
| Hct | Hematocrit |
| TIBC | Total Iron Binding Capacity |
| TS | Transferrin saturation |
References
- Hancco, I.; Bailly, S.; Baillieul, S.; Doutreleau, S.; Germain, M.; Pépin, J.-L.; Verges, S. Excessive Erythrocytosis and Chronic Mountain Sickness in Dwellers of the Highest City in the World. Front. Physiol. 2020, 11, 773. [Google Scholar] [CrossRef] [PubMed]
- Vargas, E.; Spielvogel, H. Chronic mountain sickness, optimal hemoglobin, and heart disease. High Alt. Med. Biol. 2006, 7, 138–149. [Google Scholar] [CrossRef] [PubMed]
- Beall, C.M.; Cavalleri, G.L.; Deng, L.; Elston, R.C.; Gao, Y.; Knight, J.; Li, C.; Li, J.C.; Liang, Y.; McCormack, M.; et al. Natural selection on EPAS1 (HIF2α) associated with low hemoglobin concentration in Tibetan highlanders. Proc. Natl. Acad. Sci. USA 2010, 107, 11459–11464. [Google Scholar] [CrossRef] [PubMed]
- Monge, C.; Leon-Velarde, F.; Laguë, S.L.; Coppel, J.; Court, J.; van der Kaaij, J.; Vercueil, A.; Feelisch, M.; Levett, D.; Mythen, M.; et al. Physiological adaptation to high altitude: Oxygen transport in mammals and birds. Physiol. Rev. 1991, 71, 1135–1172. [Google Scholar] [CrossRef] [PubMed]
- Moore, L.G. Measuring high-altitude adaptation. J. Appl. Physiol. 2017, 123, 1371–1385. [Google Scholar] [CrossRef] [PubMed]
- De Ferrari, A.; Miranda, J.J.; Gilman, R.H.; Dávila-Román, V.G.; León-Velarde, F.; Rivera-Ch, M.; Huicho, L.; Bernabé-Ortiz, A.; Wise, R.A.; Checkley, W. Prevalence, clinical profile, iron status, and subject-specific traits for excessive erythrocytosis in andean adults living permanently at 3825 meters above sea level. Chest 2014, 146, 1327–1336. [Google Scholar] [CrossRef]
- Sahota, I.; Panwar, N. Prevalence of Chronic Mountain Sickness in high altitude districts of Himachal Pradesh. Indian J. Occup. Environ. Med. 2013, 17, 94–100. [Google Scholar] [CrossRef]
- Monge, C.; León-Velarde, F.; Arregui, A. Increasing prevalence of excessive erythrocytosis with age among healthy high-altitude miners. N. Engl. J. Med. 1989, 321, 1271. [Google Scholar] [CrossRef]
- Arregui, A.; León-Velarde, F.; Cabrera, J.; Paredes, S.; Vizcarra, D.; Umeres, H. Migraine, polycythemia and chronic mountain sickness. Cephalalgia 1994, 14, 339–341. [Google Scholar] [CrossRef]
- León-Velarde, F.; Maggiorini, M.; Reeves, J.T.; Aldashev, A.; Asmus, I.; Bernardi, L.; Ge, R.L.; Hackett, P.; Kobayashi, T.; Moore, L.G.; et al. Consensus statement on chronic and subacute high altitude diseases. High Alt. Med. Biol. 2005, 6, 147–157. [Google Scholar] [CrossRef]
- Villafuerte, F.C.; Corante, N.; Ucrós, S.; Granados, C.M.; Castro-Rodríguez, J.A.; Hill, C.M.; Parr, N.; Wilkes, M.; Hawkes, L.A.; Grissom, C.K.; et al. Chronic Mountain Sickness: Clinical Aspects, Etiology, Management, and Treatment. High Alt. Med. Biol. 2016, 17, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Azad, P.; Stobdan, T.; Zhou, D.; Hartley, I.; Akbari, A.; Bafna, V.; Haddad, G.G. High-altitude adaptation in humans: From genomics to integrative physiology. J. Mol. Med. 2017, 95, 1269–1282. [Google Scholar] [CrossRef] [PubMed]
- León-Velarde, F.; Richalet, J.P. Respiratory control in residents at high altitude: Physiology and pathophysiology. High Alt. Med. Biol. 2006, 7, 125–137. [Google Scholar] [CrossRef]
- Stobdan, T.; Akbari, A.; Azad, P.; Zhou, D.; Poulsen, O.; Appenzeller, O.; Gonzales, G.F.; Telenti, A.; Wong, E.H.M.; Saini, S.; et al. New Insights into the Genetic Basis of Monge’s Disease and Adaptation to High-Altitude. Mol. Biol. Evol. 2017, 34, 3154–3168. [Google Scholar] [CrossRef]
- Gassmann, M.; Muckenthaler, M.U. Adaptation of iron requirement to hypoxic conditions at high altitude. J. Appl. Physiol. 2015, 119, 1432–1440. [Google Scholar] [CrossRef] [PubMed]
- Muckenthaler, M.U.; Mairbäurl, H.; Gassmann, M. Iron metabolism in high-altitude residents. J. Appl. Physiol. 2020, 129, 920–925. [Google Scholar] [CrossRef]
- Atanasiu, V.; Manolescu, B.; Stoian, I. Hepcidin–central regulator of iron metabolism. Eur. J. Haematol. 2007, 78, 1–10. [Google Scholar] [CrossRef]
- Hirota, K. An intimate crosstalk between iron homeostasis and oxygen metabolism regulated by the hypoxia-inducible factors (HIFs). Free Radic. Biol. Med. 2019, 133, 118–129. [Google Scholar] [CrossRef]
- Yoon, D.; Ponka, P.; Prchal, J.T. Hypoxia. 5. Hypoxia and hematopoiesis. Am. J. Physiol. Physiol. 2011, 300, C1215–C1222. [Google Scholar] [CrossRef]
- Staub, K.; Haeusler, M.; Bender, N.; Morozova, I.; Eppenberger, P.E.; Panczak, R.; Zwahlen, M.; Schaer, D.J.; Maggiorini, M.V.; Ulrich, S.; et al. Hemoglobin concentration of young men at residential altitudes between 200 and 2000m mirrors Switzerland’s topography. Blood 2020, 135, 1066–1069. [Google Scholar] [CrossRef]
- Shah, Y.M.; Matsubara, T.; Ito, S.; Yim, S.-H.; Gonzalez, F.J. Intestinal hypoxia-inducible transcription factors are essential for iron absorption following iron deficiency. Cell Metab. 2009, 9, 152–164. [Google Scholar] [CrossRef] [PubMed]
- Mastrogiannaki, M.; Matak, P.; Keith, B.; Simon, M.C.; Vaulont, S.; Peyssonnaux, C. HIF-2α, but not HIF-1α, promotes iron absorption in mice. J. Clin. Investig. 2009, 119, 1159–1166. [Google Scholar] [CrossRef] [PubMed]
- Das, N.; Xie, L.; Ramakrishnan, S.K.; Campbell, A.; Rivella, S.; Shah, Y.M. Intestine-specific Disruption of Hypoxia-inducible Factor (HIF)-2α Improves Anemia in Sickle Cell Disease. J. Biol. Chem. 2015, 290, 23523–23527. [Google Scholar] [CrossRef] [PubMed]
- Anderson, E.R.; Taylor, M.; Xue, X.; Ramakrishnan, S.K.; Martin, A.; Xie, L.; Bredell, B.X.; Gardenghi, S.; Rivella, S.; Shah, Y.M. Intestinal HIF2α promotes tissue-iron accumulation in disorders of iron overload with anemia. Proc. Natl. Acad. Sci. USA 2013, 110, E4922–E4930. [Google Scholar] [CrossRef] [PubMed]
- Xie, C.; Yagai, T.; Luo, Y.; Liang, X.; Chen, T.; Wang, Q.; Sun, D.; Zhao, J.; Ramakrishnan, S.K.; Sun, L.; et al. Activation of intestinal hypoxia-inducible factor 2α during obesity contributes to hepatic steatosis. Nat. Med. 2017, 23, 1298–1308. [Google Scholar] [CrossRef] [PubMed]
- Anderson, E.R.; Xue, X.; Shah, Y.M. Intestinal hypoxia-inducible factor-2α (HIF-2α) is critical for efficient erythropoiesis. J. Biol. Chem. 2011, 286, 19533–19540. [Google Scholar] [CrossRef]
- Lambert, S.A.; Jolma, A.; Campitelli, L.F.; Das, P.K.; Yin, Y.; Albu, M.; Chen, X.; Taipale, J.; Hughes, T.R.; Weirauch, M.T. The Human Transcription Factors. Cell 2018, 172, 650–665. [Google Scholar] [CrossRef]
- Liu, Y.-S.; Huang, H.; Zhou, S.-M.; Tian, H.-J.; Li, P. Excessive Iron Availability Caused by Disorders of Interleukin-10 and Interleukin-22 Contributes to High Altitude Polycythemia. Front. Physiol. 2018, 9, 548. [Google Scholar] [CrossRef]
- Brothers, M.D.; Doan, B.K.; Zupan, M.F.; Wile, A.L.; Wilber, R.L.; Byrnes, W.C.; Barnes, K.R.; Kilding, A.E.; Hamid, N.A.; Azidin, R.M.F.R.; et al. Hematological and physiological adaptations following 46 weeks of moderate altitude residence. High Alt. Med. Biol. 2010, 11, 199–208. [Google Scholar] [CrossRef]
- Northrop-Clewes, C.A.; Thurnham, D.I. Biomarkers for the differentiation of anemia and their clinical usefulness. J. Blood Med. 2013, 4, 11–22. [Google Scholar] [CrossRef]
- Salvin, H.E.; Pasricha, S.-R.; Marks, D.C.; Speedy, J. Iron deficiency in blood donors: A national cross-sectional study. Transfusion 2014, 54, 2434–2444. [Google Scholar] [CrossRef] [PubMed]
- Painschab, M.S.; Malpartida, G.E.; Dávila-Roman, V.G.; Gilman, R.H.; Kolb, T.M.; León-Velarde, F.; Miranda, J.J.; Checkley, W. Association between serum concentrations of hypoxia inducible factor responsive proteins and excessive erythrocytosis in high altitude Peru. High Alt. Med. Biol. 2015, 16, 26–33. [Google Scholar] [CrossRef] [PubMed]
- Ge, R.; Simonson, T.S.; Gordeuk, V.; Prchal, J.T.; McClain, D.A. Metabolic aspects of high-altitude adaptation in Tibetans. Exp. Physiol. 2015, 100, 1247–1255. [Google Scholar] [CrossRef]
- Mastrogiannaki, M.; Matak, P.; Delga, S.; Deschemin, J.-C.; Vaulont, S.; Peyssonnaux, C. Deletion of HIF-2α in the enterocytes decreases the severity of tissue iron loading in hepcidin knockout mice. Blood 2012, 119, 587–590. [Google Scholar] [CrossRef] [PubMed]
- Taylor, M.; Qu, A.; Anderson, E.R.; Matsubara, T.; Martin, A.; Gonzalez, F.J.; Shah, Y.M. Hypoxia-inducible factor-2α mediates the adaptive increase of intestinal ferroportin during iron deficiency in mice. Gastroenterology 2011, 140, 2044–2055. [Google Scholar] [CrossRef] [PubMed]
- Ramakrishnan, S.K.; Anderson, E.R.; Martin, A.; Centofanti, B.; Shah, Y.M. Maternal intestinal HIF-2α is necessary for sensing iron demands of lactation in mice. Proc. Natl. Acad. Sci. USA 2015, 112, E3738–E3747. [Google Scholar] [CrossRef] [PubMed]
- Lee, F.S.; Percy, M.J. The HIF pathway and erythrocytosis. Annu. Rev. Pathol. Mech. Dis. 2011, 6, 165–192. [Google Scholar] [CrossRef]
- Wallace, E.M.; Rizzi, J.P.; Han, G.; Wehn, P.M.; Cao, Z.; Du, X.; Cheng, T.; Czerwinski, R.M.; Dixon, D.D.; Goggin, B.S.; et al. A Small-Molecule Antagonist of HIF2α Is Efficacious in Preclinical Models of Renal Cell Carcinoma. Cancer Res. 2016, 76, 5491–5500. [Google Scholar] [CrossRef]
- Cho, H.; Du, X.; Rizzi, J.P.; Liberzon, E.; Chakraborty, A.A.; Gao, W.; Carvo, I.; Signoretti, S.; Bruick, R.K.; Josey, J.A.; et al. On-target efficacy of a HIF-2α antagonist in preclinical kidney cancer models. Nature 2016, 539, 107–111. [Google Scholar] [CrossRef]
- Chen, W.; Hill, H.; Christie, A.; Kim, M.S.; Holloman, E.; Pavia-Jimenez, A.; Homayoun, F.; Ma, Y.; Patel, N.; Yell, P.; et al. Targeting renal cell carcinoma with a HIF-2 antagonist. Nature 2016, 539, 112–117. [Google Scholar] [CrossRef]
- Camaschella, C. Iron-Deficiency Anemia. N. Engl. J. Med. 2015, 372, 1832–1843. [Google Scholar] [CrossRef] [PubMed]
- de Back, D.Z.; Kostova, E.B.; van Kraaij, M.; van den Berg, T.K.; van Bruggen, R. Of macrophages and red blood cells; a complex love story. Front. Physiol. 2014, 5, 9. [Google Scholar] [CrossRef] [PubMed]
- Mathieu, J.R.; Heinis, M.; Zumerle, S.; Delga, S.; Le Bon, A.; Peyssonnaux, C. Investigating the real role of HIF-1 and HIF-2 in iron recycling by macrophages. Haematologica 2014, 99, e112–e114. [Google Scholar] [CrossRef] [PubMed]
- Peng, Y.; Cui, C.; He, Y.; Ouzhuluobu; Zhang, H.; Yang, D.; Zhang, Q.; Bianbazhuoma; Yang, L.; He, Y.; et al. Down-Regulation of EPAS1 Transcription and Genetic Adaptation of Tibetans to High-Altitude Hypoxia. Mol. Biol. Evol. 2017, 34, 818–830. [Google Scholar] [CrossRef] [PubMed]

| Species | Gene | Forward Primer | Reverse Primer |
|---|---|---|---|
| Mouse | -actin | CTACCTCATGAAGATCCTGACC | CACAGCTTCTCTTTGATGTCAC |
| HIF-2a | GAGAACCTGACTCTCAAAAACG | GTTGTTGTAGACTCTCACTTGC | |
| Dmt1 | TTTTGGACAAATATGGCTTGCG | TACTCATATCCAAACGTGAGGG | |
| Dcytb | GTGTTTGAGTACCACAATGTCC | TGGAAGCAGAAAGACGAAAAAG | |
| Fpn | TTGTGTGTGATCTCCGTATTCA | GTTGTAAAGACGGTCTCAGGTA | |
| Tfrc | TCACACTCTCTCAGCTTTAGTG | TGGTTTCTGAAGAGGGTTTCAT | |
| Fth | TAAAGAAACCAGACCGTGATGA | ATTCACACTCTTTTCCAAGTGC | |
| Cxcl1 | GGCTGGGATTCACCTCAAGAACATC | TGAGTGTGGCTATGACTTCGGTTTG | |
| Steap4 | CCTCTGTGCTGTGCGTCTTCTTC | ACACGATTCGGGATGGAAATGGC | |
| Human | -ACTIN | GGCACCACACCTTCTACAATGAGC | GATAGCACAGCCTGGATAGCAACG |
| HIF-1a | CCATTAGAAAGCAGTTCCGCAAGC | GTGGTAGTGGTGGCATTAGCAGTAG | |
| HIF-2a | ATCAGCAAGTTCATGGGACTTA | AAACCAGAGCCATTTTTGAGAC | |
| DMT1 | CATCCTCACATTTACGAGCTTG | CCAACCCAAGTAGAACACAAAG | |
| DCYTB | GCCAGAAGGTGTTTTCGTAAAT | TGGTAGAATTTGGCTCCTTAGG | |
| FPN | ACAATACGAAGGATTGACCAGT | ATACCAAGTTCCATCCCGAAAT | |
| TFRC | TGAACCAATACAGAGCAGACAT | GTTTTCTCAGCATTCCCGAAAT | |
| FTH | CTCCTACGTTTACCTGTCCATG | CAAGTCATCAGGCACATACAAG |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, S.; Yan, J.; Song, K.; Ge, R.-L. High-Altitude Hypoxia Induces Excessive Erythrocytosis in Mice via Upregulation of the Intestinal HIF2a/Iron-Metabolism Pathway. Biomedicines 2023, 11, 2992. https://doi.org/10.3390/biomedicines11112992
Zhou S, Yan J, Song K, Ge R-L. High-Altitude Hypoxia Induces Excessive Erythrocytosis in Mice via Upregulation of the Intestinal HIF2a/Iron-Metabolism Pathway. Biomedicines. 2023; 11(11):2992. https://doi.org/10.3390/biomedicines11112992
Chicago/Turabian StyleZhou, Sisi, Jun Yan, Kang Song, and Ri-Li Ge. 2023. "High-Altitude Hypoxia Induces Excessive Erythrocytosis in Mice via Upregulation of the Intestinal HIF2a/Iron-Metabolism Pathway" Biomedicines 11, no. 11: 2992. https://doi.org/10.3390/biomedicines11112992
APA StyleZhou, S., Yan, J., Song, K., & Ge, R.-L. (2023). High-Altitude Hypoxia Induces Excessive Erythrocytosis in Mice via Upregulation of the Intestinal HIF2a/Iron-Metabolism Pathway. Biomedicines, 11(11), 2992. https://doi.org/10.3390/biomedicines11112992




