HER-2 Expression in Colorectal Cancer and Its Correlation with Immune Cell Infiltration
Abstract
:1. Introduction
2. Materials and Methods
2.1. Clinical Samples
2.2. Immunohistochemistry (IHC)
2.3. Immunofluorescence Staining
2.4. Quantification and Statistical Analysis
3. Results
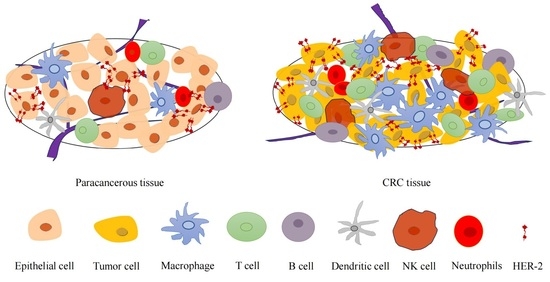
3.1. Increased HER-2 Expression and Increased Number of Immune Cells in CRC Tissues Compared to Paracancerous Tissues
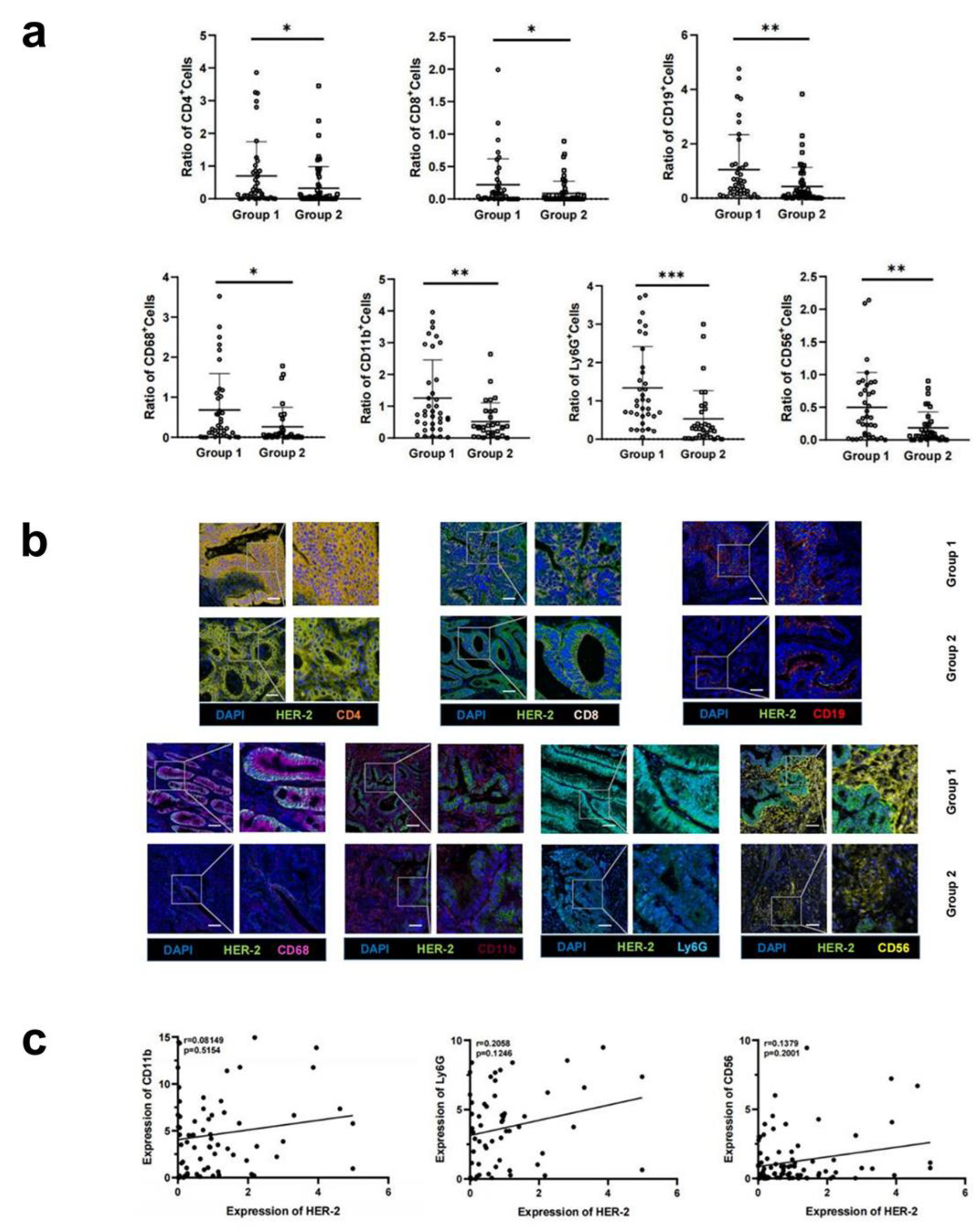
3.2. Increased HER-2 Expression in CRC Tissues Is Accompanied by Increased Infiltration of Immune Cells
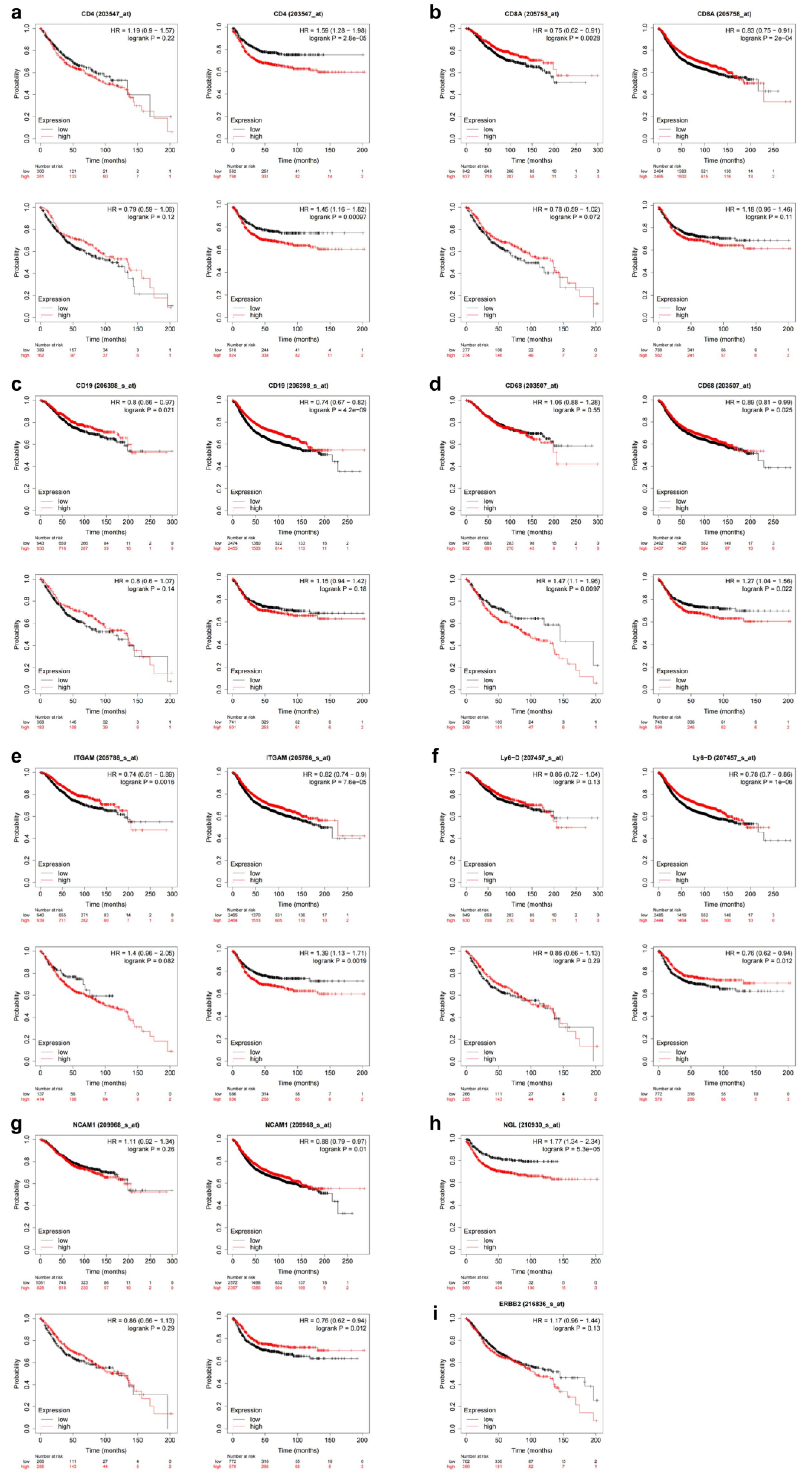
3.3. Upregulation of HER-2 Expression Is a Risk Factor for Prognosis in CRC Patients
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F.; Bsc, M.F.B.; Me, J.F.; Soerjomataram, M.I.; et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics, 2022. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef]
- Richman, S.D.; Southward, K.; Chambers, P.; Cross, D.; Barrett, J.; Hemmings, G.; Taylor, M.; Wood, H.; Hutchins, G.; Foster, J.M.; et al. HER2 overexpression and amplification as a potential therapeutic target in colorectal cancer: Analysis of 3256 patients enrolled in the QUASAR, FOCUS and PICCOLO colorectal cancer trials. J. Pathol. 2016, 238, 562–570. [Google Scholar] [CrossRef]
- Siena, S.; Sartore-Bianchi, A.; Marsoni, S.; Hurwitz, H.; McCall, S.; Penault-Llorca, F.; Srock, S.; Bardelli, A.; Trusolino, L. Targeting the human epidermal growth factor receptor 2 (HER2) oncogene in colorectal cancer. Ann. Oncol. 2018, 29, 1108–1119. [Google Scholar] [CrossRef]
- Eiermann, W. Trastuzumab combined with chemotherapy for the treatment of HER2-positive metastatic breast cancer: Pivotal trial data. Ann. Oncol. 2001, 12 (Suppl. 1), S57–S62. [Google Scholar] [CrossRef]
- Bang, Y.-J.; Van Cutsem, E.; Feyereislova, A.; Chung, H.C.; Shen, L.; Sawaki, A.; Lordick, F.; Ohtsu, A.; Omuro, Y.; Satoh, T.; et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): A phase 3, open-label, randomised controlled trial. Lancet 2010, 376, 687–697. [Google Scholar] [CrossRef]
- Keam, S.J. Trastuzumab Deruxtecan: First Approval. Drugs 2020, 80, 501–508. [Google Scholar] [CrossRef]
- Sartore-Bianchi, A.; Trusolino, L.; Martino, C.; Bencardino, K.; Lonardi, S.; Bergamo, F.; Zagonel, V.; Leone, F.; Depetris, I.; Martinelli, E.; et al. Dual-targeted therapy with trastuzumab and lapatinib in treatment-refractory, KRAS codon 12/13 wild-type, HER2-positive metastatic colorectal cancer (HERACLES): A proof-of-concept, multicentre, open-label, phase 2 trial. Lancet Oncol. 2016, 17, 738–746. [Google Scholar] [CrossRef]
- Siena, S.; Di Bartolomeo, M.; Raghav, K.; Masuishi, T.; Loupakis, F.; Kawakami, H.; Yamaguchi, K.; Nishina, T.; Fakih, M.; Elez, E.; et al. Trastuzumab deruxtecan (DS-8201) in patients with HER2-expressing metastatic colorectal cancer (DESTINY-CRC01): A multicentre, open-label, phase 2 trial. Lancet Oncol. 2021, 22, 779–789. [Google Scholar] [CrossRef]
- Strickler, J.H.; Yoshino, T.; Graham, R.P.; Siena, S.; Bekaii-Saab, T. Diagnosis and Treatment of ERBB2-Positive Metastatic Colorectal Cancer: A Review. JAMA Oncol. 2022, 8, 760–769. [Google Scholar] [CrossRef]
- Clifton, G.T.; Peoples, A.G.E. Immunotherapy as a partner for HER2-directed therapies. Expert Rev. Anticancer. Ther. 2021, 21, 739–746. [Google Scholar] [CrossRef]
- Pagès, F.; Mlecnik, B.; Marliot, F.; Bindea, G.; Ou, F.-S.; Bifulco, C.; Lugli, A.; Zlobec, I.; Rau, T.T.; Berger, M.D.; et al. International validation of the consensus Immunoscore for the classification of colon cancer: A prognostic and accuracy study. Lancet 2018, 391, 2128–2139. [Google Scholar] [CrossRef]
- Mlecnik, B.; Van Den Eynde, M.; Bindea, G.; Church, S.E.; Vasaturo, A.; Fredriksen, T.; Lafontaine, L.; Haicheur, N.; Marliot, F.; Debetancourt, D.; et al. Comprehensive Intrametastatic Immune Quantification and Major Impact of Immunoscore on Survival. J. Natl. Cancer Inst. 2018, 110, 97–108. [Google Scholar] [CrossRef]
- Denkert, C.; Von Minckwitz, G.; Darb-Esfahani, S.; Lederer, B.; Heppner, B.I.; Weber, K.E.; Budczies, J.; Huober, J.; Klauschen, F.; Furlanetto, J.; et al. Tumour-infiltrating lymphocytes and prognosis in different subtypes of breast cancer: A pooled analysis of 3771 patients treated with neoadjuvant therapy. Lancet Oncol. 2018, 19, 40–50. [Google Scholar] [CrossRef]
- Nuciforo, P.; Pascual, T.; Cortés, J.; Llombart-Cussac, A.; Fasani, R.; Paré, L.; Oliveira, M.; Galvan, P.; Martínez, N.; Bermejo, B.; et al. A predictive model of pathologic response based on tumor cellularity and tumor-infiltrating lymphocytes (CelTIL) in HER2-positive breast cancer treated with chemo-free dual HER2 blockade. Ann. Oncol. 2018, 29, 170–177. [Google Scholar] [CrossRef]
- Griguolo, G.; Pascual, T.; Dieci, M.V.; Guarneri, V.; Prat, A. Interaction of host immunity with HER2-targeted treatment and tumor heterogeneity in HER2-positive breast cancer. J. Immunother. Cancer 2019, 7, 90. [Google Scholar] [CrossRef]
- Slamon, D.J.; Clark, G.M.; Wong, S.G.; Levin, W.J.; Ullrich, A.; McGuire, W.L. Human breast cancer: Correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science 1987, 235, 177–182. [Google Scholar] [CrossRef]
- National Health Commission of the People’s Republic of China; Chinese Society of Oncology. Chinese protocol of diagnosis and treatment of colorectal cancer of the National Health Commission (2023 edition)]. Zhonghua Wei Chang Wai Ke Za Zhi 2023, 26, 505–528. [Google Scholar]
- Zhao, Y.; Zhang, W.; Huo, M.; Wang, P.; Liu, X.; Wang, Y.; Li, Y.; Zhou, Z.; Xu, N.; Zhu, H. XBP1 regulates the protumoral function of tumor-associated macrophages in human colorectal cancer. Signal Transduct. Target. Ther. 2021, 6, 357. [Google Scholar] [CrossRef]
- Valtorta, E.; Martino, C.; Sartore-Bianchi, A.; Penaullt-Llorca, F.; Viale, G.; Risio, M.; Rugge, M.; Grigioni, W.; Bencardino, K.; Lonardi, S.; et al. Assessment of a HER2 scoring system for colorectal cancer: Results from a validation study. Mod. Pathol. 2015, 28, 1481–1491. [Google Scholar] [CrossRef]
- Lánczky, A.; Győrffy, B. Web-Based Survival Analysis Tool Tailored for Medical Research (KMplot): Development and Implementation. J. Med. Internet Res. 2021, 23, e27633. [Google Scholar] [CrossRef]
- Győrffy, B. Survival analysis across the entire transcriptome identifies biomarkers with the highest prognostic power in breast cancer. Comput. Struct. Biotechnol. J. 2021, 19, 4101–4109. [Google Scholar] [CrossRef]
- Benson, A.B.; Venook, A.P.; Al-Hawary, M.M.; Cederquist, L.; Chen, Y.J.; Ciombor, K.K.; Cohen, S.; Cooper, H.S.; Deming, D.; Engstrom, P.F.; et al. NCCN Guidelines Insights: Colon Cancer, Version 2.2018. J. Natl. Compr. Cancer Netw. 2018, 16, 359–369. [Google Scholar] [CrossRef]
- Benson, A.B.; Venook, A.P.; Al-Hawary, M.M.; Arain, M.A.; Chen, Y.J.; Ciombor, K.K.; Cohen, S.; Cooper, H.S.; Deming, D.; Farkas, L.; et al. Colon Cancer, Version 2.2021, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2021, 19, 329–359. [Google Scholar] [CrossRef]
- De Cuyper, A.; Eynde, M.V.D.; Machiels, J.-P. HER2 as a Predictive Biomarker and Treatment Target in Colorectal Cancer. Clin. Color. Cancer 2020, 19, 65–72. [Google Scholar] [CrossRef]
- Wu, S.-W.; Ma, C.-C.; Yang, Y. The prognostic value of HER-2/neu overexpression in colorectal cancer: Evidence from 16 studies. Tumour Biol. 2014, 35, 10799–10804. [Google Scholar] [CrossRef]
- Wu, Q.B.; Sun, G.P. Expression of COX-2 and HER-2 in colorectal cancer and their correlation. World J. Gastroenterol. 2015, 21, 6206–6214. [Google Scholar] [CrossRef]
- Li, C.; Liu, D.-R.; Ye, L.-Y.; Huang, L.-N.; Jaiswal, S.; Li, X.-W.; Wang, H.-H.; Chen, L. HER-2 overexpression and survival in colorectal cancer: A meta-analysis. J. Zhejiang Univ. B 2014, 15, 582–589. [Google Scholar] [CrossRef]
- Dieci, M.V.; Miglietta, F.; Guarneri, V. Immune Infiltrates in Breast Cancer: Recent Updates and Clinical Implications. Cells 2021, 10, 223. [Google Scholar] [CrossRef]
- Pernas, S.; Tolaney, S.M. Clinical trial data and emerging strategies: HER2-positive breast cancer. Breast Cancer Res. Treat. 2022, 193, 281–291. [Google Scholar] [CrossRef]
- Harris, S.J.; Brown, J.; Lopez, J.; Yap, T.A. Immuno-oncology combinations: Raising the tail of the survival curve. Cancer Biol. Med. 2016, 13, 171–193. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Jiang, Z.; Mortenson, E.D.; Deng, L.; Radkevich-Brown, O.; Yang, X.; Sattar, H.; Wang, Y.; Brown, N.K.; Greene, M.; et al. The therapeutic effect of anti-HER2/neu antibody depends on both innate and adaptive immunity. Cancer Cell 2010, 18, 160–170. [Google Scholar] [CrossRef] [PubMed]
- Di Modica, M.; Sfondrini, L.; Regondi, V.; Varchetta, S.; Oliviero, B.; Mariani, G.; Bianchi, G.V.; Generali, D.; Balsari, A.; Triulzi, T.; et al. Taxanes enhance trastuzumab-mediated ADCC on tumor cells through NKG2D-mediated NK cell recognition. Oncotarget 2016, 7, 255–265. [Google Scholar] [CrossRef] [PubMed]
- Lasry, A.; Zinger, A.; Ben-Neriah, Y. Inflammatory networks underlying colorectal cancer. Nat. Immunol. 2016, 17, 230–240. [Google Scholar] [CrossRef]
- Gall, V.A.; Philips, A.V.; Qiao, N.; Clise-Dwyer, K.; Perakis, A.A.; Zhang, M.; Clifton, G.T.; Sukhumalchandra, P.; Ma, Q.; Reddy, S.M.; et al. Trastuzumab Increases HER2 Uptake and Cross-Presentation by Dendritic Cells. Cancer Res 2017, 77, 5374–5383. [Google Scholar] [CrossRef]
- Garaud, S.; Buisseret, L.; Solinas, C.; Gu-Trantien, C.; De Wind, A.; Eynden, G.V.D.; Naveaux, C.; Lodewyckx, J.-N.; Boisson, A.; Duvillier, H.; et al. Tumor-infiltrating B cells signal functional humoral immune responses in breast cancer. J. Clin. Investig. 2019, 4, e129641. [Google Scholar] [CrossRef]
- Li, G.-M. Mechanisms and functions of DNA mismatch repair. Cell Res. 2008, 18, 85–98. [Google Scholar] [CrossRef]
- Fan, A.; Wang, B.; Wang, X.; Nie, Y.; Fan, D.; Zhao, X.; Lu, Y. Immunotherapy in colorectal cancer: Current achievements and future perspective. Int. J. Biol. Sci. 2021, 17, 3837–3849. [Google Scholar] [CrossRef]
- Zhang, Q.W.; Liu, L.; Gong, C.-Y.; Shi, H.-S.; Zeng, Y.-H.; Wang, X.-Z.; Zhao, Y.-W.; Wei, Y.-Q. Prognostic Significance of Tumor-Associated Macrophages in Solid Tumor: A Meta-Analysis of the Literature. PLoS ONE 2012, 7, e50946. [Google Scholar] [CrossRef]
- Gunay, F.S.D.; Kırmızı, B.A.; Ensari, A.; İcli, F.; Akbulut, H. Tumor-associated Macrophages and Neuroendocrine Differentiation Decrease the Efficacy of Bevacizumab Plus Chemotherapy in Patients with Advanced Colorectal Cancer. Clin. Color. Cancer 2019, 18, e244–e250. [Google Scholar] [CrossRef]
- Miao, H.; Ou, J.; Peng, Y.; Zhang, X.; Chen, Y.; Hao, L.; Xie, G.; Wang, Z.; Pang, X.; Ruan, Z.; et al. Macrophage ABHD5 promotes colorectal cancer growth by suppressing spermidine production by SRM. Nat. Commun. 2016, 7, 11716. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, S.R.; Schmid, M.C. Macrophages as Key Drivers of Cancer Progression and Metastasis. Mediat. Inflamm. 2017, 2017, 9624760. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; You, D.; Jeong, Y.; Yoon, S.Y.; Kim, S.A.; Kim, S.W.; Nam, S.J.; Lee, J.E. WNT5A augments cell invasiveness by inducing CXCL8 in HER2-positive breast cancer cells. Cytokine 2020, 135, 155213. [Google Scholar] [CrossRef]
- Yuan, Q.; Deng, D.; Pan, C.; Ren, J.; Wei, T.; Wu, Z.; Zhang, B.; Li, S.; Yin, P.; Shang, D. Integration of transcriptomics, proteomics, and metabolomics data to reveal HER2-associated metabolic heterogeneity in gastric cancer with response to immunotherapy and neoadjuvant chemotherapy. Front. Immunol. 2022, 13, 951137. [Google Scholar] [CrossRef]
- Mohamed, M.M.; El-Ghonaimy, E.A.; Nouh, M.A.; Schneider, R.J.; Sloane, B.F.; El-Shinawi, M. Cytokines secreted by macrophages isolated from tumor microenvironment of inflammatory breast cancer patients possess chemotactic properties. Int. J. Biochem. Cell Biol. 2014, 46, 138–147. [Google Scholar] [CrossRef]
- Ahmed, S.; Mohamed, H.T.; El-Husseiny, N.; El Mahdy, M.M.; Safwat, G.; Diab, A.A.; El-Sherif, A.A.; El-Shinawi, M.; Mohamed, M.M. IL-8 secreted by tumor associated macrophages contribute to lapatinib resistance in HER2-positive locally advanced breast cancer via activation of Src/STAT3/ERK1/2-mediated EGFR signaling. Biochim. Biophys. Acta Mol. Cell Res. 2021, 1868, 118995. [Google Scholar] [CrossRef] [PubMed]

| Cell | Mean ± SD | t-Test | ||
|---|---|---|---|---|
| HER-2-Upregulated | HER-2-Non-Upregulated | t | p | |
| CD4+ | 0.70 ± 0.37 | 0.32 ± 0.17 | 2.15 | 0.03 |
| CD8+ | 0.22 ± 0.13 | 0.09 ± 0.06 | 2.18 | 0.03 |
| CD68+ | 0.31 ± 0.19 | 0.12 ± 0.08 | 2.41 | 0.02 |
| CD19+ | 1.05 ± 0.62 | 0.43 ± 0.21 | 3.02 | <0.01 |
| LY6G+ | 1.34 ± 0.81 | 0.53 ± 0.23 | 3.58 | <0.01 |
| CD56+ | 0.50 ± 0.31 | 0.19 ± 0.1 | 3.20 | <0.01 |
| CD11b+ | 1.26 ± 0.74 | 0.52 ± 0.24 | 3.11 | <0.01 |
| Factor | Variables | Proportion |
|---|---|---|
| Age | ≥60 | 50 (51.5%) |
| <60 | 47 (48.5%) | |
| Gender | Male | 57 (58.9%) |
| Female | 40 (41.2%) | |
| Tumor position | Ascending colon | 12 (12.4%) |
| Transverse colon | 1 (1.0%) | |
| Descending colon | 11 (11.3%) | |
| Sigmoid colon | 25 (25.8%) | |
| Rectum | 48 (49.5%) | |
| T Stage | 1 | 3 (3.1%) |
| 2 | 21 (21.6%) | |
| 3 | 42 (43.3%) | |
| 4 | 31 (32.0%) | |
| N Stage | 0 | 49 (50.5%) |
| 1 | 30 (30.9%) | |
| 2 | 18 (18.6%) | |
| M Stage | 0 | 94 (96.9%) |
| 1 | 3 (3.1%) | |
| Lymphovascular invasion | Yes | 32 (33.0%) |
| No | 65 (67.0%) | |
| Large vessel invasion | Yes | 15 (15.5%) |
| No | 82 (84.5%) | |
| Tumor budding | Yes | 24 (24.7%) |
| No | 73 (75.3%) | |
| Peripheral nerve invasion | Yes | 32 (33.0%) |
| No | 65 (67.0%) | |
| CEA (0~5 ng/mL) | <5 | 59 (60.8%) |
| ≥5 | 38 (39.2%) | |
| HER-2 | − | 48 (49.5%) |
| + | 39 (40.2%) | |
| ++ | 7 (7.2%) | |
| +++ | 3 (3.1%) | |
| Differentiation | 1 | 9 (9.3%) |
| 2 | 20 (20.6%) | |
| 3 | 64 (66.0%) | |
| 4 | 2 (2.1%) | |
| 5 | 2 (2.1%) | |
| Chemotherapy | Yes | 83 (85.6%) |
| No | 14 (14.4%) | |
| 5-year recurrence-free survival (Recurrence event = 1) | 0 | 73 (75.3%) |
| 1 | 24 (24.7%) |
| Variables | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| p | HR (95% CI) | p | HR (95% CI) | |
| Age | 0.485 | 0.987 (0.953–1.023) | ||
| Gender | 0.651 | 1.208 (0.533–2.736) | ||
| Tumor position | 0.583 | 1.093 (0.794–1.506) | ||
| T stage | 0.037 | 1.804 (1.024–3.179) | 0.924 | 1.031 (0.554–1.919) |
| N stage | 0.001 | 2.454 (1.434–4.199) | 0.001 | 3.238 (1.648–6.363) |
| M stage | 0.001 | 13.182 (2.777–62.578) | 0.001 | 97.428 (5.881–1613.942) |
| Lymphovascular invasion | 0.918 | 1.048 (0.433–2.534) | ||
| Large vessel invasion | 0.102 | 2.269 (0.827–6.224) | ||
| Tumor budding | 0.100 | 2.185 (0.861–5.547) | ||
| Peripheral nerve invasion | 0.078 | 2.104 (0.921–4.806) | ||
| CEA (0~5 ng/mL) | 0.004 | 1.007 (1.002–1.011) | 0.838 | 0.999 (0.992–1.007) |
| HER-2 | 0.047 | 2.317 (1.011–5.309) | 0.009 | 3.421 (1.359–8.613) |
| Differentiation | 0.426 | 0.807 (0.476–1.368) | ||
| Chemotherapy | 0.513 | 0.698 (0.238–2.048) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, D.; Wang, B.; Li, Y.; Zhang, J.; Gong, X.; Qin, H.; Wang, Y.; Zhao, Y.; Wang, Y. HER-2 Expression in Colorectal Cancer and Its Correlation with Immune Cell Infiltration. Biomedicines 2023, 11, 2889. https://doi.org/10.3390/biomedicines11112889
Yang D, Wang B, Li Y, Zhang J, Gong X, Qin H, Wang Y, Zhao Y, Wang Y. HER-2 Expression in Colorectal Cancer and Its Correlation with Immune Cell Infiltration. Biomedicines. 2023; 11(11):2889. https://doi.org/10.3390/biomedicines11112889
Chicago/Turabian StyleYang, Di, Bo Wang, Yinuo Li, Jingyao Zhang, Xuantong Gong, Hao Qin, Yan Wang, Yahui Zhao, and Yong Wang. 2023. "HER-2 Expression in Colorectal Cancer and Its Correlation with Immune Cell Infiltration" Biomedicines 11, no. 11: 2889. https://doi.org/10.3390/biomedicines11112889
APA StyleYang, D., Wang, B., Li, Y., Zhang, J., Gong, X., Qin, H., Wang, Y., Zhao, Y., & Wang, Y. (2023). HER-2 Expression in Colorectal Cancer and Its Correlation with Immune Cell Infiltration. Biomedicines, 11(11), 2889. https://doi.org/10.3390/biomedicines11112889