Neuro-Inflammaging and Psychopathological Distress
Abstract
1. Introduction
2. Epigenetics, Aging, and Chronic Inflammation
2.1. Proinflammatory Mediators
2.2. The Anti-Inflammatory Counterbalance
3. Cytokines and Neuroinflammation
4. Correlation between Depression and Other Psychopathological Disorders in Chronic Inflammatory Diseases
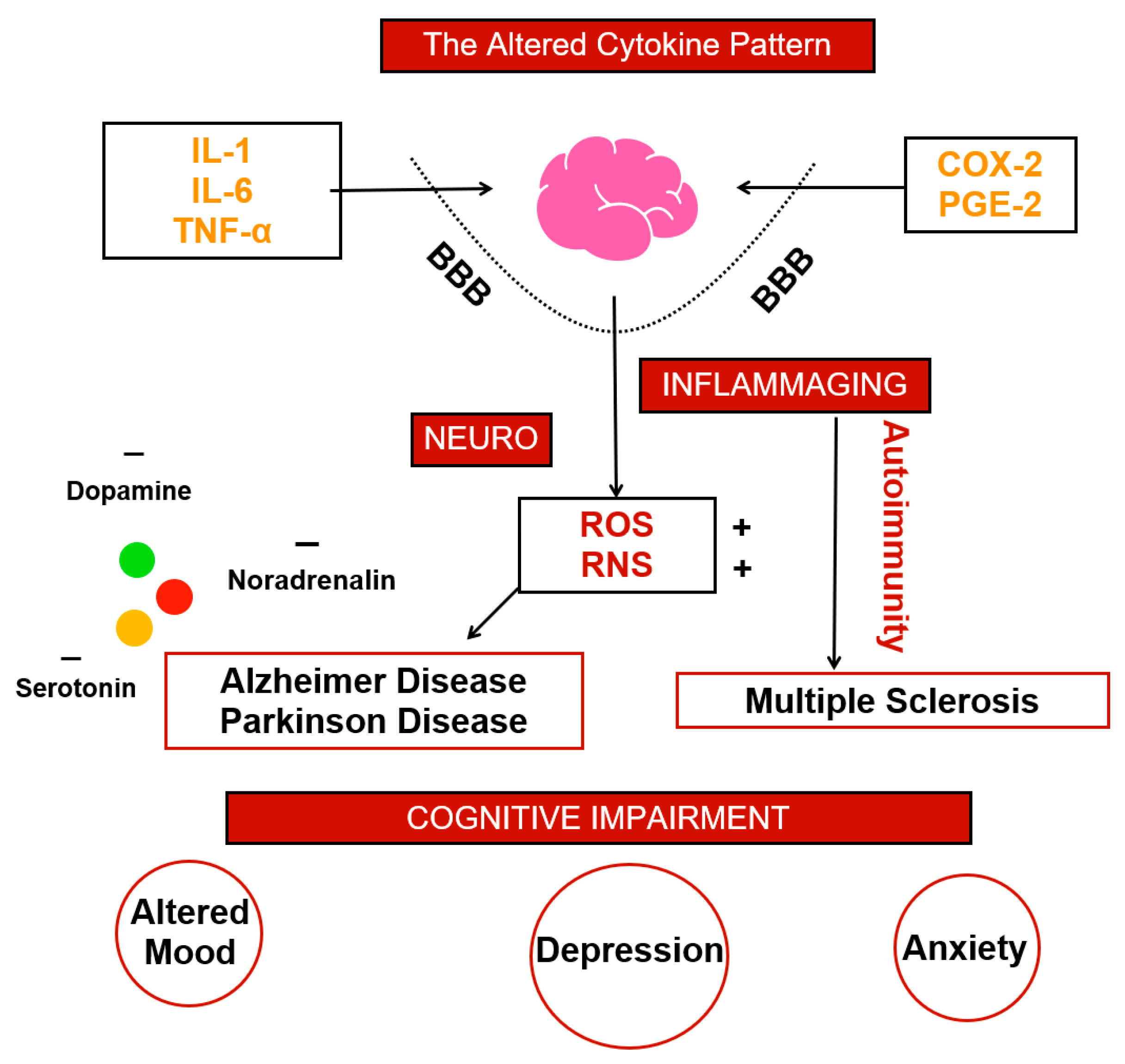
5. Criticisms: Altered Cytokine Patterns
6. Future Prospective
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Franceschi, C.; Capri, M.; Monti, D.; Giunta, S.; Olivieri, F.; Sevini, F.; Panourgia, M.P.; Invidia, L.; Celani, L.; Scurti, M.; et al. Inflammaging and Anti-Inflammaging: A Systemic Perspective on Aging and Longevity Emerged from Studies in Humans. Mech. Ageing Dev. 2007, 128, 92–105. [Google Scholar] [CrossRef] [PubMed]
- Franceschi, C.; Motta, L.; Valensin, S.; Rapisarda, R.; Franzone, A.; Berardelli, M.; Motta, M.; Monti, D.; Bonafè, M.; Ferrucci, L.; et al. Do Men and Women Follow Different Trajectories to Reach Extreme Longevity? Italian Multicenter Study on Centenarians (IMUSCE). Aging Clin. Exp. Res. 2000, 12, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Evert, J.; Lawler, E.; Bogan, H.; Perls, T. Morbidity Profiles of Centenarians: Survivors, Delayers, and Escapers. J. Gerontol. A Biol. Sci. Med. Sci. 2003, 58, 232–237. [Google Scholar] [CrossRef]
- Calabrese, V.; Santoro, A.; Monti, D.; Crupi, R.; Di Paola, R.; Latteri, S.; Cuzzocrea, S.; Zappia, M.; Giordano, J.; Calabrese, E.J.; et al. Aging and Parkinson’s Disease: Inflammaging, Neuroinflammation and Biological Remodeling as Key Factors in Pathogenesis. Free Radic. Biol. Med. 2018, 115, 80–91. [Google Scholar] [CrossRef]
- Floden, A.M.; Combs, C.K. Microglia Demonstrate Age-Dependent Interaction with Amyloid-β Fibrils. J. Alzheimers Dis. 2011, 25, 279–293. [Google Scholar] [CrossRef] [PubMed]
- Costantini, E.; D’Angelo, C.; Reale, M. The Role of Immunosenescence in Neurodegenerative Diseases. Mediat. Inflamm. 2018, 2018, 6039171. [Google Scholar] [CrossRef]
- Sochocka, M.; Diniz, B.S.; Leszek, J. Inflammatory Response in the CNS: Friend or Foe? Mol. Neurobiol. 2017, 54, 8071–8089. [Google Scholar] [CrossRef]
- Almeida, P.G.C.; Nani, J.V.; Oses, J.P.; Brietzke, E.; Hayashi, M.A.F. Neuroinflammation and Glial Cell Activation in Mental Disorders. Brain Behav. Immun. Health 2020, 2, 100034. [Google Scholar] [CrossRef]
- Surace, A.E.A.; Hedrich, C.M. The Role of Epigenetics in Autoimmune/Inflammatory Disease. Front. Immunol. 2019, 10, 1525. [Google Scholar] [CrossRef]
- Stylianou, E. Epigenetics of Chronic Inflammatory Diseases. J. Inflamm. Res. 2018, 12, 1–14. [Google Scholar] [CrossRef]
- Ramos-Lopez, O.; Milagro, F.I.; Riezu-Boj, J.I.; Martinez, J.A. Epigenetic Signatures Underlying Inflammation: An Interplay of Nutrition, Physical Activity, Metabolic Diseases, and Environmental Factors for Personalized Nutrition. Inflamm. Res. 2021, 70, 29–49. [Google Scholar] [CrossRef] [PubMed]
- Barnes, P.J. Mechanisms of Development of Multimorbidity in the Elderly. Eur. Respir. J. 2015, 45, 790–806. [Google Scholar] [CrossRef] [PubMed]
- Franceschi, C.; Campisi, J. Chronic Inflammation (Inflammaging) and Its Potential Contribution to Age-Associated Diseases. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2014, 69, S4–S9. [Google Scholar] [CrossRef] [PubMed]
- Fulop, T.; Witkowski, J.M.; Olivieri, F.; Larbi, A. The Integration of Inflammaging in Age-Related Diseases. Semin. Immunol. 2018, 40, 17–35. [Google Scholar] [CrossRef]
- Minciullo, P.L.; Catalano, A.; Mandraffino, G.; Casciaro, M.; Crucitti, A.; Maltese, G.; Morabito, N.; Lasco, A.; Gangemi, S.; Basile, G. Inflammaging and Anti-Inflammaging: The Role of Cytokines in Extreme Longevity. Arch. Immunol. Ther. Exp. 2016, 64, 111–126. [Google Scholar] [CrossRef]
- Akdis, M.; Burgler, S.; Crameri, R.; Eiwegger, T.; Fujita, H.; Gomez, E.; Klunker, S.; Meyer, N.; O’Mahony, L.; Palomares, O.; et al. Interleukins, from 1 to 37, and Interferon-γ: Receptors, Functions, and Roles in Diseases. J. Allergy Clin. Immunol. 2011, 127, 701–721. [Google Scholar] [CrossRef]
- Ma, L.; Nidadavolu, L.S.; Yang, H.; Langdon, J.; Westbrook, R.; Tsui, B.M.W.; Lee, T.-S.; Hinson, J.; Ling, S.; Marx-Rattner, R.; et al. Targeted Deletion of Interleukin-6 in a Mouse Model of Chronic Inflammation Demonstrates Opposing Roles in Aging: Benefit and Harm. J. Gerontol. A Biol. Sci. Med. Sci. 2021, 76, 211–215. [Google Scholar] [CrossRef]
- Decourt, B.; Lahiri, D.K.; Sabbagh, M.N. Targeting Tumor Necrosis Factor Alpha for Alzheimer’s Disease. Curr. Alzheimer Res. 2017, 14, 412–425. [Google Scholar] [CrossRef]
- Bradley, J.R. TNF-Mediated Inflammatory Disease. J. Pathol. 2008, 214, 149–160. [Google Scholar] [CrossRef]
- Luan, Y.-Y.; Yao, Y.-M. The Clinical Significance and Potential Role of C-Reactive Protein in Chronic Inflammatory and Neurodegenerative Diseases. Front. Immunol. 2018, 9, 1302. [Google Scholar] [CrossRef]
- Nakanishi, K.; Yoshimoto, T.; Tsutsui, H.; Okamura, H. Interleukin-18 Is a Unique Cytokine That Stimulates Both Th1 and Th2 Responses Depending on Its Cytokine Milieu. Cytokine Growth Factor Rev. 2001, 12, 53–72. [Google Scholar] [CrossRef]
- Park, S.Y.; Hisham, Y.; Shin, H.M.; Yeom, S.C.; Kim, S. Interleukin-18 Binding Protein in Immune Regulation and Autoimmune Diseases. Biomedicines 2022, 10, 1750. [Google Scholar] [CrossRef] [PubMed]
- Becher, B.; Spath, S.; Goverman, J. Cytokine Networks in Neuroinflammation. Nat. Rev. Immunol. 2016, 17, 49–59. [Google Scholar] [CrossRef] [PubMed]
- Martino, G.; Bellone, F.; Langher, V.; Caputo, A.; Catalano, A.; Quattropani, M.C.; Morabito, N. Alexithymia and Psychological Distress Affect Perceived Quality of Life in Patients with Type 2 Diabetes Mellitus. Mediterr. J. Clin. Psychol. 2019, 7. [Google Scholar] [CrossRef]
- Rea, I.M.; Gibson, D.S.; McGilligan, V.; McNerlan, S.E.; Alexander, H.D.; Ross, O.A. Age and Age-Related Diseases: Role of Inflammation Triggers and Cytokines. Front. Immunol. 2018, 9, 586. [Google Scholar] [CrossRef]
- Wagner, K.-H.; Cameron-Smith, D.; Wessner, B.; Franzke, B. Biomarkers of Aging: From Function to Molecular Biology. Nutrients 2016, 8, 338. [Google Scholar] [CrossRef]
- Gangemi, S.; Basile, G.; Merendino, R.A.; Minciullo, P.L.; Novick, D.; Rubinstein, M.; Dinarello, C.A.; Balbo, C.L.; Franceschi, C.; Basili, S.; et al. Increased Circulating Interleukin-18 Levels in Centenarians with No Signs of Vascular Disease: Another Paradox of Longevity? Exp. Gerontol. 2003, 38, 669–672. [Google Scholar] [CrossRef]
- Ribezzo, F.; Shiloh, Y.; Schumacher, B. Systemic DNA Damage Responses in Aging and Diseases. Semin. Cancer Biol. 2016, 37–38, 26–35. [Google Scholar] [CrossRef]
- Briard, B.; Place, D.E.; Kanneganti, T.-D. DNA Sensing in the Innate Immune Response. Physiology 2020, 35, 112–124. [Google Scholar] [CrossRef]
- Man, S.M.; Kanneganti, T.-D. Regulation of Inflammasome Activation. Immunol. Rev. 2015, 265, 6–21. [Google Scholar] [CrossRef]
- Man, S.M.; Karki, R.; Kanneganti, T.-D. AIM2 Inflammasome in Infection, Cancer, and Autoimmunity: Role in DNA Sensing, Inflammation, and Innate Immunity. Eur. J. Immunol. 2016, 46, 269–280. [Google Scholar] [CrossRef] [PubMed]
- Saxena, A.; Khosraviani, S.; Noel, S.; Mohan, D.; Donner, T.; Hamad, A.R.A. Interleukin-10 Paradox: A Potent Immunoregulatory Cytokine That Has Been Difficult to Harness for Immunotherapy. Cytokine 2015, 74, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Dagdeviren, S.; Jung, D.Y.; Friedline, R.H.; Noh, H.L.; Kim, J.H.; Patel, P.R.; Tsitsilianos, N.; Inashima, K.; Tran, D.A.; Hu, X.; et al. IL-10 Prevents Aging-Associated Inflammation and Insulin Resistance in Skeletal Muscle. FASEB J. 2017, 31, 701–710. [Google Scholar] [CrossRef] [PubMed]
- Salminen, A. Immunosuppressive Network Promotes Immunosenescence Associated with Aging and Chronic Inflammatory Conditions. J. Mol. Med. 2021, 99, 1553–1569. [Google Scholar] [CrossRef]
- Fulop, T.; Larbi, A.; Douziech, N.; Levesque, I.; Varin, A.; Herbein, G. Cytokine Receptor Signalling and Aging. Mech. Ageing Dev. 2006, 127, 526–537. [Google Scholar] [CrossRef]
- Udina, M.; Moreno-España, J.; Navinés, R.; Giménez, D.; Langohr, K.; Gratacòs, M.; Capuron, L.; de la Torre, R.; Solà, R.; Martín-Santos, R. Serotonin and Interleukin-6: The Role of Genetic Polymorphisms in IFN-Induced Neuropsychiatric Symptoms. Psychoneuroendocrinology 2013, 38, 1803–1813. [Google Scholar] [CrossRef]
- Felger, J.C.; Lotrich, F.E. Inflammatory Cytokines in Depression: Neurobiological Mechanisms and Therapeutic Implications. Neuroscience 2013, 246, 199–229. [Google Scholar] [CrossRef]
- Kim, Y.-K.; Na, K.-S.; Myint, A.-M.; Leonard, B.E. The Role of Pro-Inflammatory Cytokines in Neuroinflammation, Neurogenesis and the Neuroendocrine System in Major Depression. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2016, 64, 277–284. [Google Scholar] [CrossRef]
- Song, C.; Wang, H. Cytokines Mediated Inflammation and Decreased Neurogenesis in Animal Models of Depression. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2011, 35, 760–768. [Google Scholar] [CrossRef]
- Shabab, T.; Khanabdali, R.; Moghadamtousi, S.Z.; Kadir, H.A.; Mohan, G. Neuroinflammation Pathways: A General Review. Int. J. Neurosci. 2016, 127, 624–633. [Google Scholar] [CrossRef]
- Maes, M.; Yirmyia, R.; Noraberg, J.; Brene, S.; Hibbeln, J.; Perini, G.; Kubera, M.; Bob, P.; Lerer, B.; Maj, M. The Inflammatory & Neurodegenerative (I&ND) Hypothesis of Depression: Leads for Future Research and New Drug Developments in Depression. Metab. Brain Dis. 2008, 24, 27–53. [Google Scholar] [CrossRef] [PubMed]
- DiSabato, D.J.; Quan, N.; Godbout, J.P. Neuroinflammation: The Devil Is in the Details. J. Neurochem. 2016, 139, 136–153. [Google Scholar] [CrossRef] [PubMed]
- Chu, E.; Mychasiuk, R.; Hibbs, M.L.; Semple, B.D. Dysregulated Phosphoinositide 3-Kinase Signaling in Microglia: Shaping Chronic Neuroinflammation. J. Neuroinflamm. 2021, 18, 276. [Google Scholar] [CrossRef] [PubMed]
- Heneka, M.T.; Kummer, M.P.; Stutz, A.; Delekate, A.; Schwartz, S.; Vieira-Saecker, A.; Griep, A.; Axt, D.; Remus, A.; Tzeng, T.-C.; et al. NLRP3 Is Activated in Alzheimer’s Disease and Contributes to Pathology in APP/PS1 Mice. Nature 2013, 493, 674–678. [Google Scholar] [CrossRef] [PubMed]
- Raneros, A.B.; Bernet, C.R.; Flórez, A.B.; Suarez-Alvarez, B. An Epigenetic Insight into NLRP3 Inflammasome Activation in Inflammation-Related Processes. Biomedicines 2021, 9, 1614. [Google Scholar] [CrossRef]
- Mawhinney, L.J.; de Rivero Vaccari, J.P.; Dale, G.A.; Keane, R.W.; Bramlett, H.M. Heightened Inflammasome Activation Is Linked to Age-Related Cognitive Impairment in Fischer 344 Rats. BMC Neurosci. 2011, 12, 123. [Google Scholar] [CrossRef]
- Mejias, N.H.; Martinez, C.C.; Stephens, M.E.; de Rivero Vaccari, J.P. Contribution of the Inflammasome to Inflammaging. J. Inflamm. 2018, 15, 23. [Google Scholar] [CrossRef]
- Sasayama, D.; Hattori, K.; Wakabayashi, C.; Teraishi, T.; Hori, H.; Ota, M.; Yoshida, S.; Arima, K.; Higuchi, T.; Amano, N.; et al. Increased Cerebrospinal Fluid Interleukin-6 Levels in Patients with Schizophrenia and Those with Major Depressive Disorder. J. Psychiatr. Res. 2013, 47, 401–406. [Google Scholar] [CrossRef]
- Haapakoski, R.; Mathieu, J.; Ebmeier, K.P.; Alenius, H.; Kivimäki, M. Cumulative Meta-Analysis of Interleukins 6 and 1β, Tumour Necrosis Factor α and C-Reactive Protein in Patients with Major Depressive Disorder. Brain Behav. Immun. 2015, 49, 206–215. [Google Scholar] [CrossRef]
- Benatti, C.; MC Blom, J.; Rigillo, G.; Alboni, S.; Zizzi, F.; Torta, R.; Brunello, N.; Tascedda, F. Disease-Induced Neuroinflammation and Depression. CNS Neurol. Disord. -Drug Targets 2016, 15, 414–433. [Google Scholar] [CrossRef]
- Glaus, J.; von Känel, R.; Lasserre, A.M.; Strippoli, M.-P.F.; Vandeleur, C.L.; Castelao, E.; Gholam-Rezaee, M.; Marangoni, C.; Wagner, E.-Y.N.; Marques-Vidal, P.; et al. Mood Disorders and Circulating Levels of Inflammatory Markers in a Longitudinal Population-Based Study. Psychol. Med. 2017, 48, 961–973. [Google Scholar] [CrossRef] [PubMed]
- Vogelzangs, N.; de Jonge, P.; Smit, J.H.; Bahn, S.; Penninx, B.W. Cytokine Production Capacity in Depression and Anxiety. Transl. Psychiatry 2016, 6, e825. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.M.; Te, S.; Breen, E.C.; Olmstead, R.; Irwin, M.R.; Cho, J.H. Circulating versus Lipopolysaccharide-Induced Inflammatory Markers as Correlates of Subthreshold Depressive Symptoms in Older Adults. World J. Biol. Psychiatry 2020, 21, 634–641. [Google Scholar] [CrossRef] [PubMed]
- Orsolini, L.; Pompili, S.; Tempia Valenta, S.; Salvi, V.; Volpe, U. C-Reactive Protein as a Biomarker for Major Depressive Disorder? Int. J. Mol. Sci. 2022, 23, 1616. [Google Scholar] [CrossRef]
- de Oliveira, J.F.; Wiener, C.D.; Jansen, K.; Portela, L.V.; Lara, D.R.; Souza, L.D.d.M.; da Silva, R.A.; Moreira, F.P.; Oses, J.P. Serum Levels of Interleukins IL-6 and IL-10 in Individuals with Posttraumatic Stress Disorder in a Population-Based Sample. Psychiatry Res. 2018, 260, 111–115. [Google Scholar] [CrossRef]
- Baune, B.T.; Smith, E.; Reppermund, S.; Air, T.; Samaras, K.; Lux, O.; Brodaty, H.; Sachdev, P.; Trollor, J.N. Inflammatory Biomarkers Predict Depressive, but Not Anxiety Symptoms during Aging: The Prospective Sydney Memory and Aging Study. Psychoneuroendocrinology 2012, 37, 1521–1530. [Google Scholar] [CrossRef]
- Lee, C.-H.; Giuliani, F. The Role of Inflammation in Depression and Fatigue. Front. Immunol. 2019, 10, 1696. [Google Scholar] [CrossRef]
- Nerurkar, L.; Siebert, S.; McInnes, I.B.; Cavanagh, J. Rheumatoid Arthritis and Depression: An Inflammatory Perspective. Lancet Psychiatry 2019, 6, 164–173. [Google Scholar] [CrossRef]
- Wenger, A.; Calabrese, P. Comparing Underlying Mechanisms of Depression in Multiple Sclerosis and Rheumatoid Arthritis. J. Integr. Neurosci. 2021, 20, 765–776. [Google Scholar] [CrossRef]
- Du, Y.; Yang, C.; Li, B.; Wu, X.; Lv, Y.; Jin, H.; Cao, Y.; Sun, J.; Luo, Q.; Gong, W.; et al. Association of Pro-Inflammatory Cytokines, Cortisol and Depression in Patients with Chronic Obstructive Pulmonary Disease. Psychoneuroendocrinology 2014, 46, 141–152. [Google Scholar] [CrossRef]
- Karabıçak, D.; Doğruöz Karatekin, B.; İçağasıoğlu, A. Alexithymia in Ankylosing Spondylitis. Turk. J. Phys. Med. Rehabil. 2021, 67, 344–350. [Google Scholar] [CrossRef] [PubMed]
- Barchetta, S.; Martino, G.; Craparo, G.; Salehinejad, M.A.; Nitsche, M.A.; Vicario, C.M. Alexithymia Is Linked with a Negative Bias for Past and Current Events in Healthy Humans. Int. J. Environ. Res. Public Health 2021, 18, 6696. [Google Scholar] [CrossRef] [PubMed]
- La Rosa, V.L.; Gori, A.; Faraci, P.; Vicario, C.M.; Craparo, G. Traumatic Distress, Alexithymia, Dissociation, and Risk of Addiction During the First Wave of COVID-19 in Italy: Results from a Cross-Sectional Online Survey on a Non-Clinical Adult Sample. Int. J. Ment. Health Addict. 2021, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Craparo, G.; Gori, A.; Dell’Aera, S.; Costanzo, G.; Fasciano, S.; Tomasello, A.; Vicario, C.M. Impaired Emotion Recognition Is Linked to Alexithymia in Heroin Addicts. PeerJ 2016, 4, e1864. [Google Scholar] [CrossRef] [PubMed]
- Martino, G.; Caputo, A.; Schwarz, P.; Bellone, F.; Fries, W.; Quattropani, M.C.; Vicario, C.M. Alexithymia and Inflammatory Bowel Disease: A Systematic Review. Front. Psychol. 2020, 11, 1763. [Google Scholar] [CrossRef]
- Chimenti, M.S.; Fonti, G.L.; Conigliaro, P.; Hitaj, J.; Triggianese, P.; Teoli, M.; Galluzzo, M.; Talamonti, M.; Kroegler, B.; Greco, E.; et al. Evaluation of Alexithymia in Patients Affected by Rheumatoid Arthritis and Psoriatic Arthritis: A Cross-Sectional Study. Medicine 2019, 98, e13955. [Google Scholar] [CrossRef]
- Dowlati, Y.; Herrmann, N.; Swardfager, W.; Liu, H.; Sham, L.; Reim, E.K.; Lanctôt, K.L. A Meta-Analysis of Cytokines in Major Depression. Biol. Psychiatry 2010, 67, 446–457. [Google Scholar] [CrossRef]
- Keller, L.K.; Zöschg, S.; Grünewald, B.; Roenneberg, T.; Schulte-Körne, G. Chronotype and depression in adolescents—a review. Z. Kinder Jugendpsychiatr. Psychother. 2016, 44, 113–126. [Google Scholar] [CrossRef][Green Version]
- Lucifora, C.; Grasso, G.M.; Nitsche, M.A.; D’Italia, G.; Sortino, M.; Salehinejad, M.A.; Falzone, A.; Avenanti, A.; Vicario, C.M. Enhanced Fear Acquisition in Individuals with Evening Chronotype. A Virtual Reality Fear Conditioning/Extinction Study. J. Affect. Disord. 2022, 311, 344–352. [Google Scholar] [CrossRef]
- Chakradeo, P.S.; Keshavarzian, A.; Singh, S.; Dera, A.E.; Esteban, J.P.G.; Lee, A.A.; Burgess, H.J.; Fogg, L.; Swanson, G.R. Chronotype, Social Jet Lag, Sleep Debt and Food Timing in Inflammatory Bowel Disease. Sleep Med. 2018, 52, 188–195. [Google Scholar] [CrossRef]
- Kulmatycki, K.M.; Jamali, F. Drug Disease Interactions: Role of Inflammatory Mediators in Pain and Variability in Analgesic Drug Response. J. Pharm. Pharm. Sci. 2008, 10, 554. [Google Scholar] [CrossRef] [PubMed][Green Version]
- O’Brien, S.M.; Scott, L.V.; Dinan, T.G. Cytokines: Abnormalities in Major Depression and Implications for Pharmacological Treatment. Hum. Psychopharmacol. Clin. Exp. 2004, 19, 397–403. [Google Scholar] [CrossRef]
- Mesripour, A.; Shahnooshi, S.; Hajhashemi, V. Celecoxib, Ibuprofen, and Indomethacin Alleviate Depression-like Behavior Induced by Interferon-Alfa in Mice. J. Complementary Integr. Med. 2019, 17. [Google Scholar] [CrossRef] [PubMed]
- Miranda, D.O.; Anatriello, E.; Azevedo, L.R.; Santos, J.C.; Cordeiro, J.F.C.; Peria, F.M.; Flória-Santos, M.; Pereira-Da-Silva, G. Fractalkine (C-X3-C Motif Chemokine Ligand 1) as a Potential Biomarker for Depression and Anxiety in Colorectal Cancer Patients. Biomed. Rep. 2017, 7, 188–192. [Google Scholar] [CrossRef]
- Merendino, R.A.; Di Pasquale, G.; De Luca, F.; Di Pasquale, L.; Ferlazzo, E.; Martino, G.; Palumbo, M.C.; Morabito, F.; Gangemi, S. Involvement of Fractalkine and Macrophage Inflammatory Protein-1 Alpha in Moderate-Severe Depression. Mediat. Inflamm. 2004, 13, 205–207. [Google Scholar] [CrossRef]
- Müller, N. COX-2 Inhibitors, Aspirin, and Other Potential Anti-Inflammatory Treatments for Psychiatric Disorders. Front. Psychiatry 2019, 10, 375. [Google Scholar] [CrossRef] [PubMed]
- Berthold-Losleben, M.; Heitmann, S.; Himmerich, H. Anti-Inflammatory Drugs in Psychiatry. Inflamm. Allergy-Drug Targets 2009, 8, 266–276. [Google Scholar] [CrossRef] [PubMed]
- Miller, A.H.; Raison, C.L. Are Anti-Inflammatory Therapies Viable Treatments for Psychiatric Disorders?: Where the Rubber Meets the Road. JAMA Psychiatry 2015, 72, 527–528. [Google Scholar] [CrossRef]
- Uzzan, S.; Azab, A.N. Anti-TNF-α Compounds as a Treatment for Depression. Molecules 2021, 26, 2368. [Google Scholar] [CrossRef]
- Lee, Y.; Mansur, R.B.; Brietzke, E.; Carmona, N.E.; Subramaniapillai, M.; Pan, Z.; Shekotikhina, M.; Rosenblat, J.D.; Suppes, T.; Cosgrove, V.E.; et al. Efficacy of Adjunctive Infliximab vs. Placebo in the Treatment of Anhedonia in Bipolar I/II Depression. Brain Behav. Immun. 2020, 88, 631–639. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Murdaca, G.; Paladin, F.; Casciaro, M.; Vicario, C.M.; Gangemi, S.; Martino, G. Neuro-Inflammaging and Psychopathological Distress. Biomedicines 2022, 10, 2133. https://doi.org/10.3390/biomedicines10092133
Murdaca G, Paladin F, Casciaro M, Vicario CM, Gangemi S, Martino G. Neuro-Inflammaging and Psychopathological Distress. Biomedicines. 2022; 10(9):2133. https://doi.org/10.3390/biomedicines10092133
Chicago/Turabian StyleMurdaca, Giuseppe, Francesca Paladin, Marco Casciaro, Carmelo Mario Vicario, Sebastiano Gangemi, and Gabriella Martino. 2022. "Neuro-Inflammaging and Psychopathological Distress" Biomedicines 10, no. 9: 2133. https://doi.org/10.3390/biomedicines10092133
APA StyleMurdaca, G., Paladin, F., Casciaro, M., Vicario, C. M., Gangemi, S., & Martino, G. (2022). Neuro-Inflammaging and Psychopathological Distress. Biomedicines, 10(9), 2133. https://doi.org/10.3390/biomedicines10092133







