Oncological Outcomes in Patients with Metastatic Urothelial Carcinoma after Discontinuing Pembrolizumab as a Second-Line Treatment: A Retrospective Multicenter Real-World Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Treatment Schedule
2.3. Patient Evaluation
2.4. Endpoints and Statistical Analysis
3. Results
3.1. Patient Characteristics
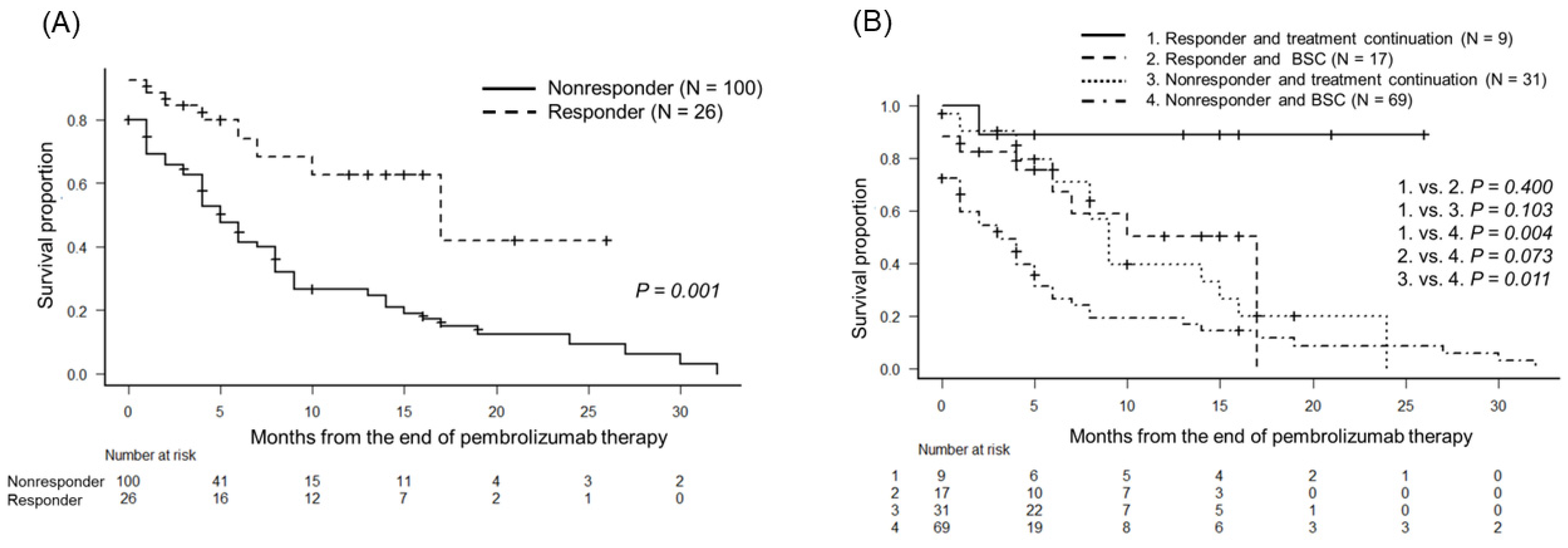
3.2. Oncological Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bamias, A.; Tzannis, K.; Harshman, L.C.; Crabb, S.J.; Wong, Y.N.; Kumar Pal, S.; De Giorgi, U.; Ladoire, S.; Agarwal, N.; Yu, E.Y.; et al. Impact of contemporary patterns of chemotherapy utilization on survival in patients with advanced cancer of the urinary tract: A Retrospective International Study of Invasive/Advanced Cancer of the Urothelium (RISC). Ann. Oncol. 2018, 29, 361–369. [Google Scholar] [CrossRef] [PubMed]
- Deininger, S.; Törzsök, P.; Oswald, D.; Lusuardi, L. Current systemic treatment options in metastatic urothelial carcinoma after progression on checkpoint inhibition therapy—A systemic review combined with single-group meta-analysis of three studies testing enfortumab vedotin. Cancers 2021, 13, 3206. [Google Scholar] [CrossRef]
- Saginala, K.; Barsouk, A.; Aluru, J.S.; Rawla, P.; Padala, S.A.; Barsouk, A. Epidemiology of bladder cancer. Med. Sci. 2020, 8, 15. [Google Scholar]
- Cathomas, R.; Lorch, A.; Bruins, H.M.; Compérat, E.M.; Cowan, N.C.; Efstathiou, J.A.; Fietkau, R.; Gakis, G.; Hernández, V.; Espinós, E.L.; et al. The 2021 Updated European Association of Urology Guidelines on Metastatic Urothelial Carcinoma. Eur. Urol. 2022, 81, 95–103. [Google Scholar] [PubMed]
- Powles, T.; Bellmunt, J.; Comperat, E.; De Santis, M.; Huddart, R.; Loriot, Y.; Necchi, A.; Valderrama, B.P.; Ravaud, A.; Shariat, S.F.; et al. Bladder cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up. Ann. Oncol. 2022, 33, 244–258. [Google Scholar] [CrossRef]
- Bladder Cancer. NCCN Guidelines® 2022. Available online: https://www.nccn.org/professionals/physician_gls/pdf/bladder.pdf (accessed on 15 May 2022).
- Von der Maase, H.; Sengelov, L.; Roberts, J.T.; Ricci, S.; Dogliotti, L.; Oliver, T.; Moore, M.J.; Zimmermann, A.; Arning, M. Long-term survival results of a randomized trial comparing gemcitabine plus cisplatin, with methotrexate, vinblastine, doxorubicin, plus cisplatin in patients with bladder cancer. J. Clin. Oncol. 2005, 23, 4602–4608. [Google Scholar] [CrossRef] [PubMed]
- De Santis, M.; Bellmunt, J.; Mead, G.; Kerst, J.M.; Leahy, M.; Maroto, P.; Skoneczna, I.; Marreaud, S.; de Wit, R.; Sylvester, R. Randomized phase II/III trial assessing gemcitabine/carboplatin and methotrexate/carboplatin/vinblastine in patients with advanced urothelial cancer “unfit” for cisplatin-based chemotherapy: Phase II—Results of EORTC study 30986. J. Clin. Oncol. 2009, 27, 5634–5639. [Google Scholar] [CrossRef] [PubMed]
- Bellmunt, J.; de Wit, R.; Vaughn, D.J.; Fradet, Y.; Lee, J.L.; Fong, L.; Vogelzang, N.J.; Climent, M.A.; Petrylak, D.P.; Choueiri, T.K.; et al. Pembrolizumab as second-line therapy for advanced urothelial carcinoma. N. Engl. J. Med. 2017, 376, 1015–1026. [Google Scholar] [CrossRef]
- Fradet, Y.; Bellmunt, J.; Vaughn, D.J.; Lee, J.L.; Fong, L.; Vogelzang, N.J.; Lee, J.L.; Fong, L.; Vogelzang, N.J.; Climent, M.A.; et al. Randomized phase III KEYNOTE-045 trial of pembrolizumab versus paclitaxel, docetaxel, or vinflunine in recurrent advanced urothelial cancer: Results of >2 years of follow-up. Ann. Oncol. 2019, 30, 970–976. [Google Scholar] [CrossRef]
- Powles, T.; Rosenberg, J.E.; Sonpavde, G.P.; Loriot, Y.; Durán, I.; Lee, J.L.; Matsubara, N.; Vulsteke, C.; Castellano, D.; Wu, C.; et al. Enfortumab vedotin in previously treated advanced urothelial carcinoma. N. Engl. J. Med. 2021, 384, 1125–1135. [Google Scholar] [CrossRef]
- Sonpavde, G.; Pond, G.R.; Mullane, S.; Ramirez, A.A.; Vogelzang, N.J.; Necchi, A.; Powles, T.; Bellmunt, J. Outcomes in patients with advanced urothelial carcinoma after discontinuation of programmed death (PD)-1 or PD ligand 1 inhibitor therapy. BJU Int. 2017, 119, 579–584. [Google Scholar] [CrossRef] [PubMed]
- Hepp, Z.; Shah, S.N.; Smoyer, K.; Vadagam, P. Epidemiology and treatment patterns for locally advanced or metastatic urothelial carcinoma: A systematic literature review and gap analysis. J. Manag. Care Spec. Pharm. 2021, 27, 240–255. [Google Scholar] [CrossRef] [PubMed]
- Sonpavde, G.; Pond, G.R.; Choueiri, T.K.; Mullane, S.; Niegisch, G.; Albers, P.; Necchi, A.; Di Lorenzo, G.; Buonerba, C.; Rozzi, A.; et al. Single-agent taxane versus taxane-containing combination chemotherapy as salvage therapy for advanced urothelial carcinoma. Eur. Urol. 2016, 69, 634–641. [Google Scholar] [CrossRef] [PubMed]
- Oken, M.M.; Creech, R.H.; Tormey, D.C.; Horton, J.; Davis, T.E.; McFadden, E.T.; Carbone, P.P. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am. J. Clin. Oncol. 1982, 5, 649–655. [Google Scholar] [CrossRef] [PubMed]
- Paner, G.P.; Stadler, W.M.; Hansel, D.E.; Montironi, R.; Lin, D.W.; Amin, M.B. Updates in the eighth edition of the Tumor-Node-Metastasis staging classification for urologic cancers. Eur. Urol. 2018, 73, 560–569. [Google Scholar] [CrossRef] [PubMed]
- Chen, A.P.; Setser, A.; Anadkat, M.J.; Cotliar, J.; Olsen, E.A.; Garden, B.C.; Lacouture, M.E. Grading dermatologic adverse events of cancer treatments: The Common Terminology Criteria for Adverse Events Version 4.0. J. Am. Acad. Dermatol. 2012, 67, 1025–1039. [Google Scholar] [CrossRef]
- Hepp, Z.; Shah, S.N.; Liang, S.Y.; Tan, K.; Balakrishna, S. Real-world outcomes in locally advanced or metastatic urothelial carcinoma following platinum and PD-1/L1 inhibitor therapy. Future Oncol. 2021, 17, 4343–4353. [Google Scholar] [CrossRef]
- Di Lorenzo, G.; Buonerba, C.; Bellelli, T.; Romano, C.; Montanaro, V.; Ferro, M.; Benincasa, A.; Ribera, D.; Lucarelli, G.; De Cobelli, O.; et al. Third-Line Chemotherapy for Metastatic Urothelial Cancer: A Retrospective Observational Study. Medicine 2015, 94, e2297. [Google Scholar] [CrossRef]
- Matsumoto, K.; Mochizuki, K.; Hirayama, T.; Ikeda, M.; Nishi, M.; Tabata, K.; Okazaki, M.; Fujita, T.; Taoka, Y.; Iwamura, M. Gemcitabine plus nedaplatin as salvage therapy is a favorable option for patients with progressive metastatic urothelial carcinoma after two lines of chemotherapy. Asian Pac. J. Cancer Prev. 2015, 16, 2483–2487. [Google Scholar] [CrossRef]
- Rozzi, A.; Santini, D.; Salerno, M.; Bordin, F.; Mancuso, A.; Minniti, G.; Nardoni, C.; Corona, M.; Falbo, P.T.; Recine, F.; et al. Pegylated liposomal doxorubicin as third-line chemotherapy in patients with metastatic transitional cell carcinoma of urothelial tract: Results of a phase II study. Med. Oncol. 2013, 30, 407. [Google Scholar] [CrossRef]
- Soga, N.; Kise, H.; Arima, K.; Sugimura, Y. Third-line gemcitabine monotherapy for platinum-resistant advanced urothelial cancer. Int. J. Clin. Oncol. 2010, 15, 376–381. [Google Scholar] [CrossRef] [PubMed]
- Barata, P.C.; Gopalakrishnan, D.; Koshkin, V.S.; Mendiratta, P.; Karafa, M.; Allman, K.; Martin, A.; Beach, J.; Profusek, P.; Tyler, A.; et al. Atezolizumab in metastatic urothelial carcinoma outside clinical trials: Focus on efficacy, safety, and response to subsequent therapies. Target. Oncol. 2018, 13, 353–361. [Google Scholar] [CrossRef] [PubMed]


| Covariates | BSC Group | Treatment Group | p |
|---|---|---|---|
| Number | 86 | 40 | |
| Follow up period (median, months, interquartile range) | 6.0 (2.2–13.7) | 12.5 (7.7–18.5) | <0.001 |
| Age (median, year, interquartile range) | 73.5 (70.0–79.0) | 71 (66.7–75.2) | 0.044 |
| Sex (number, %) | 0.132 | ||
| Male | 59 (68.6) | 33 (82.5) | |
| Female | 27 (31.4) | 7 (17.5) | |
| Body mass index (median, kg/m2, interquartile range) | 21.3 (19.3–24.1) | 22.6 (19.3–25.2) | 0.279 |
| The Eastern Cooperative Oncology Group performance status (number, %) | |||
| 0 | 1 (5.6) | 9 (26.5) | 0.008 |
| 1 | 3 (16.7) | 15 (44.1) | |
| 2 | 7 (38.9) | 7 (20.6) | |
| 3 | 5 (27.8) | 3 (8.8) | |
| 4 | 2 (11.1) | 0 (0.0) | |
| Primary site (number, %) | 0.285 | ||
| Bladder | 49 (57.0) | 24 (60.0) | |
| Upper urinary tract | 27 (31.4) | 8 (20.0) | |
| Bladder and Upper urinary tract | 10 (11.6) | 8 (20.0) | |
| Definitive therapy for primary site (number, %) | 73 (84.9) | 35 (87.5) | 0.625 |
| Location of metastases (number, %) | |||
| Lung | 40 (46.5) | 20 (50.0) | 0.848 |
| Liver | 19 (22.1) | 7 (17.5) | 0.641 |
| Bone | 17 (19.8) | 9 (22.5) | 0.814 |
| Lymph node | 66 (76.7) | 29 (72.5) | 0.659 |
| Best overall response after pembrolizumab therapy (number, %) | |||
| Complete response | 1 (1.2) | 4 (10.0) | 0.128 |
| Partial response | 16 (18.6) | 5 (12.5) | |
| Stable disease | 18 (20.9) | 9 (22.5) | |
| Progression disease | 51 (59.3) | 22 (55.0) | |
| Covariates | BSC Group | Treatment Group | p |
|---|---|---|---|
| Number | 83 | 40 | |
| Before pembrolizumab therapy | |||
| Hemoglobin (median, g/dL, interquartile range) | 10.2 (8.8–11.4) | 11.1 (10.2–12.6) | 0.005 |
| Albumin (median, g/dL, interquartile range) | 3.4 (3.1–3.9) | 3.9 (3.5–4.1) | <0.001 |
| C-reactive protein (median, mg/L, interquartile range) | 1.50 (0.50–4.52) | 0.24 (0.10–0.90) | <0.001 |
| Neutrophil-to-lymphocyte ratio (median, interquartile range) | 3.29 (2.29–6.00) | 2.52 (1.61–3.21) | <0.001 |
| After pembrolizumab therapy | |||
| Hemoglobin (median, g/dL, interquartile range) | 9.8 (8.5–10.7) | 11.3 (10.0–13.4) | 0.041 |
| Albumin (median, g/dL, interquartile range) | 2.8 (2.5–3.6) | 3.6 (3.3–4.0) | 0.003 |
| C-reactive protein (median, mg/L, interquartile range) | 4.81 (1.33–10.24) | 0.66 (0.14–4.34) | 0.007 |
| Neutrophil-to-lymphocyte ratio (median, interquartile range) | 6.80 (3.91–8.58) | 3.46 (2.21–4.88) | 0.003 |
| Covariates | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p | HR | 95% CI | p | |
| ECOG-PS, ≥2/≤1 | 5.859 | 2.506–13.7 | <0.001 | 5.031 | 1.179–21.470 | 0.029 |
| Lung metastasis, With/Without | 1.581 | 1.007–2.484 | 0.047 | |||
| Liver metastasis, With/Without | 1.752 | 1.058–2.903 | 0.029 | 4.281 | 1.192–15.370 | 0.026 |
| Hemoglobin (g/dL), ≥10.8/<10.8 | 0.364 | 0.160–0.731 | 0.016 | |||
| Albumin (g/dL), ≥3.5/<3.5 | 0.275 | 0.122–0.621 | 0.002 | |||
| C-reactive protein (mg/L), ≥0.54/<0.54 | 6.787 | 2.033–22.660 | 0.002 | |||
| Neutrophil-to-lymphocyte ratio, ≥3.91/<3.91 | 12.280 | 4.046–37.270 | <0.001 | |||
| Best response after pembrolizumab therapy, Responder/nonresponder | 0.352 | 0.175–0.707 | 0.003 | |||
| Third-line therapy, With/Without | 0.434 | 0.258–0.732 | 0.002 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yamada, T.; Nakane, K.; Enomoto, T.; Tomioka, M.; Taniguchi, T.; Ishida, T.; Ozawa, K.; Takagi, K.; Ito, H.; Takeuchi, S.; et al. Oncological Outcomes in Patients with Metastatic Urothelial Carcinoma after Discontinuing Pembrolizumab as a Second-Line Treatment: A Retrospective Multicenter Real-World Cohort Study. Biomedicines 2022, 10, 2243. https://doi.org/10.3390/biomedicines10092243
Yamada T, Nakane K, Enomoto T, Tomioka M, Taniguchi T, Ishida T, Ozawa K, Takagi K, Ito H, Takeuchi S, et al. Oncological Outcomes in Patients with Metastatic Urothelial Carcinoma after Discontinuing Pembrolizumab as a Second-Line Treatment: A Retrospective Multicenter Real-World Cohort Study. Biomedicines. 2022; 10(9):2243. https://doi.org/10.3390/biomedicines10092243
Chicago/Turabian StyleYamada, Toyohiro, Keita Nakane, Torai Enomoto, Masayuki Tomioka, Tomoki Taniguchi, Takashi Ishida, Kaori Ozawa, Kimiaki Takagi, Hiroki Ito, Shinichi Takeuchi, and et al. 2022. "Oncological Outcomes in Patients with Metastatic Urothelial Carcinoma after Discontinuing Pembrolizumab as a Second-Line Treatment: A Retrospective Multicenter Real-World Cohort Study" Biomedicines 10, no. 9: 2243. https://doi.org/10.3390/biomedicines10092243
APA StyleYamada, T., Nakane, K., Enomoto, T., Tomioka, M., Taniguchi, T., Ishida, T., Ozawa, K., Takagi, K., Ito, H., Takeuchi, S., Kawase, M., Kawase, K., Kato, D., Takai, M., Iinuma, K., Yokoi, S., Nakano, M., & Koie, T. (2022). Oncological Outcomes in Patients with Metastatic Urothelial Carcinoma after Discontinuing Pembrolizumab as a Second-Line Treatment: A Retrospective Multicenter Real-World Cohort Study. Biomedicines, 10(9), 2243. https://doi.org/10.3390/biomedicines10092243







