Combined Transcutaneous Electrical Spinal Cord Stimulation and Task-Specific Rehabilitation Improves Trunk and Sitting Functions in People with Chronic Tetraplegia
Abstract
:1. Introduction
2. Methods
2.1. Study Participants
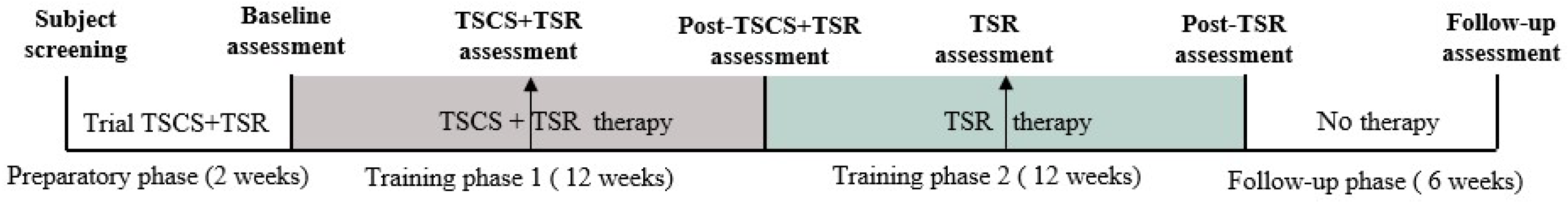
2.2. Study Design
2.3. Experimental Protocol
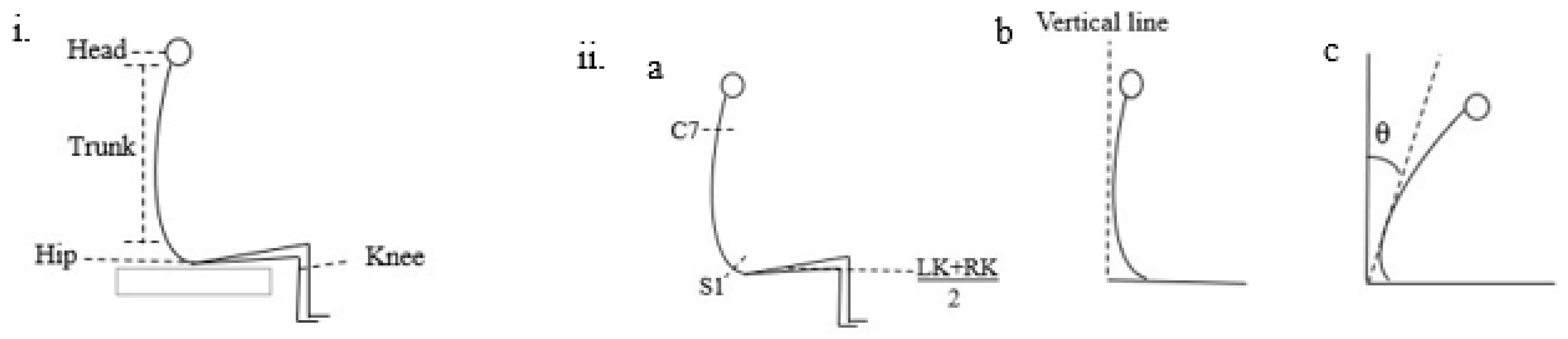
2.4. Outcome Measures
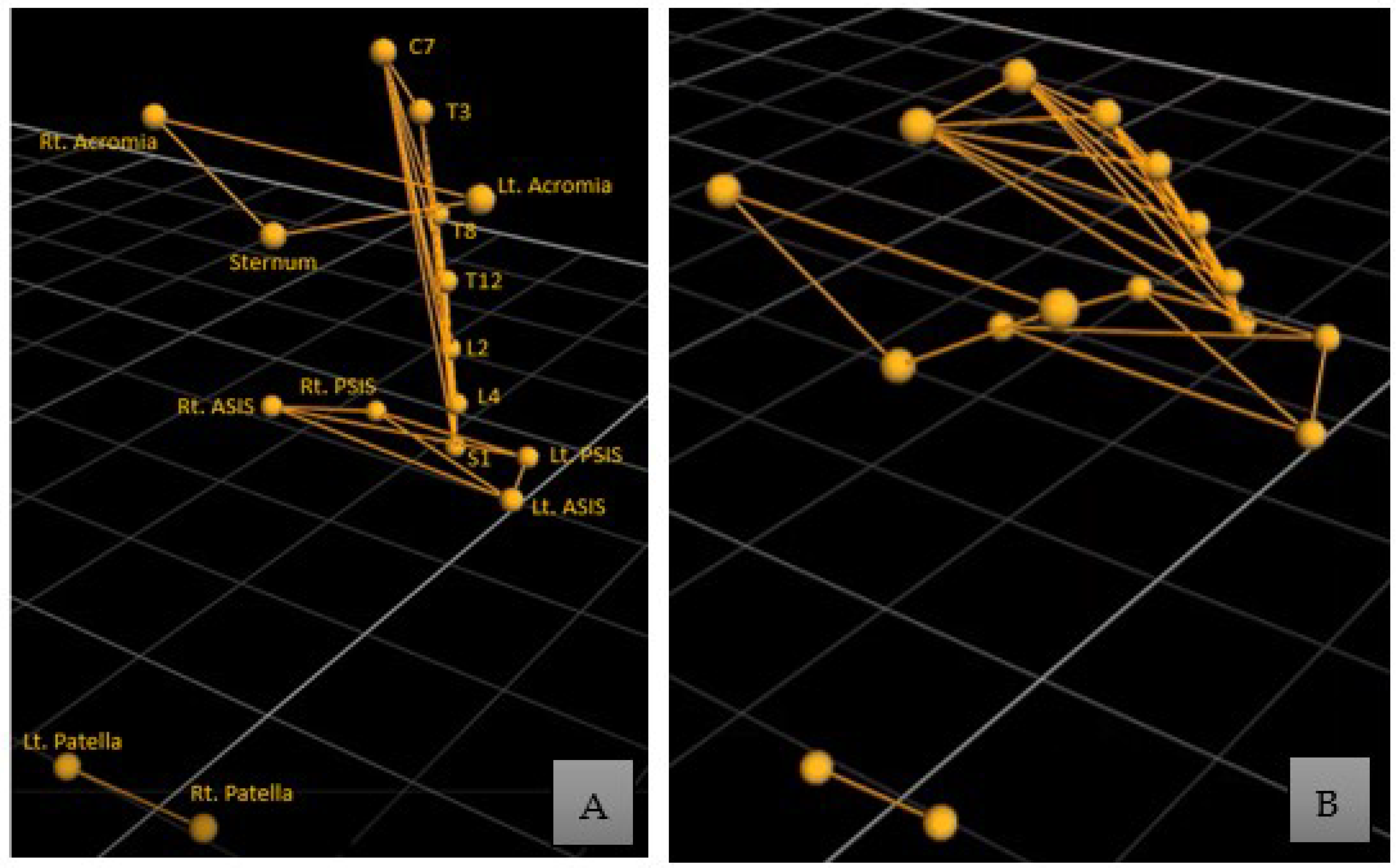
2.5. Vicon Marker and EMG Electrode Placement
2.6. Data Processing and Analysis
3. Results
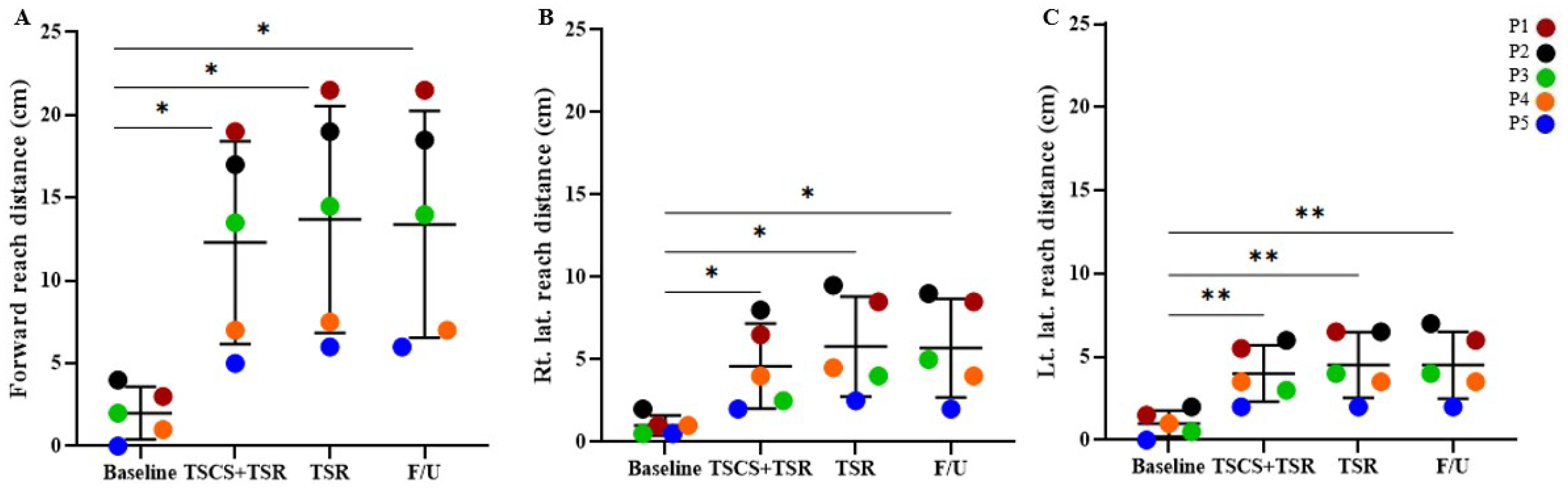
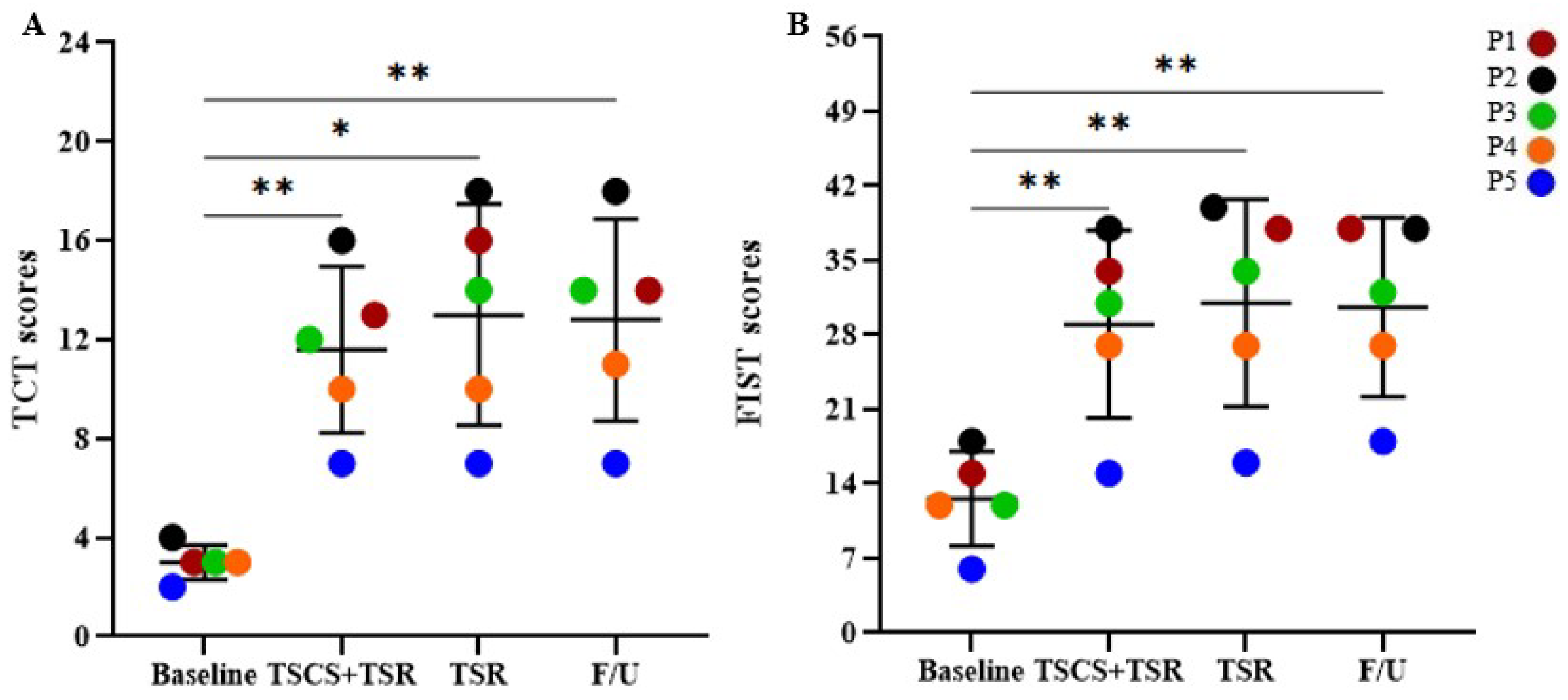
3.1. Combinational Treatment Initiated Functional Improvements in Reaching, Trunk Control, and Sitting Balance
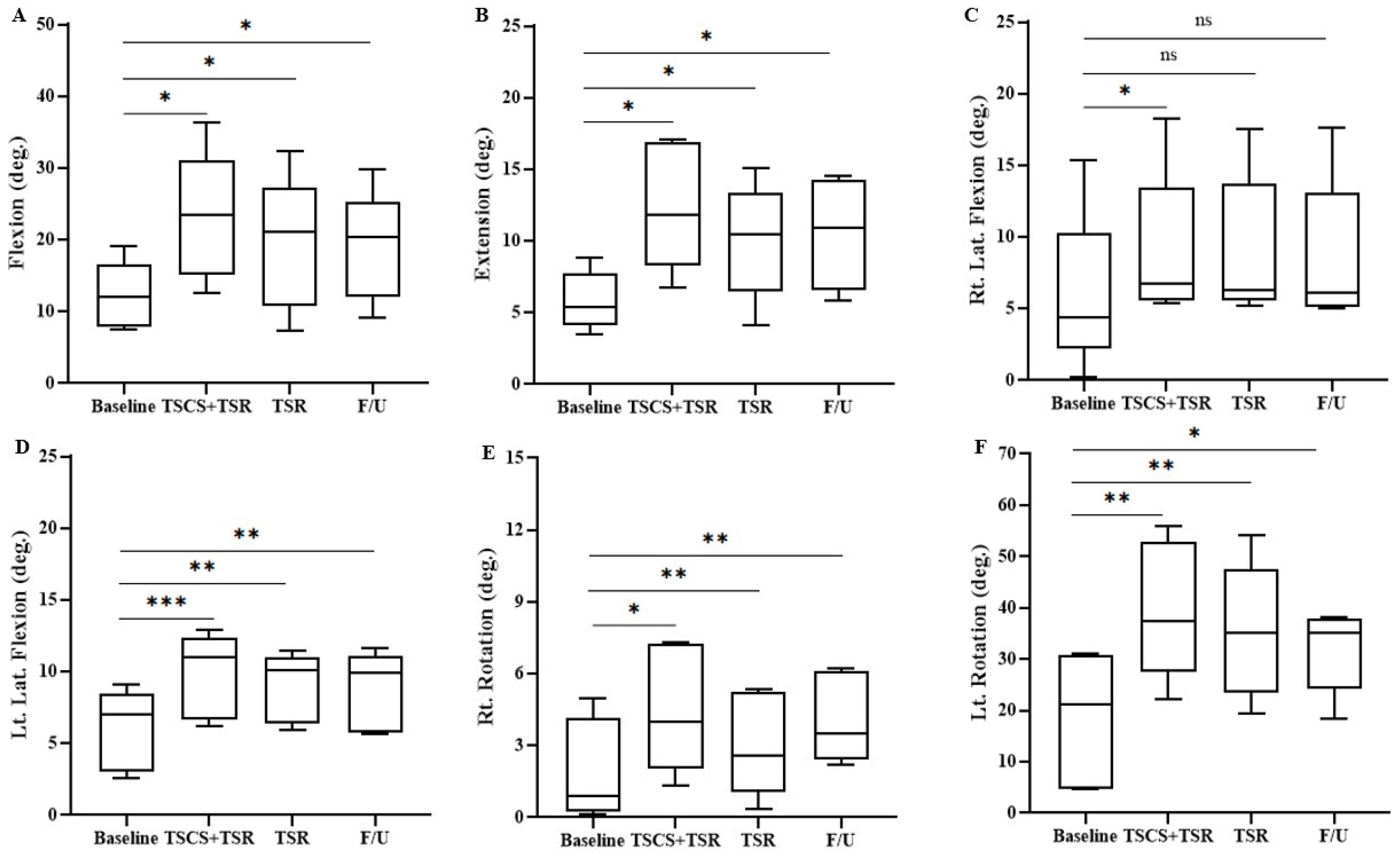
3.2. Increased Trunk Range of Motion after TSCS+TSR Treatment
3.3. Elevated Electromyographic Response of the Trunk Muscles
3.4. Improvements of Trunk Control and Function in Sitting after Combinational Treatment
3.5. Treatment Effect on Sensorimotor Recovery
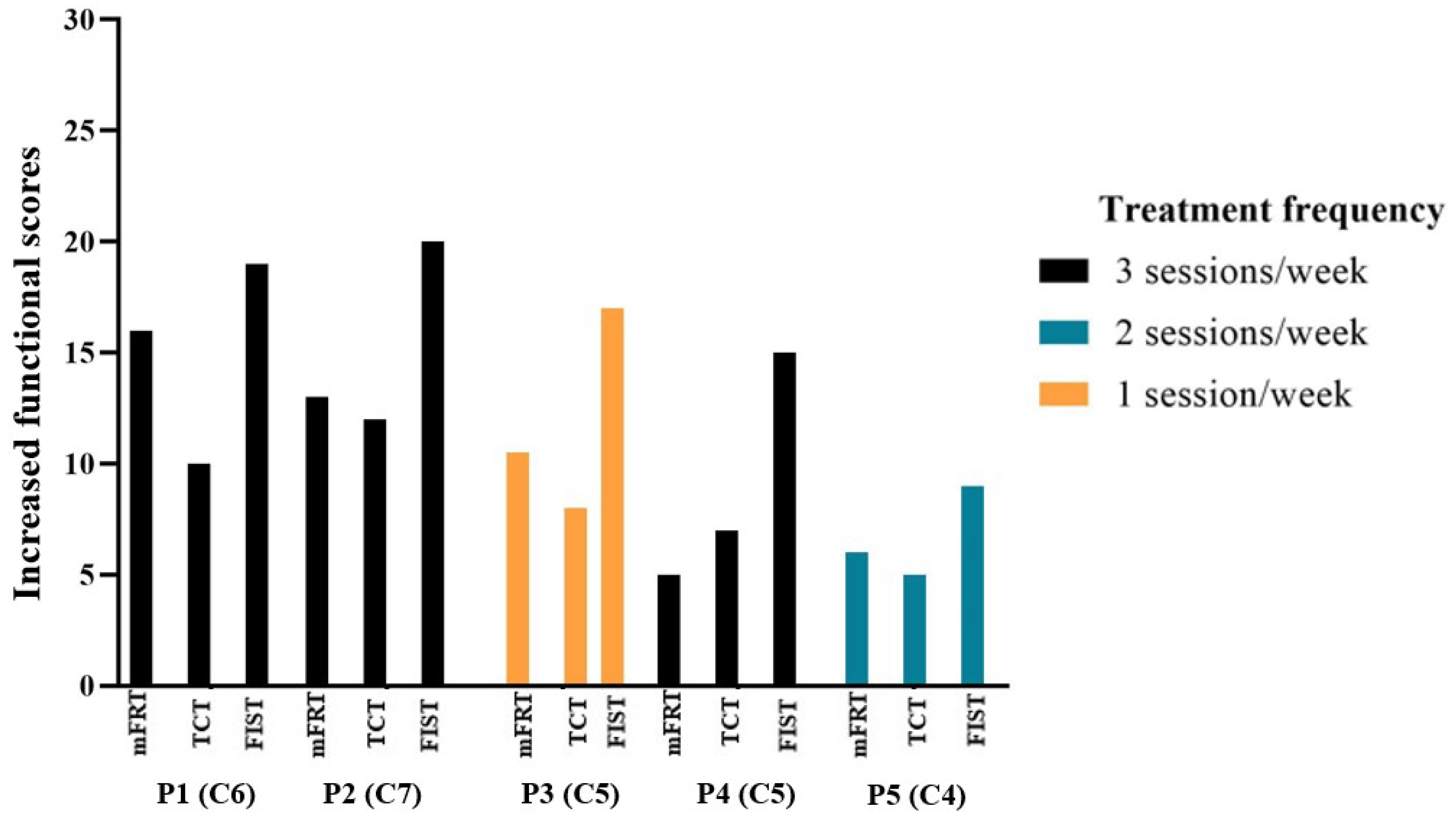
3.6. The Impact of Treatment Frequency on Functional Outcome
4. Discussion
4.1. Functional Reaching Ability in Sitting
4.2. Trunk Control and Seated Postural Stability
4.3. Trunk Muscle EMG Response and Range of Motion
4.4. TSCS and TSR for Sensorimotor Improvement
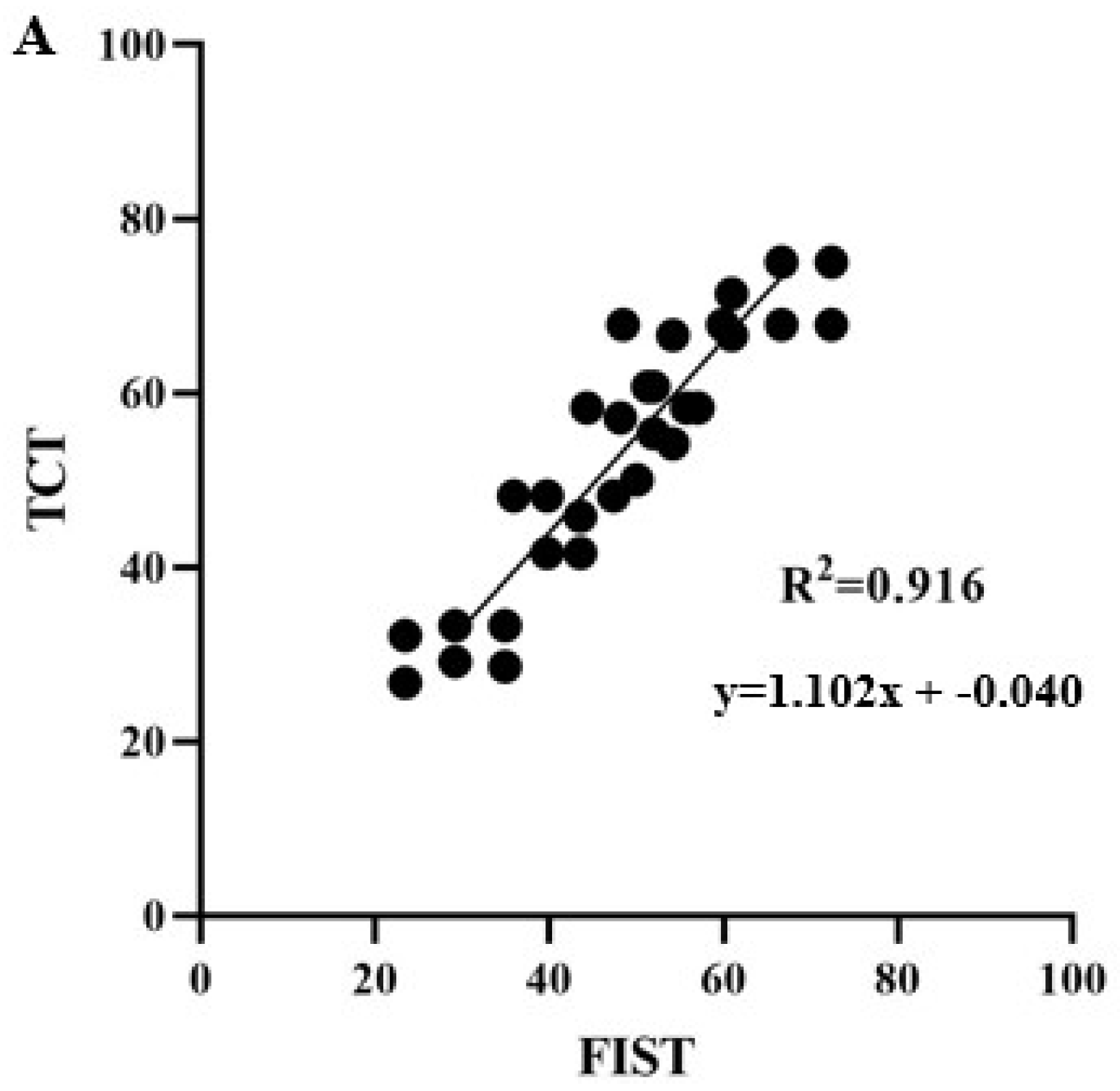
4.5. Relationship between Functional Improvement of mFRT, TCT, and FIST
4.6. Study Limitations and Indications for Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nulle, A.; Tjurina, U.; Erts, R.; Vetra, A. A profile of traumatic spinal cord injury and medical complications in Latvia. Spinal Cord Ser. Cases 2017, 3, 17088. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tharu, N.S.; Alam, M.; Bajracharya, S.; Chaudhary, G.P.; Pandey, J.; Kabir, M.A. Caregivers’ Knowledge, Attitude, and Practice towards Pressure Injuries in Spinal Cord Injury at Rehabilitation Center in Bangladesh. Adv. Orthop. 2022, 2022, 8642900. [Google Scholar] [CrossRef] [PubMed]
- Furlan, J.C.; Sakakibara, B.M.; Miller, W.C.; Krassioukov, A.V. Global incidence and prevalence of traumatic spinal cord injury. Can. J. Neurol. Sci. 2013, 40, 456–464. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Post, M.W.; Dallmeijer, A.J.; Angenot, E.L.; van Asbeck, F.W.; van der Woude, L.H. Duration and functional outcome of spinal cord injury rehabilitation in the Netherlands. J. Rehabil. Res. Dev. 2005, 42, 75. [Google Scholar] [CrossRef] [Green Version]
- Wyndaele, M.; Wyndaele, J.-J. Incidence, prevalence and epidemiology of spinal cord injury: What learns a worldwide literature survey? Spinal Cord 2006, 44, 523–529. [Google Scholar] [CrossRef] [Green Version]
- Alizadeh, A.; Dyck, S.M.; Karimi-Abdolrezaee, S. Traumatic spinal cord injury: An overview of pathophysiology, models and acute injury mechanisms. Front. Neurol. 2019, 10, 282. [Google Scholar] [CrossRef] [Green Version]
- Milosevic, M.; Masani, K.; Kuipers, M.J.; Rahouni, H.; Verrier, M.C.; McConville, K.M.; Popovic, M.R. Trunk control impairment is responsible for postural instability during quiet sitting in individuals with cervical spinal cord injury. Clin. Biomech. 2015, 30, 507–512. [Google Scholar] [CrossRef]
- Triolo, R.J.; Bailey, S.N.; Miller, M.E.; Lombardo, L.M.; Audu, M.L. Effects of stimulating hip and trunk muscles on seated stability, posture, and reach after spinal cord injury. Arch. Phys. Med. Rehabil. 2013, 94, 1766–1775. [Google Scholar] [CrossRef] [Green Version]
- Minkel, J.L. Seating and mobility considerations for people with spinal cord injury. Phys. Ther. 2000, 80, 701–709. [Google Scholar] [CrossRef] [Green Version]
- Chen, C.-L.; Yeung, K.-T.; Bih, L.-I.; Wang, C.-H.; Chen, M.-I.; Chien, J.-C. The relationship between sitting stability and functional performance in patients with paraplegia. Arch. Phys. Med. Rehabil. 2003, 84, 1276–1281. [Google Scholar] [CrossRef]
- Potten, Y.; Seelen, H.; Drukker, J.; Reulen, J.; Drost, M. Postural muscle responses in the spinal cord injured persons during forward reaching. Ergonomics 1999, 42, 1200–1215. [Google Scholar] [CrossRef] [PubMed]
- Rath, M.; Vette, A.H.; Ramasubramaniam, S.; Li, K.; Burdick, J.; Edgerton, V.R.; Sayenko, D.G. Trunk stability enabled by noninvasive spinal electrical stimulation after spinal cord injury. J. Neurotrauma 2018, 35, 2540–2553. [Google Scholar] [CrossRef] [PubMed]
- Milosevic, M. Neuromuscular Control of the Trunk during Sitting Balance; University of Toronto: Toronto, ON, Canada, 2015. [Google Scholar]
- Frasuńska, J.; Tarnacka, B.; Wojdasiewicz, P. Quality of life in patients with tetraplegia and paraplegia after traumatic spinal cord injury. Adv. Psychiatry Neurol. 2020, 29, 143–153. [Google Scholar] [CrossRef]
- Abou, L.; de Freitas, G.R.; Palandi, J.; Ilha, J. Clinical instruments for measuring unsupported sitting balance in subjects with spinal cord injury: A systematic review. Top. Spinal Cord Inj. Rehabil. 2018, 24, 177–193. [Google Scholar] [CrossRef]
- Gao, K.L.; Chan, K.; Purves, S.; Tsang, W.W. Reliability of dynamic sitting balance tests and their correlations with functional mobility for wheelchair users with chronic spinal cord injury. J. Orthop. Transl. 2015, 3, 44–49. [Google Scholar] [CrossRef] [Green Version]
- Elmgreen, S.B.; Krogh, S.; Løve, U.S.; Forman, A.; Kasch, H. Neuromodulation in spinal cord injury rehabilitation. Ugeskr. Laeger 2019, 181, V02190104. [Google Scholar]
- McDonald, J.W.; Sadowsky, C. Spinal-cord injury. Lancet 2002, 359, 417–425. [Google Scholar] [CrossRef]
- Chompoonimit, A.; Nualnetr, N. The impact of task-oriented client-centered training on individuals with spinal cord injury in the community. Spinal Cord 2016, 54, 849–854. [Google Scholar] [CrossRef]
- Lotter, J.K.; Henderson, C.E.; Plawecki, A.; Holthus, M.E.; Lucas, E.H.; Ardestani, M.M.; Hornby, T.G. Task-specific versus impairment-based training on locomotor performance in individuals with chronic spinal cord injury: A randomized crossover study. Neurorehabilit. Neural Repair 2020, 34, 627–639. [Google Scholar] [CrossRef]
- Cunningham, P.; Turton, A.J.; van Wijck, F.; van Vliet, P. Task-specific reach-to-grasp training after stroke: Development and description of a home-based intervention. Clin. Rehabil. 2016, 30, 731–740. [Google Scholar] [CrossRef]
- Tamburella, F.; Scivoletto, G.; Molinari, M. Balance training improves static stability and gait in chronic incomplete spinal cord injury subjects: A pilot study. Eur. J. Phys. Rehabil. Med. 2013, 49, 353–364. [Google Scholar] [PubMed]
- Hubbard, I.J.; Parsons, M.W.; Neilson, C.; Carey, L.M. Task-specific training: Evidence for and translation to clinical practice. Occup. Ther. Int. 2009, 16, 175–189. [Google Scholar] [CrossRef] [PubMed]
- Kloosterman, M.; Snoek, G.; Jannink, M. Systematic review of the effects of exercise therapy on the upper extremity of patients with spinal-cord injury. Spinal Cord 2009, 47, 196–203. [Google Scholar] [CrossRef] [Green Version]
- Edgerton, V.R.; Harkema, S. Epidural stimulation of the spinal cord in spinal cord injury: Current status and future challenges. Expert Rev. Neurother. 2011, 11, 1351–1353. [Google Scholar] [CrossRef] [Green Version]
- Spooren, A.; Janssen-Potten, Y.; Kerckhofs, E.; Bongers, H.; Seelen, H. Evaluation of a task-oriented client-centered upper extremity skilled performance training module in persons with tetraplegia. Spinal Cord 2011, 49, 1049–1054. [Google Scholar] [CrossRef] [Green Version]
- Huie, J.R.; Morioka, K.; Haefeli, J.; Ferguson, A.R. What is being trained? How divergent forms of plasticity compete to shape locomotor recovery after spinal cord injury. J. Neurotrauma 2017, 34, 1831–1840. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sayenko, D.G.; Alekhina, M.I.; Masani, K.; Vette, A.H.; Obata, H.; Popovic, M.R.; Nakazawa, K. Positive effect of balance training with visual feedback on standing balance abilities in people with incomplete spinal cord injury. Spinal Cord 2010, 48, 886–893. [Google Scholar] [CrossRef] [Green Version]
- Tse, C.M.; Chisholm, A.E.; Lam, T.; Eng, J.J. A systematic review of the effectiveness of task-specific rehabilitation interventions for improving independent sitting and standing function in spinal cord injury. J. Spinal Cord Med. 2018, 41, 254–266. [Google Scholar] [CrossRef]
- Jones, M.L.; Evans, N.; Tefertiller, C.; Backus, D.; Sweatman, M.; Tansey, K.; Morrison, S. Activity-based therapy for recovery of walking in chronic spinal cord injury: Results from a secondary analysis to determine responsiveness to therapy. Arch. Phys. Med. Rehabil. 2014, 95, 2247–2252. [Google Scholar] [CrossRef]
- Fisher, C.G.; Noonan, V.K.; Smith, D.E.; Wing, P.C.; Dvorak, M.F.; Kwon, B. Motor recovery, functional status, and health-related quality of life in patients with complete spinal cord injuries. Spine 2005, 30, 2200–2207. [Google Scholar] [CrossRef]
- Chan, S.C.C.; Chan, A.P.S. One-year follow-up of Chinese people with spinal cord injury: A preliminary study. J. Spinal Cord Med. 2013, 36, 12–23. [Google Scholar] [CrossRef] [PubMed]
- Rath, M. Trunk Control and Postural Stability in Individuals with Spinal Cord Injury: Noninvasive Enabling Strategies and Modeling. Ph.D. Thesis, University of California Los Angeles, (UCLA), Los Angeles, CA, USA, 2018. [Google Scholar]
- Rahman, M.A.; Tharu, N.S.; Gustin, S.M.; Zheng, Y.-P.; Alam, M. Trans-Spinal Electrical Stimulation Therapy for Functional Rehabilitation after Spinal Cord Injury. J. Clin. Med. 2022, 11, 1550. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, Z. Trans-spinal direct current stimulation modifies spinal cord excitability through synaptic and axonal mechanisms. Physiol. Rep. 2014, 2, e12157. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taylor, C.; McHugh, C.; Mockler, D.; Minogue, C.; Reilly, R.B.; Fleming, N. Transcutaneous spinal cord stimulation and motor responses in individuals with spinal cord injury: A methodological review. PLoS ONE 2021, 16, e0260166. [Google Scholar] [CrossRef]
- Hofstoetter, U.S.; McKay, W.B.; Tansey, K.E.; Mayr, W.; Kern, H.; Minassian, K. Modification of spasticity by transcutaneous spinal cord stimulation in individuals with incomplete spinal cord injury. J. Spinal Cord Med. 2014, 37, 202–211. [Google Scholar] [CrossRef] [Green Version]
- Calvert, J.S.; Manson, G.A.; Grahn, P.J.; Sayenko, D.G. Preferential activation of spinal sensorimotor networks via lateralized transcutaneous spinal stimulation in neurologically intact humans. J. Neurophysiol. 2019, 122, 2111–2118. [Google Scholar] [CrossRef]
- Gerasimenko, Y.; Gorodnichev, R.; Moshonkina, T.; Sayenko, D.; Gad, P.; Edgerton, V.R. Transcutaneous electrical spinal-cord stimulation in humans. Ann. Phys. Rehabil. Med. 2015, 58, 225–231. [Google Scholar] [CrossRef] [Green Version]
- Minassian, K.; Hofstoetter, U.S.; Danner, S.M.; Mayr, W.; Bruce, J.A.; McKay, W.B.; Tansey, K.E. Spinal rhythm generation by step-induced feedback and transcutaneous posterior root stimulation in complete spinal cord–injured individuals. Neurorehabilit. Neural Repair 2016, 30, 233–243. [Google Scholar] [CrossRef]
- Alam, M.; Ling, Y.T.; Wong, A.Y.; Zhong, H.; Edgerton, V.R.; Zheng, Y.P. Reversing 21 years of chronic paralysis via non-invasive spinal cord neuromodulation: A case study. Ann. Clin. Transl. Neurol. 2020, 7, 829–838. [Google Scholar] [CrossRef]
- Keller, A.; Singh, G.; Sommerfeld, J.H.; King, M.; Parikh, P.; Ugiliweneza, B.; D’Amico, J.; Gerasimenko, Y.; Behrman, A.L. Noninvasive spinal stimulation safely enables upright posture in children with spinal cord injury. Nat. Commun. 2021, 12, 5850. [Google Scholar] [CrossRef]
- Manson, G.; Calvert, J.S.; Ling, J.; Tychhon, B.; Ali, A.; Sayenko, D.G. The relationship between maximum tolerance and motor activation during transcutaneous spinal stimulation is unaffected by the carrier frequency or vibration. Physiol. Rep. 2020, 8, e14397. [Google Scholar] [CrossRef] [PubMed]
- Al’Joboori, Y.; Massey, S.J.; Knight, S.L.; Donaldson, N.N.; Duffell, L.D. The effects of adding transcutaneous spinal cord stimulation (tSCS) to sit-to-stand training in people with spinal cord injury: A pilot study. J. Clin. Med. 2020, 9, 2765. [Google Scholar] [CrossRef] [PubMed]
- Lynch, S.M.; Leahy, P.; Barker, S.P. Reliability of measurements obtained with a modified functional reach test in subjects with spinal cord injury. Phys. Ther. 1998, 78, 128–133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Quinzaños, J.; Villa, A.; Flores, A.; Pérez, R. Proposal and validation of a clinical trunk control test in individuals with spinal cord injury. Spinal Cord 2014, 52, 449–454. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abou, L.; Sung, J.; Sosnoff, J.J.; Rice, L.A. Reliability and validity of the function in sitting test among non-ambulatory individuals with spinal cord injury. J. Spinal Cord Med. 2020, 43, 846–853. [Google Scholar] [CrossRef]
- Pan, G.-S.; Lu, T.-W.; Lin, K.-H. Comparison of arm-trunk movement between complete paraplegic and abled bodied subjects during circle drawing. J. Spine 2014, 3, 265. [Google Scholar] [CrossRef]
- Bjerkefors, A.; Carpenter, M.G.; Cresswell, A.G.; Thorstensson, A. Trunk muscle activation in a person with clinically complete thoracic spinal cord injury. J. Rehabil. Med. 2009, 41, 390–392. [Google Scholar] [CrossRef] [Green Version]
- Sliwinski, M.M.; Akselrad, G.; Alla, V.; Buan, V.; Kaemmerlen, E. Community exercise programing and its potential influence on quality of life and functional reach for individuals with spinal cord injury. J. Spinal Cord Med. 2020, 43, 358–363. [Google Scholar] [CrossRef]
- Gill, M.; Linde, M.; Fautsch, K.; Hale, R.; Lopez, C.; Veith, D.; Calvert, J.; Beck, L.; Garlanger, G.; Edgerton, R.; et al. Epidural electrical stimulation of the lumbosacral spinal cord improves trunk stability during seated reaching in two humans with severe thoracic spinal cord injury. Front. Syst. Neurosci. 2020, 14, 79. [Google Scholar] [CrossRef]
- Brotherton, S.S.; Krause, J.S.; Nietert, P.J. Falls in individuals with incomplete spinal cord injury. Spinal Cord 2007, 45, 37–40. [Google Scholar] [CrossRef] [Green Version]
- Curtis, K.A.; Kindlin, C.M.; Reich, K.M.; White, D.E. Functional reach in wheelchair users: The effects of trunk and lower extremity stabilization. Arch. Phys. Med. Rehabil. 1995, 76, 360–367. [Google Scholar] [CrossRef] [PubMed]
- Thompson, M.; Medley, A. Forward and lateral sitting functional reach in younger, middle-aged, and older adults. J. Geriatr. Phys. Ther. 2007, 30, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Kuipers, M.J. Functional Electrical Stimulation as a Neuroprosthesis for Sitting Balance: Measuring Respiratory Function and Seated Postural Control in Able-Bodied Individuals and Individuals with Spinal Cord Injury. Master’s Thesis, University of Toronto, Toronto, ON, Canada, 2013. [Google Scholar]
- Bergmann, M.; Zahharova, A.; Reinvee, M.; Asser, T.; Gapeyeva, H.; Vahtrik, D. The effect of functional electrical stimulation and therapeutic exercises on trunk muscle tone and dynamic sitting balance in persons with chronic spinal cord injury: A crossover trial. Medicina 2019, 55, 619. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoffman, L.R.; Field-Fote, E.C. Cortical reorganization following bimanual training and somatosensory stimulation in cervical spinal cord injury: A case report. Phys. Ther. 2007, 87, 208–223. [Google Scholar] [CrossRef] [PubMed]
- Bondi, M.; Kalsi-Ryan, S.; Delparte, J.J.; Burns, A.S. Differences in sensorimotor and functional recovery between the dominant and non-dominant upper extremity following cervical spinal cord injury. Spinal Cord 2022, 60, 422–427. [Google Scholar] [CrossRef]
- Seáñez, I.; Capogrosso, M. Motor improvements enabled by spinal cord stimulation combined with physical training after spinal cord injury: Review of experimental evidence in animals and humans. Bioelectron. Med. 2021, 7, 16. [Google Scholar] [CrossRef] [PubMed]
- Estes, S.; Zarkou, A.; Hope, J.M.; Suri, C.; Field-Fote, E.C. Combined transcutaneous spinal stimulation and locomotor training to improve walking function and reduce spasticity in subacute spinal cord injury: A randomized study of clinical feasibility and efficacy. J. Clin. Med. 2021, 10, 1167. [Google Scholar] [CrossRef]
- Inanici, F.; Brighton, L.N.; Samejima, S.; Hofstetter, C.P.; Moritz, C.T. Transcutaneous spinal cord stimulation restores hand and arm function after spinal cord injury. IEEE Trans. Neural Syst. Rehabil. Eng. 2021, 29, 310–319. [Google Scholar] [CrossRef]
- Samejima, S.; Henderson, R.; Pradarelli, J.; Mondello, S.E.; Moritz, C.T. Activity-dependent plasticity and spinal cord stimulation for motor recovery following spinal cord injury. Exp. Neurol. 2022, 357, 114178. [Google Scholar] [CrossRef]
- McGeady, C.; vu Ckovi, C.A.; Singh Tharu, N.; Zheng, Y.P.; and Alam, M. Brain-Computer Interface Priming for Cervical Transcutaneous Spinal Cord Stimulation Therapy: An Exploratory Case Study. Front. Rehabilit. Sci. 2022, 3, 896766. [Google Scholar] [CrossRef]
- Aravind, N.; Harvey, L.A.; Glinsky, J.V. Physiotherapy interventions for increasing muscle strength in people with spinal cord injuries: A systematic review. Spinal Cord 2019, 57, 449–460. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.; Rodrigues, W.; Pham, B.N.; Thakor, N.V. Brain-machine interface facilitated neurorehabilitation via spinal stimulation after spinal cord injury: Recent progress and future perspectives. Brain Res. 2016, 1646, 25–33. [Google Scholar] [CrossRef] [PubMed]
- Palermo, A.E.; Cahalin, L.P.; Garcia, K.L.; Nash, M.S. Psychometric testing and clinical utility of a modified version of the function in sitting test for individuals with chronic spinal cord injury. Arch. Phys. Med. Rehabil. 2020, 101, 1961–1972. [Google Scholar] [CrossRef] [PubMed]
- Shirado, O.; Kawase, M.; Minami, A.; Strax, T.E. Quantitative evaluation of long sitting in paraplegic patients with spinal cord injury. Arch. Phys. Med. Rehabil. 2004, 85, 1251–1256. [Google Scholar] [CrossRef]
- Gabison, S.; Verrier, M.C.; Nadeau, S.; Gagnon, D.H.; Roy, A.; Flett, H.M. Trunk strength and function using the multidirectional reach distance in individuals with non-traumatic spinal cord injury. J. Spinal Cord Med. 2014, 37, 537–547. [Google Scholar] [CrossRef] [Green Version]
- Hobson, D.A.; Tooms, R.E. Seated lumbar/pelvic alignment: A comparison between spinal cord-injured and noninjured groups. Spine 1992, 17, 293–298. [Google Scholar] [CrossRef]
- Gagnon, D.H.; Roy, A.; Gabison, S.; Duclos, C.; Verrier, M.C.; Nadeau, S. Effects of seated postural stability and trunk and upper extremity strength on performance during manual wheelchair propulsion tests in individuals with spinal cord injury: An exploratory study. Rehabil. Res. Pract. 2016, 2016, 6842324. [Google Scholar] [CrossRef]

| Participants | Age | Gender | Time since Injury (Years) | Type of Injury | NLI | AIS Category |
|---|---|---|---|---|---|---|
| P1 | 57 | F | 1.5 | Traumatic | C6 | A |
| P2 | 55 | F | 19 | Traumatic | C7 | A |
| P3 | 26 | F | 12 | Traumatic | C5 | A |
| P4 | 40 | M | 12 | Traumatic | C5 | A |
| P5 | 32 | M | 2 | Traumatic | C4 | A |
| (A) | ||||||||
| Study Timeline | Extension | |||||||
| Rt. ES | Lt. ES | Rt. LD | Lt. LD | |||||
| Mean ± SD | p-Value | Mean ± SD | p-Value | Mean ± SD | p-Value | Mean ± SD | p-Value | |
| Baseline | 1.62 ± 0.95 | - | 1.79 ± 1.25 | - | 2.20 ± 1.60 | - | 2.57 ± 1.81 | - |
| TSCS+TSR | 6.93 ± 6.32 | * | 7.53 ± 5.47 | * | 8.86 ± 6.04 | *** | 9.94 ± 6.70 | * |
| TSR | 4.11 ± 2.68 | *** | 4.57 ± 3.02 | *** | 5.01 ± 3.71 | *** | 5.70 ± 4.86 | * |
| Follow-up | 4.19 ± 2.58 | *** | 4.69 ± 2.97 | *** | 5.02 ± 3.03 | ns | 6.07 ± 4.45 | *** |
| (B) | ||||||||
| Study timeline | Left rotation | |||||||
| Rt. EO | Lt. EO | |||||||
| Mean ± SD | p-Value | Mean ± SD | p-Value | |||||
| Baseline | 1.55 ± 0.93 | - | 2.07 ± 1.17 | - | ||||
| TSCS+TSR | 6.86 ± 3.94 | * | 13.47 ± 7.49 | * | ||||
| TSR | 6.06 ± 3.38 | * | 12.06 ± 6.73 | * | ||||
| Follow-up | 5.84 ± 3.40 | * | 11.19 ± 6.23 | * | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tharu, N.S.; Alam, M.; Ling, Y.T.; Wong, A.Y.; Zheng, Y.-P. Combined Transcutaneous Electrical Spinal Cord Stimulation and Task-Specific Rehabilitation Improves Trunk and Sitting Functions in People with Chronic Tetraplegia. Biomedicines 2023, 11, 34. https://doi.org/10.3390/biomedicines11010034
Tharu NS, Alam M, Ling YT, Wong AY, Zheng Y-P. Combined Transcutaneous Electrical Spinal Cord Stimulation and Task-Specific Rehabilitation Improves Trunk and Sitting Functions in People with Chronic Tetraplegia. Biomedicines. 2023; 11(1):34. https://doi.org/10.3390/biomedicines11010034
Chicago/Turabian StyleTharu, Niraj Singh, Monzurul Alam, Yan To Ling, Arnold YL Wong, and Yong-Ping Zheng. 2023. "Combined Transcutaneous Electrical Spinal Cord Stimulation and Task-Specific Rehabilitation Improves Trunk and Sitting Functions in People with Chronic Tetraplegia" Biomedicines 11, no. 1: 34. https://doi.org/10.3390/biomedicines11010034
APA StyleTharu, N. S., Alam, M., Ling, Y. T., Wong, A. Y., & Zheng, Y.-P. (2023). Combined Transcutaneous Electrical Spinal Cord Stimulation and Task-Specific Rehabilitation Improves Trunk and Sitting Functions in People with Chronic Tetraplegia. Biomedicines, 11(1), 34. https://doi.org/10.3390/biomedicines11010034








